Syphilis differential diagnosis: Difference between revisions
Ahmed Younes (talk | contribs) No edit summary |
|||
| Line 473: | Line 473: | ||
|} | |} | ||
== | Syphilitic oral lesions must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer | ||
<div style="width: 70%;"> | |||
<small><small> | |||
{| class="wikitable" | |||
!Disease | |||
!Presentation | |||
!Risk Factors | |||
!Diagnosis | |||
!Affected Organ Systems | |||
!Important features | |||
!Picture | |||
|- | |||
! colspan="3" |Diseases predominantly affecting the oral cavity | |||
! | |||
! | |||
! | |||
! | |||
|- | |||
|[[Oral candidiasis|Oral Candidiasis]] | |||
| | |||
* [[Dysphagia]] or [[odynophagia]] | |||
* White patches on the mouth and tongue | |||
| | |||
*[[Newborn]] babies | |||
*Denture users | |||
*Poorly controlled [[diabetes]] | |||
*As a side effect of medication, most commonly having taken [[antibiotic]]s. Inhaled [[corticosteroids]] for the treatment of lung conditions (e.g, [[asthma]] or [[COPD]]) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication. | |||
*People with poor [[nutrition]], specifically [[vitamin A]], [[Iron deficiency anemia|iron]] and [[Folate deficiency|folate deficiencies]]. | |||
*People with an [[immune deficiency]] (e.g. as a result of [[AIDS]]/[[HIV]] or [[chemotherapy]] treatment). | |||
*Women undergoing hormonal changes, like [[pregnancy]] or those on [[birth control pills]]. | |||
*[[Organ transplantation]] patients | |||
| | |||
* Clinical diagnosis | |||
* Confirmatory tests rarely needed | |||
|'''Localized candidiasis''' | |||
* [[Oral candidiasis|Oral]] and [[Esophageal candidiasis|esophageal candidasis]] | |||
* [[Candida vulvovaginitis]] | |||
* [[Chronic mucocutaneous candidiasis]] | |||
'''Invasive candidasis''' | |||
* [[Candidiasis|Candidaemia]] | |||
* [[Endocarditis|Candida endocarditis]] | |||
* [[Osteoarthritis|Candida osteoarticular disease]] | |||
| | |||
* [[Osteoarthritis|Oral candidiaisis is]] a benign self limiting disease unless accompanied by [[immunosuppression]]. | |||
|[[File:Human tongue infected with oral candidiasis--By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|thumb|Tongue infected with oral candidiasis - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=11717223.jpg|400x400px]] | |||
|- | |||
|[[Herpes simplex|Herpes simplex oral lesions]] | |||
| | |||
* [[Fever]] | |||
* [[Sore throat]] | |||
* Painful [[ulcer]]s | |||
| | |||
* Stress | |||
* Recent [[URTI]] | |||
* Female sex | |||
| | |||
* Physical examination | |||
* [[Viral culture]] | |||
* [[Tzanck smear]] | |||
| | |||
* Orofacial Infection | |||
* [[Herpes simplex anogenital infection|Anogenital Infection]] | |||
* [[Herpes simplex ocular infection|Ocular Infection]] | |||
