ST interval
|
WikiDoc Resources for ST interval |
|
Articles |
|---|
|
Most recent articles on ST interval Most cited articles on ST interval |
|
Media |
|
Powerpoint slides on ST interval |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on ST interval at Clinical Trials.gov Clinical Trials on ST interval at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on ST interval
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on ST interval Discussion groups on ST interval Patient Handouts on ST interval Directions to Hospitals Treating ST interval Risk calculators and risk factors for ST interval
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for ST interval |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: ST segment depression, ST segment elevation; J point elevation; vaulting of the ST segments; current of injury
Overview
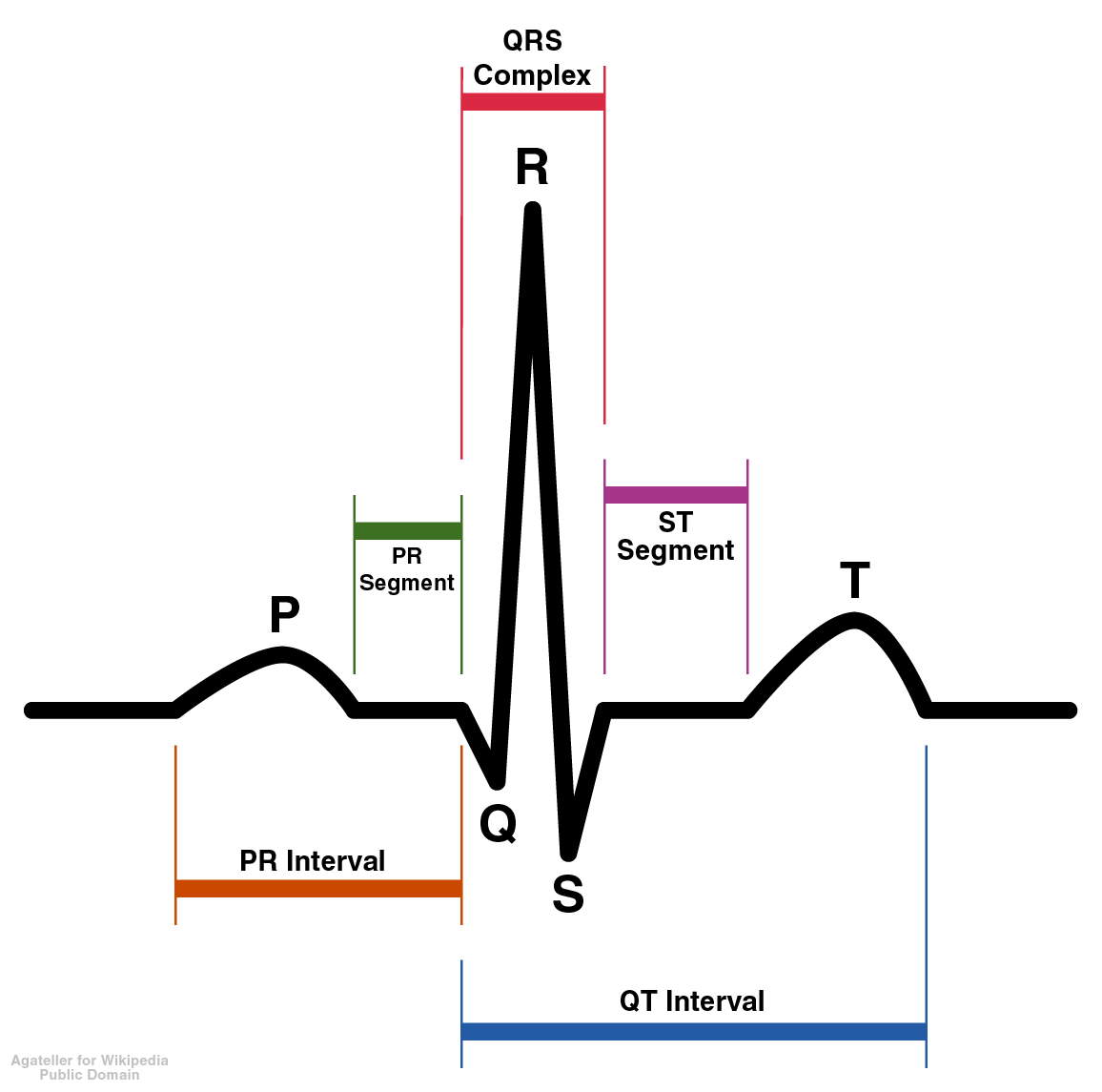
The ST interval represents the initial, slow phase of ventricular repolarization.[1] The ST segment commonly refers to the morphology of the segment between the end of the S wave (the terminal deflection of the QRS) and the beginning of the T wave.
