Pericarditis
| Pericarditis | ||
 | ||
|---|---|---|
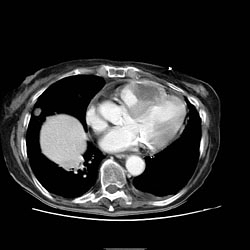
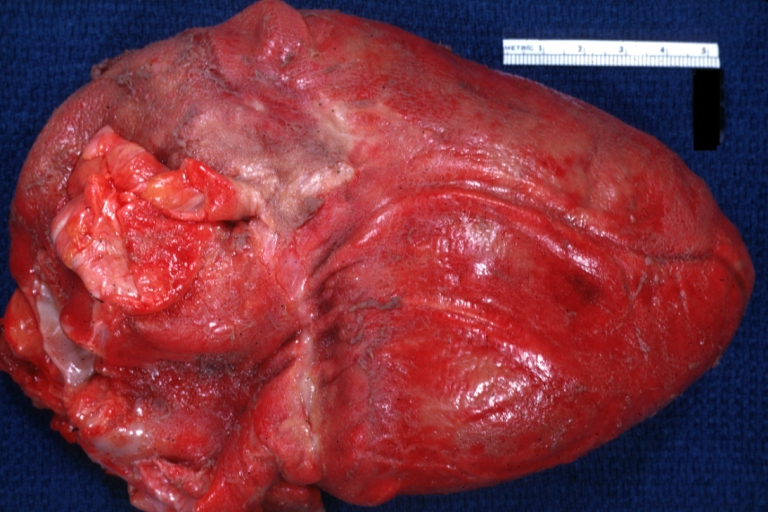
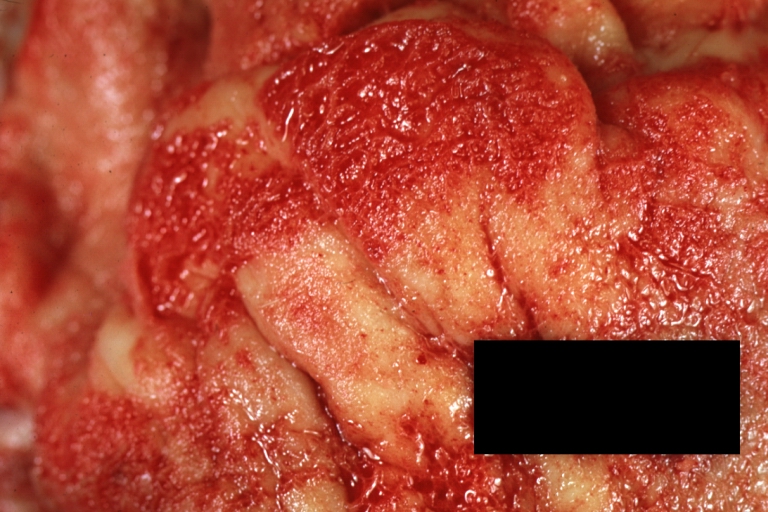
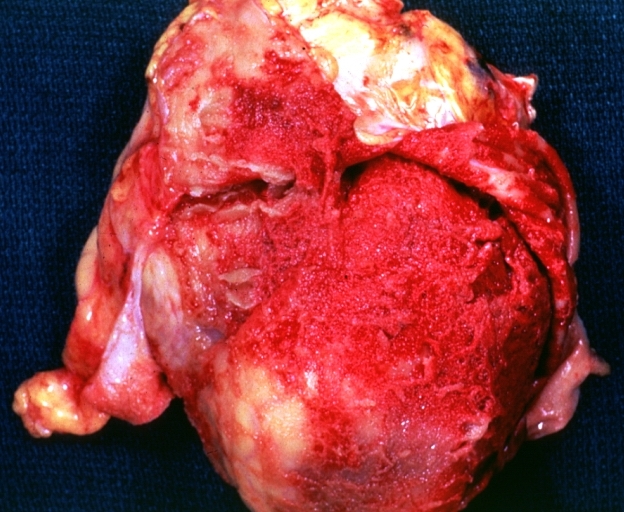
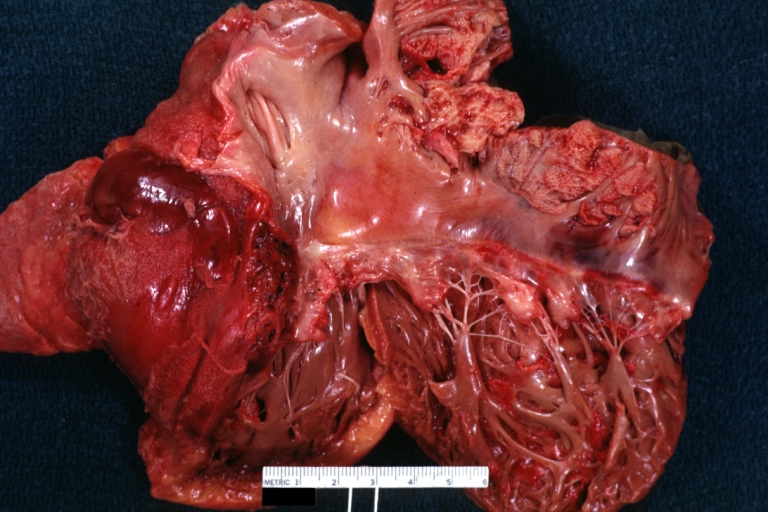
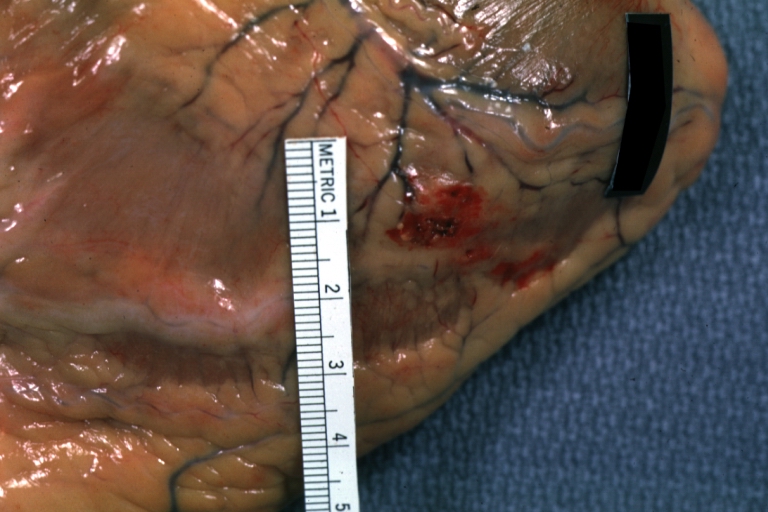
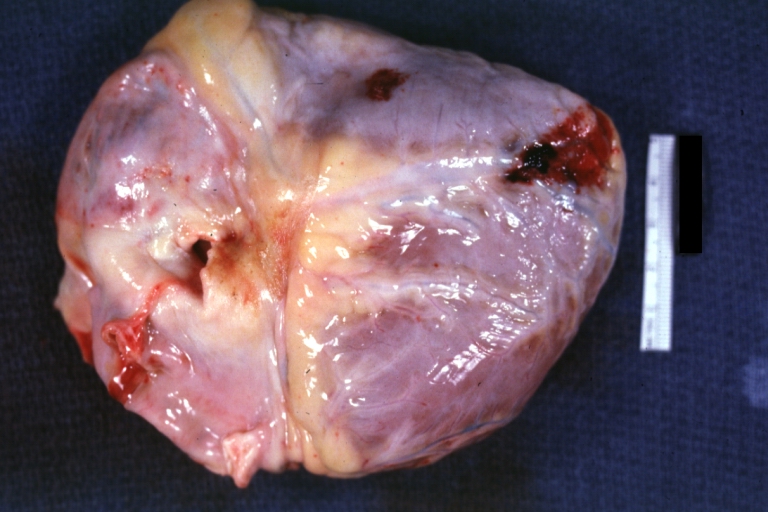
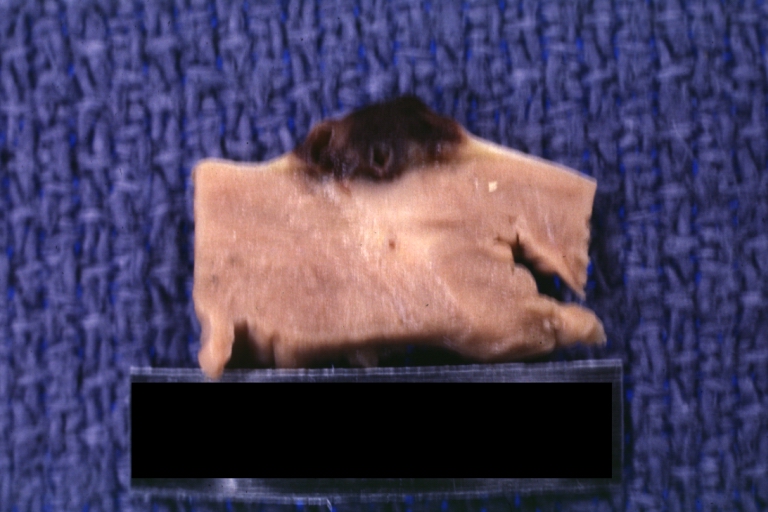
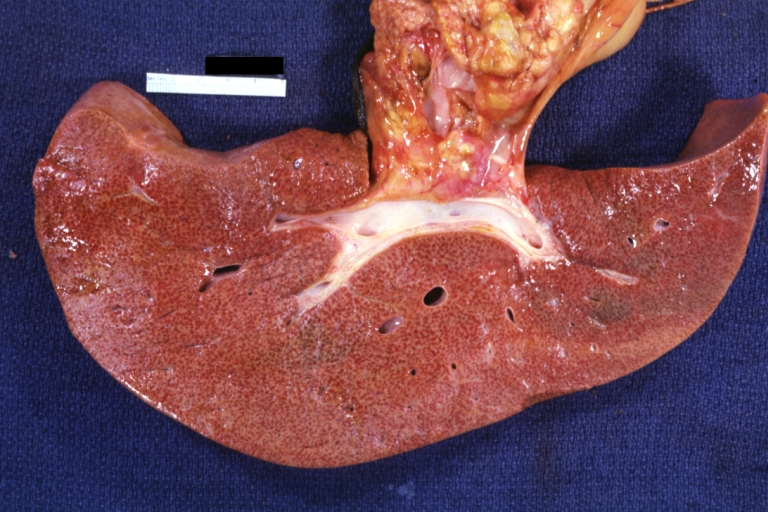
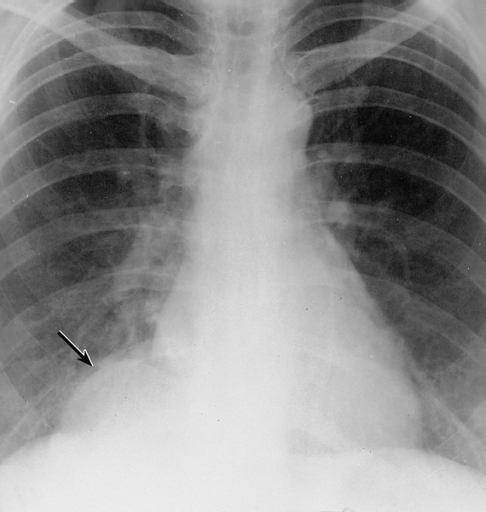
| Mesothelial cyst of the pericardium. Note the rounded mass in the right costophrenic angle (arrow). Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | ||
| ICD-10 | I01.0, I09.2, I30-I32 | |
| ICD-9 | 420.90 | |
| DiseasesDB | 9820 | |
| MedlinePlus | 000182 | |
| eMedicine | med/1781 emerg/412 | |
| MeSH | C14.280.720 | |
|
WikiDoc Resources for Pericarditis |
|
Articles |
|---|
|
Most recent articles on Pericarditis Most cited articles on Pericarditis |
|
Media |
|
Powerpoint slides on Pericarditis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Pericarditis at Clinical Trials.gov Clinical Trials on Pericarditis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Pericarditis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Pericarditis Discussion groups on Pericarditis Patient Handouts on Pericarditis Directions to Hospitals Treating Pericarditis Risk calculators and risk factors for Pericarditis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Pericarditis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss Pericarditis further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
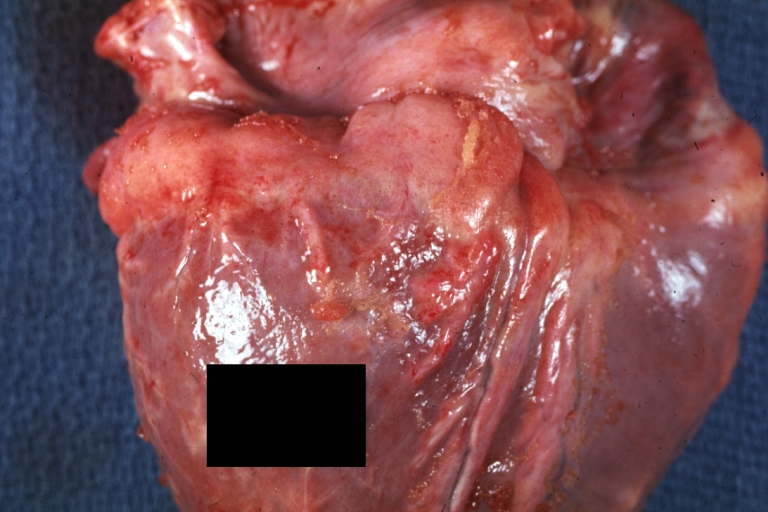
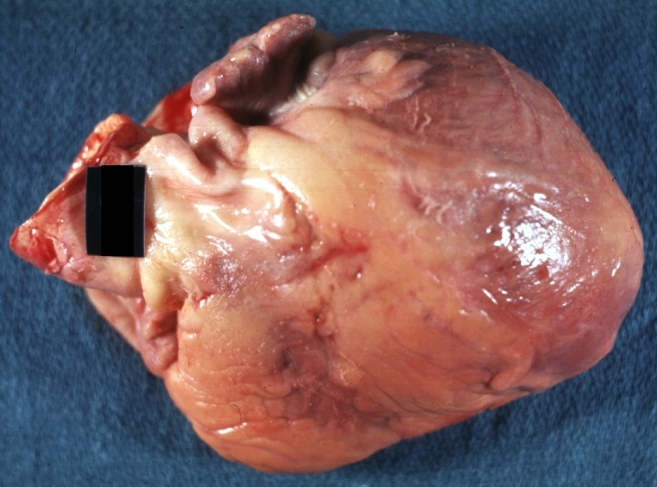
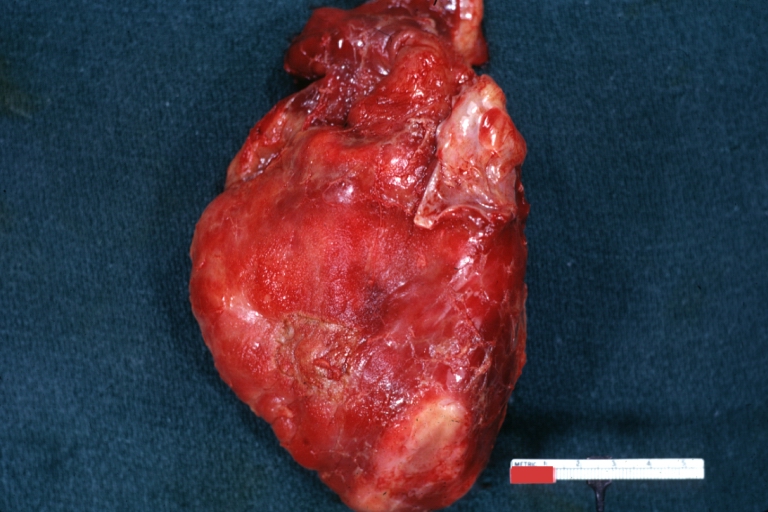
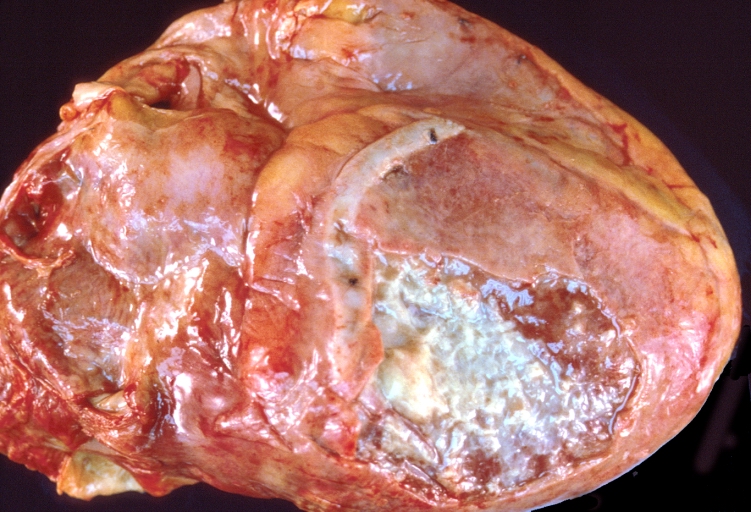
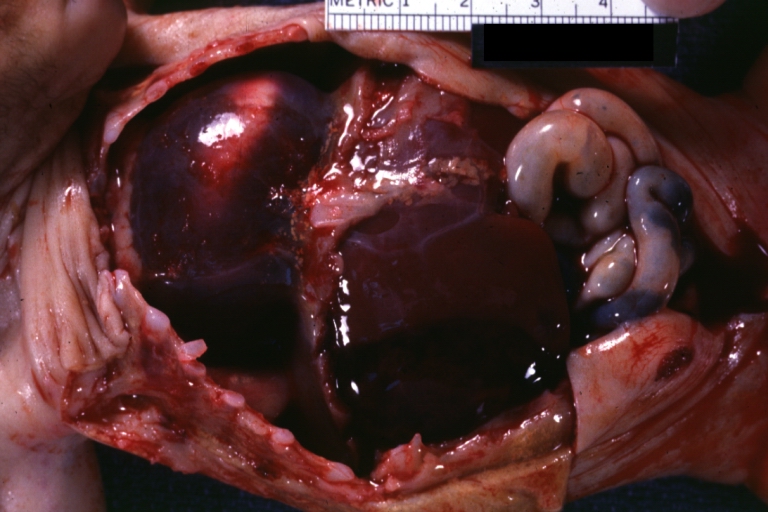
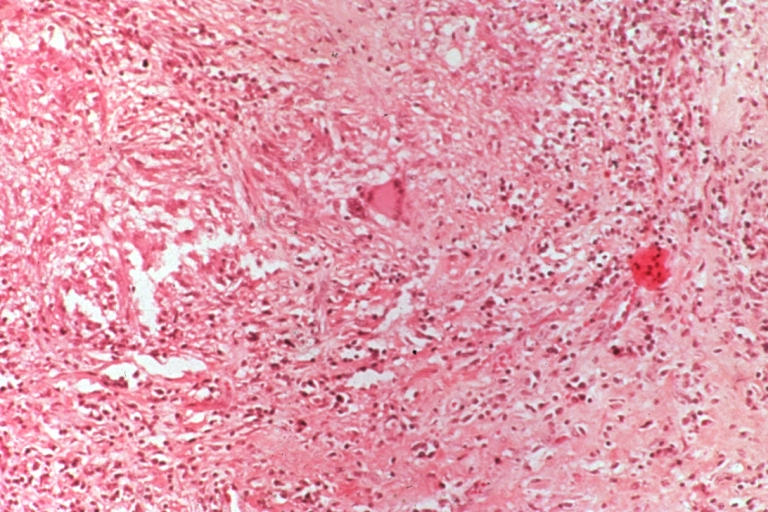
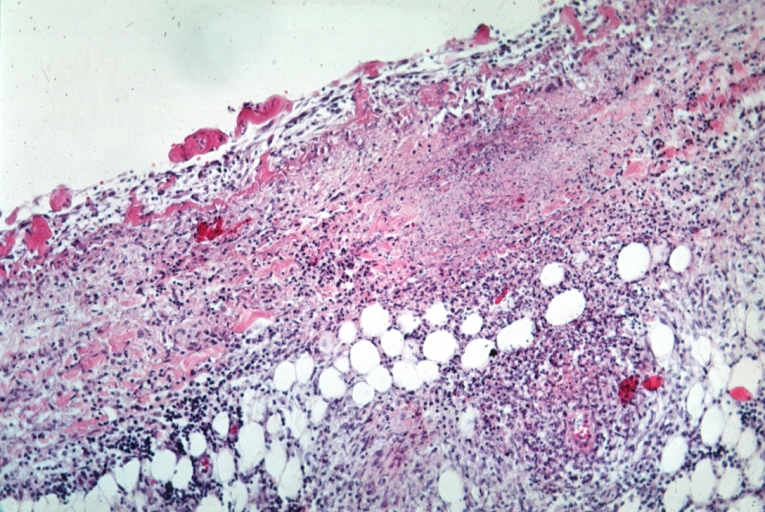
Pericarditis is an inflammation of the pericardium (the fibrous sac surrounding the heart). Pericarditis is further classified according to the composition of the inflammatory exudate: serous, purulent, fibrinous, and hemorrhagic types occur.
