ST elevation myocardial infarction history and symptoms
| Myocardial infarction | |
| ICD-10 | I21-I22 |
|---|---|
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
| Cardiology Network |
 Discuss ST elevation myocardial infarction history and symptoms further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Symptoms
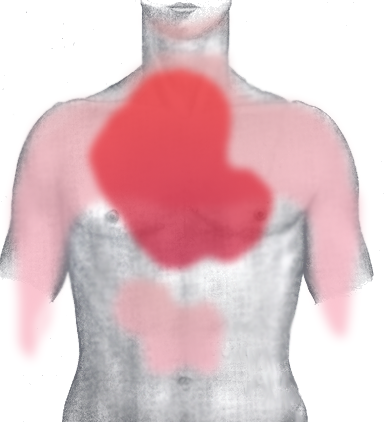
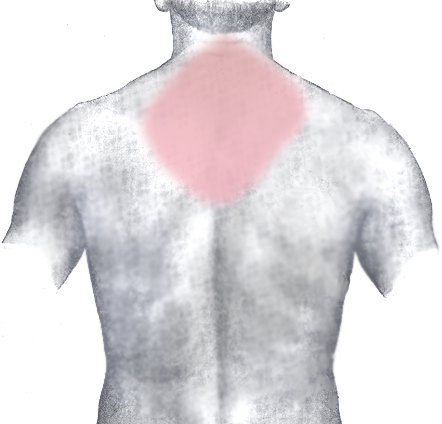
The onset of symptoms in myocardial infarction (MI) is usually gradual, over several minutes, and rarely instantaneous.[1] Chest pain is the most common symptom of acute myocardial infarction and is often described as a sensation of tightness, pressure, or squeezing. Chest pain due to ischemia (a lack of blood and hence oxygen supply) of the heart muscle is termed angina pectoris. Pain radiates most often to the left arm, but may also radiate to the lower jaw, neck, right arm, back, and epigastrium, where it may mimic heartburn. Any group of symptoms compatible with a sudden interruption of the blood flow to the heart are called an acute coronary syndrome.[2] Other conditions such as aortic dissection or pulmonary embolism may present with chest pain and must be considered in the differential diagnosis.
Shortness of breath (dyspnea) occurs when the damage to the heart limits the output of the left ventricle, causing left ventricular failure and consequent pulmonary edema. Other symptoms include diaphoresis (an excessive form of sweating), weakness, light-headedness, nausea, vomiting, and palpitations. Loss of consciousness and even sudden death can occur in myocardial infarctions.
Women often experience markedly different symptoms than men. The most common symptoms of MI in women include dyspnea, weakness, and fatigue. Fatigue, sleep disturbances, and dyspnea have been reported as frequently occurring symptoms which may manifest as long as one month before the actual clinically manifested ischemic event. In women, chest pain may be less predictive of coronary ischemia than in men.[3]
Approximately half of all MI patients have experienced warning symptoms such as chest pain prior to the infarction.[4]
Approximately one fourth of all myocardial infarctions are silent, without chest pain or other symptoms.[5] These cases can be discovered later on electrocardiograms or at autopsy without a prior history of related complaints. A silent course is more common in the elderly, in patients with diabetes mellitus[6] and after heart transplantation, probably because the donor heart is not connected to nerves of the host.[7] In diabetics, differences in pain threshold, autonomic neuropathy, and psychological factors have been cited as possible explanations for the lack of symptoms.[6]
Early Recognition of MI Symptoms
Early recognition of symptoms of STEMI by the patient or someone with the patient is the first step that must occur before evaluation and life saving treatment can be obtained. Although many lay persons are generally aware that chest pain is a presenting symptom of acute myocardial infarction, they are unaware of the common associated symptoms, such as arm pain (or a slight radiation of pain), lower jaw pain, shortness of breath, and diaphoresis or anginal equivalents. [8]
In randomized trials, the average time for a patient with ST elevation myocardial infarction to seek medical care is 2.7 to 2.9 hours after symptom onset, and this pattern appears unchanged over the last decade.[8]
Likewise, average and median delays for patients with STEMI were 4.7 and 2.3 hours, respectively, from the 14-country Global Registry of Acute Coronary Events (GRACE) registry.