* [[Herpes simplex encephalitis|Herpes Encephalitis]] | |||
* [[Herpes simplex neonatorum|Neonatal Herpes]] | |||
* [[Herpetic whitlow|Herpetic Whitlow]] | |||
* [[Herpes gladiatorum|Herpes Gladiatorum]] | |||
| | |||
* The symptoms of primary [[HSV]] infection generally resolve within two weeks | |||
|[[File:Herpesinfection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|thumb|Oral herpes simplex infection - By James Heilman, MD - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=19051042.jpg|400x400px]] | |||
|- | |||
|[[Aphthous ulcer|Aphthous ulcers]] | |||
| | |||
* Painful, red spot or bump that develops into an open [[ulcer]] | |||
| | |||
* Being a female | |||
* Between the ages of 10-40 | |||
* Family history of [[Aphthous ulcer|aphthous ulcers]] | |||
| | |||
* Physical examination | |||
* Diagnosis of exclusion | |||
| | |||
* Oral cavity | |||
| | |||
* Self-limiting , [[Pain]] decreases in 7 to 10 days, with complete healing in 1 to 3 weeks | |||
|[[File:Afta foto - By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358.jpg|thumb|Apthous ulcer on the under surface of the tongue|By Ebarruda - Own work, CC BY-SA 3.0, httpscommons.wikimedia.orgwindex.phpcurid=7903358|400x400px]] | |||
|- | |||
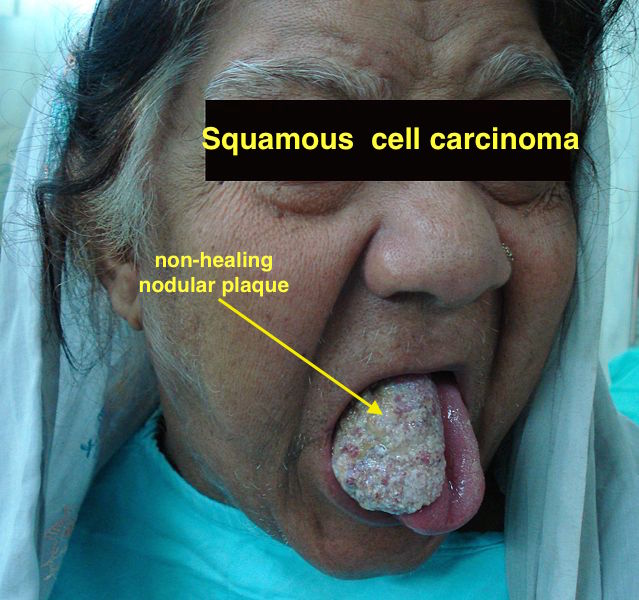
|[[Squamous cell carcinoma]] | |||
| | |||
*Non healing [[ulcer]], [[nodule]], indurated plaque or mass | |||
*May involve [[skin]], [[lips]], inside the [[mouth]], [[throat]] or [[esophagus]] | |||
| | |||
* Chronic sun or [[Ultraviolet|UV exposure]] | |||
* Fair [[skin]] | |||
* [[Elderly]] age (>45 yrs) | |||
* [[Male sex]] | |||
* [[Smoking]] | |||
| | |||
*[[Physical exam]] | |||
*[[Biopsy]] | |||
| | |||
*[[Oral Cavity]] | |||
**Floor of [[mouth]] | |||
**Lateral [[tongue]] | |||
*[[Throat]] | |||
*[[Esophagus]] | |||
| | |||
*[[Malignant]] | |||
*Can spread to [[TMJ]] | |||
*Some times associated with [[leukoplakia]] | |||
|[[File:Squamous cell carcinomaa.jpg|Squamous cell carcinoma|400x400px]] | |||
|- | |||
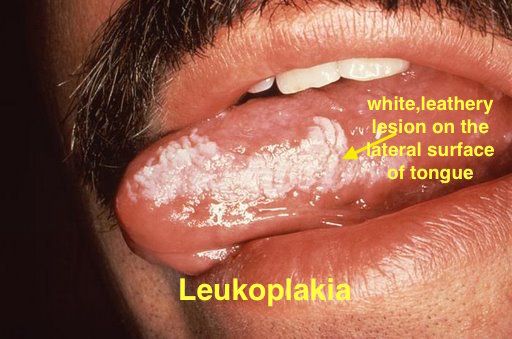
|[[Leukoplakia]] | |||
| | |||
*White leathery spots on the [[mucous membranes]] of the [[tongue]] and inside of the [[mouth]] | |||
*Lateral borders of [[tongue]] | |||
| | |||
*Atypical [[Tobacco]] use | |||
*Chronic [[irritation]] | |||
*[[Immunodeficiency]] | |||
*[[Bloodroot]] ([[Sanguinarine|sanguinaria]]) | |||
| | |||
*[[Physical exam]] | |||
*Diagnosis of exclusion | |||
*[[Biopsy]] | |||
| | |||
*[[Vulva|Vulvar]] lesions occur independent of oral lesions | |||
| | |||
*Associated with [[HIV]] | |||
*Persistant white spots | |||
*[[Benign]] but can progress to [[carcinoma]] after almost 10 years | |||