Acute pericarditis is more common than chronic pericarditis, and can occur as a complication of infections, immunologic conditions, or heart attack.
Pathophysiology & Etiology
Pericarditis is inflammation of the pericardium, the double-walled sac that contains the heart and the roots of the great vessels. There can be an accompanying accumulation of fluid that can be either serous (free flowing fluid) or fibrinous (an exudate, which is a thick fluid composed of proteins, fibrin strands, inflammatory cells, cell breakdown products, and sometimes bacteria). Vascular congestion of the pericardium is also present. The underlying myocardium may or may not be inflammed as well. If the myocardium is involved in the inflammatory process, then this is called myopericarditis, and the CK and troponin may be elevated.
The signs and symptoms of acute pericarditis can be misleading because they can occur as part of a constellation of symptoms associated with another illness.
The Most Frequent Causes of Pericarditis [1]
- (35%) Neoplastic
- (23%) Autoimmune
- (21%) Viral - adenovirus, enterovirus, cytomegalovirus, influenza virus, hepatitis B virus, and herpes simplex virus, etc
- ( 6%) Bacterial (other than tuberculosis)
- ( 6%) Uremia
- ( 4%) Tuberculosis
- ( 4%) Idiopathic
- (remaining) trauma, drugs, post-AMI, myocarditis, dissecting aortic aneurysm, radiation
Complete List of Causes of pericarditis
- Infectious:
- Viral: Coxsackie B Virus, Echovirus, Adenovirus (less commonly: Mumps, Influenza, varicella, Hepatitis B and CMV-especially in HIV patients.) Usually associated with a viral prodrome and acute pericarditis.
- Tuberculosis: usually bloody, protein greater than 2.5. Initially mostly polymorphonuclear cells, later lymphocytes, monocytes and plasma cells. Usually develops very slowly with significant fibrous reaction. Initially effusive then becomes constrictive.
- Purulent: Pneumococcus, Streptococcus and Staphylococcus most common. Also Proteus, E.coli, Psuedomonas, Klebsiella, Brucellosis, Salmonella, Neisseria, Haemophilus influenza, Tularemia, Legionella, preodominantly by hematogenous spread and approximately 20% by contiguous spread. Usually these patients are quite ill.
- Fungal: Histoplasmosis, Coccidiomycosis, Aspergillus, Blastomycosis, Candida.
- Other: Toxoplasmosis, Amebiasis, Mycoplasma, Nocardia, Actinomycosis, Echinococcus, Lyme disease (usually myopericarditis associated with conduction abnormalities).
- Neoplastic:
- Predominantly lung, breast, leukemia, lymphomas (Hodgkins and non-Hodgkins). Less commonly GI malignancies, ovarian cancer, sarcomas and melanomas, metastic, hematogenous, carcinoma, carcinoid, Sipple syndrome, mesothelioma, fibroma, lipoma . Also Kaposis sarcoma in HIV positive patients.
- Uremic:
- Uremic pericarditis is seen in up to 20% of uremic patients requiring chronic hemodialysis. The mechanism is unknown. Most commonly there is a small effusion associated with pain and a pericardial friction rub, but there can be a large effusion and present with tamponade.
- Autoimmune:
- Systemic Lupus Erythematosus or SLE: Pericarditis usually occurs in the setting of disease flares (systemic symptoms, high erythrocyte sedimentation rate (ESR) , +ANA, +dsDNA, pleural effusions). Occurs in 20-40% of patients with SLE during the course of the disease. Usually the fluid is serous or grossly bloody. Analysis of the fluid usually reveals a high protein and low glucose content. Typically WBC count is less than 10K, and is made up of primarily polymorphonuclear cells (PMNs).
- Rheumatoid arthritis or RA: Pericarditis can occur without active joint involvement. Also serous or bloody. Usually the protein is > 5 mg/dl, and the glucose is low (<45). The WBC is high at 20-90K. Complement is usually low, and the latex fixation test is usually positive.
- Other: Acute rheumatic fever, scleroderma, mixed connective tissue disease, Wegener's, PAN.
- Traumatic:
- After chest trauma, throacic surgery, PCM insertion, Valvuloplasty. Also from esophageal rupture, pancreatic-pericardial fistula (check amylase), penetrating chest injury, esophogeal perforation, gastric perforation, during catheterization (pacemaker insertion, cathether ablation for arrhythmias, diagnostic, PCI with coronary dissection).
- Drugs:
- Usually associated with small effusions. Common culprits include hydralazine, procainamide, DOH, isoniazid, phenylbutazone, dantrolene, doxorubicin, methylsergide, penicillin.
- Hypothyroidism:
- Usually in conjunction with clinically severe hypothyroidism. Most early case reports associated with myxedema and patients also had ascites, pleural effusions and uveal edema. Often resolves with thyroid replacement therapy.
- Other:
- Post-MI (Dresslers), post-pericardiotomy, radiation, dissecting aortic aneurysm, chylopericardium (from thoracic duct obstruction secondary to tumor, surgical procedure, trauma, TB, congenital). Also, sarcoidosis, amyloidosis, IBD, Whipple's, temporal arteritis and Behcet syndrome).
Clinical presentation
Chest pain, radiating to the back and relieved by sitting up forward and worsened by lying down, is the classical presentation. Other symptoms of pericarditis may include dry cough, fever, fatigue and anxiety. Pericarditis can be misdiagnosed as myocardial infarction, and vice versa.
The classic sign of pericarditis is a friction rub. Other signs include ST-elevation and PR-depression on EKG (all leads); cardiac tamponade (pulsus paradoxus with hypotension), and congestive heart failure (elevated jugular venous pressure with peripheral edema).
Natural History
Most cases of acute idiopathic pericarditis resolve without complications or recurrence. Complications may include:
Types & Forms of Pericarditis
- A. Congenital Diseases of the Pericardium
- B. Acquired Diseases of the Pericardium
B. Acquired Diseases of the Pericardium
Acute Pericarditis
Chronic pericarditis
Chronic pericardial inflammation (>3 months) includes effusive, adhesive, and constrictive forms. It is important to differentiate chronic inflammatory effusions from noninflammatory hydropericardium (congestive heart failure). Symptoms are usually mild (chest pain, palpitations, fatigue), related to the degree of chronic cardiac compression and residual pericardial inflammation.
The diagnostic algorithm is similar as in acute pericarditis (see above and Table 2 of the original guideline document). The detection of the curable causes (e.g., tuberculosis, toxoplasmosis, myxedema, autoimmune, and systemic diseases) allows specific therapy with high success rate. Symptomatic treatment is as in acute pericarditis. Intrapericardial instillation of crystalloid nonabsorbable corticosteroids is highly efficient in autoreactive forms. Pericardiocentesis is indicated as a diagnostic and therapeutic procedure. If the recurrences are frequent, pleuropericardial fenestration and percutaneous balloon pericardiotomy may be appropriate (level of evidence B, class IIb). For chronic persistent/recurrent large effusions despite intrapericardial therapy or balloon pericardiotomy, pericardiectomy should be considered.
Recurrent pericarditis
The term recurrent pericarditis encompasses (1) the intermittent type (widely varying symptom-free interval without therapy) and (2) the incessant type (discontinuation of anti-inflammatory therapy always ensures a relapse). Mechanisms suggested to explain recurrence include (1) insufficient dose or/and insufficient treatment duration of antiphlogistics or corticoids in an autoimmune pericardial disease, (2) early corticosteroids treatment causing augmented viral deoxyribonucleic acid/ribonucleic acid (DNA/RNA) replication in pericardial tissue leading to increased viral antigen exposure, (3) reinfection, and (4) exacerbation of the connective tissue disease. Evidence for an immunopathological process includes (1) the latent period lasting for months; (2) the presence of anti-heart antibodies; and (3) the quick response to steroid treatment and the similarity and coexistence of recurrent pericarditis with other autoimmune conditions (lupus, serum sickness, polyserositis, postpericardiotomy/postmyocardial infarction syndrome, celiac disease, dermatitis herpetiformis, frequent arthralgias, eosinophilia, allergic drug reaction, and history of allergy). Evidence of a potential underlying genetic disorder in recurrent pericarditis is rare familial clustering with autosomal dominant inheritance with incomplete penetrance and sex-linked inheritance (chronic recurrent pericarditis associated with ocular hypertension) suggested in two families. Precordial pain, often with a pleuritic component, is characteristic. Fever, pericardial rub, dyspnoea, elevated erythrocyte sedimentation rate, and electrocardiographic changes may also occur. Massive pericardial effusion, cardiac tamponade, and pericardial constriction are rare.
Symptomatic management relies on exercise restriction and the regimen used in acute pericarditis. Indomethacin should be avoided in elderly patients due to its flow reduction in the coronaries. Colchicine inhibits mitoses in the cell nucleus, binds to tubulin, inhibits various polymorphonuclear functions, and interferes with transcellular movement of collagen. It was effective for recurrent pericarditis when NSAIDs and corticosteroids failed to prevent relapses. During 1,004 months of colchicine treatment, only 13.7% new recurrences occurred. During the 2,333 months of follow-up, 60.7% of the patients remained recurrence-free. The recommended dose is two mg/day for one or two days, followed by one mg/day (level of evidence B, class I). Corticosteroids should be used only in patients with poor general condition or in frequent crises (level of evidence C, class IIa). A common mistake is to use a dose too low to be effective or to taper the dose too rapidly. The recommended regimen is prednisone 1 to 1.5 mg/kg, for at least one month. If patients do not respond adequately, azathioprine (75 to 100 mg/day) or cyclophosphamide can be added. Tapering of corticoids should occur over a three-month period. If symptoms recur during the taper, return to the last dose that suppressed the manifestations, maintain that dose for 2 to 3 weeks, and then recommence tapering. Towards the end of the taper, introduce anti-inflammatory treatment with colchicines or NSAIDs. Renewed treatment should continue for at least three months. Pericardiectomy is indicated only in frequent and highly symptomatic recurrences resistant to medical treatment (level of evidence B, class IIa). Before pericardiectomy, the patient should be on a steroid-free regimen for several weeks. Post pericardiectomy recurrences were also demonstrated, possibly due to incomplete resection of the pericardium.
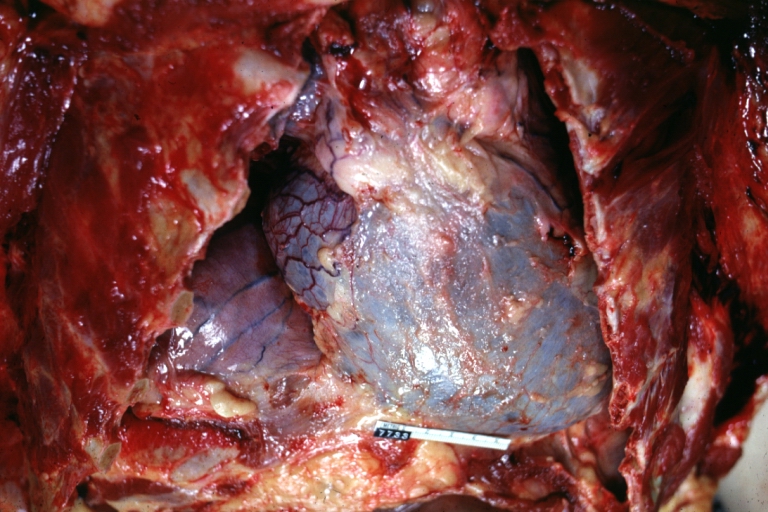
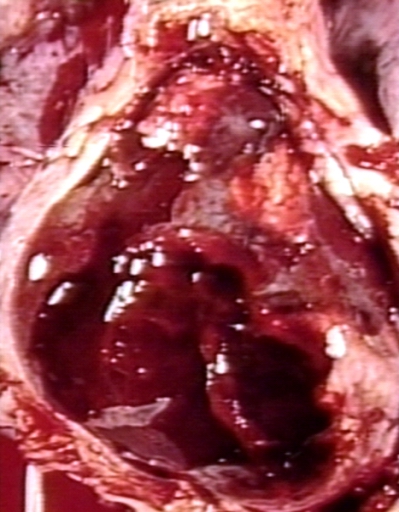
Pericardial effusion and cardiac tamponade
Pericardial effusion may appear as transudate (hydropericardium), exudate, pyopericardium, or haemopericardium. Large effusions are common with neoplastic, tuberculous, cholesterol, uremic pericarditis, myxedema, and parasitoses. Effusions that develop slowly can be remarkably asymptomatic, while rapidly accumulating smaller effusions can present with tamponade. Loculated effusions are more common when scarring has supervened (e.g., postsurgical, posttrauma, postpurulent pericarditis). Massive chronic pericardial effusions are rare (2 to 3.5% of all large effusions). Cardiac tamponade is the decompensated phase of cardiac compression caused by effusion accumulation and the increased intrapericardial pressure. In "surgical" tamponade, intrapericardial pressure is rising rapidly, in the matter of minutes to hours (i.e., haemorrhage), whereas a low-intensity inflammatory process is developing in days to weeks before cardiac compression occurs ("medical" tamponade). The volume of fluid causing tamponade varies inversely with both parietal pericardial stiffness and thickness (150 to 2,000 mL). In local compression, dyspnoea, dysphagia, hoarseness (recurrent laryngeal nerve), hiccups (phrenic nerve), or nausea (diaphragm) can occur. Heart sounds are distant. Compression of the base of the lung results in a dullness under the left scapula (Bamberger–Pins–Ewart's sign). In tamponade, chest discomfort, tachypnea, and dyspnoea on exertion progress to orthopnoea, cough, and dysphagia, occasionally also with episodes of unconsciousness. Insidiously developing tamponade may present with the signs of its complications (renal failure, abdominal plethora, shock liver and mesenteric ischaemia). In 60% of the patients, the cause of pericardial effusion may be a known medical condition. Tamponade without two or more inflammatory signs (typical pain, pericardial friction rub, fever, diffuse ST segment elevation) is usually associated with a malignant effusion (likelihood ratio 2.9). Electrocardiography may demonstrate diminished QRS and T-wave voltages, PR-segment depression, ST-T changes, bundle branch block, and electrical alternans (rarely seen in the absence of tamponade). In chest radiography large effusions are depicted as globular cardiomegaly with sharp margins ("water bottle" silhouette). On well-penetrated lateral radiographies, or better on cine films, pericardial fluid is suggested by lucent lines within the cardiopericardial shadow (epicardial halo sign or various other terms for this phenomenon). Recently, it was suggested that this sign might be useful for fluoroscopic guidance of pericardiocentesis. The separation of pericardial layers can be detected in echocardiography, when the pericardial fluid exceeds 15 to 35 mL (Please refer to figure 1 of the original guideline document for information on the Horowitz classification of pericardial effusions). The size of effusions can be graded as (1) small (echo-free space in diastole <10 mm), (2) moderate (at least >10 mm posteriorly), (3) large (>20 mm), or (4) very large (>20 mm and compression of the heart). In large pericardial effusions, the heart may move freely within the pericardial cavity ("swinging heart"). This exaggerated motion of the heart induces "pseudo" motions like pseudomitral valve prolapse, pseudosystolic anterior motion of the mitral valve, paradoxical motion of the interventricular septum, and midsystolic aortic valve closure. Importantly, effusion size is an overall predictor of prognosis: large effusions generally indicate more serious disease. Two-dimensional echocardiography also provides information about the nature of the fluid, suggesting the presence of fibrin, clot, tumour, air, and calcium. Intrapericardial bands, often found after radiation of the chest, are frequently combined with a thick visceral or parietal pericardium. Rarely tumour masses, sometimes cauliflower-like, are found within or adjacent to the pericardium. In parasternal long-axis view, pericardial fluid reflects at the posterior atrioventricular groove, while pleural fluid continues under the left atrium, posterior to the descending aorta. Diagnostic pitfalls are small loculated effusions, haematoma, cysts, tumours, foramen of Morgagni hernia, hiatus hernia, lipodystrophia with paracardial fat, inferior left pulmonary vein, left pleural effusion, mitral annulus calcification, giant left atrium, epicardial fat (best differentiated in CT), and left ventricular pseudoaneurysm. Metastatic infiltration of the pericardium may masquerade pericardial tamponade in echocardiography in patients with no pericardial effusion. After open-heart surgery, localized effusion at the posterior wall can be found with complete compression of the right atrium leading to cardiac tamponade. This may be misinterpreted as atrial myxoma or other cardiac tumour. When bleeding into the pericardium occurs and thrombosis develops, the typical echolucent areas may disappear, so that development of cardiac tamponade may be overlooked. Transesophageal echocardiography is particularly useful in postoperative loculated pericardial effusion or intrapericardial clot as well as in identifying metastases and pericardial thickening. CT, spin-echo, and cine MRI can also be used to assess the size and extent of simple and complex pericardial effusions. The effusions measured by CT or by MRI may tend to be larger than by echocardiography. Up to one-third of patients with asymptomatic large pericardial chronic effusion developed unexpected cardiac tamponade. Triggers for tamponade include hypovolemia, paroxysmal tachyarrhythmia, and intercurrent acute pericarditis; often no trigger is identifiable. Major diagnostic findings in cardiac tamponade are noted in Table 4 and Focus box 2 of the original guideline document.
Pericardiocentesis may not be necessary when the diagnosis can be made based on other systemic features or the effusions are very small or resolving under anti-inflammatory treatment. Where doubt remains, pericardiocentesis, pericardioscopy, and epicardial and pericardial biopsy (including PCR, immunocytochemistry, and immunohistochemistry) may be valuable (level of evidence B, class IIa). Please see above and refer to focus box 1 of the original guideline document for information on pericardiocentesis. Haemodynamic compromise and cardiac tamponade is an absolute indication for drainage (class I). Patients with dehydration and hypovolemia may temporarily improve with intravenous fluids enhancing ventricular filling. Pericardiocentesis is not applicable in wounds, ruptured ventricular aneurysm, or dissecting aortic haematoma, when clotting makes needle evacuation impossible so that surgical drainage with suppression of bleeding sources is mandatory. Loculated effusions may require thoracoscopic drainage, subxyphoid window, or open surgery. All patients should be monitored for postdrainage decompensation. Whenever possible, treatment should be aimed at the underlying aetiology rather than the effusion itself. However, even in idiopathic effusions extended pericardial catheter drainage (3 + 2 days, range 1 to 13 days) was associated with a trend to lower recurrence rates (6% vs. 23%) than in those without catheter drainage during the follow-up of 3.8 + 4.3 years. Resistant neoplastic processes require intrapericardial treatment, percutaneous balloon pericardiotomy, or rarely pericardiectomy. Surgical approach is recommended only in patients with very large chronic effusion (with or without symptoms) in whom repeated pericardiocentesis and/or intrapericardial therapy were not successful.