Data from the REACT research program demonstrated longer delay times among non Hispanic blacks, older patients, and Medicaid only recipients and shorter delay times among Medicare recipients (compared with privately insured patients) and among patients who came to the hospital by ambulance. [9] In the majority of studies examined to date, women in both univariate and multivariate adjusted analyses (in which age and other potentially confounding variables have been controlled) exhibit more prolonged delay patterns than men.[8]
Reasons for Delays in Symptom Recognition and Seeking Medical Care
It is notable that in the REACT study, while 89.4% of community survey respondents indicated that they would use EMS, only 23.2% of patients who in fact developed chest pain actually used EMS. Thus, there is a disconnect between what people know versus their actual course of behavior when confronted with a cardiac emergency. This may reflect potentially modifiable belief factors or situational factors.
One such modifiable factor is patient denial. It has been shown that if the patient believes the chest discomfort is “due to a heart attack” then they are more likely to call for EMS. On the other hand, if a patient can attribute the chest discomfort to another illness they are less likely to use Emergency Medical Services (EMS). One such scenario would include a patient who is self-prescribing antacids or aspirin. In contrast to these patients with other illnesses, those patients who were familiar with heart disease who were taking nitroglycerin were more likely to use EMS. These data point to the potential role of patient education in improving delays in seeking medical care.[10]
- Patient, lay person or relatives expected a dramatic presentation; patients or their relatives commonly hold a preexisting expectation that a heart attack would present dramatically with severe, crushing chest pain, such that there would be no doubt that one was occurring.
- Thought symptoms were not serious/would go away
- Took a “wait and see” approach to the initial symptoms that included self-evaluation, self-treatment, and reassessment until having a “certain one"
- Tended to attribute symptoms to other chronic conditions (e.g., arthritis, muscle strain) or common illnesses (e.g., influenza)
- Lacked awareness of the benefits of rapid action, reperfusion treatment, or of the importance of calling Emergency Medical Services or 911 for acute MI symptoms
- Expressed fear of embarrassment if symptoms turned out to be a false alarm; reluctant to “bother” physicians or EMS unless “really sick”; need “permission” from others such as health care providers, spouses, family to take rapid action.
- Few ever discussed symptoms, responses, or actions for a heart attack in advance with family or providers.
Transfer to Medical Facility
Patients with possible symptoms of STEMI should be transported to the hospital by ambulance rather than by friends or relatives, because there is a significant association between arrival at the emergency department by ambulance and early reperfusion therapy.
Differential Diagnosis of ST elevation myocardial infarction history and symptoms
See also
- acute coronary syndrome
- angina
- Cardiac arrest
- coronary thrombosis
- Hibernating myocardium
- Stunned myocardium
- Ventricular remodeling
References
- ↑ National Heart, Lung and Blood Institute. Heart Attack Warning Signs. Retrieved November 22, 2006.
- ↑ Acute Coronary Syndrome. American Heart Association. Retrieved November 25, 2006.
- ↑ McSweeney JC, Cody M, O'Sullivan P, Elberson K, Moser DK, Garvin BJ (2003). "Women's early warning symptoms of acute myocardial infarction". Circulation. 108 (21): 2619–23. PMID 14597589.
- ↑ D Lee, D Kulick, J Marks. Heart Attack (Myocardial Infarction) by MedicineNet.com . Retrieved November 28, 2006.
- ↑ Kannel WB. (1986). "Silent myocardial ischemia and infarction: insights from the Framingham Study". Cardiol Clin. 4 (4): 583–91. PMID 3779719.
- ↑ 6.0 6.1 Davis TM, Fortun P, Mulder J, Davis WA, Bruce DG (2004). "Silent myocardial infarction and its prognosis in a community-based cohort of Type 2 diabetic patients: the Fremantle Diabetes Study". Diabetologia. 47 (3): 395–9. PMID 14963648.
- ↑ Rubin's Pathology - Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. 2001. pp. p. 549. ISBN 0-7817-4733-3. Unknown parameter
|coauthors=ignored (help) - ↑ 8.0 8.1 8.2 Gibson CM (2001). "Time is myocardium and time is outcomes". Circulation. 104 (22): 2632–4. PMID 11723008.
- ↑ Brown AL, Mann NC, Daya M; et al. (2000). "Demographic, belief, and situational factors influencing the decision to utilize emergency medical services among chest pain patients. Rapid Early Action for Coronary Treatment (REACT) study". Circulation. 102 (2): 173–8. PMID 10889127.
- ↑ Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr, Alpert JS, Anderson JL, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 1999 Guidelines for the Management of Patients With Acute Myocardial Infarction). Circulation 2004; 110:588–636.
External links
- The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research
- Clinical Trial Results: An up to dated resource of Cardiovascular Research
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American College of Cardiology (ACC) Door to Balloon (D2B) Initiative.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.