Atrial fibrillation: Difference between revisions
No edit summary |
No edit summary |
||
| Line 32: | Line 32: | ||
===[[Atrial fibrillation overview|Overview]]=== | ===[[Atrial fibrillation overview|Overview]]=== | ||
===[[Atrial fibrillation epidemiology|Epidemiology]]=== | ===[[Atrial fibrillation epidemiology|Epidemiology]]=== | ||
==Diagnosis== | |||
===[[Atrial fibrillation classification|Classification]]=== | |||
===[[Atrial fibrillation differential diagnosis| Differential Diagnosis]]=== | |||
==Classification== | ==Classification== | ||
| Line 69: | Line 73: | ||
Lone [[atrial fibrillation]] is defined as [[atrial fibrillation]] in the absence of clinical or echocardiographic findings of cardiopulmonary disease including [[hypertension]].<ref name="pmid16908781"/> Patients in this group are young individuals (less than 60 years old). | Lone [[atrial fibrillation]] is defined as [[atrial fibrillation]] in the absence of clinical or echocardiographic findings of cardiopulmonary disease including [[hypertension]].<ref name="pmid16908781"/> Patients in this group are young individuals (less than 60 years old). | ||
==Pathophysiology== | ==Pathophysiology== | ||
| Line 188: | Line 180: | ||
==The autonomic nervous system may trigger [[AF]] in susceptible patients through heightened vagal or adrenergic tone== | ==The autonomic nervous system may trigger [[AF]] in susceptible patients through heightened vagal or adrenergic tone== | ||
===Morphology=== | ===Morphology=== | ||
Revision as of 15:01, 15 June 2009
| Conduction | ||
Sinus rhythm  |
Atrial fibrillation  | |
| Atrial fibrillation | |
 | |
|---|---|
| The P waves, which represent depolarization of the atria, are irregular or absent during atrial fibrillation. | |
| ICD-10 | I48 |
| ICD-9 | 427.31 |
| DiseasesDB | 1065 |
| MedlinePlus | 000184 |
| eMedicine | med/184 emerg/46 |
| Cardiology Network |
 Discuss Atrial fibrillation further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Synonyms and related keywords: AF, Afib, fib
Overview
Overview
Epidemiology
Diagnosis
Classification
Differential Diagnosis
Classification
Although several clinical classification plans and protocols have been proposed, none of them fully account for all aspects of atrial fibrillation. The American Heart Association, American College of Cardiology, and the European Society of Cardiology have proposed the following classification system based on simplicity and clinical relevance:[1]
| AF Category | Defining Characteristics |
|---|---|
| First detected | only one diagnosed episode |
| Paroxysmal | recurrent episodes that self-terminate in less than 7 days |
| Persistent | recurrent episodes that last more than 7 days |
| Permanent | an ongoing long-term episode |
First detected atrial fibrillation
Any patient with new diagnosed AF is in this category, as the exact onset and chronicity of the disease is often uncertain.
Recurrent atrial fibrillation
Two or more identified episodes of atrial fibrillation are named as recurrent form of atrial fibrillation. This is further classified into paroxysmal and persistent based on when the episode terminates without therapy. Atrial fibrillation is said to be paroxysmal when it terminates spontaneously within 7 days, most commonly within 24 hours.
The term 'Persistent' or 'chronic' is used if diagnosis of atrial fibrillation established for more than seven days. Differentiation of paroxysmal from chronic or established AF is based on the history of recurrent episodes and the duration of the current AF episode.[1][2][3]
Lone atrial fibrillation (LAF)
Lone atrial fibrillation is defined as atrial fibrillation in the absence of clinical or echocardiographic findings of cardiopulmonary disease including hypertension.[1] Patients in this group are young individuals (less than 60 years old).
Pathophysiology
Etiology of atrial fibrillation
AF can be associated with underlying cardiac diseases, but it may also occur in otherwise normal hearts.
Common Causes
Complete Differential Diagnosis of Underlying Etiologies for Atrial Fibrillation
| Cardiovascular | Acute myocardial infarction • Congenital heart disease especially atrial septal defect in adults • Coronary artery disease • Heart failure (especially diastolic dysfunction and diastolic heart failure) • Hypertrophic cardiomyopathy (HCM) • Hypertension • Mitral regurgitation
Mitral stenosis (e.g. due to Rheumatic heart disease or Mitral valve prolapse) • Myocarditis • Pericarditis • Previous heart surgery • Dual-chamber pacemakers in the presence of normal atrioventricular conduction.[4] • Restrictive cardiomyopathies (such as amyloidosis, hemochromatosis, and endomyocardial fibrosis), cardiac tumors, and constrictive pericarditis |
| Congenital | |
| Dermatologic | No underlying causes |
| Drugs | Digoxin in patients with vagally mediated AF |
| Ear Nose Throat | No underlying causes |
| Endocrine | Hyperthyroidism • Hypothyroidism • Pheochromocytoma |
| Gastroenterologic | Vomiting |
| Genetic | A family history of AF increases risk by 30%.[5] Various genetic mutations may be responsible.[6] |
| Hematologic | No underlying causes |
| Infectious Disease | No underlying causes |
| Musculoskeletal / Ortho | No underlying causes |
| Neurologic | Multiple sclerosis |
| Nutritional / Metabolic | No underlying causes |
| Oncologic | No underlying causes |
| Opthalmologic | No underlying causes |
| Overdose / Toxicity | Excessive alcohol consumption ("binge drinking" or "holiday heart syndrome") • Carbon monoxide poisoning • Caffeine • Stimulants |
| Post-Op Complication | Surgery,particularly coronary artery bypass surgery • During pulmonary artery line placement and right heart catheterization trauma to the right atrium can result in atrial fibrillation |
| Pulmonary | Hypoxia of any cause • Lung cancer • Pneumonia • Pulmonary embolism • Sarcoidosis • sleep apnea syndrome |
| Renal / Electrolyte | Hypokalemia |
| Rheum / Immune / Allergy | No underlying causes |
| Trauma | Electrocution • Cardiac contusion |
| Miscellaneous | Hypothermia • Fever |
The autonomic nervous system may trigger AF in susceptible patients through heightened vagal or adrenergic tone
Morphology
The primary pathologic change seen in atrial fibrillation is the progressive fibrosis of the atria. This fibrosis is primarily due to atrial dilatation, however genetic causes and inflammation may have a cause in some individuals.
Dilatation of the atria can be due to almost any structural abnormality of the heart that can cause a rise in the intra-cardiac pressures. This includes valvular heart disease (such as mitral stenosis, mitral regurgitation, and tricuspid regurgitation), hypertension, and congestive heart failure. Any inflammatory state that affects the heart can cause fibrosis of the atria. This is typically due to sarcoidosis but may also be due to autoimmune disorders that create autoantibodies against myosin heavy chains. Mutation of the lamin AC gene is also associated with fibrosis of the atria that can lead to atrial fibrillation.
Once dilatation of the atria has occurred, this begins a chain of events that leads to the activation of the renin aldosterone angiotensin system (RAAS) and subsequent increase in matrix metaloproteinases and disintegrin, which leads to atrial remodeling and fibrosis, with loss of atrial muscle mass.
This process is not immediate, and experimental studies have revealed patchy atrial fibrosis may precede the occurrence of atrial fibrillation and may progress with prolonged durations of atrial fibrillation.
Fibrosis is not limited to the muscle mass of the atria, and may occur in the sinus node (SA node) and atrioventricular node (AV node), correlating with sick sinus syndrome. Prolonged episodes of atrial fibrillation have been shown to correlate with prolongation of the sinus node recovery time,[1] [7][8] suggesting that dysfunction of the SA node is progressive with prolonged episodes of atrial fibrillation.
Signs and symptoms
In general, clinical manifestations are;
- Palpitations
- Chest pain
- Dyspnea
- Fatigue
- Lightheadedness
- Syncope: Syncope is an uncommon but serious complication that is usually associated with sinus node dysfunction or hemodynamic obstruction, such as valvular aortic stenosis, HCM, cerebrovascular disease, or an accessory AV pathway.