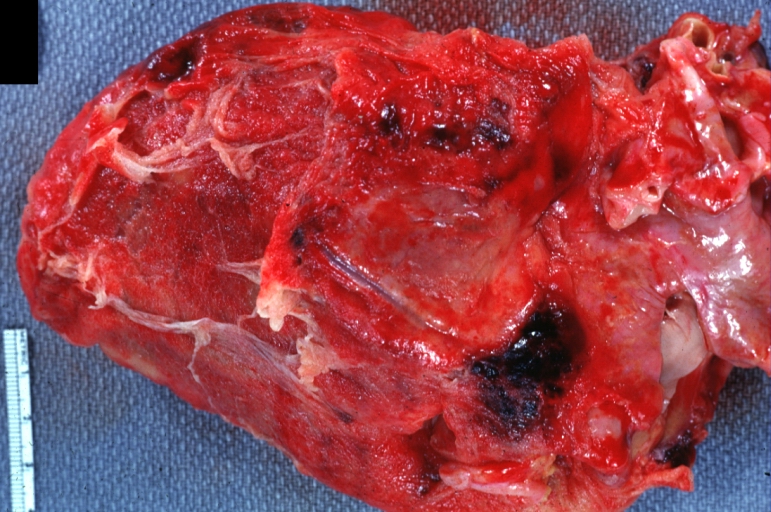
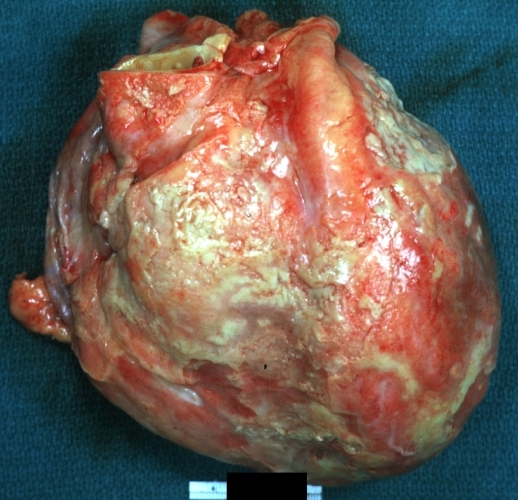
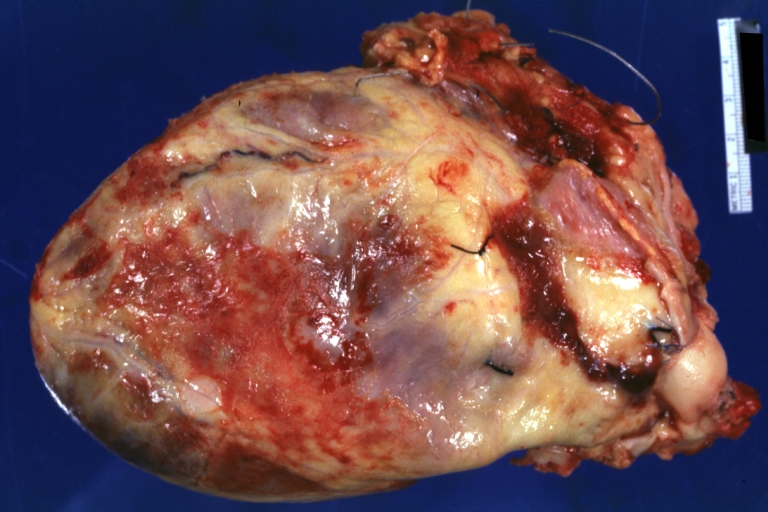
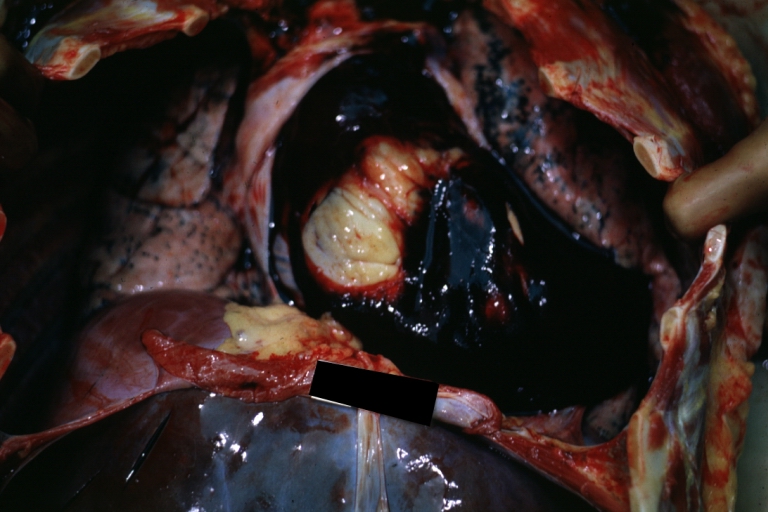
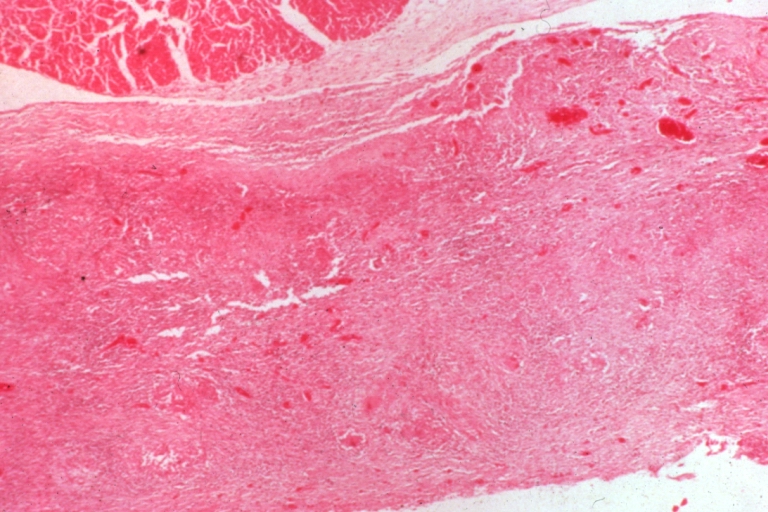
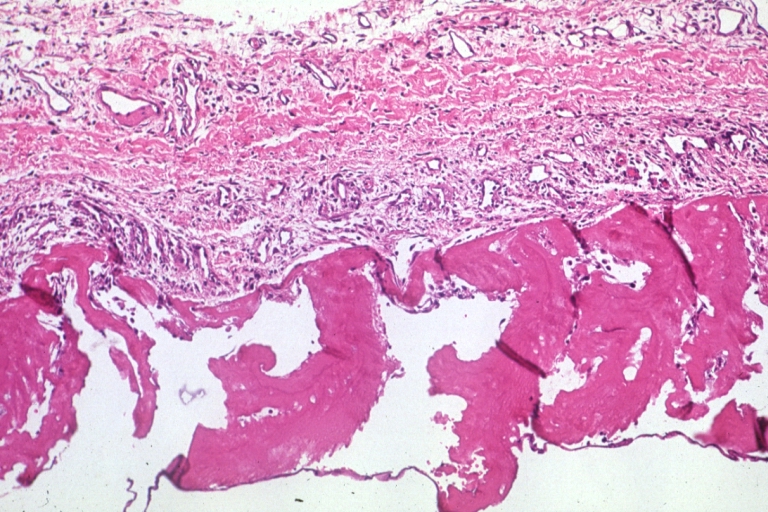
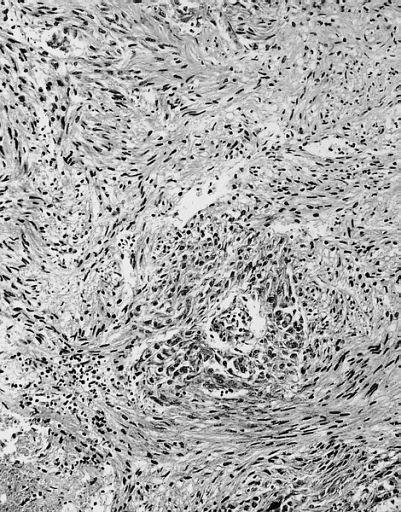
Constrictive pericarditis
Constrictive pericarditis is a rare but severely disabling consequence of the chronic inflammation of the pericardium, leading to an impaired filling of the ventricles and reduced ventricular function. Tuberculosis, mediastinal irradiation, and previous cardiac surgical procedures are frequent causes of the disease, which can present in several pathoanatomical forms (please refer to figure 2 of the original guideline document for information on the pathoanatomical forms of constrictive pericarditis vs. restrictive cardiomyopathy). Constrictive pericarditis may rarely develop only in the epicardial layer in patients with previously removed parietal pericardium. Transient constrictive pericarditis is rare entity, distinguished by its self-limiting nature. Patients complain about fatigue, peripheral oedema, breathlessness, and abdominal swelling, which may be aggravated by a protein-loosing enteropathy. Typically, there is a long delay between the initial pericardial inflammation and the onset of constriction. In decompensated patients, venous congestion, hepatomegaly, pleural effusions, and ascites may occur. Haemodynamic impairment of the patient can be additionally aggravated by a systolic dysfunction due to myocardial fibrosis or atrophy. Clinical, echocardiographic, and haemodynamic parameters can be derived from Table 5 of the original guideline document. Differential diagnosis has to include acute dilatation of the heart, pulmonary embolism, right ventricular infarction, pleural effusion, chronic obstructive lung diseases, and restrictive cardiomyopathy. The best way to distinguish constrictive pericarditis from restrictive cardiomyopathy is the analysis of respiratory changes with or without changes of preload by Doppler and/or tissue Doppler echocardiography, but physical findings, ECG, chest radiography, CT and MRI, haemodynamics, and endomyocardial biopsy may be helpful as well (Please refer to table 6 of the original guideline document for information on differential diagnosis: constrictive pericarditis vs. restrictive cardiomyopathy).
Pericardiectomy is the only treatment for permanent constriction. The indications are based upon clinical symptoms, echocardiography findings, CT/MRI, and heart catheterisation. There are two standard approaches, both aiming at resecting the diseased pericardium as far as possible: (1) the antero-lateral thoracotomy (fifth intercostal space) and (2) median sternotomy (faster access to the aorta and right atrium for extracorporeal circulation). A primary installation of cardiopulmonary bypass is not recommended, due to the enhanced diffuse bleeding during dissection of the pericardium, following systemic heparinisation. If severe calcified adhesions between peri- and epicardium or a general affection of the epicardium ("outer porcelain heart") are present, surgery carries a high risk of either incomplete success or severe myocardial damage. An alternative approach in such cases may be a "laser shaving" using an Excimer laser. Areas of strong calcification or dense scarring may be left as islands to avoid major bleeding. Pericardiectomy for constrictive pericarditis has a mortality rate of 6 to 12% in the current series. The complete normalization of cardiac haemodynamics is reported in only 60% of the patients. The deceleration time (DT) may remain prolonged, and postoperative respiratory variations of mitral/tricuspid flow are found in 9 to 25%. Left ventricular ejection fraction increases due to a better ventricular filling, but consistent changes of the left and right atrial sizes were not reported. Major complications include acute perioperative cardiac insufficiency and ventricular wall rupture. Cardiac mortality and morbidity at pericardiectomy is mainly caused by the presurgically unrecognised presence of myocardial atrophy or myocardial fibrosis (Please refer to figure 2 of the original guideline document for information on the pathoanatomical forms of constrictive pericarditis vs. restrictive cardiomyopathy). Myocardial atrophy in CT is characterized by (1) thinning of the interventricular septum and posterolateral wall (<1 cm), (2) reduction of the wall thickening during the cardiac cycle (<40%), and (3) reduction of the left-ventricular muscle mass (LVMM)/end-diastolic volume (EDV) ratio (<1). Myocardial fibrosis should be considered whenever the thickened/calcified pericardium is not separated from the myocardium by subepicardial fat and when the myocardial wall is showing wave-like appearance with wall thinning. Exclusion of patients with extensive myocardial fibrosis and/or atrophy led to a reduction of the mortality rate for pericardiectomy to 5%. Postoperative low cardiac output should be treated by fluid substitution and catecholamines, high doses of digitalis, and intra-aortic balloon pump in most severe cases. If indication for surgery was established early, long-term survival after pericardiectomy corresponds to that of the general population. However, if severe clinical symptoms were present for a longer period before surgery, even a complete pericardiectomy may not achieve a total restitution.
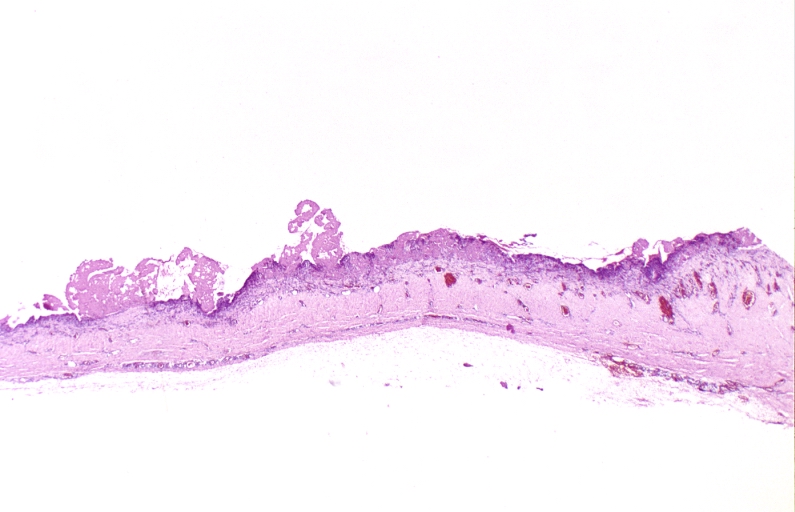
Pericardial cysts
Congenital pericardial cysts are uncommon and may have both unilocular and multilocular forms, with the diameter from 1 to 5 cm. Inflammatory cysts comprise pseudocysts as well as encapsulated and loculated pericardial effusions, caused by rheumatic pericarditis, bacterial infection, particularly tuberculosis, trauma, and cardiac surgery. Echinococcal cysts usually originate from ruptured hydatid cysts in the liver and lungs. Most patients are asymptomatic and cysts are detected incidentally on chest roentgenograms as an oval, homogeneous radiodense lesion, usually at the right cardiophrenic angle. However, the patients can also present with chest discomfort, dyspnoea, cough, or palpitations, due to the compression of the heart. Echocardiography is useful, but additional imaging by CT (density readings) or MRI is often needed.
The treatment for congenital and inflammatory cysts is percutaneous aspiration and ethanol sclerosis. If this is not feasible, video assisted thoracotomy or surgical resection may be necessary. The surgical excision of echinococcal cysts is not recommended. Percutaneous aspiration and instillation of ethanol or silver nitrate after pretreatment with Albendazole (800 mg/day 4 weeks) is safe and effective.
Specific forms of pericarditis
Viral pericarditis
Viral pericarditis is the most common infection of the pericardium. Inflammatory abnormalities are due to direct viral attack, the immune response (antiviral or anticardiac), or both. Early viral replication in pericardial and epimyocardial tissue elicits cellular and humoral immune responses against the virus and/or cardiac tissue. Viral genomic fragments in pericardial tissue may not necessarily replicate, yet they serve as a source of antigen to stimulate immune responses. Deposits of immunoglobulin M (IgM), immunoglobulin G (IgG), and occasionally immunoglobulin A (IgA), can be found in the pericardium and myocardium for years. Various viruses cause pericarditis (entero-, echo-, adeno-, cytomegalo-, Ebstein Barr-, herpes simplex-, influenza, parvo B19, hepatitis C, human immunodeficiency virus (HIV), etc.). Attacks of enteroviral pericarditis follow the seasonal epidemics of Coxsackie virus A+B and Echovirus infections. Cytomegalovirus pericarditis has an increased incidence in immunocompromised and HIV infected hosts. Infectious mononucleosis with sore throat, adenopathy, and positive mumps or Epstein Barr virus (EBV) serology may also present with pericarditis.
The diagnosis of viral pericarditis is not possible without the evaluation of pericardial effusion and/or pericardial/epicardial tissue, preferably by PCR or in-situ hybridisation (level of evidence B, class IIa) (please refer to focus boxes 3 to 5 of the original guideline document for information on analyses of pericardial effusion, pericardioscopy and epicardial/pericardial biopsy, and epicardial/pericardial tissue analyses). A fourfold rise in serum antibody levels is suggestive but not diagnostic for viral pericarditis (level of evidence B, class IIb).
Treatment of viral pericarditis is directed to resolve symptoms (see acute pericarditis), prevent complications, and eradicate the virus. In patients with chronic or recurrent symptomatic pericardial effusion and confirmed viral infection, the following specific treatment is under investigation: (1) cytomegalovirus (CMV) pericarditis: hyperimmunoglobulin – 1 time per day 4 mL/kg on day 0, 4, and 8; 2 mL/kg on day 12 and 16; (2) Coxsackie B pericarditis: Interferon alpha: 2.5 Mio. IU/m2 surface area subcutaneously 3x per week; (3) adenovirus and parvovirus B19 perimyocarditis: immunoglobulin treatment: 10 g intravenously at day 1 and 3 for 6 to 8 h.
Pericardial manifestation of HIV infection can be due to infective, noninfective, and neoplastic diseases (Kaposi sarcoma and/or lymphoma). Infective (myo)pericarditis results from the local HIV infection and/or from the other viral (cytomegalovirus, herpes simplex), bacterial (Staphylococcus aureus, Klebsiella pneumoniae, Mycobacterium avium, and tuberculosis) and fungal coinfections (Cryptococcus neoformans). In progressive disease the incidence of echocardiographically detected pericardial effusion is up to 40%. Cardiac tamponade is rare. During the treatment with retroviral compounds, lipodystrophy can develop (best demonstrated by MRI) with intense paracardial fat deposition leading to heart failure. Treatment is symptomatic, while in large effusions and cardiac tamponade pericardiocentesis is necessary. The use of corticoid therapy is contraindicated except in patients with secondary tuberculous pericarditis, as an adjunct to tuberculostatic treatment (level of evidence A, class I).
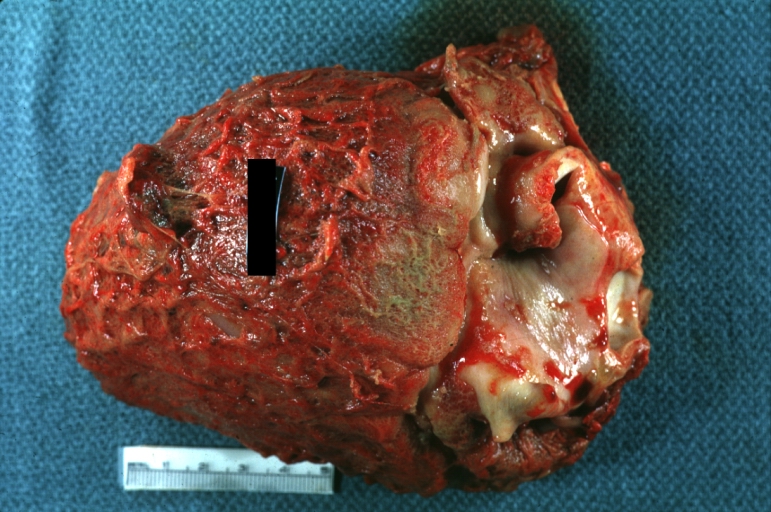
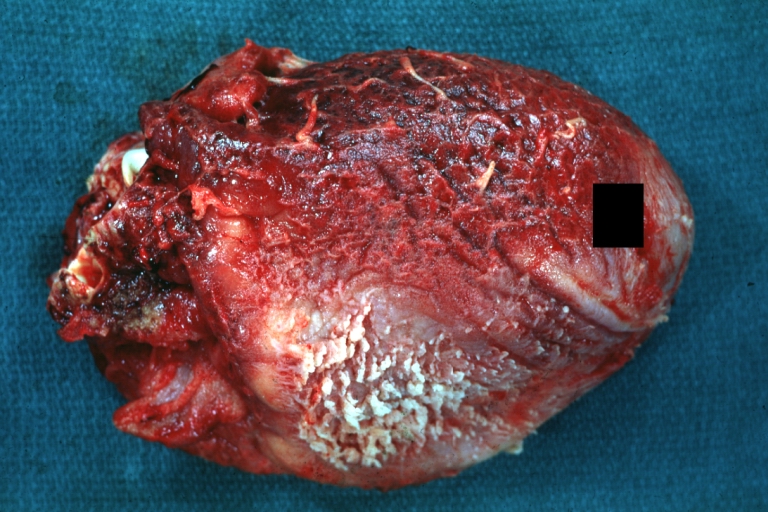
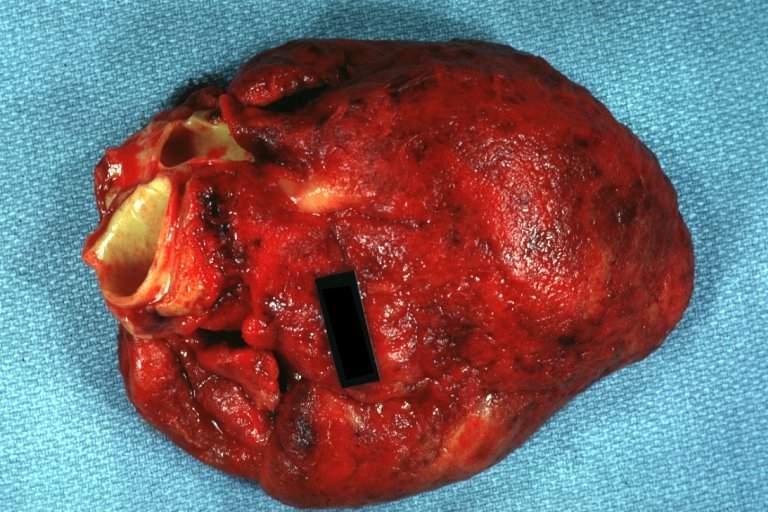
Bacterial pericarditis
Purulent pericarditis in adults is rare (please refer to table 7 of the original guideline document for information on the differential diagnosis of the specific forms of pericarditis) but always fatal if untreated. Mortality rate in treated patients is 40%, mostly due to cardiac tamponade, toxicity, and constriction. It is usually a complication of an infection originating elsewhere in the body, arising by contiguous spread or haematogenous dissemination. Predisposing conditions are preexisting pericardial effusion, immunosuppression, chronic diseases (alcohol abuse, rheumatoid arthritis, etc), cardiac surgery, and chest trauma. Rarely, left ventricular pseudoaneurysm may complicate bacterial pericarditis.
