AV junctional rhythms
(Redirected from AV Junctional Rhythms)
| AV junctional rhythms | |
 | |
|---|---|
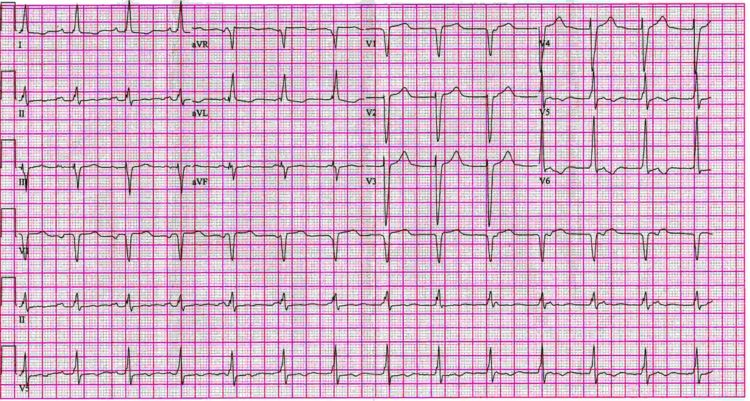
| Lead II and V5 rhthm strip of a patients with junctional rhythm with AV dissociation. Note to P wave - QRS complex relations. | |
| ICD-10 | 147.1, 149.2 |
| eMedicine | med/ |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
EKG findings of Junctional Rhythms
- The P wave axis is -60 to -80 degrees (normal is 0 to 75 degrees)
- The P wave of the junctional beat may
- Precede the QRS in an "upper" nodal rhythm
- Superimpose on the QRS in a "middle" nodal rhythm
- Follow the QRS in a "lower" nodal rhythm
- This depends not only on the location of the pacemaker (upper, middle, or lower) but also on the retrograde conduction of the impulse.
- There could be a pacemaker located in the upper portion of the node, but if retrograde conduction was slow, then the P wave would not precede the QRS
- Thus these terms pertaining to the nodal location may be misleading and are no longer used.
- Typically the PR interval is < .11 second, the RP interval may be up to .20 seconds
- The morphology of the QRS is not altered.
"Passive" Junctional Rhythms
- AV junction is the site of impulse formation when there is depression of the SA node, SA block, sinus bradycardia, sinus arrhythmia.
- In this case the rhythm is an escape rhythm
- Occurs if the sinus rate is slower than that of the junctional pacemaker (35 to 60 BPM)
- May occur after the postextrasystolic pause on an atrial or ventricular premature beat.
- Occasionally the sinus and the AV junctional rhythm ore at similar rates and the P waves and the QRS complexes are in proximity to each other but are unrelated to each other. This phenomenon is called isorhythmic AV dissociation.
- The ventricular rate increases with atropine
- The QRS morphology is similar to that in NSR, including any aberrancy
- May be seen in patients with SA nodal, AV nodal disease, digoxin, healthy people with sinus bradycardia.
"Active" Junctional Rhythms
- Junctional tachycardia at a rate > 60 BPM
- When there is a junctional pacemaker the P waves are inverted in leads 2,3,F.
- includes premature junctional beats
- Are premature
- Morphologic characteristics of an AV junctional beat
- Usually have a constant coupling interval
- In most cases the postextrasystolic pause is not fully compensatory. The retrograde conducted impulse discharges the SA node and resets its rhythmicity.
- Differential diagnosis:
- PACs: PJCs more likely if the P waves are inverted inferiorly, if the PR is < .12, and if the QRS is normal in duration.
- PVCs: if a retrograde P occurs after the beat, and the RP is < .11, then it is unlikely to be a PVC because the interval is too short to complete VA conduction.
- Includes paroxysmal AV junctional tachycardia (AV nodal reentrant and automatic junctional tachycardia)
- May be due to reentry or increased automaticity.
- Onset and termination are abrupt. May last seconds, hours or days.
- Rate 140 to 220 BPM and is regular.
- The P-QRS complex has the morphologic characteristic of a junctional beat.
- P waves are inverted in 2,3,F. In many cases they are buried and cannot be identified.
- QRS can be wide if there is preexistent IVCD.