Atrial fibrillation is usually accompanied by symptoms related to the rapid heart rate. Rapid and irregular heart rates may be perceived as palpitations, exercise intolerance, and occasionally produce angina (if the rate is faster and puts the heart under strain) and congestive symptoms of shortness of breath or edema. Sometimes the arrhythmia will be identified only with the onset of a stroke or a transient ischemic attack (TIA, stroke symptoms resolving within 24 hours). It is not uncommon to identify atrial fibrillation on a routine physical examination or electrocardiogram (ECG/EKG), as it may be asymptomatic in many cases.[1]
As most cases of atrial fibrillation are secondary to other medical problems, the presence of chest pain or angina, symptoms of hyperthyroidism (an overactive thyroid gland) such as weight loss and diarrhea, and symptoms suggestive of lung disease would indicate an underlying cause. A previous history of stroke or TIA, as well as hypertension (high blood pressure), diabetes, heart failure and rheumatic fever, may indicate whether someone with atrial fibrillation is at a higher risk of complications.[1]
Diagnosis of atrial fibrillation
The evaluation of atrial fibrillation involves diagnosis, determination of the etiology of the arrhythmia, and classification of the arrhythmia. A minimal evaluation performed should be performed in all individuals with atrial fibrillation. This includes a history and physical examination, surface electrocardiogram, transthoracic echocardiogram, and routine blood work. Certain individuals may benefit from an extended evaluation which may include an evaluation of the heart rate response to exercise, exercise stress testing, a chest x-ray, trans-esophageal echocardiography, and other studies.
- Screening and routine primary care visit for atrial fibrillation
- History and physical examination for atrial fibrillation
- Electrocardiogram for diagnosis of atrial fibrillation
- Chest x-ray for diagnosis of atrial fibrillation
- Echocardiography for diagnosis of atrial fibrillation
- Recorders (Holter monitors) for diagnosis of atrial fibrillation
- Exercise stress tests (Tilt-Table Test) for diagnosis of atrial fibrillation
- Electrophysiologic Testing or Electrophysiologic Studies for diagnosis of atrial fibrillation
Screening and routine primary care visit
Screening for atrial fibrillation is not generally performed, although a study of routine pulse checks or electrocardiograms during routine office visits, found that the annual rate of detection of atrial fibrillation in elderly patients improved from 1.04% to 1.63%; selection of patients for prophylactic anticoagulation would improve stroke risk in that age category.[9]
Estimated sensitivity of the routine primary care visit is 64%. This low result probably reflects the pulse not being checked routinely or carefully.[9]
History and physical examination for atrial fibrillation
The history of the individual's atrial fibrillation episodes is likely the most important part of the evaluation. Distinctions should be made to those who are entirely asymptomatic when they are in atrial fibrillation (in which case the atrial fibrillation is found as an incidental finding on an electrocardiogram or physical examination) and those who have gross and obvious symptoms due to atrial fibrillation and can pinpoint whenever they go into atrial fibrillation and revert to sinus rhythm.
Detailed history and physical examination are essential to define;
- The presence and nature of symptoms associated with AF
- The clinical type of AF (first episode, paroxysmal, persistent, or permanent)
- The onset of the first symptomatic attack or date of discovery of AF
- The frequency, duration, precipitating factors, and modes of termination of AF
- The response to any pharmacological agents that have been administered
- The presence of any underlying heart disease or other reversible conditions (e.g., hyperthyroidism or alcohol consumption)
Routine blood work
While many cases of AF have no definite cause, it may be the result of various other problems (Blood tests of thyroid function are required, especially for a first episode of AF, when the ventricular rate is difficult to control, or when AF recurs unexpectedly after cardioversion)
Hence, renal function and electrolytes are routinely determined, as well as thyroid-stimulating hormone (commonly suppressed in hyperthyroidism and of relevance if amiodarone is administered for treatment) and a blood count.[1]
In acute-onset AF associated with chest pain, cardiac troponins or other markers of damage to the heart muscle may be ordered. Coagulation studies (INR/aPTT) are usually performed, as anticoagulant medication may be commenced.[1]
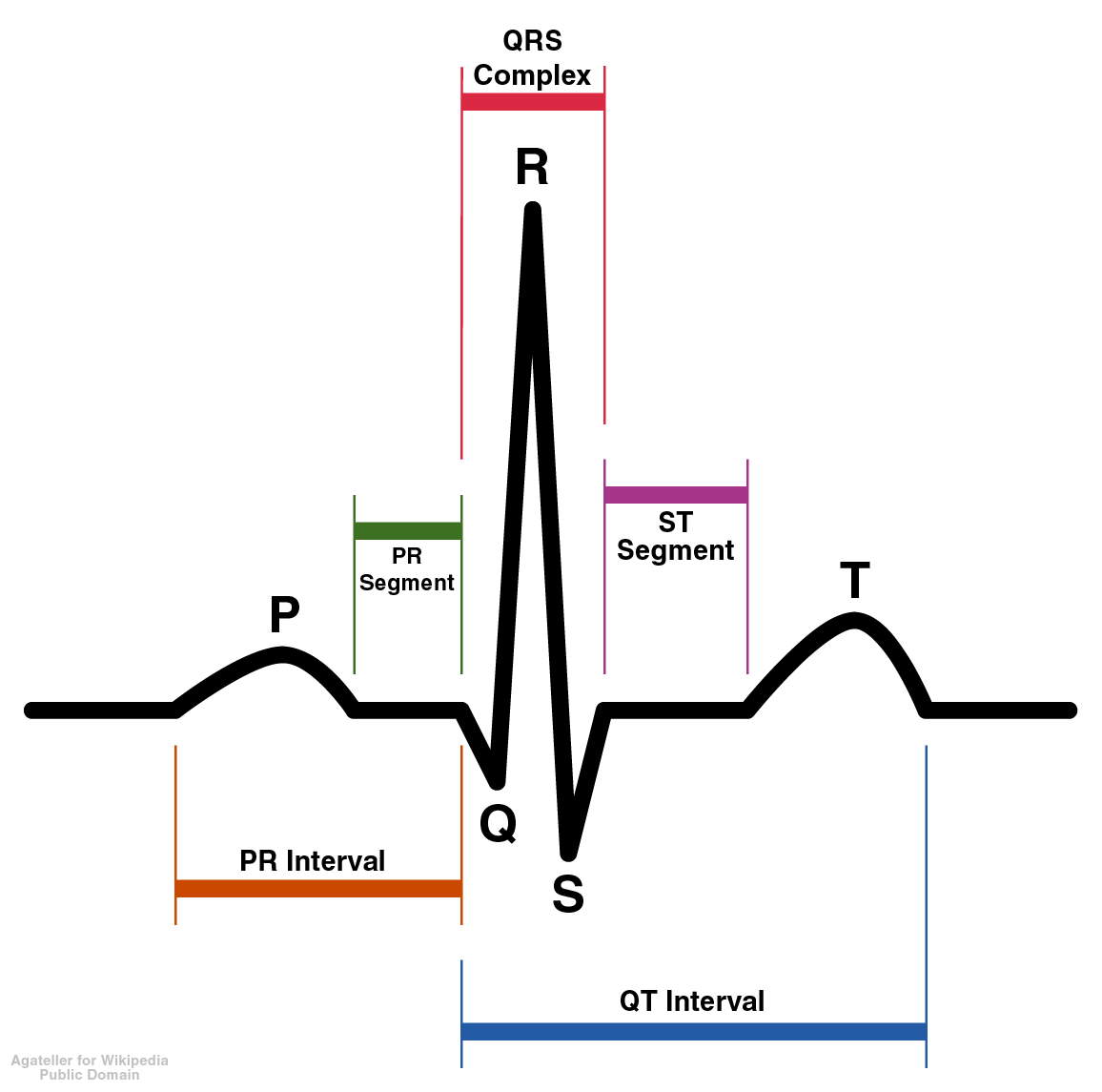
Electrocardiogram

Atrial fibrillation is diagnosed on an electrocardiogram, an investigation performed routinely whenever irregular heart beat is suspected. Characteristic findings are the absence of P waves, with unorganized electrical activity in their place, and irregularity of R-R interval due to irregular conduction of impulses to the ventricles.[1]
EKG is helpful to identify;
- Rhythm (verify AF)
- LV hypertrophy
- P-wave duration and morphology or fibrillatory waves
- Preexcitation
- Bundle-branch block
- Prior MI
- Other atrial arrhythmias
- To measure and follow the RR, QRS, and QT intervals in conjunction with antiarrhythmic drug therapy
Summary of Electrocardiographic findings
- Absent P waves
- Irregularly irregular ventricular response rate. Regular RR intervals are possible in the presence of AV block or interference due to ventricular or junctional tachycardia.