The disease appears as an acute, fulminant infectious illness with short duration. Percutaneous pericardiocentesis must be promptly performed. Obtained pericardial fluid should undergo urgent Gram, acid-fast, and fungal staining, followed by cultures of the pericardial and body fluids (level of evidence B, class I).
Rinsing of the pericardial cavity, combined with effective systemic antibiotic therapy, is mandatory (combination of antistaphylococcal antibiotic and aminoglycoside, followed by tailored antibiotic therapy according to the results of pericardial fluid and blood cultures). Intrapericardial instillation of antibiotics (e.g., gentamycin) is useful but not sufficient. Frequent irrigation of the pericardial cavity with urokinase or streptokinase using large catheters may liquefy the purulent exudate, but open surgical drainage through subxiphoid pericardiotomy is preferable. Pericardiectomy is required in patients with dense adhesions, loculated and thick purulent effusion, recurrence of tamponade, persistent infection, and progression to constriction. Surgical mortality up to 8% was reported for pericardiectomy combined with antibiotic treatment, but the total mortality is higher.
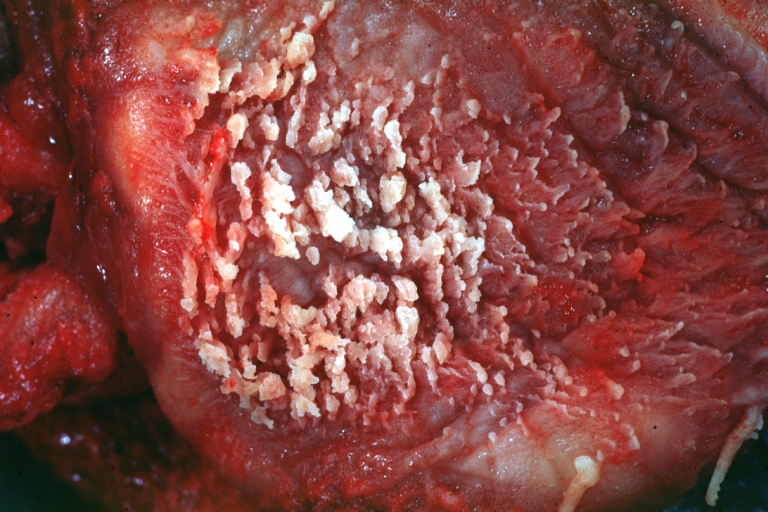
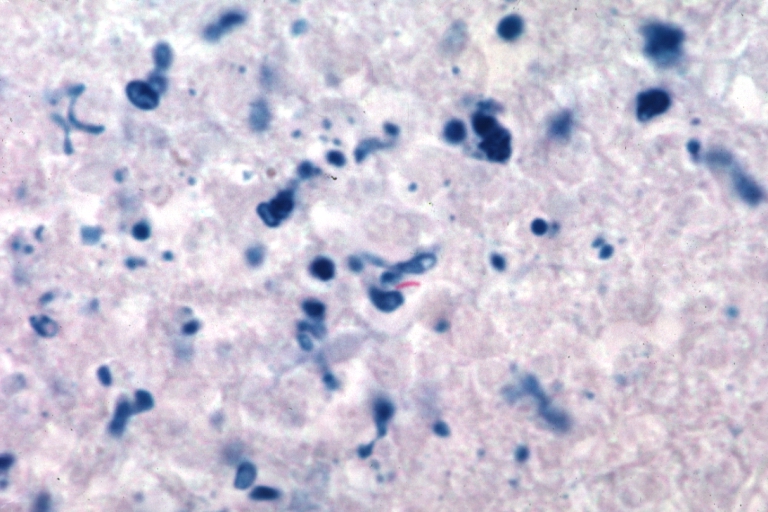
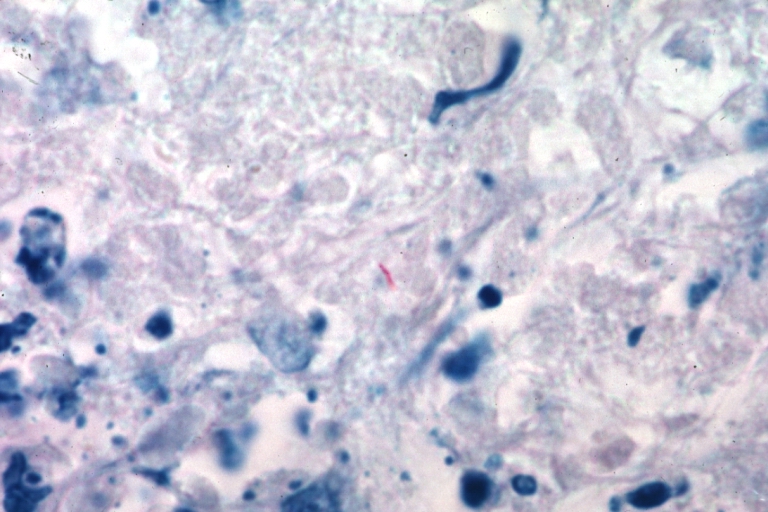
Tuberculous (TBC) pericarditis
In the last decade TBC pericarditis in the developed countries has been primarily seen in immunocompromised patients (acquired immunodeficiency syndrome [AIDS]). The mortality rate in untreated acute effusive TBC pericarditis approaches 85%. Pericardial constriction occurs in 30 to 50%. The clinical presentation is variable: acute pericarditis with or without effusion; cardiac tamponade; silent, often large, pericardial effusion with a relapsing course; toxic symptoms with persistent fever; acute constrictive pericarditis; subacute constriction; effusive-constrictive or chronic constrictive pericarditis; and pericardial calcifications. The diagnosis is made by the identification of Mycobacterium tuberculosis in the pericardial fluid or tissue and/or the presence of caseous granulomas in the pericardium. Pericarditis in a patient with proven extracardiac tuberculosis is strongly suggestive of TBC aetiology (several sputum cultures should be taken). The tuberculin skin test may be false negative in 25 to 33% of patients and false positive in 30 to 40% (elderly patients). A more accurate enzyme-linked immunospot (ELISPOT) test was recently developed, detecting T-cells specific for Mycobacterium tuberculosis antigen. Perimyocardial TBC involvement is also associated with high titres of antimyolemmal and antimyosin antibodies in the sera. The diagnostic yield of pericardiocentesis in TBC pericarditis ranges from 30 to 76% according to the methods applied for the analyses of pericardial effusion. Pericardial fluid demonstrates high specific gravity, high protein levels, and high white-cell count (from 0.7 to 54 x 109/L). Importantly, PCR can identify DNA of Mycobacterium tuberculosis rapidly from only 1 microliter of pericardial fluid. High adenosine deaminase activity and interferon gamma concentration in pericardial effusion are also diagnostic, with a high sensitivity and specificity (please refer to Focus box 4 of the original guideline document for information on pericardioscopy and epicardial/pericardial biopsy): Both pericardioscopy and pericardial biopsy have also improved the diagnostic accuracy for TBC pericarditis. Pericardial biopsy enables rapid diagnosis with better sensitivity than pericardiocentesis (100 vs. 33%).
Various antituberculous drug combinations of different lengths (6, 9, 12 months) have been applied. However, only patients with proven or very likely TBC pericarditis should be treated. Prevention of constriction in chronic pericardial effusion of undetermined aetiology by "ex iuvantibus" antitubercular treatment was not successful. The use of steroids remains controversial. A meta- analysis of patients with effusive and constrictive TBC pericarditis suggested that tuberculostatic treatment combined with steroids might be associated with fewer deaths, less frequent need for pericardiocentesis or pericardiectomy (level of evidence A, class IIa). If given, prednisone should be administered in relatively high doses (1 to 2 mg/kg per day) since rifampicin induces its liver metabolism. This dose is maintained for 5 to 7 days and is progressively reduced to discontinuation in 6 to 8 weeks. If, in spite of combination therapy, constriction develops pericardiectomy is indicated (level of evidence B, class I).
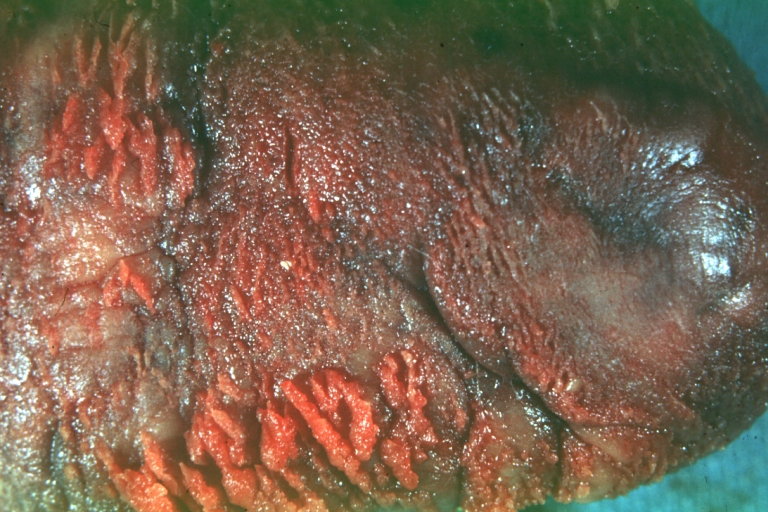
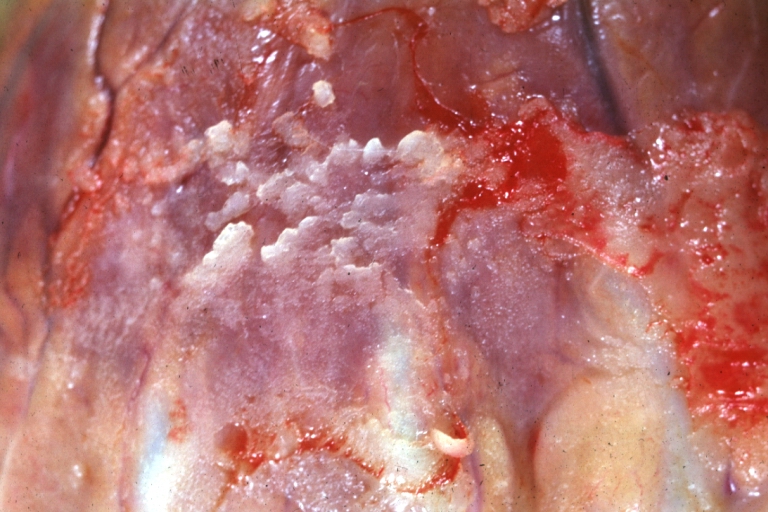
Pericarditis in renal failure
Renal failure is a common cause of pericardial disease, producing large pericardial effusions in up to 20% of patients. Two forms have been described: (1) Uremic pericarditis – in 6 to 10% of patients with advanced renal failure (acute or chronic) before dialysis has been instituted or shortly thereafter. It results from inflammation of the visceral and parietal pericardium and correlates with the degree of azotemia (the blood urea nitrogen [BUN] is usually >60 mg/dL). (2) Dialysis-associated pericarditis – in up to 13% of patients on maintenance haemodialysis, and occasionally with chronic peritoneal dialysis due to inadequate dialysis and/or fluid overload. Pathologic examination of the pericardium shows adhesions between the thickened pericardial membranes ("bread and butter" appearance). The clinical features may include fever and pleuritic chest pain, but many patients are asymptomatic. Pericardial rubs may persist even in large effusions or may be transient. Due to autonomic impairment in uremic patients, heart rate may remain slow (60 to 80 beats/min) during tamponade, despite fever and hypotension. Anaemia, due to induced resistance to erythropoetin may worsen the clinical picture. The ECG does not show the typical diffuse ST/T wave elevations observed with other causes of acute pericarditis due to the lack of the myocardial inflammation. If the ECG is typical of acute pericarditis, intercurrent infection must be suspected.
Most patients with uremic pericarditis respond rapidly to haemo- or peritoneal dialysis with resolution of chest pain and pericardial effusion. To avoid haemopericardium, heparin-free haemodialysis should be used. Care should be taken since acute fluid removal with haemodialysis can lead to cardiovascular collapse in patients with tamponade or pre-tamponade. Hypokalemia and hypophosphatemia should be prevented by supplementing the dialysis solution when appropriate. Intensified dialysis usually leads to resolution of the pericarditis within 1 to 2 weeks. Peritoneal dialysis, which does not require heparinisation, may be therapeutic in pericarditis resistant to haemodialysis, or if heparin-free haemodialysis cannot be performed. NSAIDs and systemic corticosteroids have limited success when intensive dialysis is ineffective. Cardiac tamponade and large chronic effusions resistant to dialysis must be treated with pericardiocentesis (level of evidence B, class IIa). Large, non-resolving symptomatic effusions should be treated with instillation of intrapericardial corticosteroids after pericardiocentesis or subxiphoid pericardiotomy (triamcinolone hexacetonide 50 mg every 6 h for 2 to 3 days). Pericardiectomy is indicated only in refractory, severely symptomatic patients due to its potential morbidity and mortality. Within two months after renal transplantation pericarditis has been reported in 2.4% of patients. Uraemia or infection (CMV) may be the causes.
Autoreactive pericarditis and pericardial involvement in systemic autoimmune diseases
The diagnosis of autoreactive pericarditis is established using the following criteria:
(1) increased number of lymphocytes and mononuclear cells >5,000/mm3 (autoreactive lymphocytic), or the presence of antibodies against heart muscle tissue (antisarcolemmal) in the pericardial fluid (autoreactive antibody-mediated);
(2) signs of myocarditis on epicardial/endomyocardial biopsies by >14 cells/mm2;
(3) exclusion of active viral infection both in pericardial effusion and endomyocardial/epimyocardial biopsies (no virus isolation, no IgM-titer against cardiotropic viruses in pericardial effusion, and negative PCR for major cardiotropic viruses);
(4) tuberculosis, Borrelia burgdorferi, Chlamydia pneumoniae, and other bacterial infection excluded by PCR and/or cultures;
(5) neoplastic infiltration absent in pericardial effusion and biopsy samples;
(6) exclusion of systemic, metabolic disorders, and uraemia. Intrapericardial treatment with triamcinolone is highly efficient with low incidence of side effects.
Pericarditis, with or without effusion, is also a component of a multiserositis in systemic autoimmune diseases: rheumatoid arthritis, systemic lupus erythematosus (SLE), progressive systemic sclerosis, polymyositis/ dermatomyositis, mixed connective tissue disease, seronegative spondyloarthropathies, systemic and hypersensitivity vasculitides, Behcet syndrome, Wegener granulomatosis, and sarcoidosis. Intensified treatment of the underlying disease and symptomatic management are indicated (level of evidence B, class I). Treatment should focus on pericardial symptoms, management of the pericardial effusion, and the underlying systemic disease.
The post-cardiac injury syndrome: postpericardiotomy syndrome
Post-cardiac injury syndrome develops within days to months after cardiac, pericardial injury or both. It resembles the post-myocardial infarction syndrome, both appearing to be variants of a common immunopathic process. Unlike post-myocardial infarction syndrome, post-cardiac injury syndrome acutely provokes a greater antiheart antibody response (antisarcolemmal and antifibrillary), probably related to more extensive release of antigenic material. Pericardial effusion also occurs after orthotopic heart transplantation (21%). It is more frequent in patients receiving aminocaproic acid during the operation. Cardiac tamponade after open heart surgery is more common following valve surgery (73%) than coronary artery bypass grafting (CABG) alone (24%) and may be related to the preoperative use of anticoagulants. Constrictive pericarditis may also occur after cardiac surgery. Warfarin administration in patients with early postoperative pericardial effusion imposes the greatest risk, particularly in those who did not undergo pericardiocentesis and drainage of the effusion. Symptomatic treatment is as in acute pericarditis (NSAIDs or colchicine for several weeks or months, even after disappearance of effusion). Long-term (3 to 6 months) oral corticoids or preferably pericardiocentesis and intrapericardial instillation of triamcinolone (300 mg/m2) are therapeutic options in refractory forms. Redo surgery and pericardiectomy are very rarely needed. Primary prevention of postpericardiotomy syndrome using short-term perioperative steroid treatment or colchicine is under investigation.
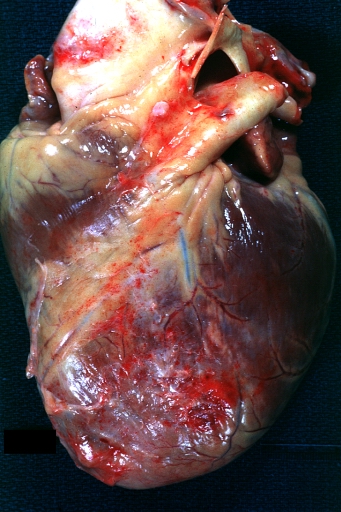
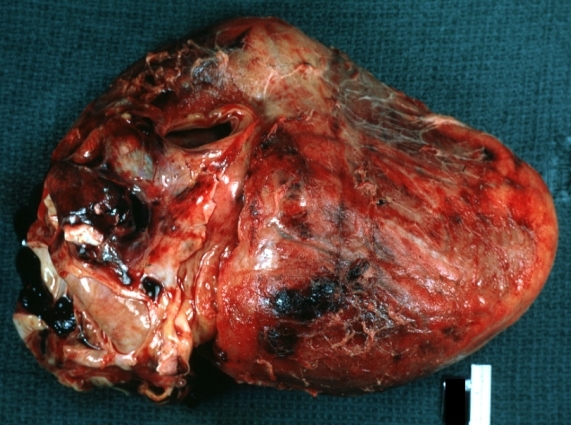
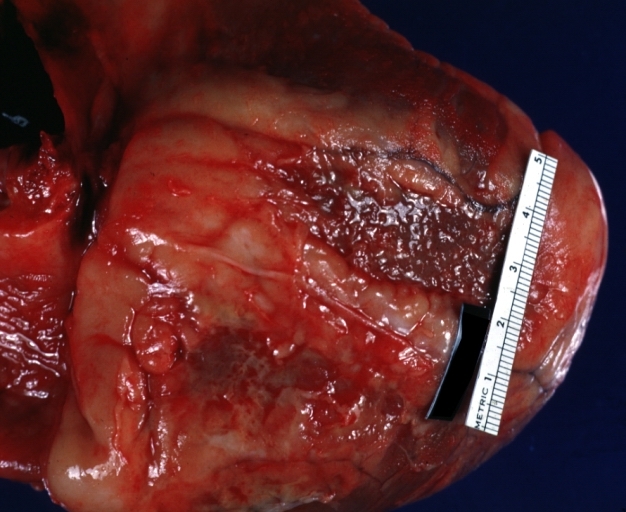
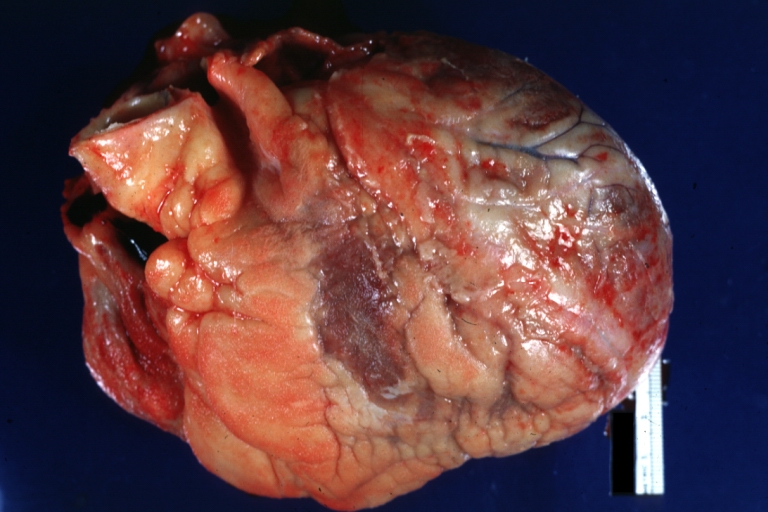
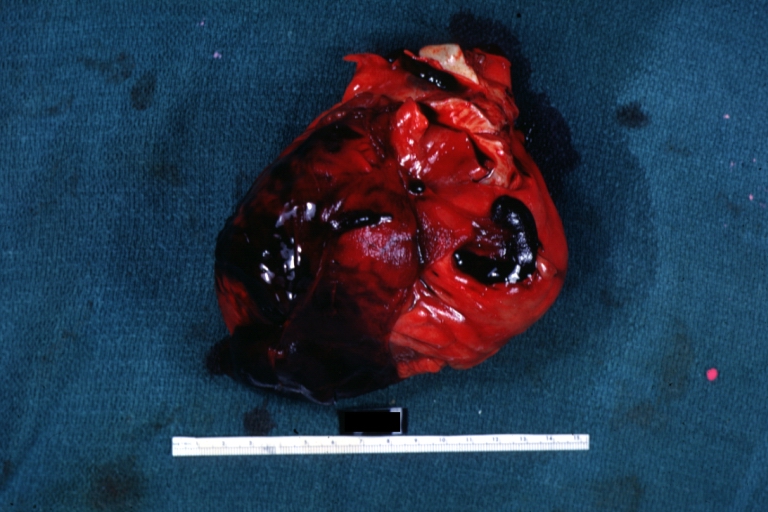
Postinfarction pericarditis
Two forms of postinfarction pericarditis can be distinguished: an "early" form (pericarditis epistenocardica) and a "delayed" form (Dressler's syndrome). Epistenocardiac pericarditis, caused by direct exudation, occurs in 5 to 20% of transmural myocardial infarctions but is clinically discovered rarely. Dressler's syndrome occurs from one week to several months after clinical onset of myocardial infarction, with symptoms and manifestations similar to the post-cardiac injury syndrome. It does not require transmural infarction and can also appear as an extension of epistenocardiac pericarditis. Its incidence is 0.5 to 5% and is still lower in patients treated with thrombolytics (<0.5%), but was more frequent in cases of pericardial bleeding after antithrombotic treatment. Of note, ECG changes are often overshadowed by myocardial infarction changes. Stage I ECG changes are uncommon and suggest "early" post-myocardial infarction syndrome whereas failure to evolve or "resurrection" of previously inverted T waves strongly suggest myocardial infarction pericarditis. Postinfarction pericardial effusion >10 mm is most frequently associated with haemopericardium, and two thirds of these patients may develop tamponade/free wall rupture. Urgent surgical treatment is life saving. However, if the immediate surgery is not available or contraindicated pericardiocentesis and intrapericardial fibrin-glue instillation could be an alternative in subacute tamponade.