The Normal ST segment
The ST segment represents the ventricular repolarisation. Repolarisation follows upon contraction and depolarisation. During repolarisation the cardiomyocytes elongate and prepare for the next heartbeat. This process takes much more time than the depolarisation. Repolarisation is not passive elongation by stretch, it is an active process during which energy is consumed. On the ECG, the repolarisation phase starts at the junction, or j point, and continues until the T wave. The normal ST segment should not be flat. It should have an upward concavity sometimes referred to as a “take-off”.
The T wave is usually concordant with the QRS complex. Thus if the QRS complex is positive in a certain lead (the area under the curve above the baseline is greater than the area under the curve below the baseline) than the T wave usually is positive too in that lead. Accordingly the T wave is normally upright or positive in leads I, II, AVL, AVF and V3-V6. The T wave is negative in V1 and AVR. The T wave flips around V2, but there is some genetical influence in this as in Blacks the T wave usually flips around V3.
The T wave angle is the result of small differences in the duration of the repolarisation between the endocardial and epicardial layers of the left ventricle. The endocardial myocytes need a little more time to repolarise (about 22 msec). This difference causes an electrical current from the endocardium to the epicardium, which reads as a positive signal on the ECG. [2]
ST Segment Changes in Acute Myocardial Injury or Ischemia
EKG manifestations of acute myocardial injury or ischemia in absence of left ventricular hypertrophy and LBBB are as follow:[3] [4]
- ST segment elevation
In general, ST segment elevation reflects myocardial injury, which may be irreversible (unlike ischemia which may be reversible) and which is associated with a risk of necrosis. ST elevation is defined as new ST segment elevation at the J point in two contiguous leads with the cut off points ≥0.2 mV in men or ≥0.15 mV in women in V2-V3 and ≥0.1 mV in other leads.
- ST segment depression and T wave changes
In general, ST depresstion represents reversible ischemia (less likely to result in irreversible necorsis). One exception is the presence of ST depression in the anterior precordial leads that can reflect posterior injury rather than anterior ischemia. Ischemia is defined as new horizontal or downsloping ST segment changes as ≥0.05 mV in two contiguous leads and/or T wave inversion ≥0.1 mV in two contiguous leads with prominent R wave or in situations which R wave amplitude / S wave amplitude ratio is >1.
Althought it is not observed in women, the J point elevation in men decreases with increasing age.[5]
The term of contiguous lead represents lead groups such as anterior leads (V1-V6), inferior leads (II, III, and aVF), or lateral/apical leads (I and aVL).
Shown below is a table depicting the interpretation of ST elevation and ST depression by the involved contiguous leads.