- An atrial rate that ranges from 400 to 700 BPM.
- sometimes V1 may look as though there is atrial flutter. This may be because the electrode overlies a portion of the RA with rhythmic activity.
- Some authors believe that fine f waves (<.5 mm) are associated with coronary artery disease and that coarse F waves are associated with LA enlargement and rheumatic heart disease.
- the ventricular rate is usually between 100 and 180 BPM.
- if the atrial rate is greater than 200 BPM, then consider WPW or an accessory pathway.
- In the presence of AV junctional disease, the ventricular rate may be below 70 bpm.
- a rapid, irregular, sustained, wide-QRS-complex tachycardia strongly suggests AF with conduction over an accessory pathway or AF with underlying bundle-branch block.
- Complete AV block is indicated by a slow ventricular rhythm with a regular RR interval.
- In patients with electronic pacemakers, diagnosis of AF may require temporary inhibition of the pacemaker to expose atrial fibrillatory activity.
- Differential diagnosis includes tremor due to artifact. The oscillations in this case are largest in the limb leads.
When electrocardiograms are used for screening? The SAFE trial found that electronic software, primary care physicians and the combination of the two had the following sensitivities and specificities:[10]:
- Interpreted by software: sensitivity = 83%, specificity = 99%
- Interpreted by a primary care physician: sensitivity = 80%, specificity = 92%
- Interpreted by a primary care physician with software: sensitivity = 92%, specificity = 91%
If paroxysmal AF is suspected but the electrocardiogram shows a regular rhythm, episodes may be documented with the use of Holter monitoring (continuous ECG recording for 24 hours). If the symptoms are very infrequent, longer periods of continuous monitoring may be required.[1]
Chest X-ray
A chest X-ray is generally only performed if a pulmonary cause of atrial fibrillation is suggested. This may reveal an underlying problem in the lungs or the blood vessels in the chest. [1] In particular, if an underlying pneumonia is suggested, then treatment of the pneumonia may cause the atrial fibrillation to terminate on its own.
As a summary a chest radiograph is required to evaluate;
- The lung parenchyma, when clinical findings suggest an abnormality
- The pulmonary vasculature, when clinical findings suggest an abnormality
Echocardiography
Performing an echocardiogram is essential to identify;
- Valvular heart disease
- Left and right atrial size
- LV size and function
- Peak RV pressure (pulmonary hypertension)
- LV hypertrophy
- LA thrombus (low sensitivity)
- Pericardial disease
Transthoracic echocardiography (TTE)
A transthoracic echocardiogram is generally performed in newly diagnosed AF, as well as if there is a major change in the patient's clinical state. This ultrasound-based scan of the heart may help identify valvular heart disease (which may increase the risk of stroke manifold), left and right atrial size (which indicates likelihood that AF may become permanent), left ventricular size and function, peak right ventricular pressure (pulmonary hypertension), presence of left ventricular hypertrophy and pericardial disease.[1]
Significant enlargement of both the left and right atria is associated with long-standing atrial fibrillation and, if noted at the initial presentation of atrial fibrillation, suggests that the atrial fibrillation is likely of a longer duration than the individual's symptoms.
Transesophageal echocardiography (TEE)
A normal echocardiography (transthoracic or TTE) has a low sensitivity for identifying thrombi (blood clots) in the heart. If this is suspected - e.g. when planning urgent electrical cardioversion - a transesophageal echocardiogram (TEE) is preferred.[1]
The TEE has much better visualization of the left atrial appendage than transthoracic echocardiography. This structure, located in the left atrium, is the place where thrombus most commonly is formed in the setting of atrial fibrillation or flutter. TEE has a very high sensitivity for locating thrombus in this area and can also detect sluggish bloodflow in this area that is suggestive of thrombus formation.
If no thrombus is seen on TEE, the incidence of stroke immediately after cardioversion is performed is very low.
Ambulatory Holter monitoring
A holter monitor is a wearable ambulatory heart monitor that continuously monitors the heart rate and heart rhythm for a short duration, typically 24 hours. In individuals with symptoms of significant shortness of breath with exertion or palpitations on a regular basis, a holter monitor may be of benefit to determine if rapid heart rates (or unusually slow heart rates) during atrial fibrillation are the cause of the symptoms.
Exercise stress testing
Some individuals with atrial fibrillation do well with normal activity but develop shortness of breath with exertion. It may be unclear if the shortness of breath is due to a blunted heart rate response to exertion due to excessive AV node blocking agents, a very rapid heart rate during exertion, or due to other underlying conditions such as chronic lung disease or coronary ischemia. An exercise stress test will evaluate the individual's heart rate response to exertion and determine if the AV node blocking agents are contributing to the symptoms. As a summary the main benefits of performing an exercise stress testing;
- If the adequacy of rate control is in question (permanent AF)
- To reproduce exercise-induced AF
- To exclude ischemia before treatment of selected patients with a type IC antiarrhythmic drug
Electrophysiologic Testing or Electrophysiologic Studies
Treatment of atrial fibrillation
- Pharmacological treatment
- Invasive treatment
- Surgical treatment
Pharmacological treatment of atrial fibrillation
The main goals of treatment of atrial fibrillation are to prevent temporary circulatory instability and to prevent stroke. Rate and rhythm control are principally used to achieve the former, while anticoagulation may be required to decrease the risk of the latter.[11] In emergencies, when circulatory collapse is imminent due to uncontrolled tachycardia, immediate cardioversion may be indicated.[1]
The primary factors determining atrial fibrillation treatment are duration and evidence of hemodynamic instability. Cardioversion is indicated with new onset AF (for less than 48 hours) and with hemodynamic instability. If rate and rhythm control cannot be maintained by medication or cardioversion, electrophysiological studies with pathway ablation may be required.[1]
Antithrombotic Strategies for Prevention of Ischemic Stroke and Systemic Embolism
Oral anticoagulation is a mainstay of atrial fibrillation management. For both primary and secondary prevention of stroke, there is a 61% relative risks reduction in the incidence of all cause stroke (both ischemic and hemorrhagic) associated with adjusted-dose oral anticoagulation.[12]
Increasing patient age (which is associated with smaller body weight, female gender and a progressive decline in renal function) and higher INRs or greater intensity of anticoagulation are both associated with a higher risk of major bleeding. This is critical in so far as bleeding is in turn associated with non-compliance with pharmacotherapy. [12][13][14] [12][15] Given that many patients with atrial fibrillation are elderly, there is often a narrow therapeutic window in achieving the optimal INR. The optimal INR should obviously maximize efficacy in reducing the risk of stroke and simultaneously minimize the risk of bleeding. In the setting of atrial fibrillation, an INR of 2 to 3 appears to be optimal. INRs lower than this, such as those in the range of 1.6 to 2.5, are associated with efficacy that is only 80% of that in the target range.[16][17] [18][19]
Interruption of anticoagulation with coumadin
No mechanical valve, high risk of bleeding with procedure: Coumadin can be discontinued for one week without heparin bridging.