Hospitalisation to observe for tamponade, differential diagnosis, and adjustments of treatment is needed. Ibuprofen, which increases coronary flow, is the agent of choice. Aspirin, up to 650 mg every 4 h for 2 to 5 days has also been successfully applied. Other nonsteroidal agents risk thinning the infarction zone. Corticosteroid therapy can be used for refractory symptoms only but could delay myocardial infarction healing (level of evidence B, class IIa).
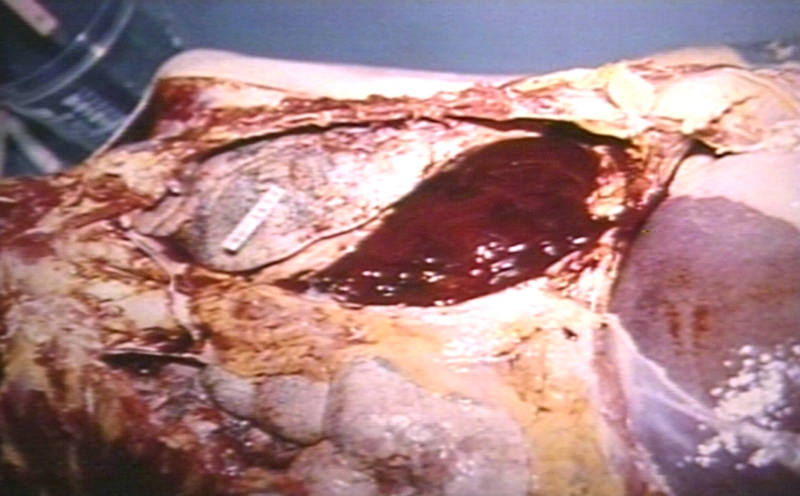
Traumatic pericardial effusion and haemopericardium in aortic dissection
Direct pericardial injury can be induced by accidents or iatrogenic wounds. Blood loss, vasoconstriction, and haematothorax leading to severe hypotension and shock may mask pulses paradoxus. Thoracotomy and surgical repair should be performed to stabilize the haemodynamics.
Iatrogenic tamponade occurs most frequently in percutaneous mitral valvuloplasty, during or after transseptal puncture, particularly if no biplane catheterisation laboratory is available and a small left atrium is present. Whereas the puncture of the interatrial septum is asymptomatic, the passage of the free wall induces chest-pain immediately. If high-pressure containing structures are punctured, rapid deterioration occurs. However, if only the atrial wall is passed, the onset of symptoms and the tamponade may be delayed for 4 to 6 h. Rescue pericardiocentesis is successful in 95 to 100% with a mortality of less than 1% (please refer to table 8 of the original guideline document for information on traumatic pericardial effusion).
Dissection of the coronary artery and acute or subacute cardiac tamponade may occur during percutaneous coronary interventions. A breakthrough in the treatment of coronary perforation is membrane-covered graft stents. Perforation of the coronary artery by a guidewire is not infrequent and causes very rarely a relevant pericardial haemorrhage.
During right ventricular endomyocardial biopsy due to the low stiffness of the myocardium, the catheter may pass the myocardium, particularly, when the bioptome has not been opened before reaching the endocardial border. The rate of perforation is reported to be in the range of 0.3 to 5%, leading to tamponade and circulatory collapse in less than half of the cases. The incidence of pericardial haemorrhage in left ventricular endomyocardial biopsy is lower (0.1 to 3.3%). Frank cardiac perforations seem to be accompanied by sudden bradycardia and hypotension. Severe complications, leading to procedure related mortality were reported in only 0.05% in a worldwide survey of more than 6,000 cases and in none of the 2,537 patients from the registry of an experienced reference centre.
Pacemaker leads penetrating the right ventricle or epicardial fixed electrodes may cause pericarditis with tamponade, adhesions, or constriction. A right bundle brand block instead of a usually induced left bundle branch block can be a first clue.
Blunt chest trauma is the major risk of car accidents. The deceleration force can lead to myocardial contusion with intrapericardial haemorrhage, cardiac rupture, pericardial rupture, or herniation. Transesophageal echocardiography in the emergency room or immediate CT should be performed. Indirect injury of the pericardium is more difficult to detect. Pericardial laceration and partial extrusion of the heart into the mediastinum and pleural space may also occur after injury.
In dissection of the ascending aorta, pericardial effusion can be found in 17 to 45% of the patients and in 48% of the autopsy cases (Please refer to table 8 of the original guideline document for information on traumatic pericardial effusion). In a clinical series of aortic dissection, pericardial tamponade was found by CT, MRI, or echocardiography in 17 to 33% of patients with type I dissection and 18 to 45% in type II dissection and 6% in type III dissection. Pericardiocentesis is contraindicated, due to the risk of intensified bleeding and extension of the dissection. Surgery should be performed immediately after the diagnosis is established by echocardiography and/or CT/MRI, even if no coronary angiography or aortography is available (level of evidence B, class I).
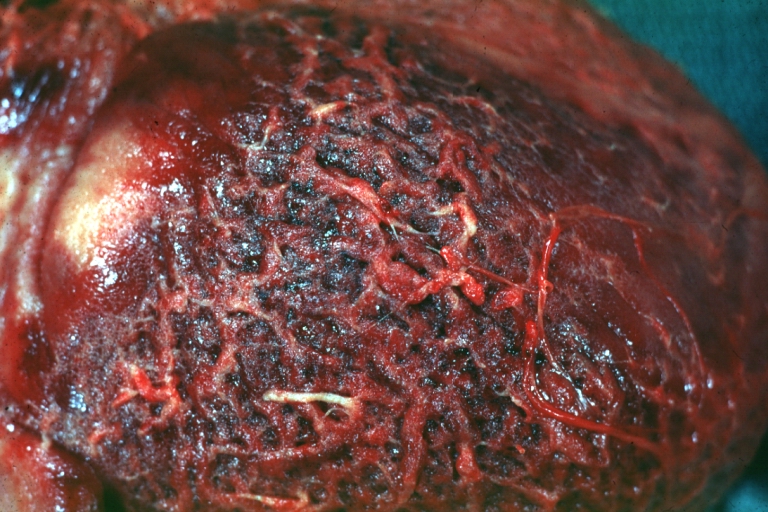
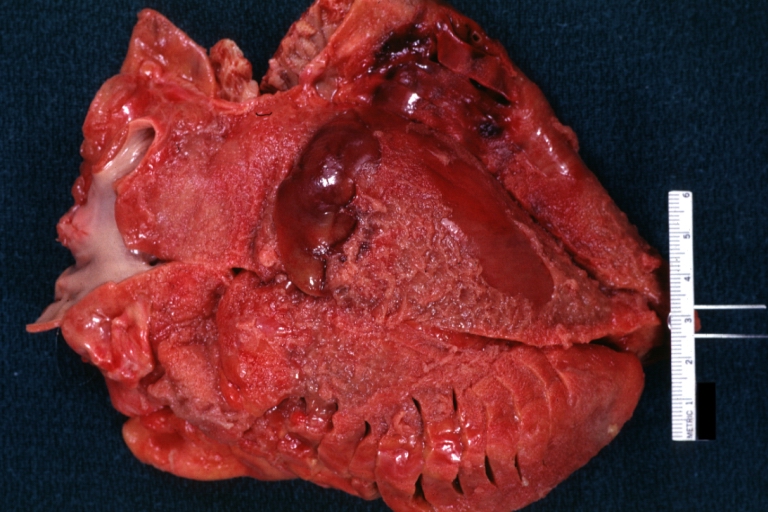
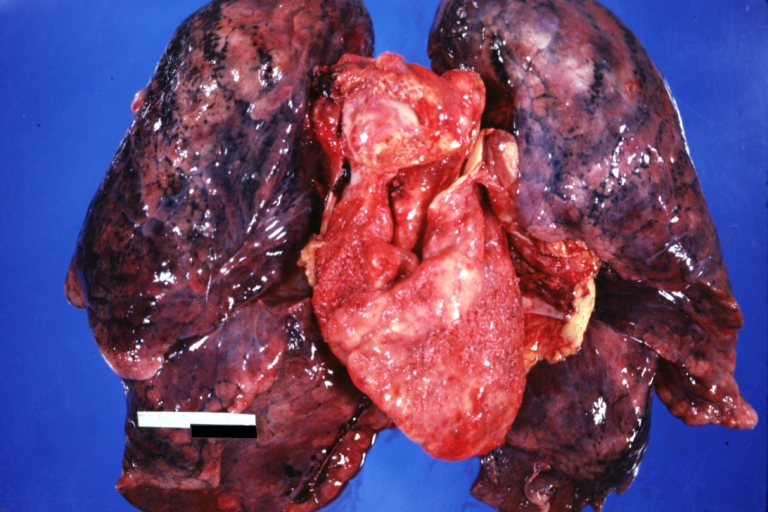
Neoplastic pericarditis
Primary tumours of the pericardium are 40 times less common than the metastatic ones. Mesothelioma, the most common of the primary tumours, is almost always incurable. Metastatic tumours of the pericardium are found in 15 to 30% of all autopsies performed in patients with malignant disease and in 4% in general autopsies. The most common secondary malignant tumours are lung cancer, breast cancer, malignant melanoma, lymphomas, and leukemias. Effusions may be small or large with an imminent tamponade (frequent recurrences) or constriction. It even may be the initial sign of malignant disease. The majority of patients with malignant pericardial effusion are asymptomatic, particularly if the accumulation of pericardial effusion is gradual. The onset of dyspnoea, cough, chest pain, tachycardia, and jugular venous distension is observed when the volume of fluid exceeds 500 mL. Orthopnea, weakness, dysphagia, syncope, palpitations, pericardial friction rub, hiccups, distant heart sounds, pleural effusion, hepatomegaly, oliguria, and oedema can also be present. Pulsus paradoxus, hypotension, cardiogenic shock, and paradoxical movement of the jugular venous pulse are important signs of cardiac tamponade.
The diagnosis is based on the confirmation of the malignant infiltration within pericardial sac. Of note, in almost two thirds of the patients with documented malignancy, pericardial effusion is caused by non-malignant diseases (e.g., radiation pericarditis) or opportunistic infections. The chest roentgenogram, CT, and MRI may reveal mediastinal widening, hilar masses, and pleural effusion. The analyses of pericardial fluid and pericardial or epicardial biopsy are essential for the confirmation of malignant pericardial disease (level of evidence B, class I) (
Treatment of cardiac tamponade is a class I indication for pericardiocentesis. The following steps are recommended in suspected neoplastic pericardial effusion without tamponade:
- Systemic antineoplastic treatment as baseline therapy which can prevent recurrences in up to 67% of cases (level of evidence B, class I);
- Pericardiocentesis to relieve symptoms and establish diagnosis (level of evidence B, class IIa);
- Intrapericardial instillation of cytostatic / sclerosing agent (level of evidence B, class IIa).
Pericardial drainage is recommended, when technically possible, in all patients with large effusions because of the high recurrence rate (40 to 70%) (level of evidence B, class I).
Prevention of recurrences, may be achieved by intrapericardial instillation of: sclerosing, cytotoxic agents, or immunomodulators. Intrapericardial treatment tailored to the type of the tumour indicate that administration of cisplatin is most effective in secondary lung cancer and intrapericardial instillation of thiotepa was more effective in breast cancer pericardial metastases. No patient showed signs of constrictive pericarditis (for both agents, level of evidence B, class IIa).
Tetracycline as sclerosing agents also control the malignant pericardial effusion in around 85% of cases, but side effects and complications are quite frequent: fever (19%), chest pain (20%), and atrial arrhythmias (10%) (level of evidence B, class IIb). Although classic sclerotherapy after intrapericardial instillation of tetracycline, doxycycline, minocycline and bleomycin is an effective procedure, constrictive pericarditis secondary to fibrosis remains a severe problem in long-term survivors. Although intrapericardial administration of radionuclides has yielded very good results, it is not widely accepted because of the logistic problems connected with their radioactivity (level of evidence B, class IIa).
Radiation therapy is very effective (93%) in controlling malignant pericardial effusion (level of evidence B, class IIa) in patients with radiosensitive tumours such as lymphomas and leukemias. However, radiotherapy of the heart can cause myocarditis and pericarditis by itself. Subxyphoid pericardiotomy is indicated when pericardiocentesis cannot be performed (level of evidence B, class IIb). The procedure can be carried out in local anaesthesia, but complications include myocardial laceration, pneumothorax, and mortality.
Pleuropericardiotomy allows drainage of malignant pericardial fluid into the pleural space (level of evidence C, class IIb). It is associated with a higher complications rate and offers no advantage over pericardiocentesis or subxyphoid pericardiotomy. Pericardiectomy is rarely indicated, mainly for pericardial constriction or complications of previous procedures.
Percutaneous balloon pericardiotomy creates a pleuro-pericardial direct communication, which allows fluid drainage into the pleural space (level of evidence B, class IIa). In large malignant pericardial effusions and recurrent tamponade, it seems to be effective (90 to 97%) and safe but has the potential risk of dissemination of neoplastic cells.
Rare forms of pericardial disease
Fungal pericarditis
Fungal pericarditis occurs mainly in immunocompromised patients or in the course of endemic-acquired fungal infections. The clinical picture comprises the full spectrum of pericardial diseases, including fungal myocarditis. Fungal pericarditis is mainly due to endemic fungi (Histoplasma, Coccidioides), or nonendemic opportunistic fungi (Candida, Aspergillus, Blastomyces) and semifungi (Nocardia, Actinomyces). Diagnosis is obtained by staining and culturing pericardial fluid or tissue. Antifungal antibodies in serum are also helpful in establishing the diagnosis of fungal infection. Antifungal treatment with fluconazole, ketoconasole, itraconasole, amphotericin B, liposomal amphotericin B, or amphotericin B lipid complex is indicated in patients with documented fungal pericarditis (level of evidence B, class I). Corticosteroids and NSAIDs can support the treatment with antifungal drugs (level of evidence C, class IIa). Patients with pericarditis in the course of histoplasmosis do not need antifungal therapy, but respond to NSAIDs given during 2 to 12 weeks. Sulfonamides are the drugs of choice for a nocardiosis infection. Combination of three antibiotics including penicillin should be given for actinomycosis (level of evidence C, class I). Pericardiocentesis or surgical treatment is indicated for haemodynamic impairment. Pericardiectomy is indicated in fungal constrictive pericarditis (level of evidence C, class I).
Radiation pericarditis
The probability to develop radiation-induced pericarditis is influenced by the applied source, dose, its fractionation, duration, radiation exposed volume, form of mantel field therapy, and the age of the patients. Radiation-induced pericarditis may occur already during the therapy or months and years later – with latency of up to 15 to 20 years. The effusion may be serous or haemorrhagic, later on with fibrinous adhesions or constriction, typically without tissue calcification. The symptoms may be masked by the underlying disease or the applied chemotherapy. Imaging should start with echocardiography, followed by cardiac CT or MRI if necessary. Pericarditis without tamponade may be treated conservatively or by pericardiocentesis for diagnostic purposes or if haemodynamic compromise/tamponade occurs. Pericardial constriction may happen in up to 20% of patients, requiring pericardiectomy. The operative mortality is high (21%) and the postoperative five years survival rate is very low (1%) mostly due to myocardial fibrosis.
Chylopericardium
Chylopericardium refers to a communication between the pericardial sac and the thoracic duct, as a result of trauma, congenital anomalies, or as a complication of open-heart surgery, mediastinal lymphangiomas, lymphangiomatous hamartomas, lymphangiectasis, and obstruction or anomalies of the thoracic duct. Infection, tamponade, or constriction may aggravate the prognosis. The pericardial fluid is sterile, odourless, and opalescent with a milky white appearance and the microscopic finding of fat droplets. The chylous nature of the fluid is confirmed by its alkaline reaction, specific gravity between 1010 and 1021, Sudan III stain for fat, the high concentrations of triglycerides (5 to 50 g/L) and protein (22 to 60 g/L). Enhanced CT, alone or combined with lymphography, can identify not only the location of the thoracic duct but also its lymphatic connection to the pericardium. Treatment depends on the aetiology and the amount of chylous accumulation. Chylopericardium after thoracic or cardiac operation without signs of tamponade is preferably treated by pericardiocentesis and diet (medium chain triglycerides). If further production of chylous effusion continues, surgical treatment is mandatory (level of evidence B, class I). When conservative treatment and pericardiocentesis fail, pericardio-peritoneal shunting by a pericardial window is a reasonable option. Alternatively, when the course of the thoracic duct was precisely identified, its ligation and resection just above the diaphragm is the most effective treatment. In secondary chylopericardium the underlying disease (e.g., mediastinal tumour) should be treated.
Pericardial reactions to drugs are rare. However, several medications and toxic substances can induce pericarditis, tamponade, adhesions, fibrosis, or constriction (Please refer to table 9 of the original guideline document for information on drug- and toxin-related pericardial diseases). Mechanisms include drug induced lupus reactions, idiosyncrasy, "serum sickness," foreign substance reactions, and immunopathy. Management is based on discontinuation of the causative agent and symptomatic treatment.
Pericardial effusion in thyroid disorders
Pericardial effusion occurs in 5 to 30% of patients with hypothyroidism. Fluid accumulates slowly and tamponade occurs rarely. In some cases cholesterol pericarditis may be observed. The diagnosis of hypothyroidism is based on serum levels of thyroxin and thyroid stimulating hormone. Bradycardia, low-voltage of the QRS and T-wave inversion or flattening in the ECG, cardiomegaly in the roentgenogram, and pericardial effusion in echocardiography, as well as a history of radiation-induced thyroid dysfunction, myopathy, ascites, pleural effusion, and uveal oedema may be observed. Therapy with thyroid hormone decreases pericardial effusion (level of evidence B, class I).
Pericardial effusion in pregnancy
There is no evidence that pregnancy affects susceptibility to pericardial disease. However, many pregnant women develop a minimal to moderate clinically silent hydropericardium by the third trimester. Cardiac compression is rare. ECG changes of acute pericarditis in pregnancy should be distinguished from the slight ST-segment depressions and T-wave changes seen in normal pregnancy (please refer to Table 10 of the original guideline document for information on the diagnostic approach to pericardial effusion in pregnancy). Occult constriction becomes manifest in pregnancy due to the increased blood volume. Most pericardial disorders are managed as in nonpregnant. Caution is necessary while high-dose aspirin may prematurely close the ductus arteriosus, and colchicine is contraindicated in pregnancy. Pericardiotomy and pericardiectomy can be safely performed if necessary and do not impose a risk for subsequent pregnancies. Foetal pericardial fluid can be detected by echocardiography after 20 weeks’ gestation and is normally 2 mm or less in depth. More fluid should raise questions of hydrops foetalis, Rh disease, hypoalbuminemia, and immunopathy or maternally transmitted mycoplasmal or other infections, and neoplasia.
Diagnosis
History and Symptoms
A diagnosis of pericarditis can be made depending on its etiology and speed of onset. For example, both uremic and tuberculosis induced pericarditis develop more slowly and can be undetectable until presenting "as a fever of unknown origin." On the other hand, both bacterial and viral pericarditis develop rapidly and can present as increasing "pain over several hours."