| ST elevation | ||
| Leads | Interpretation | Involved artery |
| V1-V2 | Septal MI, or Right ventricular MI[6] |
LAD RCA |
| V3-V4 | Anterior MI | LAD |
| V5-V6 I-aVL |
Lateral MI | Left circumflex artery |
| II-III-aVF | Inferior MI | RCA in 85% of the cases Left circumflex artery in 15% of the cases |
| V1-V2- V4R | Right ventricular MI[7] | RCA |
| ST depression | ||
| Leads | Interpretation | Involved artery |
| V1-V2-V3 | Anterior ischemia[8], or Posterior MI [9], or Reciprocal changes[10] |
LAD RCA or left circumflex artery - |
ST Depression
Causes of ST Segment Depression
- Ischemia particularly if the ST segment is downsloping
- "Reciprocal changes" which are associated with a pattern of injury (ST segment elevation) in other leads. It is unclear if the ST depression is truly simply a reciprocal change which is a mirror image electrically of the injury in the other leads or if the ST depression is due to active ischemia in the other territory. Reciprocal changes are associated with a poorer prognosis. Reciprocal changes in the anterior precordial leads in association with an inferior MI are associated with slower flow in the LAD
- Digoxin effect (concave up;"reverse-checkmark")
- LV "strain"-associated with LVH (asymmetric ST depression, concave up, with slow downstroke and rapid upstroke, most often in I, aVL, V4-6)
- RV "strain"-associated with RVH (asymmetric ST depression, concave up, with slow downstroke and rapid upstroke, most often in V1-2)
- Hypokalemia (usually slight ST depression)
- Hypercalcemia
- Hypomagnesemia
- Heart rate-induced changes (post tachycardia)
- Neurologic events
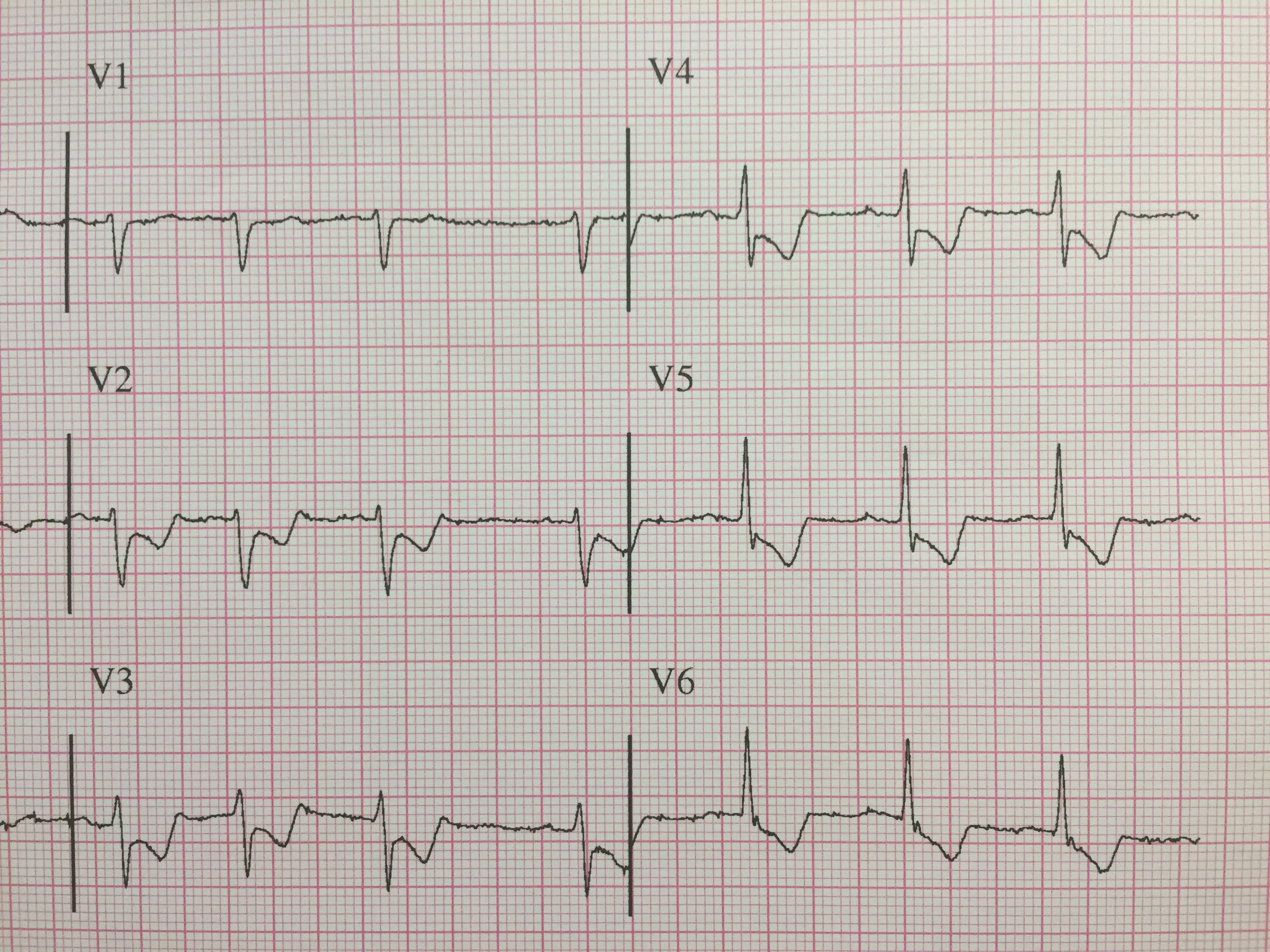
Shown below is an ECG depicting ST depression in the precordial leads.