Presence of mechanical valve, patients with AF who are at high risk of stroke, or patients in whom Coumadin must be interrupted for over a week: These patients should be administered either unfractionated heparin or low molecular weight heparin.
Investigational antithrombin agents
Newer agents that inhibit factor Xa are under investigation for the management of atrial fibrillation. These agents include apixabin and rivaroxaban.
Antiplatelet therapy for atrial fibrillation
Aspirin Monotherapy
Aspirin monotherapy is associated with only a modest and inconsistent reduction in the risk of stroke associated with atrial fibrillation. [19] [19]
[20] Studies suggest that the efficacy of aspirin may be greater in patients with hypertension or diabetes. Aspirin may also be more efficacious in reducing the risk of non cardioembolic stroke as opposed to the more disabling cardioembolic form of stroke. [21][22]
Dual Antiplatelet therapy
Among patients who are not deemed candidates for Coumadin therapy (estimated to be approximately 40-50% of patients), dual antiplatelet therapy with both aspirin and clopidogrel (at a maintenance dose of 75 mg/day) was superior to aspirin monotherapy in the ACTIVE A trial. The primary endpoint of the trial was the composite of stroke, myocardial infarction, non–central nervous system systemic embolism, or death from vascular causes. After a median of 3.6 years of follow-up in 7,554 randomized patients, the addition of clopidogrel to aspirin alone yielded a reduction in events from 7.6% to 6.8% (relative risk reduction with clopidogrel, 0.89; 95% confidence interval [CI], 0.81 to 0.98; P=0.01). The addition of clopidogrel to aspirin alone reduced the risk of stroke by 28% (from 3.3% to 2.4%, p<0.001) and reduced the risk of MI by 22% (from 0.9% per year to 0.7% per year, p=0.08). The risk of major bleeding among patients treated with aspirin and clopidogrel was 2.0% per year whereas it was 1.3% per year among patients treated with aspirin alone (relative risk, 1.57; 95% CI, 1.29 to 1.92; P<0.001). If 1000 patients were treated for 3 years, the combination of aspirin plus clopidogrel would prevent 28 strokes (17 disabling or fatal), and 6 myocardial infarctions, at a cost of 20 major bleeds compared to aspirin alone.
Oral Anticoagulation (Coumadin) versus Dual Antiplatelet Therapy (ASA/Clopidogrel)
In the ACTIVE W trial, dual antiplatelet therapy with aspirin(75-100 mg per day) and clopidogrel (75 mg per day) was found to be statistically inferior to coumadin therapy (target INR 2.0 to 3.0) in the management of patients with atrial fibrillation who had one or more risk factors for stroke[23]. The primary endpoint of ACTIVE W was the first occurrence of stroke, non-CNS systemic embolus, myocardial infarction, or vascular death. The annual risk in the coumadin group was 3.93% per year, and in the Aspirin/Clopidogrel group it was 5.60% per year yielding a relative risk of 1.44 (1.18-1.76; p=0.0003). The efficacy was not as great among patients who were coumadin naive, although the p-value for the interaction was negative. There was no excess bleeding among patients treated with coumadin, and in fact there was an excess of minor bleeds among patients treated with ASA and clopidogrel (13.6% / yr vs 11.5% year, p=0.0009).
When examining the data from atrial fibrillation trials, it is critical to evaluate the results in patients who were previously treated with coumadin separate from those patients who were naive to coumadin. Patients previously treated with coumadin are likely to be those patients who best tolerate coumadin and have passed their "bleeding stress test" and have a lower rate of bleeding on coumadin. Those patients who bleed while on coumadin have already been culled out from the population. When the data in ACTIVE W were evaluated including only those patients previously treated with coumadin(again a population to be anticipated to be at low risk of bleeding), the risk of major bleeding was indeed statistically significantly lower among patients previously treated with coumadin (p=0.03) than patients not previously treated.
The majority of the reduction in events was due to a reduction in stroke and non-CNS emolization associated with [[coumadin therapy. The pathophysiology of stroke among patients with atrial fibrillation is thought to be embolization from clot in the left atrium. The data from ACTIVE W suggest that platelet activation and its treatment may not play a pivotal role in the treatment of mural thrombus and embolization in atrial fibrillation. Coumadin was more effective in the reduction of non-disabling stroke rather than disabling stroke. There were more fatal hemorrhagic strokes (which may more often be fatal), and this may explain in part why coumadin was not associated with a reduction in mortality in the study.
While clopidogrel plus aspirin has been found to reduce the risk of recurrent myocardial infarction among patients with presumed plaque rupture and acute coronary syndromes, it is notable in ACTIVE W that the risk of myocardial infarction tended to be higher among patients treated with aspirin plus clopidogrel versus coumadin (0.86% vs 0.55%,p=0.09)[24].
Conversion to sinus rhythm and thromboembolism
Electrical & mechanical dissociation
Despite the restoration of sinus rhythm on the ECG following cardioversion (either spontaneous, pharmacologic or electrical or after radiofrequency catheter ablation of atrial flutter), in some patients there is a persistent lack of atrial contractility. This state is known as electrical mechanical dissociation and may be sue to mechanical stunning in the atrium and the atrial appendage. [25] [26][27][27][28][29][30] The lack of atrial contraction can be diagnosed on echocardiography by the appearance of spontaneous echo contrast. [25] In general, the longer the patient was in atrial fibrillation, the longer the time it takes for the recoery of atrial mechanical function. The period of recovery can be quite variable, and it can take several weeks in total. Recovery of mechanical function can be delayed for several weeks, depending in part on the duration of AF before restoration of sinus rhythm[31][32][33] This kind of electrical mechanical dissociation may explain in part the observation that some patients develop thromboembolic events following cardioversion despite the fact that they had no visible left atrial clot on TEE. [34] It has been hypothesized that the low shear state and turbulent nature of left atrial hemodynamics during this period leads to the development of clot which then embolizes once there is restoration of sufficient mechanical force.[35] It is in part due to the presence of atrial mechanical dissociation and the risk of clot formation and embolization that oral anticoagulation is recommended for 3 to 4 weeks following successful electrical cardioversion in patients in whom the duration of Afib is unknown or in whom the duration of atrial fibrillation has been documented to be longer than 48 hours. Among patients in whom the duration of atrial fibrillation is less than 48 hours, the necessity for anticoagulation is not as clear, although it should be noted that stroke has been observed in these patients as well. No matter what the duration of atrial fibrillation, if a patient becomes hemodynamically unstable, this is an indication for immediate cardioversion.
Management Strategies
New diagnosed or First Episode of Atrial Fibrillation
In patients who have self-limited episodes of paroxysmal AF, antiarrhythmic drugs to prevent recurrence are usually unnecessary, unless AF is associated with severe symptoms related to hypotension, myocardial ischemia, or HF. Whether these individuals require longterm or even short-term anticoagulation is not clear, and the decision must be individualized for each patient based on the intrinsic risk of thromboembolism.
Persistent Atrial Fibrillation
Recurrent Paroxysmal Atrial Fibrillation
Vagally mediated Atrial fibrillation
Adrenergically induced Atrial Fibrillation
Beta blockers (sotalol)
Congestive Heart Failure
amiodarone or dofetilide to maintain sinus rhythm.