- In AV junctional tachycardia, vagal stimulation has little effect on this rhythm
- Can be seen in healthy patients, those with CAD, and with dig toxicity
- Includes nonparoxysmal junctional tachycardia (accelerated AV junctional rhythm)
The Frequently Used Term "Paroxysmal Supraventricular Tachycardia"
- Sudden onset of a regular, narrow complex tachycardia
- Two basic mechanisms: reentry and automaticity
- Differential diagnosis includes
- Sinus node reentry
- Uncommon, < 5% of cases of SVT
- Suggested if the P waves are identical those to the P waves of NSR
- Rate is between 100 and 160 BPM (average 130 BPM)
- Slower than other forms of PSVT
- May be slowed and terminated by CSM
- Intraatrial reentry
- Uncommon with same incidence as sinus node reentry tachycardia
- P waves usually upright in inferior leads, have a different morphology than in NSR
- Not influenced by CSM
- AV nodal reentry
- Causes 60% of PSVTs
- P waves are inverted in the inferior leads
- In 2/3rds of these cases they are superimposed on the QRS
- In other cases they appear immediately after the QRS
- Rate is fast, 140 to 200 BPM
- As a rule vagal maneuvers terminate the tachycardia
- Reentry using an accessory pathway (WPW):
- The accessory pathway is either the anterograde or the retrograde pathway of the reentry circuit
- If conduction is down the regular AV node, then the QRS is not widened, this is more common.
- If conduction is down the accessory pathway, then the QRS is widened.
- Reentry using a concealed AV bypass tract:
- The bypass tract conducts only retrograde, resting EKG is unrevealing
- Narrow QRS complex during tachycardia.
- In both this and in WPW there are always inverted P waves that follow the QRS.
- The fact that P waves can be identified in these tachyarrhythmias is how WPW and bypass tracts can be distinguished for AV nodal reentry tachycardias.
- The rate of tachycardias associated with bypass tracts is faster than that due to AV nodal reentry and is 150 to 240 BPM, suspect this when the rate is > 200 BPM.
- Although patients with WPW frequently experience tachyarrhythmias, it is more common for a person with a narrow complex tachycardia to have a concealed bypass tract as a cause. Concealed bypass tracts cause 15 to 30% of PSVTs
- Enhanced automaticity of an atrial focus
- P waves always precede the QRS.
- May be inverted in the inferior leads if there is a low atrial focus.
- Relatively slow, 100 to 180 BPM.
- The PR is > .12 seconds.
- After a few beats the tachycardia accelerates.
- The tachycardia may be associated with AV block (i.e. PAT with block).
- Accounts for < 5% of PSVTs.
- Vagal maneuvers do not terminate these.
- Enhanced automaticity of an AV junctional focus
- Rare, similar characteristics to that of an atrial focus
- Sinus node reentry
Nonparoxysmal Junctional Tachycardia (Accelerated AV Junctional Rhythm)
- Abnormal impulse formation at the AV junction.
- Rate is only moderately increased to about 70 to 130 BPM.
- Lacks the sudden onset and termination characteristic of the paroxysmal type.
- Often the result of dig intoxication, acute MI, CT surgery, myocarditis.
Reciprocal or Echo Beats
- Occurs when the impulse activates a chamber, returns, and reactivates the chamber again.
- Used to refer to the phenomenon of one or two beats.
- If the process continues, it is called reentrant tachycardia.
- An anterograde and a retrograde pathway are required, and both are usually in the AV node.
- In Echo beats of atrial origin, there is a P-QRS-P sequence.
- In Echo beats of ventricular origin, there is a QRS-P-QRS sequence.