ST Elevation
Pathophysiology
ST segment corresponds to a period of ventrical systolic depolarization, when the cardiac muscle is contracted. Subsequent relaxation occurs during the diastolic repolarization phase. The normal course of ST segment reflects a certain sequence of muscular layers undergoing repolarization and certain timing of this activity. When the cardiac muscle is damaged or undergoes a pathological process (e.g. inflammation), its contractile and electrical properties change. Usually, this leads to early repolarization, or premature ending of the systole.
The exact topology and distribution of the affected areas depend on the underlying condition. Thus, ST elevation may be present on all or some leads of ECG.
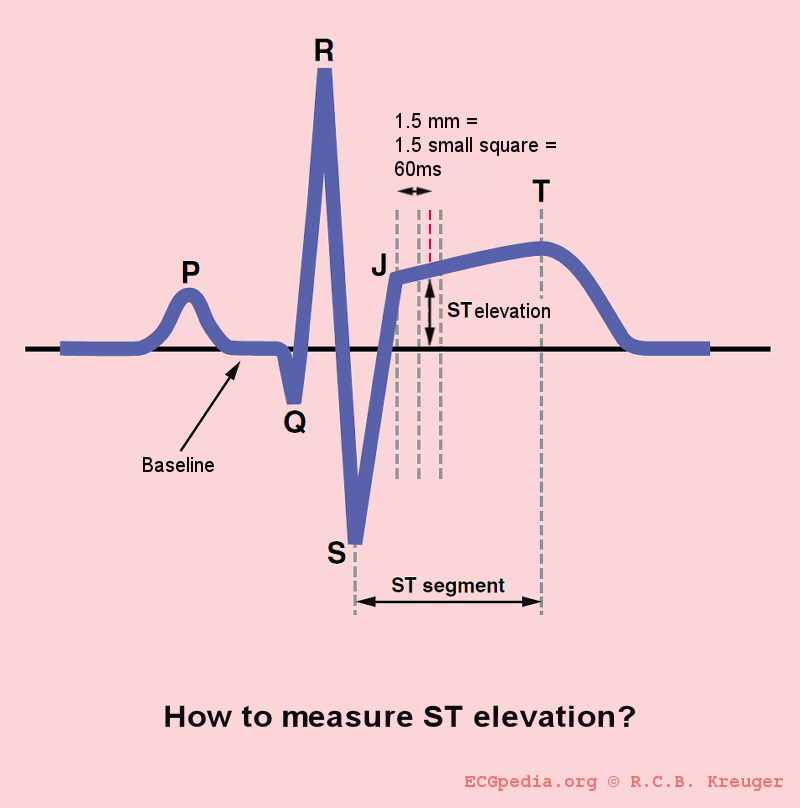
Measurement
The optimal time after the J point to measure ST elevation is debated. This example shows the technique of measuring the magnitude of ST elevation 60 milliseconds or 1.5 small boxes after the J point.[11]
Causes
Common Causes
Causes in Alphabetical Order
- Acute MI or heart attack
- Brugada syndrome
- Coronary vasospasm
- Early repolarization
- Hyperkalemia and this is known as a dialyzable current of injury
- Intracranial hemorrhage
- Left bundle branch block
- Left ventricular aneurysm
- Pericardiocentesis with contact of the needle with the myocardium creating a current of injury
- Pericarditis[12][13]
- Prinzmetal's angina
- Pulmonary embolism
- Short QT syndrome (some variants)
- Vasospastic angina
Differentiating the Causes of ST Segment Elevation
Myocardial Injury
- The ST elevation is usually localized to an anatomic distribution that follows the coronary arteries (e.g. leads II,III, aVF).