Ischemic heart disease
Hypertension without LVH
Left ventricular hypertrophy
ACC / AHA Guidelines- Recommendation for Pacing to Prevent Atrial Fibrillation (DO NOT EDIT) [36]
| “ |
Class III1. Permanent pacing is not indicated for the prevention of AF in patients without any other indication for pacemaker implantation. (Level of Evidence: B) |
” |
Sources
- The ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities [36]
Recurrent Persistent AF
Permanent AF
Anticoagulation
Patients with atrial fibrillation, even lone atrial fibrillation without other evidence of heart disease, are at increased risk of stroke during long term follow up.[37] A systematic review of risk factors for stroke in patients with nonvalvular atrial fibrillation concluded that a prior history of stroke or TIA is the most powerful risk factor for future stroke, followed by advancing age, hypertension, diabetes.[38] The risk of stroke increases whether the lone atrial fibrillation was an isolated episode, recurrent, or chronic.[39] The risk of systemic embolization (atrial clots migrating to other organs) depends strongly on whether there is an underlying structural problem with the heart (e.g. mitral stenosis) and on the presence of other risk factors, such as diabetes and high blood pressure. Finally, patients under 65 are much less likely to develop embolization compared with patients over 75. In young patients with few risk factors and no structural heart defect, the benefits of anticoagulation may be outweighed by the risks of hemorrhage (bleeding). Those at a low risk may benefit from mild (and low-risk) anticoagulation with aspirin (or clopidogrel in those who are allergic to aspirin). In contrast, those with a high risk of stroke derive most benefit from anticoagulant treatment with warfarin or similar drugs.
In the United Kingdom, the NICE guidelines recommend using a clinical prediction rule for this purpose.[40] The CHADS/CHADS2 score is the best validated clinical prediction rule for determining risk of stroke (and therefore who should be anticoagulated); it assigns points (totaling 0-6) depending on the presence or absence of co-morbidities such hypertension and diabetes. In a comparison of seven prediction rules, the best rules were the CHADS2 which performed similarly to the SPAF[41] and Framingham[42] prediction rules. [43]
To compensate for the increased risk of stroke, anticoagulants may be required. However, in the case of warfarin, if a patient has a yearly risk of stroke that is less than 2%, then the risks associated with taking warfarin outweigh the risk of getting a stroke. [44][45]
Acute anticoagulation
If anticoagulation is required urgently (e.g. for cardioversion), heparin or similar drugs achieve the required level of protection much quicker than warfarin, which may take several days to reach adequate levels.
In the initial stages after an embolic stroke, anticoagulation may be risky, as the damaged area of the brain is relatively prone to bleeding (hemorrhagic transformation).[46] As a result, a clinical practice guideline by National Institute for Health and Clinical Excellence recommends that anticoagulation should begin two weeks after stroke if no hemorrhage occurred.[40]
Chronic anticoagulation
Among patients with "non-valvular" atrial fibrillation, anticoagulation with warfarin can reduce stroke by 60% while antiplatelet agents can reduce stroke by 20%. [47][48]. There is evidence that aspirin and clopidogrel are effective when used together, but the combination is still inferior to warfarin.[49]
Warfarin treatment requires frequent monitoring with a blood test called the international normalized ratio (INR); this determines whether the correct dose is being used. In atrial fibrillation, the usual target INR is between 2.0 and 3.0 (higher targets are used in patients with mechanical artificial heart valves, many of whom may also have atrial fibrillation). A high INR may indicate increased bleeding risk, while a low INR would indicate that there is insufficient protection from stroke.
An attempt was made to find a better method of implementing warfarin therapy without the inconvenience of regular monitoring and risk of intracranial hemorrhage. A combination of aspirin and fixed-dose warfarin (initial INR 1.2-1.5) was tried. Unfortunately, in a study of AF patients with additional risk factors for thromboembolism, the combination of aspirin and the lower dose of warfarin was significantly inferior to the standard adjusted-dose warfarin (INR 2.0-3.0), yet still had a similar risk of intracranial hemorrhage.[50]
Elderly patients
The very elderly (patients aged 75 years or more) may benefit from anticoagulation provided that their anticoaguation does not increase hemorrhagic complications, which is a difficult goal. Patients aged 80 years or more may be especially susceptible to bleeding complications, with a rate of 13 bleeds per 100 person-years.[51] A rate of 13 bleeds per 100 person years would seem to preclude use of warfarin; however, a randomized controlled trial found benefit in treating patients 75 years or over with a number needed to treat of 50.[52] Of note, this study had very low rate of hemorrhagic complications in the warfarin group.
Rate control versus rhythm control
AF can cause disabling and annoying symptoms. Palpitations, angina, lassitude (weariness), and decreased exercise tolerance are related to rapid heart rate and inefficient cardiac output caused by AF. Furthermore, AF with a persistent rapid rate can cause a form of heart failure called tachycardia induced cardiomyopathy. This can significantly increase mortality and morbidity, which can be prevented by early and adequate treatment of the AF.
There are two ways to approach these symptoms: rate control and rhythm control. Rate control treatments seek to reduce the heart rate to normal, usually 60 to 100 beats per minute. Rhythm control seeks to restore the normal heart rhythm, called normal sinus rhythm. Studies suggest that rhythm control is mainly a concern in newly diagnosed AF, while rate control is more important in the chronic phase. Rate control with anticoagulation is as effective a treatment as rhythm control in long term mortality studies, the AFFIRM Trial.[53]
The AFFIRM study showed no difference in risk of stroke in patients who have converted to a normal rhythm with anti-arrhythmic treatment, compared to those who have only rate control.[53]
Rate control
Rate control is achieved with medications that work by increasing the degree of block at the level of the AV node, effectively decreasing the number of impulses that conduct down into the ventricles. This can be done with:[1]
- Beta blockers (preferably the "cardioselective" beta blockers such as metoprolol, atenolol, bisoprolol)
- Cardiac glycosides (i.e. digoxin)
- Calcium channel blockers (i.e. diltiazem or verapamil)
In addition to these agents, amiodarone has some AV node blocking effects (particularly when administered intravenously), and can be used in individuals when other agents are contraindicated or ineffective (particularly due to hypotension).
Cardioversion
Rhythm control methods include electrical and chemical cardioversion:[1]
- Electrical cardioversion involves the restoration of normal heart rhythm through the application of a DC electrical shock.
- Chemical cardioversion is performed with drugs, such as amiodarone, dronedarone[54], procainamide, ibutilide, propafenone or flecainide.
The main risk of cardioversion is systemic embolization of a thrombus (blood clot) from the previously fibrillating left atrium. Cardioversion should not be performed without adequate anticoagulation in patients with more than 48 hours of atrial fibrillation. Cardioversion may be performed in instances of AF lasting more than 48 hours if a transesophogeal echocardiogram (TEE) demonstrates no evidence of clot within the heart.[1]
Whichever method of cardioversion is used, approximately 50% of patient relapse within one year, although the continued daily use of oral antiarrhythmic drugs may extend this period. The key risk factor for relapse is duration of AF, although other risk factors that have been identified include the presence of structural heart disease, and increasing age.
Maintenance of sinus rhythm
The mainstay of maintaining sinus rhythm is the use of antiarrhythmic agents. Recently, other approaches have been developed that promise to decrease or eliminate the need for antiarrhythmic agents.
Antiarrhythmic agents
The anti-arrhythmic medications often used in either pharmacological cardioversion or in the prevention of relapse to AF alter the flux of ions in heart tissue, making them less excitable, setting the stage for spontaneous and durable cardioversion. These medications are often used in concert with electrical cardioversion.
Invasive treatment of atrial fibrillation
Radiofrequency ablation
In patients with AF where rate control drugs are ineffective and it is not possible to restore sinus rhythm using cardioversion, non-pharmacological alternatives are available. For example, to control rate it is possible to destroy the bundle of cells connecting the upper and lower chambers of the heart - the atrioventricular node - which regulates heart rate, and to implant a pacemaker instead. A more complex technique, which avoids the need for a pacemaker, involves ablating groups of cells near the pulmonary veins where atrial fibrillation is thought to originate, or creating more extensive lesions in an attempt to prevent atrial fibrillation from establishing itself.[1]
Ablation is a newer technique and has shown some promise for cases of recurrent AF that are unresponsive to conventional treatments. Radiofrequency ablation (RFA) uses radiofrequency energy to destroy abnormal electrical pathways in heart tissue. The energy emitting probe (electrode) is placed into the heart through a catheter inserted into veins in the groin or neck. Electrodes that can detect electrical activity from inside the heart are also inserted, and the electrophysiologist uses these to "map" an area of the heart in order to locate the abnormal electrical activity before eliminating the responsible tissue.