Symptoms:
- Chest Pain: however, pain is often absent (depending on the type of pericarditis e.g. rheumatoid pericarditis). It is the most common symptom.
- Some causes of pain include: inflammation of the pericardium, phrenic nerves, and nearby pleura.
- Quality of pain: sharp, "sticking", dull, aching, or pressure-like. It can be rated anywhere from 1-10. In the beginning stages, the pain usually starts out as sharp. "Inspiration and cough" can increase the pain so patients usually "sit upright for relief."
- Nonproductive cough that elicites pleuritic pain
- Productive cough, which usually occurs in the presence of other illness(es)
- Hiccup (rarely)
- Odynophagia with or without Dysphagia
- Faintness and Dizziness (uncommon unless cardiac tamponade is present]]
- Chest wall palpitations: causing local tenderness and may be indicative of costochondritis, Tietze syndrome, or rib fractures (in cases of traumatic pericarditis)
Physical Examination
Appearance of the Patient with Pericarditis
- Fever less than 39° C or 102.2° F
- Patients who are elderly may not exhibit fever; however, they may be hypothermic especially those with renal failure.
- Chills (suppurative pericarditis and idiopathic (viral) pericarditis)
- Weakness
- Depression
- Anxiety
- Pallor (may also indicate tuberculosis, uremia, neoplasia, and rheumatic carditis)
Heart
Ausculatory Phenomena:
- Pericardial Rub(s): Usually heard with acute pericarditis, sometimes with subacute and chronic. This is the major indicator of pericarditis.
- endopericardial rub: inflamed, scarred or tumor-invaded serosal surfaces
- exopericardial rub: after sclerotherapy of effusions, between parietal pericardium and pleura or chest wall (occasionally)
- endo-exopericardial rub: both of the above
- pleuropericardial rub: pleuritis as a result of pleural or both pleural and pericardial both
- Abnormal Heart Sounds:
- Sounds are dampened as a result of fluid insullation
- Hemodynamic changes diminish S1 and S2
- Clicks: Ventricular volume shrinks disproportionately and psuedoprolapse/true prolapse of mitral and/or tricuspid valvular structures result in clicks.
- Murmurs: are epiphenomena and may be present if there is coinciding heart disease, narrowing of a valve, aorta, pulmonary artery or another area of the heart.
Lungs
Rales are frequent examination findings, occasionally pleural fluid may present.
Extremities
- May be poorly perfused in the setting of tamponade
- Edema may be present in the setting of pericardial constriction
Laboratory Findings
Electrolyte and Biomarker Studies
Inflammatory markers. A CBC may show an elevated white count and a serum C-reactive protein may be elevated.
Molecular markers. Acute pericarditis is associated with a modest increase in serum creatine kinase MB (CK-MB)[2][3] and cardiac troponin I (cTnI)[4][5], both of which are also markers for myocardial injury. Therefore, it is imperative to also rule out acute myocardial infarction in the face of these biomarkers. The elevation of these substances is related to inflammation of the myocardium. Also, ST elevation on EKG (see below) is more common in those patients with a cTnI > 1.5 µg/L[5]. Coronary angiography in those patients should indicated normal vascular perfusion. The elevation of these biomarkers are typically transient and should return to normal within a week. Persistence may indicated myopericarditis. As a summary:
- ESR: mild to marked elevation
- CRP: mild to marked elevation
- CK-MB: depends on the extent of myocardial involvement
- LDH: depends on the extent of myocardial involvement
- troponin I: depends on the extent of myocardial involvement
- serum myoglobin: normal (but not always, usually rises with increased ST segment deviation
- gallium-67 scanning: helps ID "inflammatory and leukemic infiltrations"
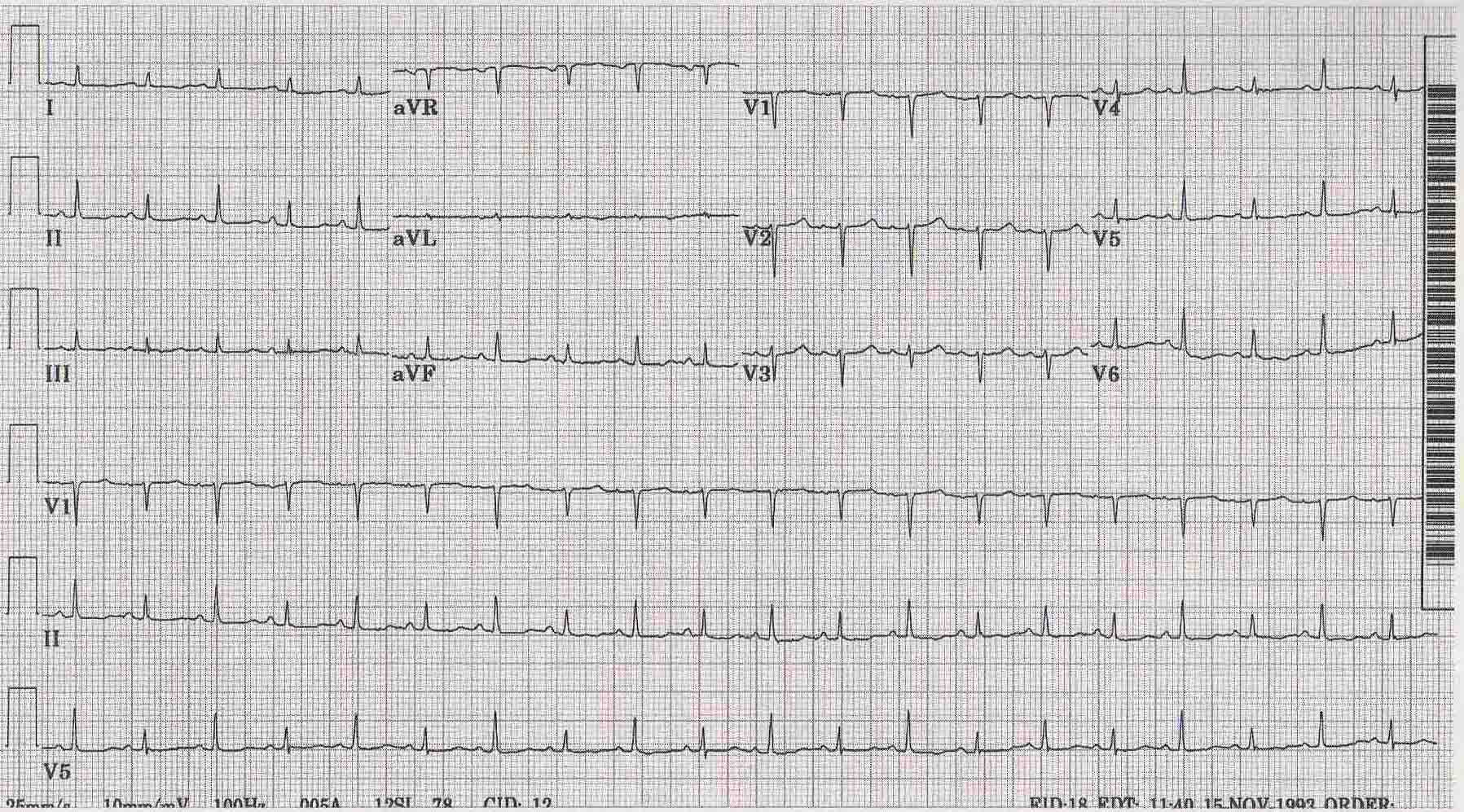
Electrocardiogram
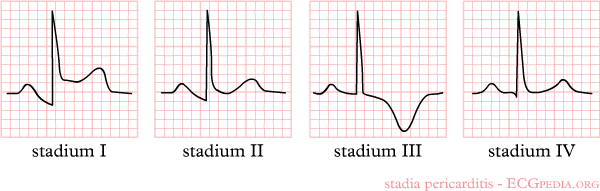
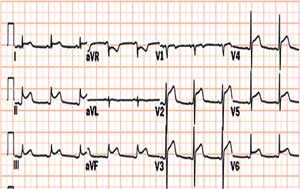
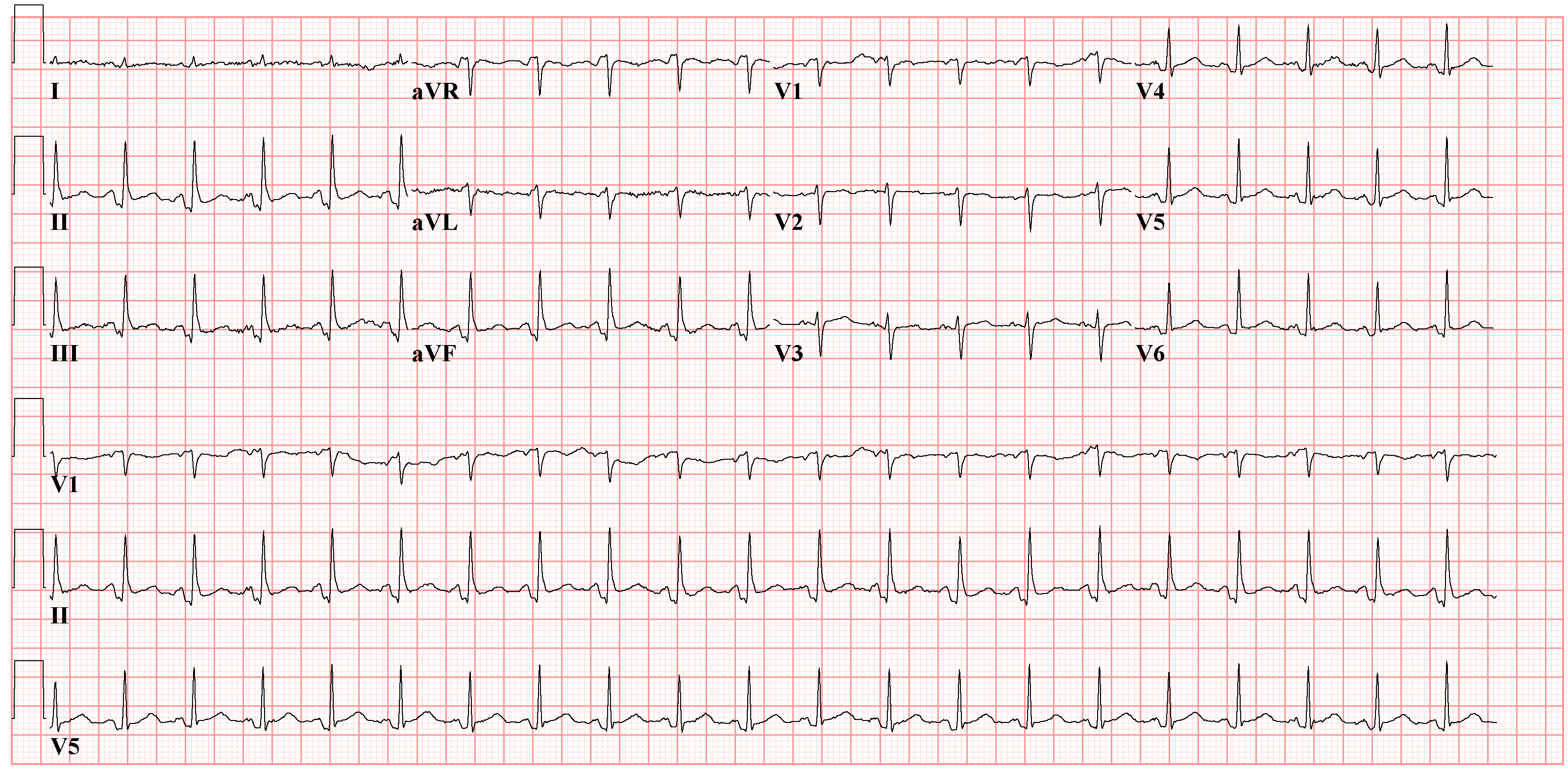
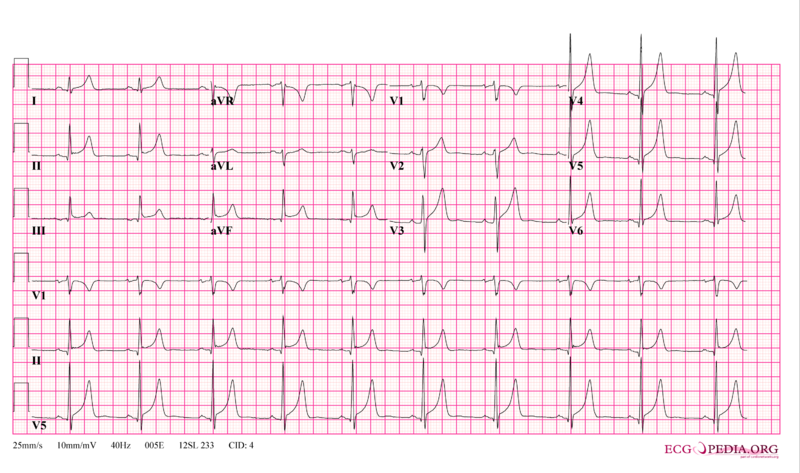
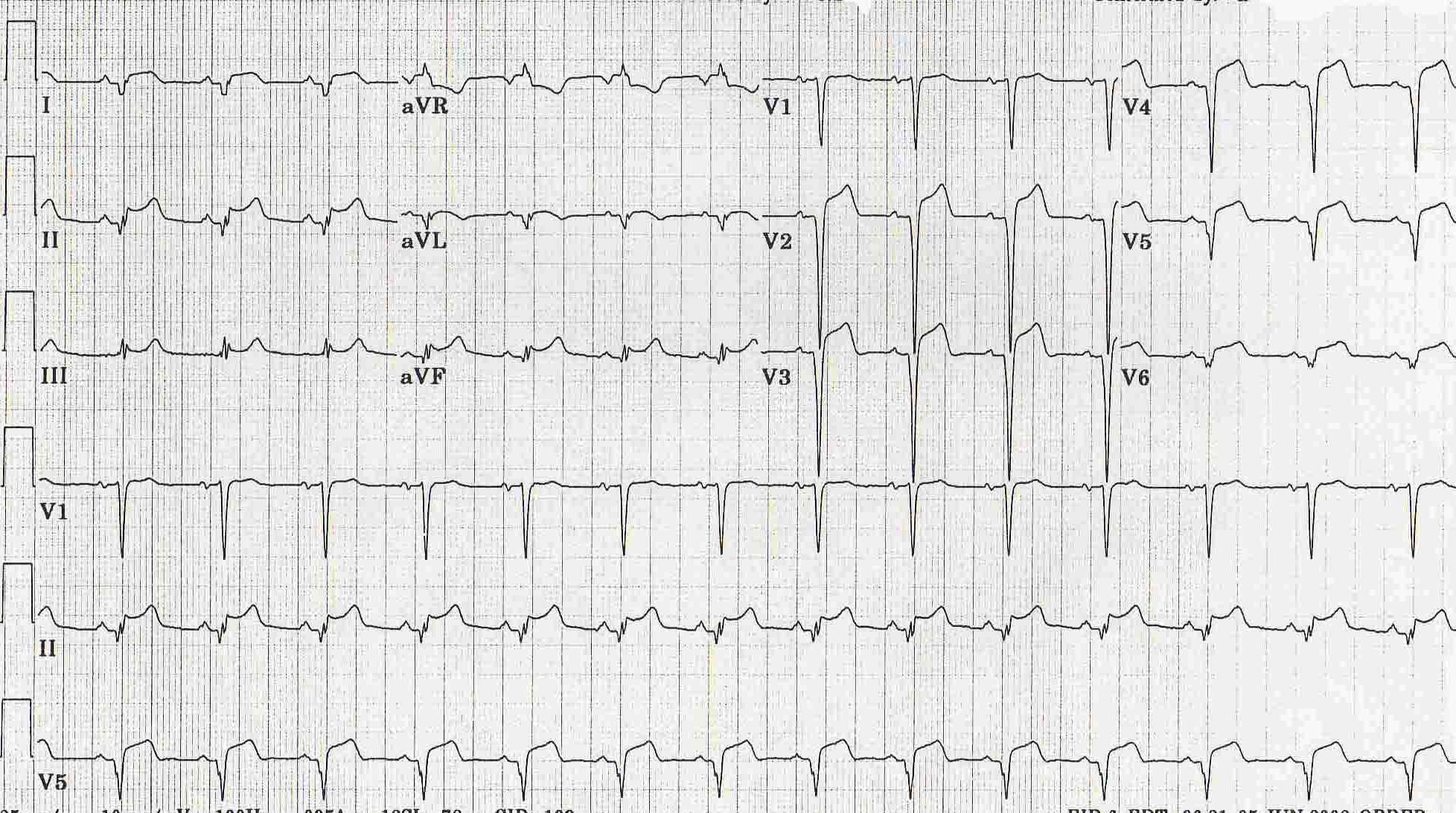
ECG Abnormalities: Increase in scar tissue, fluid and fibrin can reduce voltage, quasi-specific ST-T waves can present. The ECG abnormalities vary depending on the stage/severity of the pericarditis. Below are the stages/types of pericarditis:[6][2]
- Acute Pericarditis (see also Electrocardiography#The PR Interval and Electrocardiography#The EKG of Cardiac Transplantation): this variation of the disease in conjunction with myocarditis can lead to ST-T anomalies that are characteristic of the acute stages of pericarditis.
- Stage 1: Stage 1 of acute pericarditis, in and of itself, presents as "early repolarization" and acute infarction. It shows signs of anterior and inferior ST elevation on the ECG. There are usually no deviations in the QRS complex. This stage is largely characteristic of acute pericarditis when almost all of the leads are effected. Leads I, II, avL, avF, and V3-V6.
- Stage 2: During the early phase of this stage, ST segments should become baseline again; whereas, PR segments may have deviated. During the latter phase of stage 2, the ST segments that were previously elvated usually flatten and invert.
- Stage 3: Virtually all of the leads in stage 3 exhibit T wave inversion. Acute pericarditis cannot be diagnosed on an ECG of a stage 3 patient because its presentation is the same as myocardial injury and frank myocarditis.
- Stage 4: This stage presents itself on the ECG as a return to a prepericarditis state. Stage 4 does not always occur and in its absence, there can be residual T wave inversions that may be permanent, generalized or focal.
- Rate and Rhythm: Rapid heart rates are typical in patients with pericarditis, but in patients with uremic pericarditis slower rates are observed. Heart rhythms appear normal unless there is another complication such as cardiac disease, the presence of myocardial/pericardial tumor, or a metabolic disorder.
- Pericardial Effusion (see also Electrocardiography#Amplitude): These can present differently on the ECG depending on whether they are chronic vs large effusions. The former typically leads to low amplitude ECGs; whereas, the latter can show no voltage or various ECG abnormalities. ST-T wave abnormalities can be caused by superficial myocarditis or because of the accumulated fluid, they may be caused by the compression of the myocardium or ischemia. The primary cause of ST segment variation during pericardial effusions is usually the rapid accumulation of fluid. Large effusions can lead to the reduction of P wave voltage. Pleural effusions can cause a decrease in voltage, which occurs mainly on the left. Also, cirrhosis and congestive heart failure (CHF), which similarily involve the accumulation of fluid in the body, can decrease voltage in the absence of any pericardial disease.
- Cardiac tamponade (see also Cardiac tamponade#Electrocardiogram): Generally has little ECG effect; however, in the acute form, tamponade may present on the ECG as any one of the stages of acute pericarditis.
- Electrical Alternation: This occurs more often in cases of tamponade than in those of pericarditis (2:1). There is alternation of the QRS complex on the spatial axis. Alternation of the T wave, P wave, and PR segement are difficult to see and are uncommon. The removal of even a small amount of fluid can end alternation.
- Early Repolarization: This finding can be misleading and may look like pericarditis, when in fact it is not. A strong indication of pericarditis is "if the J point is more than 25% the height of the T wave apex."
- Constrictive Pericarditis: Cases of constrictive pericarditis have nonspecific ECG abnormalities. Common abnormalities include: a slightly "low voltage QRS" segment combined with "flattened to inverted T waves", during stage 3 of acute/subacute constriction the T wave inversions remain or worsen and "P waves can be wide and bifid." It is not uncommon for patients to have normal ECGs. Many patients may only exhibit "nonspecific T wave abnormality." Other influencial factors that may effect the ECG in constrictive pericarditis are: fluid retention, ascites, and pleural effusions. The two most common arrhythmias that occur are atrial fibrillation and atrial flutter.
- QRS Abnormality: characteristic RV hypertrophy QRS abnormalities may develop as a result of disproportionate constriction or postpericardiectomy scarring. Also, "focal atrophy, scarring or inflamation" may cause "abnormal Q waves."