- In the setting of myocardial injury, "reciprocal changes" representing ischemia in other leads or a mirror like effect of the ST elevation presenting as ST depression in other leads, may be present. For example, ST elevation in the anterior leads in acute MI may be accompanied by ST depression in the inferior leads.
- Prinzmetal's angina can cause transient ST elevation during chest pain.
- Contact of the needle can cause a "current of injury" and ST segment elevation during pericardiocentesis.
Pericarditis
- There is diffuse ST segment elevation (usually flat or concave up) together with PR segment depression. ST elevation reflects inflammation of the ventricular subepicardial layer and PR segment depression reflects inflammation of the atrial subepicardial layer.
- T wave inversion can be seen in pericarditis but usually not until the ST elevation has resolved, so *T wave inversion accompanying ST elevation is probably not due to pericarditis
Hyperkalemia
Hyperkalemia may not affect all leads.
Ventricular Aneurysm
- Ventricular aneurysm should be suspected if the ST segment elevation persists > 6 weeks after acute MI and if there is a wall motion abnormality on echocardiography.
Early Repolarization
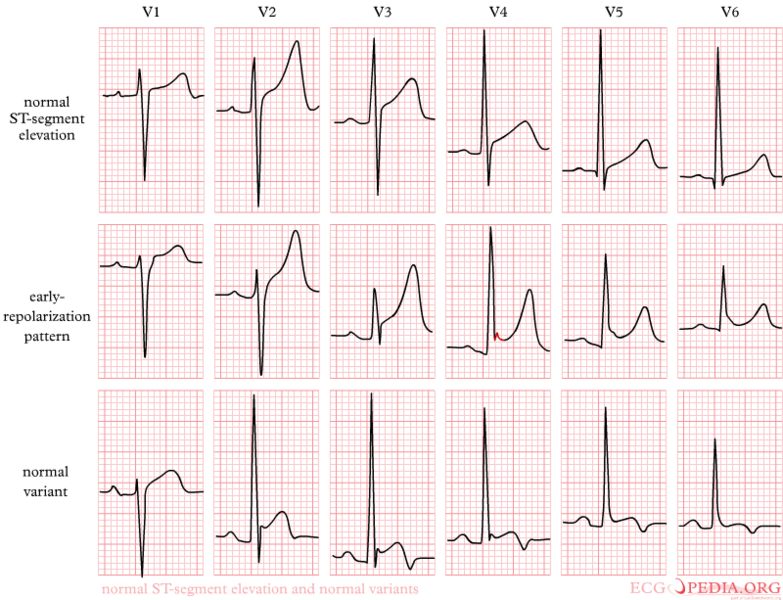
- "J point" elevation aka "early repolarization" is a concave-upward ST segment deflection.
- Vaulting ST segment or J point elevation is a normal variant in leads V1-V3.
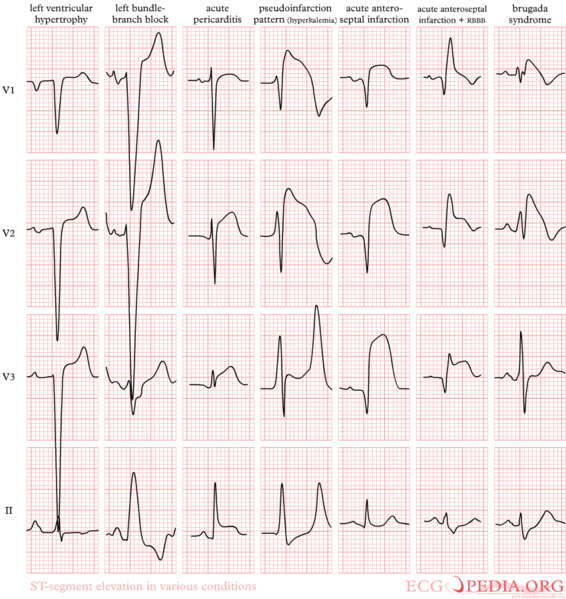
Differentiating the Causes of ST Segment Elevation EKG Examples
Shown below is an example of EKG illustrating ST elevation in various pathological states.