*Oral proliferative [[Leukoplakia|verrucous leukoplakia]] is an aggressive sub type with multiple lesions and higher conversion to [[warts]] or [[carcinoma]]<ref>{{Cite journal | |||
| author = [[Ann M. Gillenwater]], [[Nadarajah Vigneswaran]], [[Hanadi Fatani]], [[Pierre Saintigny]] & [[Adel K. El-Naggar]] | |||
| title = Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity! | |||
| journal = [[Advances in anatomic pathology]] | |||
| volume = 20 | |||
| issue = 6 | |||
| pages = 416–423 | |||
| year = 2013 | |||
| month = November | |||
| doi = 10.1097/PAP.0b013e3182a92df1 | |||
| pmid = 24113312 | |||
}}</ref> | |||
|[[File:Oral hairy leukoplakia (EBV, in HIV)a.jpg|Leukoplakia|400x300px]] | |||
|- | |||
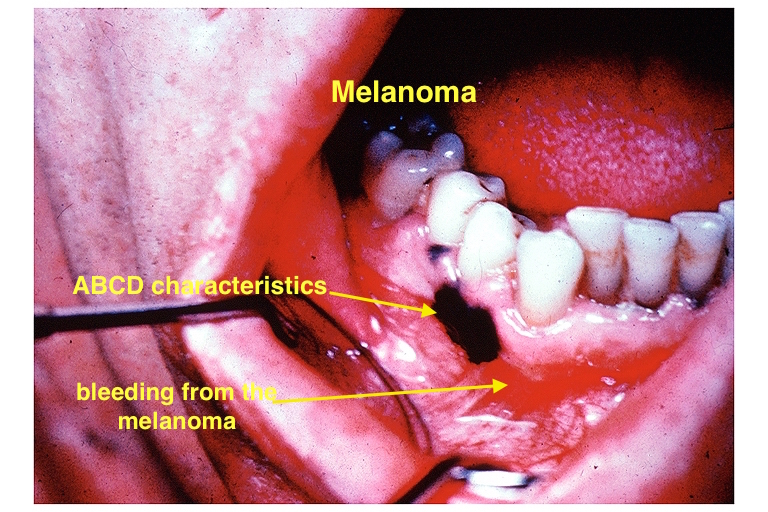
|[[Melanoma]] | |||
| | |||
*A lesion with [[ABCD]] | |||
**[[Asymmetry]] | |||
**Border irregularity | |||
**Color variation | |||
**[[Diamete]]r changes | |||
*[[Bleeding]] from the lesion | |||
| | |||
*[[Ultraviolet|UV radiations]] | |||
*[[Genetic predisposition]] | |||
*[[Old age]] | |||
*[[Male gender]] | |||
*Family or personal history of [[melanoma]] | |||
*Multiple benign or atypical [[Nevus|nevi]] | |||
| | |||
*[[ABCD]] characteristics | |||
*[[Bleeding]] or [[ulceration]] may show [[malignancy]] | |||
*Serum [[LDH]] may be elevated in case of [[malignancy]] | |||
*[[Biopsy]] | |||
| | |||
*Can [[metastasize]] | |||
*All [[UV radiation]] or sun exposed areas can be effected independently | |||
*1-2 to hundreds of [[granules]] | |||
| | |||
*[[Neural crest cell]] derivative | |||
*Development begins with disruption of [[nevus]] growth control | |||
*Progression involves [[MAPK/ERK pathway]] | |||
*[[RAS|N-RAS]] or [[BRAF]] [[oncogene]] also involved | |||
|[[File:Melanoma oral 001a.jpg|Oral melanoma|400x400px]] | |||
|- | |||
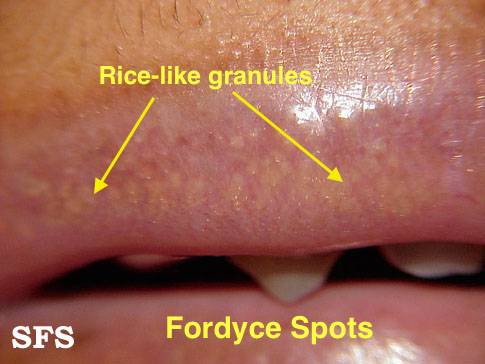
|[[Fordyce spots]] | |||
| | |||
*Rice-like [[granules]] or [[spots]] | |||
*Small, [[painless]], [[raised]], [[pale]], red or white | |||
*1 to 3 mm in [[diameter]] | |||
| | |||
*Greasy skin types | |||
*Some [[Rheumatic|rheumatic disorders]] | |||
*[[Hereditary nonpolyposis colorectal cancer]] | |||
**Lower [[gingiva]] (gums) | |||
**[[Vestibular system|Vestibular mucosa]] | |||
| | |||
*[[Physical exam]] | |||
*Small [[keratin]]-filled [[pseudocysts]] | |||
*May be seen on [[incidental]] [[mucosal]] [[biopsy]] | |||
**[[Biopsy]] not done for them primarily | |||
| | |||
*[[Oral cavity]] | |||
**[[Vermillion border|Vermilion border]] of the lips | |||
**[[Oral mucosa]] of the upper lip | |||
*[[Buccal mucosa]] in the commissural region often bilaterally | |||
*[[Genitals]] | |||
| | |||
*[[Benign neoplasms]] with [[sebaceous]] features | |||
*Visible [[sebaceous glands]] | |||
*No surrounding [[mucosal]] change | |||