- Chronic Constrictive Pericarditis: low volatage and myocardial atrophy, "frontal QRS axis" is usually vertical (becomes more vertical with increasing chronicity),
- Acute/Subacute Pericarditis: QRS axis appears as normal
- QRS Abnormality: characteristic RV hypertrophy QRS abnormalities may develop as a result of disproportionate constriction or postpericardiectomy scarring. Also, "focal atrophy, scarring or inflamation" may cause "abnormal Q waves."
Chest X Ray
The heart will be enlarged on CXR in the setting of tamponade with a significant pericardial effusion.
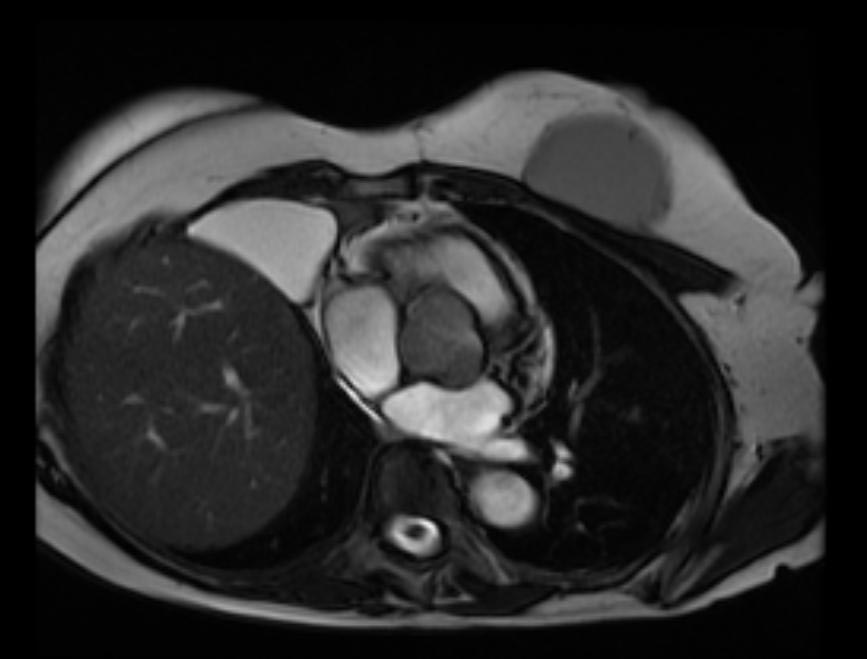
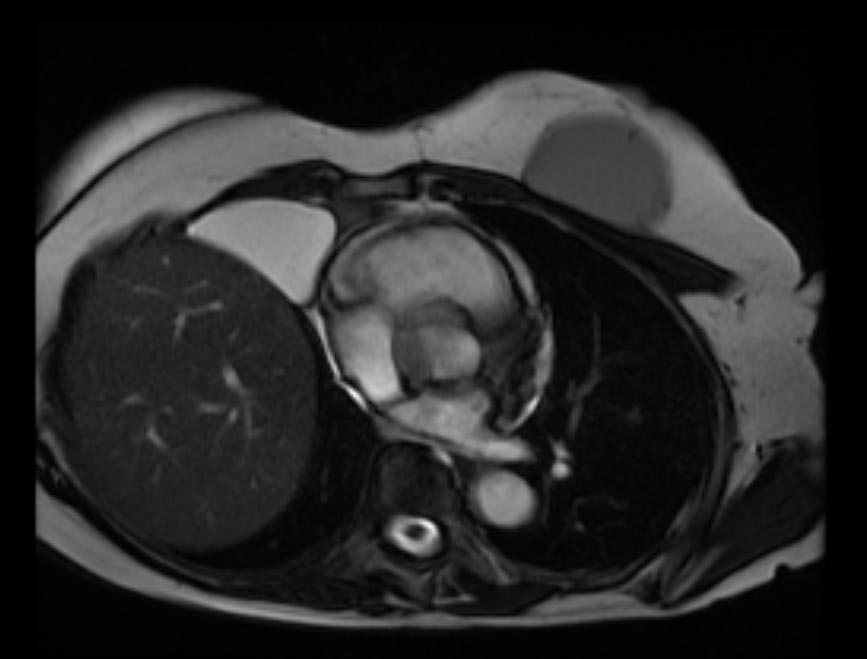
MRI and CT [7] [8] [9]
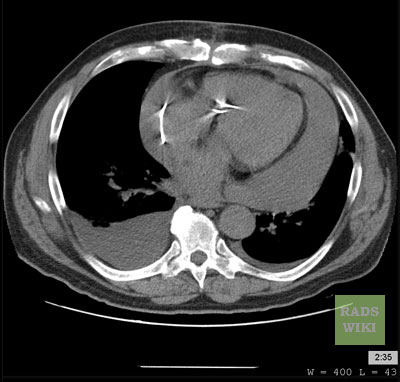
Pericardial Effusion
Cross-sectional imaging by CT or MRI is very sensitive in the detection of generalized or loculated pericardial effusions. Some fluid in the pericardial sac contributes to the apparent thickness and should be considered normal. Commonly, free-flowing fluid accumulates first at the posterolateral aspect of the left ventricle, when the patient is imaged in the supine position.
Estimation of the amount of fluid is possible to a limited extent based on the overall thickness of the crescent of fluid. Compared to cardiac ultrasound, CT and MRI may be particularly helpful in detecting loculated effusions, owing to the wide field of view provided by these techniques. Hemorrhagic effusions can be differentiated from a transudate or an exudate based on signal characteristics (high signal on T1-weighted images) or density (high-density clot on CT). Pulsation artefacts may cause local areas of low signal in a hemorrhagic effusion. Effusions are often incidentally noted on CT scans obtained for other indications.
Pericardial thickening (thickness >4 mm) is difficult to differentiate from a small generalized effusion. Both entities will reveal a low signal/density line that is thicker than the normal pericardial thickness. In acute pericarditis, the pericardial lining can show intermediate signal intensity and may enhance after gadolinium administration.
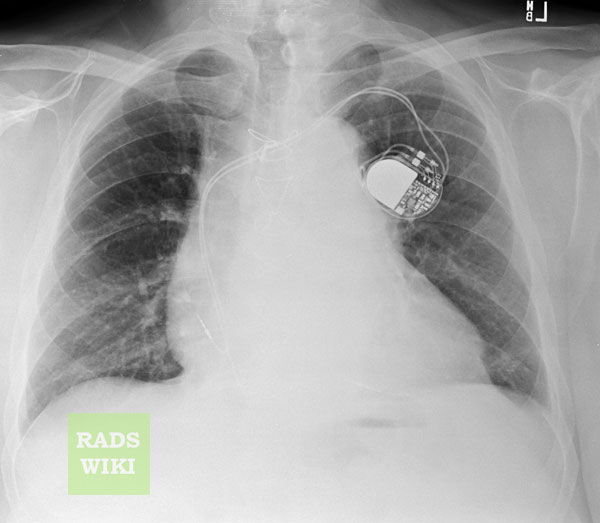
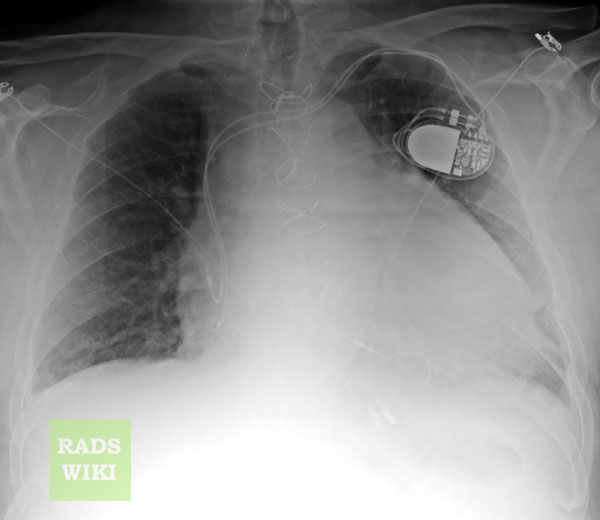
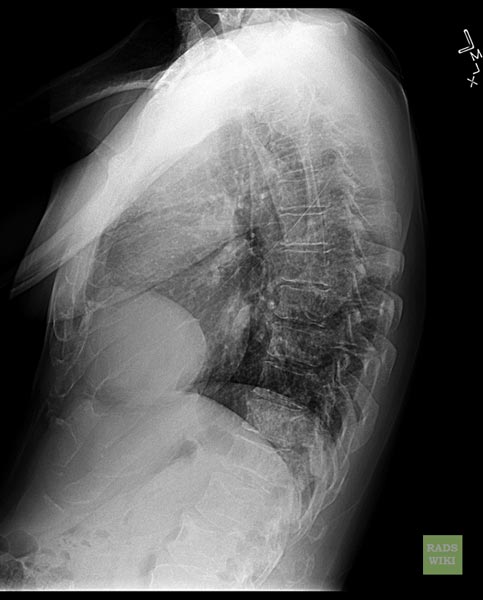
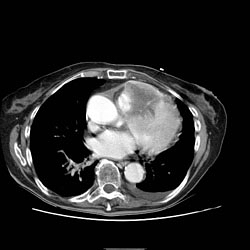
Images shown below are courtesy of RadsWiki and copylefted
-
Chest x-ray: Pericardial effusion
-
Chest x-ray: Pericardial effusion. The second day of admission
-
Cardiac MSCT: Pericardial effusion
Constrictive Pericarditis
Pericardial thickening may result in constrictive pericarditis. In this entity, pericardial thickening will hamper cardiac function, with hemodynamic consequences. Many disease conditions can lead to constrictive pericarditis (infection, tumor, radiation, heart surgery, etc.).
The diagnostic features include thickened pericardium in conjunction with signs of impaired right ventricular function: dilatation of caval veins and hepatic veins, enlargement of the right atrium, and the right ventricle itself may be normal or even reduced (tubular, sigmoid) in size due to compression. Localized pericardial thickening may also cause functional impairment (localized constrictive pericarditis). Sometimes constriction may occur despite a normal appearance of the pericardium.
Pericardial calcifications are easily visualized by CT but may be difficult or impossible to appreciate on MRI.
Pericardial Tumor
A pericardial cyst is most commonly located at the right cardiophrenic angle. On T1, it appears either as a low signal or an intermediate signal due to high protein content, or with a characteristic light-bulb appearance on T2.
Unusual tumors may arise from the pericardium (mesothelioma, angiosarcoma, etc.). Malignant primary tumors have many overlapping imaging features and generally cannot be differentiated. The role of cross-sectional imaging is to establish a diagnosis and to define the extent of the lesion (invasion of cardiac structures, veins, pericardium, etc.). Sometimes lesions may have helpful signal characteristics to suggest a specific diagnosis, e.g., high-signal fat on T1 or low-density fat on CT in lipoma / liposarcoma.
Secondary tumors are much more common than primary tumors. Lung cancer may invade the mediastinal and cardiac structures directly or indirectly.
The most common secondary tumors affecting the heart are lung cancer, breast cancer, and lymphoma. Metastatic pericardial disease commonly presents as hemorrhagic effusion. Tumor nodules may enhance after intravenous gadolinium administration.
Images shown below are courtesy of RadsWiki and copylefted
Pericardial Metastases
Echocardiographic Findings
Radioscopic Findings
- Calcified pericardium in constructive pericarditis
<youtube v=blSXL5z02fY/>
<youtube v=LXWitpJQEGQ/>
Pericardiocentesis
Pericardiocentesis is life saving in cardiac tamponade (level of evidence B, class I). Aortic dissection is a major contraindication. Relative contraindications include uncorrected coagulopathy; anticoagulant therapy; thrombocytopenia <50,000/mm3; and small, posterior, and loculated effusions. Pericardiocentesis in acute traumatic haemopericardium and purulent pericarditis is probably less appropriate than surgical drainage. In effusions causing no haemodynamic compromise, pericardiocentesis is indicated in effusions >20 mm in echocardiography in diastole or for diagnostic purposes if additional procedures are available (e.g., pericardial fluid and tissue analyses, pericardioscopy, and epicardial/pericardial biopsy) which could reveal the etiology of the disease and permit further causative therapy (level of evidence B, class IIa).
Pericardiocentesis guided by fluoroscopy is performed in the cardiac catheterisation laboratory with ECG monitoring. Direct ECG monitoring from the puncturing needle is not an adequate safeguard. Right-heart catheterization can be performed simultaneously with pericardiocentesis, allowing monitoring the improvement as the effusion is drained. The subxiphoid approach has been used most commonly, with a long needle with a mandrel (Tuohy or thin-walled 18-gauge) directed towards the left shoulder at a 30 degree angle to the skin. This route is extrapleural and avoids the coronary, pericardial, and internal mammary arteries.
The operator intermittently attempts to aspirate fluid and injects small amounts of contrast. If hemorrhagic fluid is freely aspirated, a few millilitres of contrast medium may be injected under fluoroscopic observation. The appearance of sluggish layering of contrast medium inferiorly indicates that the needle is correctly positioned. A soft J-tip guidewire is introduced and, after dilatation, exchanged for a multi-holed pigtail catheter. It is prudent to drain the fluid in steps of less than 1L at a time to avoid the acute right-ventricular dilatation ("sudden decompression syndrome"). It is essential to check the position of the guidewire in at least two angiographic projections. If the guidewire was erroneously placed intracardially, this should be recognized before insertion of the dilator and drainage catheter. If, despite the caution, the introducer set or the catheter have perforated the heart and are laying intracardially, the catheter should be secured and the patient promptly transferred to the cardiac surgery. Alternatively, a second puncture can be attempted. If successful, surgery may be avoided using autotransfusion of pericardial blood.
Echocardiographic guidance of pericardiocentesis is technically less demanding and can be performed in the intensive care unit at the bedside. Echocardiography should identify the shortest route where the pericardium can be entered intercostally (usually in the sixth or seventh rib space in the anterior axillary line). Prolonged pericardial drainage is performed until the volume of effusion obtained by intermittent pericardial aspiration (every 4 to 6 h) fall to <25 mL per day.
The feasibility is high (93%) in patients with anterior effusion >10 mm, while the rate of success is only 58% with small, posteriorly located effusions. Fluoroscopic and haemodynamic monitoring improve feasibility (93.1% vs. 73.3%) in comparison to emergency pericardial puncture with no imaging control. The tangential approach using the epicardial halo phenomenon in the lateral view significantly increased the feasibility of fluoroscopically guided pericardiocentesis in patients with small effusions (200 to 300 mL) (92.6% vs. 84.9%) and very small effusions (<200 mL) (89.3% vs. 76.7%).
Pericardiocentesis with echocardiography guidance was feasible in 96% of loculated pericardial effusions after cardiac surgery. A rescue pericardiocentesis guided by echocardiography successfully relieved tamponade after cardiac perforation in 99% of 88 patients and was the definitive therapy in 82% of the cases. The most serious complications of pericardiocentesis are laceration and perforation of the myocardium and the coronary vessels. In addition, patients can experience air embolism, pneumothorax, arrhythmias (usually vasovagal bradycardia), and puncture of the peritoneal cavity or abdominal viscera. Internal mammary artery fistulas, acute pulmonary oedema, and purulent pericarditis were rarely reported. The safety was improved with echocardiographic or fluoroscopic guidance. A large echocardiographic series reported an incidence of major complications of 1.3 to 1.6%. In a large series of fluoroscopy-guided percutaneous pericardiocenteses, cardiac perforations occurred in 0.9%, serious arrhythmias in 0.6%, arterial bleeding in 1.1%, pneumothorax in 0.6%, infection in 0.3%, and a major vagal reaction in 0.3%. Incidence of major complications was further significantly reduced by utilizing the epicardial halo phenomenon for fluoroscopic guidance.
Pathological Findings
Gross Images
-
Fibrinous pericarditis: Gross, natural color, an excellent example of bread and butter appearance. Uremia, chronic glomerulonephritis and sepsis.
-
Fibrinous pericarditis: Gross, a good example (bread and butter appearance).
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, an excellent example, close-up view of fibrin.
-
Fibrinous pericarditis: Gross, an excellent example, close-up view.
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, external view of localized pericarditis over an acute infarction
-
Fibrinous pericarditis: Gross, intact heart, good example
-
Fibrinous pericarditis: Gross, good example, mild, with small amount of fibrin
-
Fibrinous pericarditis: Gross, close-up, an excellent example of color and detail
-
Fibrinous pericarditis: Gross, a good example
-
Fibrinous pericarditis: Gross, a good example, very mild case
-
Fibrinous pericarditis: Gross, an excellent example.
-
Fibrinous pericarditis: Gross, a close-up view, an excellent illustration of fibrinous exudate.
-
Pericarditis in uremia
-
Fibrinous pericarditis: Gross, fixed tissue (note to color changes), a close-up view of fibrin on epicardial surface of heart. A typical example.
-
Fibrinous pericarditis: Gross, natural color, large right atrial thrombus and fibrinous pericarditis. Normal tricuspid valve with some aging changes (good example)
-
Fibrinous pericarditis: Gross, natural color
-
Fibrinous pericarditis: Gross, natural color, an excellent example
-
Fibrinous pericarditis: Gross, natural color, very close-up photo showing fibrinous exudate simulating frost (an excellent example)
-
Rheumatoid fibrinous pericarditis: Gross, natural color, a typical lesion in 22 years old white female due to juvenile rheumatoid arthritis.
-
Fibrinous pericarditis: Gross, natural color, close-up view of minimal fibrinous exudate on epicardial surface due to terminal renal failure
-
Fibrinous pericarditis: Gross, natural color, anterior view of heart with mild fibrinous exudate over epicardium due to terminal renal failure
-
Tuberculous pericarditis: Gross, natural color, shaggy hemorrhagic exudate. This case is much more hemorrhagic than the typical tuberculous pericarditis.
-
Heart transplant: Gross, natural color, external view of heart. Two months after transplantation with fibrinous pericarditis
-
Neoplastic pericarditis: Gross, natural color, shaggy pericarditis. Primer is adenocarcinoma of the lung.
-
Heart: Septic pericarditis
-
Hemopericardium: Gross, an excellent in situ view
-
Hemopericardium: Gross, in situ, unopened pericardium (a very good example)
-
Hemopericardium: Gross, natural color, heart in situ with opened pericardium and filled with red blood clot (quite good example) dissecting aneurysm
-
Hemopericardium due to Needle Puncture: Gross, natural color, external view of heart covered by blood
-
Needle Puncture Mark in Epicardium: Gross, natural color, close-up of needle puncture marks tap resulted in hemopericardium
-
Hemopericardium: Hemopericardium caused by pericardiocentesis: Gross, natural color, close-up view of apex of the heart. Needle apparently entered the distal posterior descending artery.
-
Hemopericardium: Hemopericardium caused by pericardiocentesis: Gross, natural color, view of apex of the heart. Needle apparently entered the distal posterior descending artery
-
Hemopericardium: Hemopericardium due to pericardiocentesis: Gross, fixed tissue, close-up view of slice through distal posterior descending artery showing periarterial hemorrhage
-
Hemopericardium: Liver: Gross, natural color, typical shock liver case of death due to hemopericardium secondary to pericardiocentesis
-
Hemopericardium in newborn: Gross, natural color, opened body with large collection blood in pericardial sac. Cause uncertain. A 26 week premature with hyaline membrane disease and DIC
-
Hemopericardium: Myocardial Infarction and Ventricular Rupture
-
Hemopericardium: Infarct rupture after 7 days of chest pain onset.
-
Hemopericardium in dissecting aneurysm: Gross, heart with root of aorta to show hemorrhage into pericardium (very good example)
Microscopic Images
-
Tuberculous pericarditis.
-
Tuberculous pericarditis.
-
Tuberculous pericarditis: Micro oil acid fast stain. The organism easily seen.
-
Tuberculous pericarditis: Micro oil acid fast stain. The organism easily seen.
-
Uremic pericarditis: Micro med mag, H&E. A good example
-
Tuberculous pericarditis: Micro med mag, H&E, a typical lesion
-
Fibrinous pericarditis.
-
Pericarditis fibrinosa (Fibrinous pericarditis).
-
Malignant Mesothelioma, Biphasic Type: Pericardium: This tumor has epithelioid cells (lower half) surrounded by spindled cells. The patient was a 46-year-old woman with constrictive pericarditis; the pericardium was studded with coalescing tumor nodules.
- <Youtube v=AKS7kSl4x5k/>
- Acute fibrinous pericarditis
<Youtube v=5fz_W1YxbC8/>
Differential Diagnosis for Diseases of the Pericardium
Many other conditions produce signs and symptoms similar to those produced by pericarditis. Keep in mind that pericarditis might also be one of the following: "part of a generalized disease", "apparently isolated", or "part of a disease that affects a nearby organ", and "sometimes is the presenting syndrome of multiple diseases."
Key Signs & Symptoms to Differentiate Pericarditis:
- Pain on the trapezius ridge(s), is a pathognomonic of pericarditis. Often pain can radiate mimicking pain that is commonly felt during angina.