Most AF ablations consist of isolating the electrical pathways from the pulmonary veins (PV)[55], which are located on the posterior wall of the left atrium. All other veins from the body (including neck and groin) lead to the right atrium, so in order to get to the left atrium the catheters must get across the atrial septum. This is done by piercing a small hole in the septal wall. This is called a transseptal approach. Once in the left atrium, the physician may perform Wide Area Circumferential Ablation (WACA) to electrically isolate the PVs from the left atrium.[56]
Some more recent approaches to ablating AF is to target sites that are particularly disorganized in both atria as well as in the coronary sinus (CS). These sites are termed complex fractionated atrial electrogram (CFAE) sites.[57]. It is believed by some that the CFAE sites are the cause of AF, or a combination of the PVs and CFAE sites are to blame. New techniques include the use of cryoablation (tissue freezing using a coolant which flows through the catheter), microwave ablation, where tissue is ablated by the microwave energy "cooking" the adjacent tissue, and high intensity focused ultrasound (HIFU), which destroys tissue by heating. This is an area of active research, especially with respect to the RF ablation technique and emphasis on isolating the pulmonary veins that enter into the left atrium.
Efficacy and risks of catheter ablation of atrial fibrillation are areas of active debate. A worldwide survey of the outcomes of 8745 ablation procedures[58] demonstrated a 52% success rate (ranging from 14.5% to 76.5% among centers), with an additional 23.9% of patients becoming asymptomatic with addition of an antiarrhythmic medication. In 27.3% of patients, more than one procedure was required to attain these results. There was at least one major complication in 6% of patients. A thorough discussion of results of catheter ablation was published in 2007[59]; it notes that results are widely variable, due in part to differences in technique, follow-up, definitions of success, use of antiarrhythmic therapy, and in experience and technical proficiency.
Surgical treatment of atrial fibrillation
Maze procedure
James Cox, MD, and associates developed the Cox maze procedure, an open-heart surgical procedure intended to eliminate atrial fibrillation, and performed the first one in 1987. "Maze" refers to the series of incisions made in the atria, which are arranged in a maze-like pattern. The intention was to eliminate AF by using incisional scars to block abnormal electrical circuits (atrial macro reentry) that AF requires. This procedure required an extensive series of endocardial (from the inside of the heart) incisions through both atria, a median sternotomy (vertical incision through the breastbone) and cardiopulmonary bypass (heart-lung machine). A series of improvements were made, culminating in 1992 in the Cox maze III procedure, which is now considered to be the "gold standard" for effective surgical cure of AF. The Cox maze III is sometimes referred to as the "traditional maze", the "cut and sew maze", or simply the "maze".[60]
Minimaze surgery is minimally invasive cardiac surgery similarly intended to cure atrial fibrillation. The "Minimaze" procedure refers to "mini" versions of the original maze procedure. These procedures are less invasive than the Cox maze procedure and do not require a median sternotomy (vertical incision in the breastbone) or cardiopulmonary bypass (heart-lung machine). These procedures use microwave, radiofrequency, or acoustic energy to ablate atrial tissue near the pulmonary veins.
Prognosis
Follow up & Secondary prevention
Risk factors for ischemic stroke or systemic embolization in patient with non valvular atrial fibrillation
Numbers represents relative risks[61]
- Advanced age (continuous, per decade) 1.4
- History of hypertension 1.6
- Heart failure or impaired left ventricular systolic function 1.4
- Coronary artery disease (CAD) 1.5
- Diabetes mellitus (DM) 1.7
- Previous stroke or Transient Ischemic Attack (TIA) 2.5
Clinical Trial Data
Results from the Pulmonary Vein Antrum Isolation versus AV Node Ablation with Bi-Ventricular Pacing for Treatment of Atrial Fibrillation in Patients with Congestive Heart Failure (PABA-CHF) study suggest that pulmonary-vein (PV) isolation leads to better morphologic and functional results than atrioventricular (AV) node ablation with biventricular pacing for congestive heart failure (CHF) in patients with atrial fibrillation.
In this prospective, multicenter study, 41 patients were randomized to PV isolation and 40 to AV node ablation with biventricular pacing. At 6 months, patients in the PV isolation group had higher mean ejection fractions (35% vs 29%, p<0.001), greater 6 minute distances walked (340 vs 297 meters, p <0.001), and better quality of life scores as determined by the Minnesota Living with Heart Failure questionnaire (60 vs 82, p<0.001, where lower scores indicate better quality of life) than those in the AV node ablation arm.
These PABA-CHF study findings thus suggest the potential advantages of performing PV isolation over AV node ablation with biventricular pacing for this patient population.
Noted limitations of the study include using sites with extensive experience in performing ablations, an unblinded study design, and a relatively short follow-up time. (NEJM by Mohammed N. Khan, et al.)
Guidelines: Diagnosis and Management of Atrial Fibrillation
External links
- American Heart Association's page on atrial fibrillation
- Atrial fibrillation
- Bandolier: Evidence-based medicine resource on atrial fibrillation
- Cleveland Clinic Webchat - Atrial Fibrillation Webchat with Dr. Jennifer Cummings
See also
EKG Examples of atrial fibrillation
External EKG Sources
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 Fuster V, Rydén LE, Cannom DS; et al. (2006). "ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation. 114 (7): e257–354. doi:10.1161/CIRCULATIONAHA.106.177292. PMID 16908781.
- ↑ Levy S (1998). "Epidemiology and classification of atrial fibrillation". J Cardiovasc Electrophysiol. 9 (8 Suppl): S78–82. PMID 9727680
- ↑ Levy S (2000). "Classification system of atrial fibrillation". Curr Opin Cardiol. 15 (1): 54–7. PMID 10666661
- ↑ Sweeney MO, Bank AJ, Nsah E; et al. (2007). "Minimizing ventricular pacing to reduce atrial fibrillation in sinus-node disease". N. Engl. J. Med. 357 (10): 1000–8. doi:10.1056/NEJMoa071880. PMID 17804844.
- ↑ Fox CS, Parise H, D'Agostino RB; et al. (2004). "Parental atrial fibrillation as a risk factor for atrial fibrillation in offspring". JAMA. 291 (23): 2851–5. doi:10.1001/jama.291.23.2851. PMID 15199036.
- ↑ Saffitz JE (2006). "Connexins, conduction, and atrial fibrillation". N. Engl. J. Med. 354 (25): 2712–4. doi:10.1056/NEJMe068088. PMID 16790707.
- ↑ Elvan A, Wylie K, Zipes D (1996). "Pacing-induced chronic atrial fibrillation impairs sinus node function in dogs. Electrophysiological remodeling". Circulation. 94 (11): 2953–60. PMID 8941126.
- ↑ Manios EG, Kanoupakis EM, Mavrakis HE, Kallergis EM, Dermitzaki DN, Vardas PE (2001). "Sinus pacemaker function after cardioversion of chronic atrial fibrillation: is sinus node remodeling related with recurrence?". Journal of Cardiovascular Electrophysiology. 12 (7): 800–6. doi:10.1046/j.1540-8167.2001.00800.x. PMID 11469431.
- ↑ 9.0 9.1 Fitzmaurice DA, Hobbs FD, Jowett S; et al. (2007). "Screening versus routine practice in detection of atrial fibrillation in patients aged 65 or over: cluster randomized controlled trial". doi:10.1136/bmj.39280.660567.55. PMID 17673732.
- ↑ Mant J, Fitzmaurice DA, Hobbs FD; et al. (2007). "Accuracy of diagnosing atrial fibrillation on electrocardiogram by primary care practitioners and interpretative diagnostic software: analysis of data from screening for atrial fibrillation in the elderly (SAFE) trial". doi:10.1136/bmj.39227.551713.AE. PMID 17604299.