Shown below is an example of an EKG showing early repolarization ST elevation and normal ST elevation variants.
Shown below is a example of an ECG demonstrating early repolarization ST changes.

References
- ↑ Hammill S. C. Electrocardiographic diagnoses: Criteria and definitions of abnormalities, Chapter 18, MAYO Clinic, Concise Textbook of Cardiology, 3rd edition, 2007 ISBN 0-8493-9057-5
- ↑ Braunwald, Eugene; Zipes, Douglas P. (2005). Braunwald's heart disease: a textbook of cardiovascular medicine. St. Louis, Mo: Elsevier Saunders. ISBN 0-8089-2305-6.
- ↑ Wong C-K, French JK, Aylward PEG, Stewart RAH, Gao W, Armstrong PW, Van De Werf FJJ, Simes RJ, Raffel OC, Granger CB, Califf RM, White HD. Patients with prolonged ischemic chest pain and presumed-new left bundle branch block have heterogenous outcomes depending on the presence of ST-segment changes. J Am Coll Cardiol. 2005;46:29–38. PMID 15992631
- ↑ Sgarbossa EB, Pinsky SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM, Wagner GS. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle branch block. N Engl J Med. 1996;334:481–87. PMID 8559200
- ↑ Mcfarlane PW. Age, sex, and the ST amplitude in health and disease. J Electrocardiol. 2001; 34: 235–241. PMID 11781962
- ↑ Tsuka Y, Sugiura T, Hatada K, Nakamura S, Yuasa F, Iwasaka T (2001). "Clinical significance of ST-segment elevation in lead V1 in patients with acute inferior wall Q-wave myocardial infarction". Am Heart J. 141 (4): 615–20. doi:10.1067/mhj.2001.113996. PMID 11275929.
- ↑ Klein HO, Tordjman T, Ninio R, Sareli P, Oren V, Lang R; et al. (1983). "The early recognition of right ventricular infarction: diagnostic accuracy of the electrocardiographic V4R lead". Circulation. 67 (3): 558–65. PMID 6821897.
- ↑ Gibson CM, Chen M, Angeja BG, Murphy SA, Marble SJ, Barron HV; et al. (2002). "Precordial ST-segment depression in inferior myocardial infarction is associated with slow flow in the non-culprit left anterior descending artery". J Thromb Thrombolysis. 13 (1): 9–12. PMID 11994554.
- ↑ Pride YB, Tung P, Mohanavelu S, Zorkun C, Wiviott SD, Antman EM; et al. (2010). "Angiographic and clinical outcomes among patients with acute coronary syndromes presenting with isolated anterior ST-segment depression: a TRITON-TIMI 38 (Trial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet Inhibition With Prasugrel-Thrombolysis In Myocardial Infarction 38) substudy". JACC Cardiovasc Interv. 3 (8): 806–11. doi:10.1016/j.jcin.2010.05.012. PMID 20723851.
- ↑ Norell MS, Lyons JP, Gardener JE, Layton CA, Balcon R (1989). "Significance of "reciprocal" ST segment depression: left ventriculographic observations during left anterior descending coronary angioplasty". J Am Coll Cardiol. 13 (6): 1270–4. PMID 2522957.
- ↑ Gibbons RJ, Balady GJ, Bricker JT, Chaitman BR, Fletcher GF, Froelicher VF; et al. (2002). "ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines)". Circulation. 106 (14): 1883–92. PMID 12356646.
- ↑ 12.0 12.1 Tingle LE, Molina D, Calvert CW (2007). "Acute pericarditis". Am Fam Physician. 76 (10): 1509–14. PMID 18052017. Unknown parameter
|month=ignored (help) - ↑ 13.0 13.1 Chew HC, Lim SH (2005). "Electrocardiographical case. ST elevation: is this an infarct? Pericarditis" (PDF). Singapore Med J. 46 (11): 656–60. PMID 16228101. Unknown parameter
|month=ignored (help)