*Several adjacent [[glands]] may coalesce into a larger cauliflower-like cluster | |||
|[[File:Fordyce spots 02a.jpg|Fordyce spots|400x400px]] | |||
|- | |||
|[[Burning mouth syndrome]] | |||
| | |||
*Burning or [[tingling]] on the [[lips]], [[tongue]], or entire [[mouth]] | |||
| | |||
*[[Nutritional deficiencies]] | |||
*Chronic [[anxiety]] or [[depression]] | |||
*[[Diabetes type 2]] | |||
*[[Menopause]] | |||
*[[Oral thrush]] or [[dry mouth]], or damaged [[nerves]] transmitting taste | |||
*[[Female gender ]] | |||
*[[Menopause]] | |||
| | |||
*[[Presentation]] | |||
*[[Physical exam]] | |||
| | |||
*[[Oral cavity]] | |||
| | |||
*Pain typically is low in the morning and builds up over the day | |||
*Low dosages of [[benzodiazepines]], [[tricyclic antidepressants]] or [[anticonvulsants]] may be effective | |||
| | |||
|- | |||
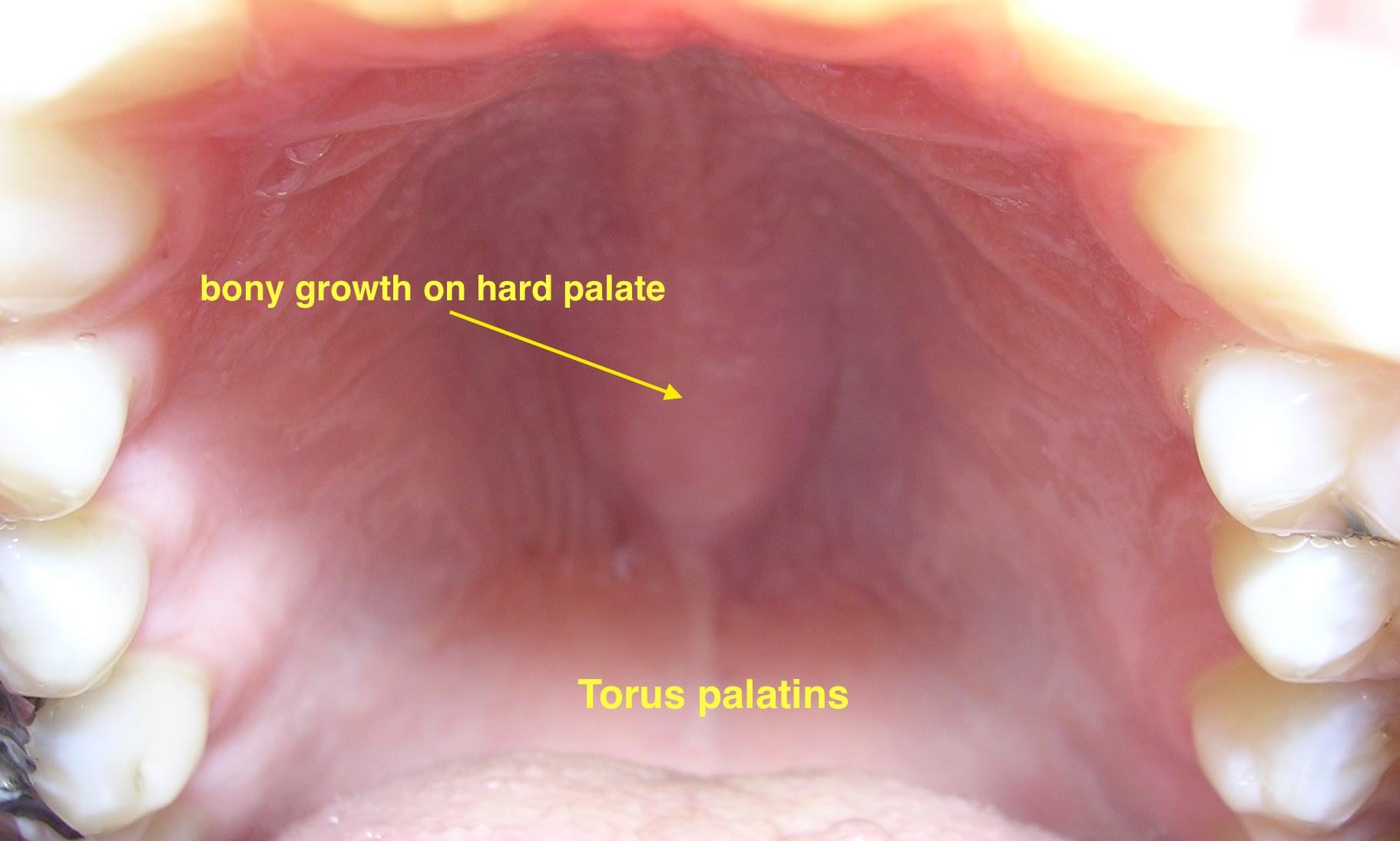
|[[Torus palatinus]] | |||
| | |||
*Bony growth on midline of the [[hard palate]] | |||
*[[Nodular]] mass covered with normal [[mucosa]] | |||
| | |||
*[[Genetic predisposition]] | |||
**[[Autosomal dominant]] | |||
| | |||
*[[Physical exam]] | |||
*Types | |||
**[[Torus palatinus|Flat tori]] | |||
**[[Torus palatinus|Spindle tori]] | |||
**[[Torus palatinus|Nodular tori]] | |||
**[[Torus palatinus|Lobular tori]] | |||
| | |||
*[[Hard palate]] | |||
| | |||
*More common in [[Asian]] and Inuit populations | |||
*Twice more common in [[females]] | |||
*Repeated [[trauma]] can cause [[bleeding]] | |||
*[[Surgery]] may be required in symptomatic | |||
|[[File:06-06-06palataltoria.jpg|Torus palatinus|400x400px]] | |||
|- | |||
| colspan="4" |'''Diseases involving oral cavity and other organ systems''' | |||
| | |||
| | |||
| | |||
|- | |||
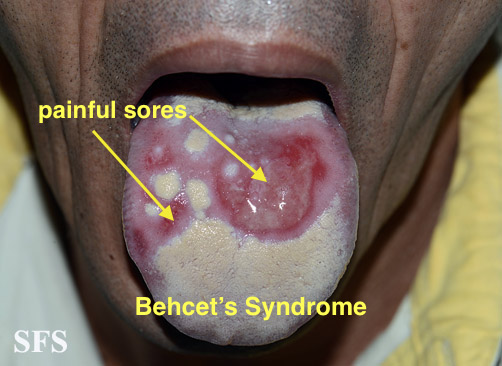
|[[Behçet's disease|Behcet's disease]] | |||
| | |||
*Painful [[mouth sores]] | |||
*[[Acne]] like skin lesions | |||
*Headache, [[fever]], poor [[balance]], [[disorientation]] | |||
*[[Abdominal pain]], [[diarrhea]] or [[bleeding]] | |||
*[[Uveitis]] | |||
*Joint [[swelling]] and joint [[pain]] | |||
*Genital [[sores]] wit [[pain]] and [[scaring]] | |||
*[[Aneurysms]] | |||
| | |||
*Over active [[immune system]] | |||
| | |||
*[[Physical examination]] | |||
| | |||
*[[Mouth]] | |||
*[[Genitals]] | |||
*[[GIT]] | |||
*[[Eye]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
*[[Vascular system]] | |||
*[[Brain]] | |||
| | |||
*[[Outbreaks]] of exaggerated [[inflammation]] | |||
*Affects smaller [[blood vessels]] | |||
|[[File:Behcet's syndrome 11a.jpg|Behcet's disease|400x400px]] | |||
|- | |||
|[[Crohn's disease]] | |||
| | |||
*Chronic, episodic [[diarrhea]] or [[constipation]] | |||
*[[Abdominal pain]] | |||
*[[Vomiting]] | |||