- ↑ Prystowsky EN (2000). "Management of atrial fibrillation: therapeutic options and clinical decisions". Am J Cardiol. 85 (10A): 3D–11D. PMID 10822035
- ↑ 12.0 12.1 12.2 Hart RG, Benavente O, McBride R, Pearce LA (1999). "Antithrombotic therapy to prevent stroke in patients with atrial fibrillation: a meta-analysis". Ann. Intern. Med. 131 (7): 492–501. Unknown parameter
|month=ignored (help) - ↑ Gorter JW (1999). "Major bleeding during anticoagulation after cerebral ischemia: patterns and risk factors. Stroke Prevention In Reversible Ischemia Trial (SPIRIT). European Atrial Fibrillation Trial (EAFT) study groups". Neurology. 53 (6): 1319–27. PMID 10522891. Unknown parameter
|month=ignored (help) - ↑ Hylek EM, Singer DE (1994). "Risk factors for intracranial hemorrhage in outpatients taking warfarin". Ann. Intern. Med. 120 (11): 897–902. PMID 8172435. Unknown parameter
|month=ignored (help) - ↑ Hart RG, Halperin JL (1999). "Atrial fibrillation and thromboembolism: a decade of progress in stroke prevention". Ann. Intern. Med. 131 (9): 688–95. PMID 10577332. Unknown parameter
|month=ignored (help) - ↑ Hylek EM, Skates SJ, Sheehan MA, Singer DE (1996). "An analysis of the lowest effective intensity of prophylactic anticoagulation for patients with nonrheumatic atrial fibrillation". N. Engl. J. Med. 335 (8): 540–6. PMID 8678931. Unknown parameter
|month=ignored (help) - ↑ "Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial". Lancet. 348 (9028): 633–8. 1996. PMID 8782752. Unknown parameter
|month=ignored (help) - ↑ "Optimal oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and recent cerebral ischemia. The European Atrial Fibrillation Trial Study Group". N. Engl. J. Med. 333 (1): 5–10. 1995. PMID 7776995. Unknown parameter
|month=ignored (help) - ↑ 19.0 19.1 19.2 Hart RG (1998). "Intensity of anticoagulation to prevent stroke in patients with atrial fibrillation". Ann. Intern. Med. 128 (5): 408. PMID 9490603. Unknown parameter
|month=ignored (help) - ↑ "The efficacy of aspirin in patients with atrial fibrillation. Analysis of pooled data from 3 randomized trials. The Atrial Fibrillation Investigators". Arch. Intern. Med. 157 (11): 1237–40. 1997. PMID 9183235. Unknown parameter
|month=ignored (help) - ↑ Miller VT, Rothrock JF, Pearce LA, Feinberg WM, Hart RG, Anderson DC (1993). "Ischemic stroke in patients with atrial fibrillation: effect of aspirin according to stroke mechanism. Stroke Prevention in Atrial Fibrillation Investigators". Neurology. 43 (1): 32–6. PMID 8423907. Unknown parameter
|month=ignored (help) - ↑ Hart RG, Pearce LA, Miller VT; et al. (2000). "Cardioembolic vs. noncardioembolic strokes in atrial fibrillation: frequency and effect of antithrombotic agents in the stroke prevention in atrial fibrillation studies". Cerebrovasc. Dis. 10 (1): 39–43. PMID 10629345.
- ↑ The ACTIVE Writing Group on behalf of the ACTIVE Investigators. Lancet 2006;367:1903-12.
- ↑ The ACTIVE Writing Group on behalf of the ACTIVE Investigators. Lancet 2006;367:1903-12.
- ↑ 25.0 25.1 Fatkin D, Kuchar DL, Thorburn CW, Feneley MP (1994). "Transesophageal echocardiography before and during direct current cardioversion of atrial fibrillation: evidence for "atrial stunning" as a mechanism of thromboembolic complications". J. Am. Coll. Cardiol. 23 (2): 307–16. PMID 8294679. Unknown parameter
|month=ignored (help) - ↑ Antonielli E, Pizzuti A, Bassignana A; et al. (1999). "Transesophageal echocardiographic evidence of more pronounced left atrial stunning after chemical (propafenone) rather than electrical attempts at cardioversion from atrial fibrillation". Am. J. Cardiol. 84 (9): 1092–6, A9–10. PMID 10569673. Unknown parameter
|month=ignored (help) - ↑ 27.0 27.1 Falcone RA, Morady F, Armstrong WF (1996). "Transesophageal echocardiographic evaluation of left atrial appendage function and spontaneous contrast formation after chemical or electrical cardioversion of atrial fibrillation". Am. J. Cardiol. 78 (4): 435–9. PMID 8752189. Unknown parameter
|month=ignored (help) - ↑ Bellotti P, Spirito P, Lupi G, Vecchio C (1998). "Left atrial appendage function assessed by transesophageal echocardiography before and on the day after elective cardioversion for nonvalvular atrial fibrillation". Am. J. Cardiol. 81 (10): 1199–202. PMID 9604945. Unknown parameter
|month=ignored (help) - ↑ Harjai K, Mobarek S, Abi-Samra F; et al. (1998). "Mechanical dysfunction of the left atrium and the left atrial appendage following cardioversion of atrial fibrillation and its relation to total electrical energy used for cardioversion". Am. J. Cardiol. 81 (9): 1125–9. PMID 9605054. Unknown parameter
|month=ignored (help) - ↑ Sparks PB, Jayaprakash S, Vohra JK; et al. (1998). "Left atrial "stunning" following radiofrequency catheter ablation of chronic atrial flutter". J. Am. Coll. Cardiol. 32 (2): 468–75. PMID 9708477. Unknown parameter
|month=ignored (help) - ↑ Mitusch R, Garbe M, Schmücker G, Schwabe K, Stierle U, Sheikhzadeh A (1995). "Relation of left atrial appendage function to the duration and reversibility of nonvalvular atrial fibrillation". Am. J. Cardiol. 75 (14): 944–7. PMID 7733009. Unknown parameter
|month=ignored (help) - ↑ Manning WJ, Silverman DI, Katz SE; et al. (1995). "Temporal dependence of the return of atrial mechanical function on the mode of cardioversion of atrial fibrillation to sinus rhythm". Am. J. Cardiol. 75 (8): 624–6. PMID 7887393. Unknown parameter
|month=ignored (help) - ↑ Grimm RA, Leung DY, Black IW, Stewart WJ, Thomas JD, Klein AL (1995). "Left atrial appendage "stunning" after spontaneous conversion of atrial fibrillation demonstrated by transesophageal Doppler echocardiography". Am. Heart J. 130 (1): 174–6. PMID 7611109. Unknown parameter
|month=ignored (help) - ↑ Black IW, Fatkin D, Sagar KB; et al. (1994). "Exclusion of atrial thrombus by transesophageal echocardiography does not preclude embolism after cardioversion of atrial fibrillation. A multicenter study". Circulation. 89 (6): 2509–13. PMID 8205657. Unknown parameter
|month=ignored (help) - ↑ Berger M, Schweitzer P (1998). "Timing of thromboembolic events after electrical cardioversion of atrial fibrillation or flutter: a retrospective analysis". Am. J. Cardiol. 82 (12): 1545–7, A8. PMID 9874066. Unknown parameter
|month=ignored (help) - ↑ 36.0 36.1 Epstein AE, DiMarco JP, Ellenbogen KA, Estes NAM III, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices). Circulation. 2008; 117: 2820–2840. PMID 18483207
- ↑ Brand FN, Abbott RD, Kannel WB, Wolf PA (1985). "Characteristics and prognosis of lone atrial fibrillation. 30-year follow-up in the Framingham Study". JAMA. 254 (24): 3449–53. PMID 4068186.
- ↑ "Independent predictors of stroke in patients with atrial fibrillation: a systematic review". Neurology. 69 (6): 546–54. 2007. doi:10.1212/01.wnl.0000267275.68538.8d. PMID 17679673.