- Central pleuritic chest pain (can also be indicative of pleurisy; however, may be both)
- Pain that lasts longer, is sharper and unresponsive to vasodilator therapy (similar "to that of cardiac ischemia")
- Most acute pericarditis ECGs are similar to ECGs of ischemic heart disease rather than infarction
- Pulmonary embolism can present similarly to pericarditis, but can be differentiated from pericarditis in the presence of one of the following findings: a nonspecifically altered ECG, a plerual rub, and non-precordial (someitmes precordial pain is present regardless).
Acute Pericarditis
- Actinomycosis
- Acute idiopathic pericarditis
- Acute rheumatic fever
- Adenovirus
- Addison's crisis
- Amyloidosis
- Amebiasis
- Ankylosing Spondylitis
- Aortic dissection
- Behcet's Disease
- Borrelia
- Breast cancer
- Chylopericardium
- Coxsackie A
- Coxsackie B
- Cytomegalovirus
- Dermatomyositis
- Dermatosclerosis
- Dressler's Syndrome
- EBV
- ECHO virus
- Echinococcosis
- Familial Mediterranian Fever
- Francisella
- HIV
- Infectious mononucleosis
- Inflammatory Bowel Disease
- Influenza virus
- Legionella
- Leukemia
- Lung cancer
- Lymphoma
- Meningococci
- Mixed Connective Tissue Disease
- Mumps virus
- Mycoplasma infection
- Neisseria gonorrhoeae
- Perforated esophagus
- Pneumococci
- Polyarteritis Nodosa
- Polymyositis
- Postpericardiotomy syndrome
- Reiter's Syndrome
- Radiation therapy
- Renal Failure
- Rheumatoid Arthritis
- Rickettsia
- Sarcoidosis
- Scleroderma
- Serum sickness
- Staphylococci
- Streptococci
- Systemic Lupus Erythematosus
- Thorax trauma
- Treponema pallidum
- Toxoplasmosis
- Tuberculosis
- Uremia
- Varicella virus
- Wegener's granulomatosis
- Whipple's Disease
Chronic Pericarditis
- Amebiasis
- Bacterial infections
- Cholesterol pericarditis
- Chylopericardium
- Coccidioidomycosis
- Collagen Vascular Disease
- Coxsackie B
- Echinococcosis
- Histoplasmosis
- Neoplastic pericarditis
- Tuberculosis
- Uremic pericarditis
Treatment
The majority of patients with pericarditis are hospitalized so they can be observed and monitored for complications while they recover. The treatment of viral or idiopathic pericarditis is with non-steroidal anti-inflammatory drugs. Patients should be observed for side effects since NSAIDs are known to effect the GI mucosa.
Severe cases of pericarditis may require:
Patients with uncomplicated acute pericarditis can generally be treated and followed up in an outpatient clinic. However, those with high risk factors for developing complications (see above) will need to be admitted to an inpatient service, most likely an ICU setting. High risk patients include:[10]
- subacute onset
- high fever (> 100.4 F) and leukocytosis
- development of cardiac tamponade
- large pericardial effusion (echo-free space > 20 mm) resistant to NSAID treatment
- immunocompromised
- history of oral anticoagulation therapy
- acute trauma
- failure to respond to seven days of NSAID treatment.
Usual Steps in Treatment of Pericarditis
Pericardiocentesis is a procedure whereby the fluid in a pericardial effusion is removed through a needle. It is performed under the following conditions:[11]
- presence of moderate or severe cardiac tamponade
- diagnostic purpose for suspected purulent, tuberculosis, or neoplastic pericarditis
- persistent symptomatic pericardial effusion
NSAIDs in viral or idiopathic pericarditis. In patients with underlying causes other than viral, the specific etiology should be treated. With idiopathic or viral pericarditis, NSAID is the mainstay treatment. Goal of therapy is to reduce pain and inflammation. The course of the disease may not be affected. The preferred NSAID is ibuprofen because of rare side effects, better effect on coronary flow, and larger dose range.[11] Depending on severity, dosing is between 300-800 mg every 6-8 hours for days or weeks as needed. An alternative protocol is aspirin 800 mg every 6-8 hours.[10] Dose tapering of NSAIDs may be needed. In pericarditis following acute myocardial infarction, NSAIDs other than aspirin should be avoided since they can impair scar formation. As with all NSAID use, GI protection should be engaged. Failure to respond to NSAIDs within one week (indicated by persistence of fever, worsening of condition, new pericardial effusion, or continuing chest pain) likely indicates that a cause other than viral or idiopathic is in process.
Colchicine can be used alone or in conjunction with NSAIDs in prevention of recurrent pericarditis and treatment of recurrent pericarditis. For patients with a first episode of acute idiopathic or viral pericarditis, they should be treated with an NSAID plus colchicine 1-2 mg on first day followed by 0.5 daily or BID for three months. [12][13][14]
Corticosteroids are usually used in those cases that are clearly refractory to NSAIDs and colchicine and a specific cause has not been found. Systemic corticosteroids are usually reserved for those with autoimmune disease.
Pharmacotherapy
Acute Pharmacotherapies
As previously mentioned, the typical pharmacotherapy in viral or idiopathic pericarditis is with NSAIDs. These drugs have analgesic, antipyretic and anti-inflammatory effects. The most prominent members of this group of drugs are aspirin and ibuprofen. Paracetamol (acetaminophen) has negligible anti-inflammatory activity.
Chronic Pharmacotherapies
Severe cases may require one of the aforementioned procedures or one of the alternative pharmacotherapies listed below:
- Antibiotics
- Steroids
Surgical and Device Based Therapies
Pericardiocentesis
A thoracoscopic approach to creating a pericardial window
A surgical subxiphoid incision to create a pericardial window
Pericardial Stripping for Constrictive Pericarditis
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This may be effective in up to 50% of patients. This procedure has significant risk involved, since the thickened pericardium is often adherent to the myocardium and coronary arteries.
In patients who have undergone coronary artery bypass surgery with pericardial sparing, there is danger of tearing a bypass graft while removing the pericardium. If any pericardium is not removed, it is possible for bands of pericardium to cause localized constriction which may cause symptoms and signs consistent with constriction.
Treatment Related Videos
- <youtube v=lJ6KzpnjbRg/>
Complications
Fibrinous pericarditis
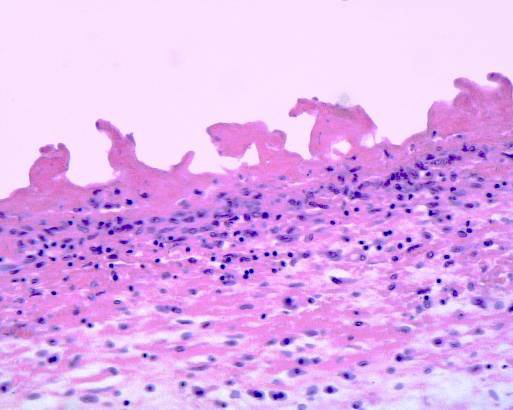
Fibrinous pericarditis is an exudative inflammation. The pericardium is infiltrated by the fibrinous exudate. This consists of fibrin strands and leukocytes. Fibrin describes an amorphous, eosinophilic (pink) network. Leukocytes (mainly neutrophils) are found within the fibrin deposits and intrapericardic. Vascular congestion is also present. The myocardium has no changes. Sometimes referred to as having "Bread and Butter Appearance". Photo at: Atlas of Pathology
Pericarditis due to tuberculosis
Pericarditis caused by tuberculosis is difficult to diagnose, because definitive diagnosis requires culturing Mycobacterium tuberculosis from aspirated pericardial fluid or pericardial biopsy, which requires high technical skill and is often not diagnostic (the yield from culture is low even with optimum specimens).
The Tygerberg scoring system helps the clinician to decide whether pericarditis is due to tuberculosis or whether it is due to another cause:
- Night sweats (1 point),
- Weight loss (1 point),
- Fever (2 point),
- Serum globulin > 40g/l (3 points),
- Blood total leucocyte count <10 x 109/l (3 points);
A total score of 6 or more is highly suggestive of tuberculous pericarditis.[15]
Pericardial fluid with an interferon-γ level greater than 50pg/ml is highly specific for tuberculous pericarditis.
The definitive treatment for constrictive pericarditis is pericardial stripping, which is a surgical procedure where the entire pericardium is peeled away from the heart. This procedure has significant risk involved,[16] with mortality rates of 6% or higher in major referral centers.[17][18] The high risk of the procedure is attributed to adherence of the thickened pericardium to the myocardium and coronary arteries. In patients who have undergone coronary artery bypass surgery with pericardial sparing, there is danger of tearing a bypass graft while removing the pericardium.
References
- ↑ Maisch B, Ristic AD (2002). "The classification of pericardial disease in the age of modern medicine". Curr Cardiol Rep. 4 (1): 13–21. doi:10.1007/s11886-002-0121-6. PMID 11743917.
- ↑ 2.0 2.1 Spodick DH (2003). "Acute pericarditis: current concepts and practice". JAMA. 289 (9): 1150–3. doi:10.1001/jama.289.9.1150. PMID 12622586.
- ↑ Karjalainen J, Heikkila J (1986). ""Acute pericarditis": myocardial enzyme release as evidence for myocarditis". Am Heart J. 111 (3): 546–52. doi:10.1016/0002-8703(86)90062-1. PMID 3953365.
- ↑ Bonnefoy E, Godon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P (2000). "Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis". Eur Heart J. 21 (10): 832–6. doi:10.1053/euhj.1999.1907. PMID 10781355.
- ↑ 5.0 5.1 Imazio M, Demichelis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R (2003). "Cardiac troponin I in acute pericarditis". J Am Coll Cardiol. 42 (12): 2144–8. doi:10.1016/j.jacc.2003.02.001. PMID 14680742.
- ↑ Troughton RW, Asher CR, Klein AL (2004). "Pericarditis". Lancet. 363 (9410): 717–27. doi:10.1016/S0140-6736(04)15648-1. PMID 15001332.
- ↑ Chotas HG, Dobbins JT, Ravin CE (1999) Principles of digital radiography with large-area, electronically readable detectors: a review of the basics. Radiology 210:595-599
- ↑ Higgins CB, De Roos A (2003) Cardiovascular MRI and MRA. Lippincott Williams & Wilkins, Philadelphia
- ↑ Ohnesorge BM, Becker CR, Flohr TG, Reiser MF (2001) Multislice CT in cardiac imaging. Springer-Verlag
- ↑ 10.0 10.1 Imazio M, Demichelis B, Parrini I, Giuggia M, Cecchi E, Gaschino G, Demarie D, Ghisio A, Trinchero R (2004). "Day-hospital treatment of acute pericarditis: a management program for outpatient therapy". J Am Coll Cardiol. 43 (6): 1042–6. doi:10.1016/j.jacc.2003.09.055. PMID 15028364.
- ↑ 11.0 11.1 Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH (2004). "Guidelines on the diagnosis and management of pericardial diseases executive summary; The Task force on the diagnosis and management of pericardial diseases of the European Society of Cardiology". Eur Heart J. 25 (7): 587–10. doi:10.1016/j.ehj.2004.02.002. PMID 15120056.
- ↑ Adler Y, Zandman-Goddard G, Ravid M, Avidan B, Zemer D, Ehrenfeld M, Shemesh J, Tomer Y, Shoenfeld Y (1994). "Usefulness of colchicine in preventing recurrences of pericarditis". Am J of Cardiol. 73 (12): 916–7. doi:10.1016/0002-9149(94)90828-1. PMID 8184826.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Demichelis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) trial". Circulation. 112 (13): 2012–6. doi:10.1161/CIRCULATIONAHA.105.542738. PMID 16186437.
- ↑ Imazio M, Bobbio M, Cecchi E, Demarie D, Pomari F, Moratti M, Ghisio A, Belli R, Trinchero R (2005). "Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial". Arch Intern Med. 165 (17): 1987–91. doi:10.1001/archinte.165.17.1987. PMID 16186468.
- ↑ Reuter H, Burgess L, van Vuuren W, Doubell A. (2006). "Diagnosing tuberculous pericarditis". Q J Med. 99: 827&ndash, 39. PMID 17121764.
- ↑ Cinar B, Enc Y, Goksel O, Cimen S, Ketenci B, Teskin O, Kutlu H, Eren E. (2006). "Chronic constrictive tuberculous pericarditis: risk factors and outcome of pericardiectomy". Int J Tuberc Lung Dis. 10 (6): 701–6. PMID 16776460.
- ↑ Chowdhury UK, Subramaniam GK, Kumar AS, Airan B, Singh R, Talwar S, Seth S, Mishra PK, Pradeep KK, Sathia S, Venugopal P (2006). "Pericardiectomy for constrictive pericarditis: a clinical, echocardiographic, and hemodynamic evaluation of two surgical techniques". Ann Thorac Surg. 81 (2): 522–9. doi:10.1016/j.athoracsur.2005.08.009. PMID 16427843.
- ↑ Ling LH, Oh JK, Schaff HV, Danielson GK, Mahoney DW, Seward JB, Tajik AJ (1999). "Constrictive pericarditis in the modern era: evolving clinical spectrum and impact on outcome after pericardiectomy". Circulation. 100 (13): 1380–6. PMID 10500037.
Acknowledgements
The content on this page was first contributed by C. Michael Gibson, M.S., M.D.
Additional Resources
- Adler Y, Finkelstein Y, Guindo J, de la Serna R, Shoenfeld Y, Bayes-Genis A, Sagie A, Bayes de Luna A, Spodick DH. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183–2185.
- Applegate RJ, Johnston WE, Vinten-Johansen J, Klopfenstein HS, Little WC. Restraining effect of intact pericardium during acute volume leading. Am J Physiol. 1992;262:H1725–H1733.
- Artom G, Koren-Morag N, Spodick DH, Brucato A, Guindo J, Bayesde-Luna A, Brambilla G, Finkelstein Y, Granel B, Bayes-Genis A, Schwammenthal E, Adler Y. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: a multicentre all-case analysis. Eur Heart J. 2005;26:723–727.
- Arunasalam S, Siegel RJ. Rapid resolution of symptomatic acute pericarditis with ketorolac tromethamine: a parenteral nonsteroidal antiinflammatory agent. Am Heart J. 1993;125(pt 1):1455–1458.
- Bonnefoy E, Gordon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832–836.
- Correale E, Maggioni AP, Romano S, Ricciardiello V, Battista R, Salvarola G, Santoro E, Tognoni G, on behalf of the Gruppo Italiano perlo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI). Comparison of frequency, diagnostic and prognostic significance of pericardial involvement in acute myocardial infarction treated with and without thrombolytics. Am J Cardiol. 1993;71:1377–1381.
- Fowler NO. Tuberculous pericarditis. JAMA. 1991;266:99 –103.
- Freeman GL, LeWinter MM. Determinants of the intrapericardial pressure in dogs. J Appl Physiol. 1986;60:758 –764.
- Freeman GL, LeWinter MM. Pericardial adaptations during chronic cardiac dilation in dogs. Circ Res. 1984;54:294 –300.
- Freeman GL, Little WC. Comparison of in situ and in vitro studies of pericardial pressure-volume relation in the dog. Am J Physiol. 1986;251: H421–H427.
- Gunukula SR, Spodick DH. Pericardial disease in renal patients. Semin Nephrol. 2001;21:52–56.
- Hoit BD, Gabel M, Fowler NO. Cardiac tamponade in left ventricular dysfunction. Circulation. 1990;82:1370–1376.
- Imazio M, Bobbio M, Cecchi E, Demarie D, Demichellis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghiso A, Belli R, Trinchero R. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) Trial. Circulation. 2005;112:2012–2016.
- Imazio M, Demichellis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42:2144–2148.
- Imazio M, Demichellis B, Parrini I, Gluggia M, Cecchi E, Gaschino G, Demarie D, Ghislo A, Trinchero R. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042–1046.
- Jerjes-Sanchez C, Ramirez-Rivera A, Ibarra-Perez C. The Dressler syndrome after pulmonary embolism. Am J Cardiol. 1996;78:343–345.
- Kansal S, Roitman D, Sheffield LT. Two-dimensional echocardiography of congenital absence of pericardium. Am Heart J. 1985;109:912–915.
- Klopfenstein HS, Schuchard GH, Wann LS, Palmer TE, Hartz AJ, Gross CM, Singh S, Brooks HL. The relative merits of pulsus paradoxus and right ventricular diastolic collapse in the early detection of cardiac tamponade: an experimental echocardiographic study. Circulation. 1985;71: 829–833.
- Knopf WD, Talley JD, Murphy DA. An echo-dense mass in the pericardial space as a sign of left ventricular free wall rupture during acute myocardial infarction. Am J Cardiol. 1987;59:1202.
- Lange RA, Hillis D. Acute pericarditis. N Engl J Med. 2004;351: 2195–2202.
- LeWinter MM, Kabbani S. Pericardial diseases. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald’s Heart Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders; 2005:1757–1780.
- Maisch B, Ristic D, Pankuweit S. Intrapericardial treatment of autoreactive pericardial effusion with triamcinolone. Eur Heart J. 2002;23: 1503–1508.
- Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH, for the Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases: executive summary. Eur Heart J. 2004;25:587– 610.
- Maisch B. Recurrent pericarditis: mysterious or not so mysterious? Eur Heart J. 2005;26:631– 633.
- Mandell BF. Cardiovascular involvement in systemic lupus erythematosus. Semin Arthritis Rheum. 1987;17:126 –141.
- Miyazaki T, Pride HP, Zipes DP. Prostaglandins in the pericardial fluid modulate neural regulation of cardiac electrophysiological properties. Circ Res. 1990;66:163–175.
- Park JH, Choo SJ, Park SW. Acute pericarditis caused by acrylic bone cement after percutaneous vertebroplasty. Circulation. 2005; 111:e98.
- Permanyer-Miralda G, Sagrista-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985;56:623– 630.
- Permanyer-Miralda G. Acute pericardial disease: approach to the aetiologic diagnosis. Heart. 2004;90:252–254.
- Reddy PS, Curtiss EI, O’Toole JD, Shaver JA. Cardiac tamponade: hemodynamic observations in man. Circulation. 1978;58:265–272.
- Reddy PS, Curtiss EI, Uretsky BF. Spectrum of hemodynamic changes in cardiac tamponade. Am J Cardiol. 1990;66:1487–1491.
- Shabetai R, Fowler NO, Guntheroth WG. The hemodynamics of cardiac tamponade and constrictive pericarditis. Am J Cardiol. 1970;26: 480–489.
- Shabetai R. Pericardial effusion: haemodynamic spectrum. Heart. 2004; 90:255–256.
- Shabetai R. Recurrent pericarditis: recent advances and remaining questions. Circulation. 2005;112:1921–1923.
- Singh S, Wann S, Schuchard GH, Klopfenstein HS, Leimgruber PP, Keelan MH, Brooks HL. Right ventricular and right atrial collapse in patients with cardiac tamponade: a combined echocardiographic and hemodynamic study. Circulation. 1984;70:966–971.
- Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349: 684–690.
- Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150 –1153.
- Spodick DH. Intrapericardial treatment of persistent autoreactive pericarditis / myopericarditis and pericardial effusion. Eur Heart J. 2002;23: 1481–1482.
- Spodick DH. Macrophysiology, microphysiology, and anatomy of the pericardium: a synopsis. Am Heart J. 1992;124:1046 –1051.
- Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363: 717–727.
- Tsang TS, Barnes ME, Hayes SN, Freeman WK, Dearani JA, Butler SL, Seward JB. Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echo-guided pericardiocentesis for management: Mayo Clinic experience, 1979–1998. Chest. 1999;116:322–331.
- Tsang TS, Oh JK, Seward JB, Tajik AJ. Diagnostic value of echocardiography in cardiac tamponade. Herz. 2000;25:734–740.
- Zayas R, Anguita M, Torres F, Gimenez D, Bergillos F, Ruiz M, Ciudad M, Gallardo A, Valles F. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378 –382.
Suggested Links and Web Resources
- Pericarditis - Mayo Clinic series
- Pericarditis - cardiologychannel.com
- Pericarditis information from Seattle Children's Hospital Heart Center
- Pulsus paradoxus - Journal of Postgraduate Medicine
- http://en.wikipedia.org/wiki/Pericarditis
- SeeMyHeart - Patient Information on Echocardiograms (Heart Ultrasounds)
- American Society of Echocardiography
- Stress Test with Echocardiography from Angioplasty.Org
- Echocardiography information from Children's Hospital Heart Center, Seattle.
- Coronary heart disease And echocardiography
- Echocardiography Resources Simple echocardiography tutorials
- Atlas of Echocardiography Echocardiography Database
- E-chocardiography Internet Journal of Cardiac Ultrasound
- Echobasics Basic introduction to echocardiography - German/Spanish English planned for 2007
- Echocardiography Basic information about echocardiography - HealthwoRx
For Patients
de:Perikarditis
nl:Pericarditis
sv:Hjärtsäcksinflammation