*[[Weight loss]] or [[weight gain]] | |||
| | |||
*[[Smoking]] | |||
*[[Whites]] and [[European]] [[Jews]] | |||
*[[Hormonal contraception]] | |||
*Diets high in microparticles, sweet, fatty or refined foods | |||
*Industrialized country | |||
| | |||
*Typical [[history]] and [[symptoms]] | |||
*[[Skip lesions]] on [[biopsy]] | |||
*[[Anti saccharomyces cerevisiae antibodies|Anti-Saccharomyces cerevisiae antibodies (ASCA)]] | |||
*[[Anti-neutrophil cytoplasmic antibodies]] ([[ANCA]]) | |||
| | |||
*[[Eyes]] | |||
*[[Joints]] | |||
*[[Skin]] | |||
| | |||
*May lead to | |||
**[[Obstruction]]s | |||
**[[Abscess]]es | |||
**Free [[perforation]] | |||
**[[Hemorrhage]] | |||
| | |||
|- | |||
|[[Agranulocytosis]] | |||
| | |||
*[[Fever]] or [[chills]] | |||
*Frequent [[infections]] | |||
*Unusual [[redness]], [[pain]], or [[swelling]] around a wound | |||
*Mouth [[ulcers]] | |||
*[[Abdominal pain]] | |||
*[[Burning sensation when urinating]] | |||
*[[Sore throat]] | |||
| | |||
*[[Medications]]<ref name="PMID17142169">{{cite journal |author=Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. |title=Idiosyncratic drug-induced agranulocytosis: Update of an old disorder. |journal=Eur J Intern Med. |volume=17|issue=8 |pages=529-35 |year=2006|pmid 17142169|doi=|url=https://www.ncbi.nlm.nih.gov/pubmed/17142169}}</ref> | |||
*[[List of chemotherapeutic agents#Cytotoxic Chemotherapy|Cytotoxic chemotherapy]] | |||
*[[Hematological malignancy|Hematologic malignancies]] | |||
*[[Autoimmune disorders]] | |||
| | |||
*[[Neutropenia]] <100 cells per micro litre | |||
*[[Eosinopenia]] | |||
*[[Basopenia]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[GIT]] | |||
*[[Urinary system]] | |||
*[[Conjunctiva]] | |||
| | |||
*[[Immunocompromised|Immunocompromization]] | |||
*Types | |||
**[[Drug-induced]] | |||
**[[Malignant]] | |||
**[[Autoimmune]] | |||
| | |||
|- | |||
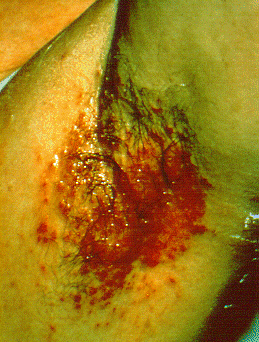
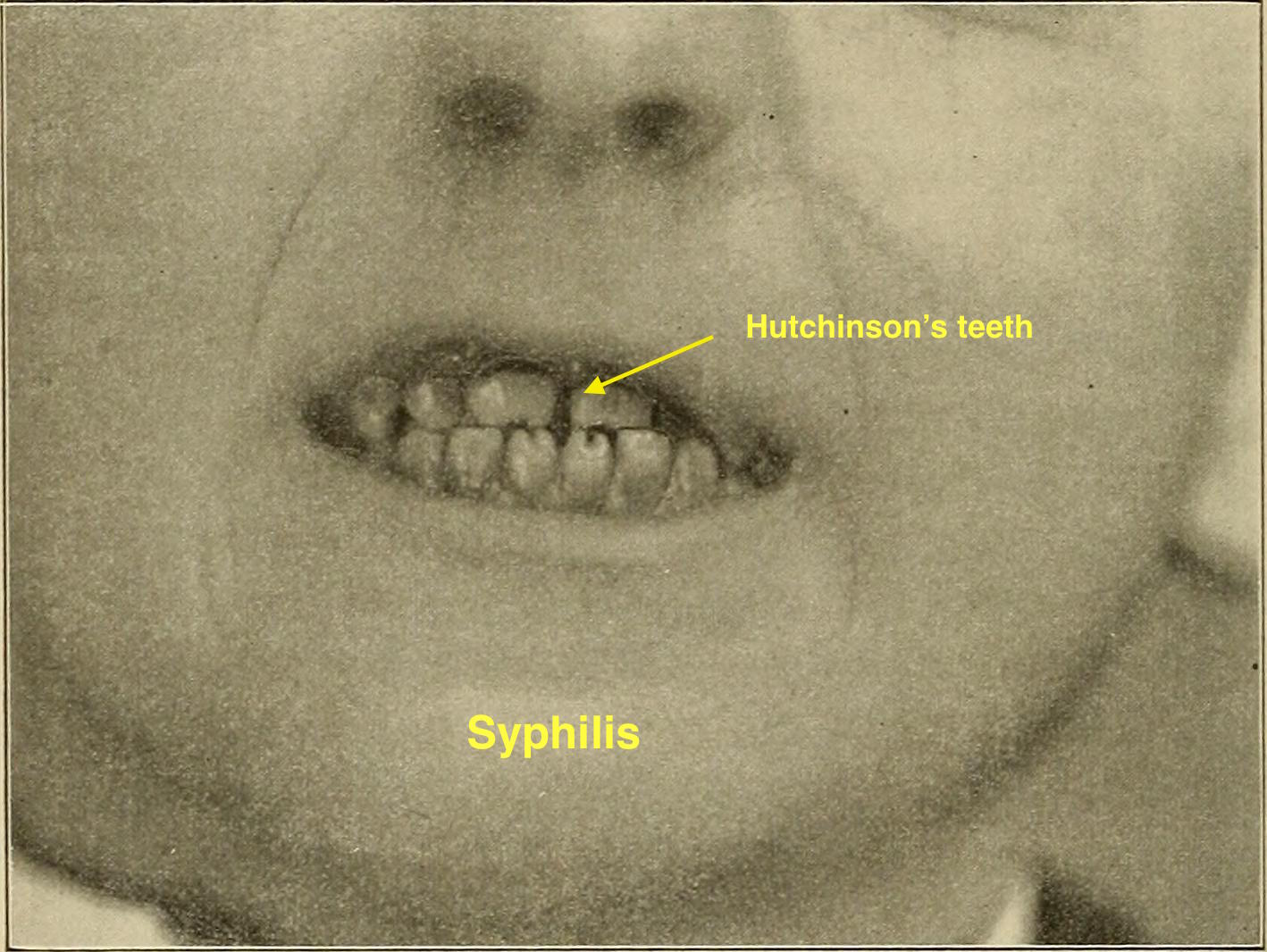
|[[Syphilis]]<ref> title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"</ref> | |||
| | |||
*[[Chancre]] | |||
*Regional [[lymphadenopathy]] | |||
| | |||
*[[Multiple sexual partners]] | |||
*Illicit [[drug use]] | |||
*[[Unprotected sex]] | |||
*[[Homosexual men|Men who have sex with men]] | |||
*Residence in highly prevalent areas | |||
*[[Human Immunodeficiency Virus (HIV)|HIV]] infection | |||
*Presence of other [[STI]]s | |||
*Previous history of [[Sexually transmitted disease|STIs]] | |||
*[[Intravenous drug use]] | |||
| | |||
*[[Darkfield microscope|Darkfield microscopy]] | |||
*Non [[Treponema|treponemal]] tests like [[VDRL]] and [[RPR test]]) | |||