References
- Hammill S. C. Electrocardiographic diagnoses: Criteria and definitions of abnormalities, Chapter 18, MAYO Clinic, Concise Textbook of Cardiology, 3rd edition, 2007 ISBN 0-8493-9057-5
Additional resources
- ECGpedia: Course for interpretation of ECG
- The whole ECG - A basic ECG primer
- 12-lead ECG library
- Simulation tool to demonstrate and study the relation between the electric activity of the heart and the ECG
- ECG information from Children's Hospital Heart Center, Seattle
- ECG Challenge from the ACC D2B Initiative
- National Heart, Lung, and Blood Institute, Diseases and Conditions Index
- A history of electrocardiography
- EKG Interpretations in infants and children
EKG Examples
-
12 lead EKG: AV junctional rhythm with Atrioventricular dissociation
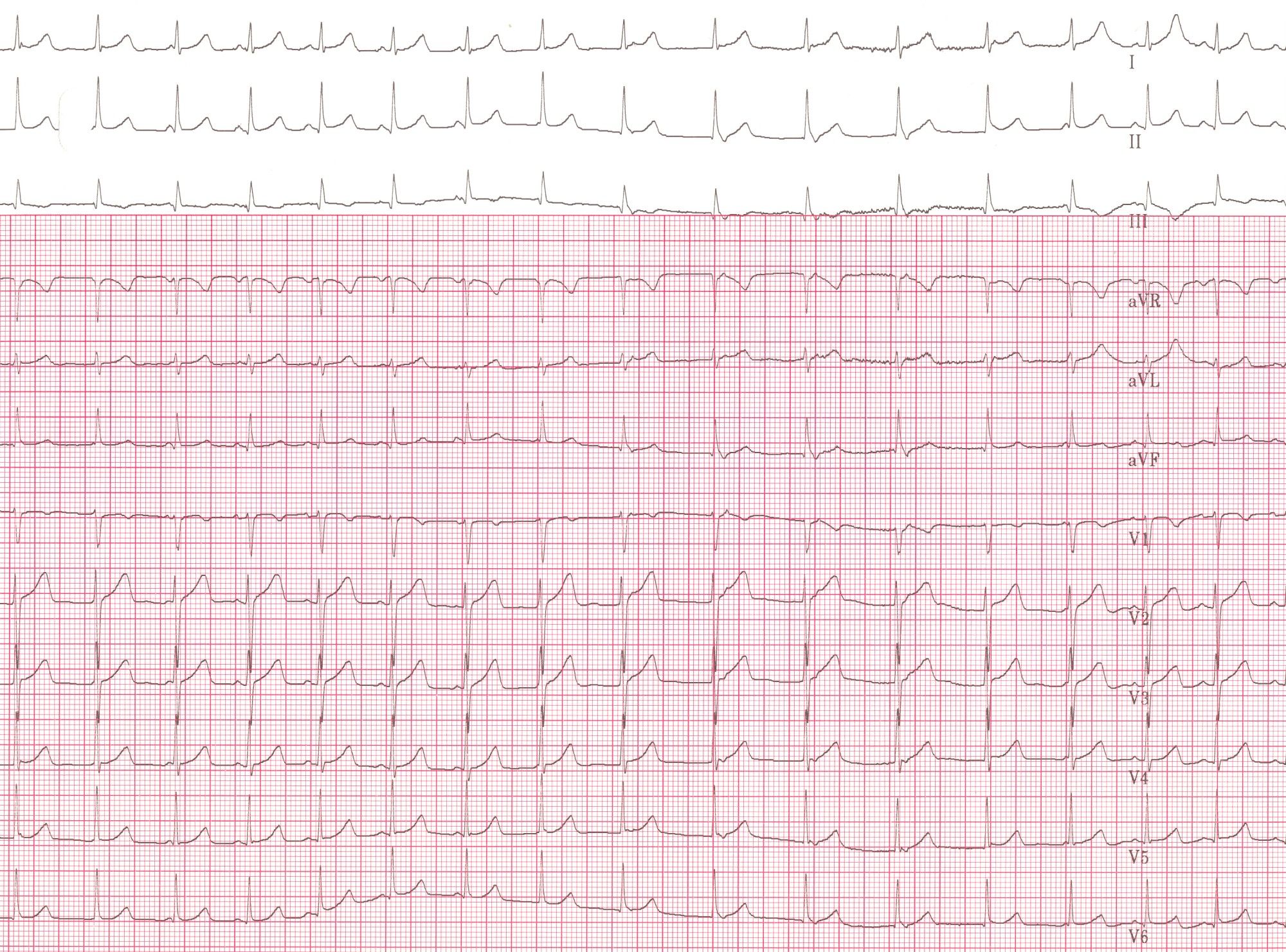
-
12 lead EKG: Junctional Ectopic Tachycardia (JET)