- ↑ Kopecky SL, Gersh BJ, McGoon MD; et al. (1987). "The natural history of lone atrial fibrillation. A population-based study over three decades". N. Engl. J. Med. 317 (11): 669–74. PMID 3627174.
- ↑ 40.0 40.1 National Institute for Health and Clinical Excellence (June 2006). "Clinical Guideline 36 - Atrial fibrillation". Retrieved 2007-08-15.
- ↑ Hart RG, Pearce LA, McBride R, Rothbart RM, Asinger RW (1999). "Factors associated with ischemic stroke during aspirin therapy in atrial fibrillation: analysis of 2012 participants in the SPAF I-III clinical trials. The Stroke Prevention in Atrial Fibrillation (SPAF) Investigators". Stroke. 30 (6): 1223–9. PMID 10356104.
- ↑ Wang TJ, Massaro JM, Levy D; et al. (2003). "A risk score for predicting stroke or death in individuals with new-onset atrial fibrillation in the community: the Framingham Heart Study". JAMA. 290 (8): 1049–56. doi:10.1001/jama.290.8.1049. PMID 12941677.
- ↑ Baruch L, Gage BF, Horrow J; et al. (2007). "Can patients at elevated risk of stroke treated with anticoagulants be further risk stratified?". Stroke. 38 (9): 2459–63. doi:10.1161/STROKEAHA.106.477133. PMID 17673721.
- ↑ van Walraven C, Hart RG, Singer DE; et al. (2002). "Oral anticoagulants vs aspirin in nonvalvular atrial fibrillation: an individual patient meta-analysis". JAMA. 288 (19): 2441&ndash, 48. PMID 12435257.
- ↑ Gage BF, Cardinalli AB, Owens D. (1998). "Cost-effectiveness of preference-based antithrombotic therapy for patients with nonvalvular atrial fibrillation". Stroke. 29: 1083&ndash, 91. PMID 9626276.
- ↑ Paciaroni M, Agnelli G, Micheli S, Caso V (2007). "Efficacy and safety of anticoagulant treatment in acute cardioembolic stroke: a meta-analysis of randomized controlled trials". Stroke. 38 (2): 423–30. doi:10.1161/01.STR.0000254600.92975.1f. PMID 17204681. ACP JC synopsis
- ↑ Hart RG, Pearce LA, Aguilar MI (2007). "Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation". Ann Intern Med. 146 (12): 857–67. PMID 17577005.
- ↑ Aguilar M, Hart R, Pearce L (2007). "Oral anticoagulants versus antiplatelet therapy for preventing stroke in patients with non-valvular atrial fibrillation and no history of stroke or transient ischemic attacks". Cochrane Database Syst Rev. 3: CD006186. doi:10.1002/14651858.CD006186.pub2. PMID 17636831.
- ↑ Connolly S, Pogue J, Hart R; et al. (2006). "Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE W): a randomised controlled trial". Lancet. 367 (9526): 1903–12. doi:10.1016/S0140-6736(06)68845-4. PMID 16765759.
- ↑ "Adjusted-dose warfarin versus low-intensity, fixed-dose warfarin plus aspirin for high-risk patients with atrial fibrillation: Stroke Prevention in Atrial Fibrillation III randomised clinical trial". Lancet. 348 (9028): 633–638. 1996. doi:10.1016/S0140-6736(96)03487-3. PMID 8782752.
- ↑ Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S (2007). "Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation". Circulation. 115 (21): 2689–96. doi:10.1161/CIRCULATIONAHA.106.653048. PMID 17515465.
- ↑ Mant J; et al. (2007). "Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial". Lancet. 370: 493–503. doi:10.1016/S0140-6736(07)61233-1.
- ↑ 53.0 53.1 Wyse DG, Waldo AL, DiMarco JP, Domanski MJ, Rosenberg Y, Schron EB, Kellen JC, Greene HL, Mickel MC, Dalquist JE, Corley SD (2002). "A comparison of rate control and rhythm control in patients with atrial fibrillation". N Engl J Med. 347 (23): 1825–33. PMID 12466506
- ↑ Singh BN, Connolly SJ, Crijns HJ; et al. (2007). "Dronedarone for maintenance of sinus rhythm in atrial fibrillation or flutter". N. Engl. J. Med. 357 (10): 987–99. doi:10.1056/NEJMoa054686. PMID 17804843.
- ↑ The Cleveland Clinic
- ↑ Medscape
- ↑ Nademanee K, McKenzie J, Kosar E, Schwab M, Sunsaneewitayakul B, Vasavakul T, Khunnawat C, Ngarmukos T. (2004). "A new approach for catheter ablation of atrial fibrillation: mapping of the electrophysiologic substrate". J Am Coll Cardiol. 43 (11): 2044–53. doi:10.1016/j.jacc.2003.12.054. PMID 15172410.
- ↑ Cappato R, Calkins H, Chen SA, Davies W, Iesaka Y, Kalman J, Kim YH, Klein G, Packer D, Skanes A. (2005). "Worldwide survey on the methods, efficacy, and safety of catheter ablation for human atrial fibrillation". Circulation. 111: 1100–1105. doi:10.1161/01.CIR.0000157153.30978.67. PMID 15723973.
- ↑ Calkins H, Brugada J, Packer DL, Cappato R, Chen SA, Crijns HJ, Damiano RJ Jr, Davies DW, Haines DE, Haissaguerre M, Iesaka Y, Jackman W, Jais P, Kottkamp H, Kuck KH, Lindsay BD, Marchlinski FE, McCarthy PM, Mont JL, Morady F, Nademanee K, Natale A, Pappone C, Prystowsky E, Raviele A, Ruskin JN, Shemin RJ. (2007). "HRS/EHRA/ECAS expert Consensus Statement on catheter and surgical ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and surgical ablation of atrial fibrillation". Heart Rhythm. 4 (6): 816–61. PMID 17556213.
- ↑ Cox JL, Schuessler RB, Lappas DG, Boineau JP (1996). "An 8 1/2-year clinical experience with surgery for atrial fibrillation". Ann. Surg. 224 (3): 267–73, discussion 273-5. PMID 8813255.
- ↑ Estes NAM 3rd, Halperin JL, Calkins H, Ezekowitz MD, Gitman P, Go AS, McNamara RL, Messer JV, Ritchie JL, Romeo SJW, Waldo AL, Wyse DG. ACC/AHA/Physician Consortium 2008 clinical performance measures for adults with non valvular atrial fibrillation or atrial flutter: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and the Physician Consortium for Performance Improvement (Writing Committee to Develop Performance Measures for Atrial Fibrillation). Circulation 2008; 117:1101–1120
Further Readings
- Fuster V, Rydén LE, Cannom DS, et al (2006). "ACC/AHA/ESC 2006 Guidelines for the Management of Patients with Atrial Fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients With Atrial Fibrillation): developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society". Circulation 114 (7): e257-354. doi:10.1161/CIRCULATIONAHA.106.177292. PMID 16908781.
- Estes NAM 3rd, Halperin JL, Calkins H, Ezekowitz MD, Gitman P, Go AS, McNamara RL, Messer JV, Ritchie JL, Romeo SJW, Waldo AL, Wyse DG. ACC/AHA/Physician Consortium 2008 clinical performance measures for adults with non valvular atrial fibrillation or atrial flutter: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures and the Physician Consortium for Performance Improvement (Writing Committee to Develop Performance Measures for Atrial Fibrillation). Circulation 2008; 117:1101–1120
- Braunwald's Heart Disease, Libby P, 8th ed., 2007, ISBN 978-1-41-604105-4
- Hurst's the Heart, Fuster V, 12th ed. 2008, ISBN 978-0-07-149928-6
- Willerson JT, Cardiovascular Medicine, 3rd ed., 2007, ISBN 978-1-84628-188-4
de:Vorhofflimmern it:Fibrillazione atriale nl:Boezemfibrilleren no:Atrieflimmer fi:Eteisvärinä