*[[Treponema|Treponemal]] tests[[FTA-ABS|FTA-ABS tests]], (TP-PA) assay, [[Enzyme linked immunosorbent assay (ELISA)|enzyme immunoassays]], and [[Chemiluminescence|chemiluminescence immunoassays]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Penis]] | |||
*[[Cervix]] | |||
*[[Labia]] | |||
*[[Anal canal]] | |||
*[[Rectum ]] | |||
*[[CNS]] | |||
*[[Cardiovascular|CVS]] | |||
| | |||
*[[Primary syphilis]] | |||
**[[Chancre]] | |||
*[[Secondary syphilis]] | |||
**[[Condyloma latum|Condylomata lata]] | |||
*[[Latent syphilis]] | |||
**[[Asymptomatic]] | |||
*[[Tertiary syphilis]] | |||
**[[Gumma|Gummas]] | |||
**[[Neurosyphilis]] | |||
|[[File:Syphilis orala.jpg|oral syphilis|400x400px]] | |||
|- | |||
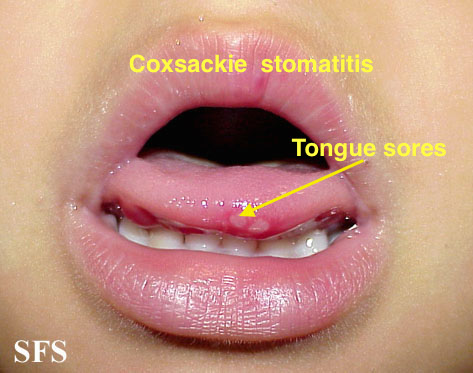
|[[Coxsackie virus]] | |||
| | |||
*[[Fever]] | |||
*[[Sores]] in the [[mouth]] | |||
*[[Rash]] with [[blisters]] | |||
*[[Aches]] | |||
| | |||
*[[Pregnancy]] | |||
*[[immunodeficiency]] | |||
| | |||
*[[History]] and [[Physical exam]] | |||
*[[Swabbing|Throat swabs]] | |||
*Swabs from the lesion | |||
*[[Tzanck test]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*Symptomatic treatment | |||
|[[File:Hand foot mouth disease 07a.jpg|Hand-foot-and-mouth disease|400x400px]] | |||
|- | |||
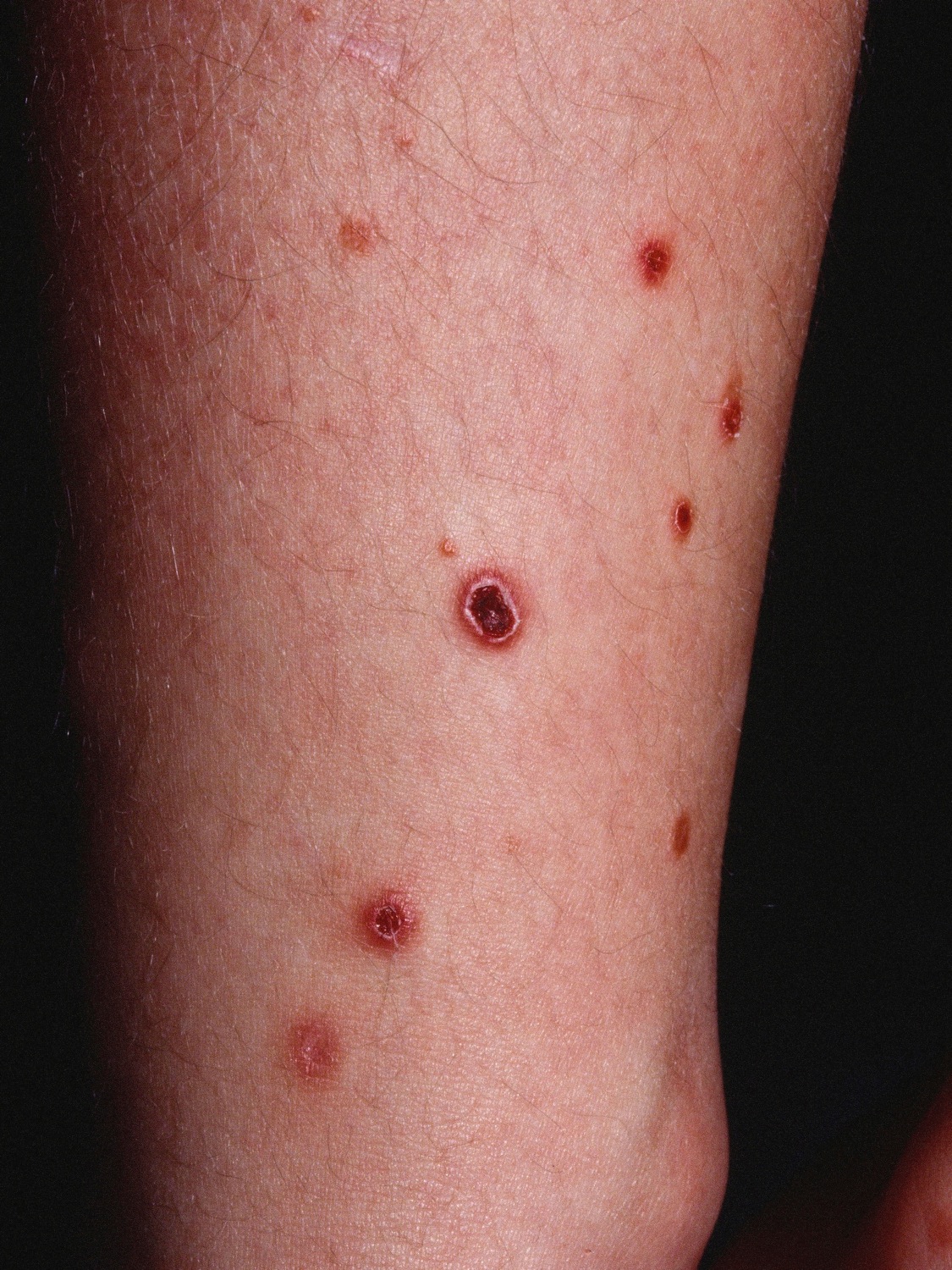
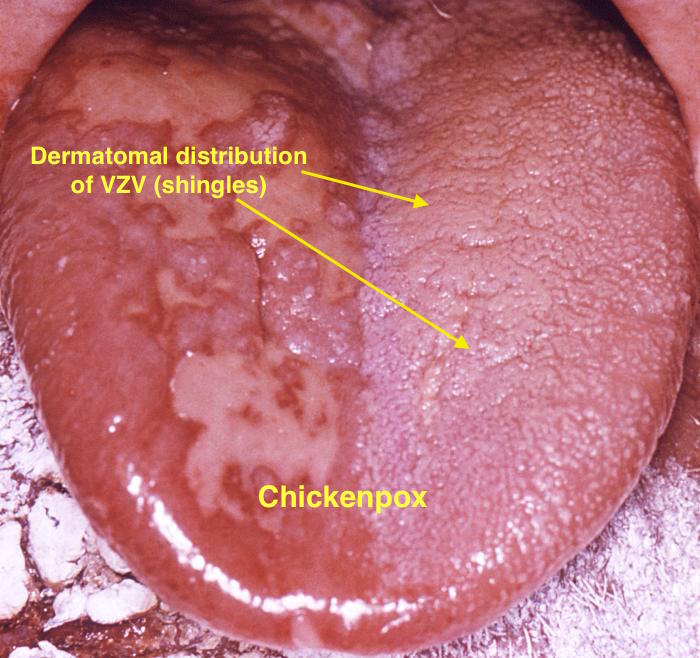
|[[Chickenpox|Chicken pox]] | |||
| | |||
*[[Conjunctival]] symptoms | |||
*[[Catarrhal]] symptoms | |||
*Characteristic [[spots]] on the trunk appearing in two or three waves | |||
*[[Itching]] | |||
| | |||
*[[Pregnancy]] | |||
*[[Premature infants]] born to susceptible mothers | |||
*All [[infants]] born at less than 28 weeks [[gestation]] or who weigh =1000 grams | |||
*[[Immunocompromised]] | |||
| | |||
*[[History]] and [[physical exam]] | |||
*[[PCR]] to detect [[VZV]] in [[skin lesions]] ([[vesicles]], [[scabs]], [[Maculopapular|maculopapular lesions]]) | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
| | |||
*[[Sodium bicarbonate]] in baths or [[antihistamines]] for [[itching]] | |||
*[[Paracetamol]] ([[acetaminophen]]) for [[fever]] | |||
*[[Prednisolone]] is [[contraindicated]] | |||
|[[File:Chickenpox18a.jpg|Chickenpox|400x400px]] | |||
|- | |||
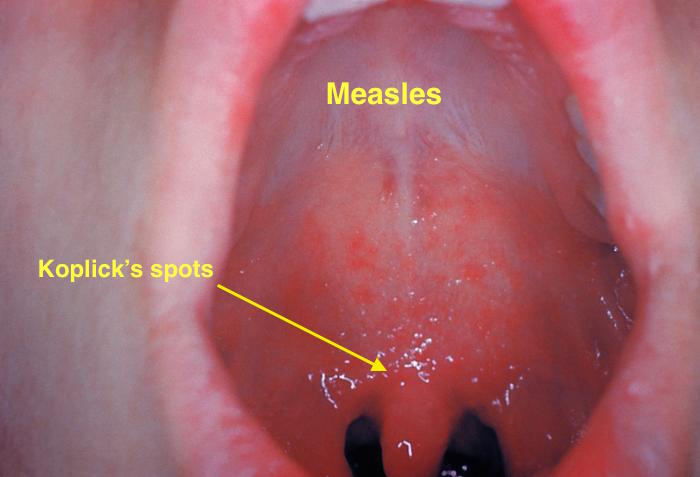
|[[Measles]] | |||
| | |||
*[[Fever]] | |||
*[[Rash]] | |||
*[[Cough]] | |||
*[[Coryza]] (runny nose) | |||
*[[Conjunctivitis]] (pink eye) | |||
*[[Malaise]] | |||
*[[Koplick spots]] in mouth | |||
| | |||
*Unvaccinated individuals<ref name="pmid11135778">{{cite journal| author=Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE| title=Individual and community risks of measles and pertussis associated with personal exemptions to immunization. | journal=JAMA | year= 2000 | volume= 284 | issue= 24 | pages= 3145-50 | pmid=11135778 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11135778 }} </ref><ref name="pmid9009400">{{cite journal| author=Ratnam S, West R, Gadag V, Williams B, Oates E| title=Immunity against measles in school-aged children: implications for measles revaccination strategies. | journal=Can J Public Health | year= 1996 | volume= 87 | issue= 6 | pages= 407-10 | pmid=9009400 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9009400 }} </ref> | |||
*Crowded and/or unsanitary conditions | |||
*Traveling to less developed and developing countries | |||
*Immunocompromized | |||
*Winter and [[spring]] seasons | |||
*Born after 1956 and never fully vaccinated | |||
*Health care workers | |||
| | |||
*[[History]] and [[examination]] | |||
*[[PCR]] for [[Measles]]-specific [[IgM|IgM antibody]] | |||
*[[PCR]] for [[Measles]] [[RNA]] | |||
| | |||
*[[Oral cavity]] | |||
*[[Skin]] | |||
*[[Respiratory tract]] | |||
*[[Eyes]] | |||
*[[Throat]] | |||
| | |||
*Caused by [[Morbillivirus]] | |||
*Primary site of infection is the [[respiratory epithelium]] of the [[nasopharynx]] | |||
*Transmitted in [[respiratory secretions]], via [[aerosol droplets]] containing [[Virus|virus particles]] | |||
|[[File:Koplikspot1a.jpg|Koplick spots (Measles)|400x400px]] | |||
|}</small></small> | |||
</div> | |||
==References== | |||
{{reflist|2}} | |||
Revision as of 20:20, 28 August 2017
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: João André Alves Silva, M.D. [2] Aysha Anwar, M.B.B.S[3]
|
Syphilis Microchapters | |
|
Diagnosis | |
|
Treatment | |
|
Case Studies | |
|
Syphilis differential diagnosis On the Web | |
|
American Roentgen Ray Society Images of Syphilis differential diagnosis | |
|
Risk calculators and risk factors for Syphilis differential diagnosis | |
Overview
Syphilis is named as the "Great Imitator" because the symptomatology and physical exam findings of syphilis in different stages mimicks large variety of other diseases. Syphilis must be differentiated from other common diseases that cause rash such as measles, rubella, Kawasaki disease , and mononucleosis. Syphilis also has overlapping symptoms with the other genital infections such as chancroid, condyloma acuminata, genital warts, herpes simplex, and herpes zoster.[1][2][3][4][5]
Differentiating Syphilis from other Diseases
Syphilis is named as a "great imitator" because symptomatology and physical exam findings of syphilis in different stages mimicks large variety of other diseases.[1][2][3][4][5][6][7][8][9][10][8][11][12][13][14][15][16][17]
| Stage of Syphilis | Differential diagnosis | Findings |
|---|---|---|
| Primary | Herpes simplex(1,2) | Presents as multiple, round, superficial oral and genital ulcers which are painful.[2] Adults with non-typical presentation are more difficult to diagnose. However, prodromal symptoms that occur before the appearance of herpetic lesions helps to differentiate HSV from other conditions with similar symptoms like allergic stomatitis. Genital herpes can be more difficult to diagnose than oral herpes since most genital herpes/HSV-2-infected persons have no classical signs and symptoms.[2] |
| Granuloma inguinale | Commonly characterized as painless, progressive ulcerative lesions without regional lymphadenopathy. The lesions are highly vascular and bleed easily on contact.[3] | |
| Chancroid | Characterized by painful sores on the genitalia.[4] | |
| Lymphogranuloma venereum | Self-limited genital ulcer or papule with tender inguinal or femoral lymphadenopathy.[5][6] | |
| Condyloma acuminatum | Presents as warty lesions in the form of clusters and can be very tiny or can spread into large masses in the genital or penile area.[7][18][19] | |
| Urethritis | Discharge (milky or pus-like) from the penis, stinging or burning during urination, itching, tingling, burning or irritation inside the penis. | |
| Cystitis | Presents as abnormal urine color (cloudy), blood in the urine, frequent urination or urgent need to urinate, painful or burning urination, pressure in the lower pelvis or back, flank pain, back pain, nausea, vomiting, and chills | |
| Candidiasis | Presents as redness, itching and discomfort of affected area.[20][21] | |
| Other STIs | Such as Chlamydia, Gonorrhea, and Trichomonas vaginalis | |
| Secondary | HIV | Acute illness present with fever, lymphadenopathy, rash, fatigue, and myalgia. AIDS classically presents with weight loss, night sweats, fatigue, diarrhea, mucosal sores, cough, and cognitive and neurological deficits. |
| Pityriasis rosea | Pink and flaky oval-shaped rash followed by clusters of smaller, more numerous patches of rash. May be accompanied by headache, fever, nausea and fatigue. | |
| Viral exanthem | Such as measles, mumps, chicken pox, cytomegalovirus, coxsackie virus, rubella. Findings may include fever, rash, and constitutional symptoms.[22] | |
| Scarlet fever | Presenting symptoms include fever, punctate red macules on the hard and soft palate and uvula (Forchheimer's spots), bright red tongue with a "strawberry" appearance, sore throat and headache and lymphadenopathy. | |
| Insect bite | Immediate skin reaction often resulting in a rash and swelling in the injured area, often with formation of vesicles. | |
| Mononucleosis | Common symptoms include low-grade fever without chills, sore throat, white patches on tonsils and back of the throat, muscle weakness and sometime extreme fatigue, tender lymphadenopathy, petechial hemorrhage and skin rash. | |
| Rocky mountain spotted fever | Symptoms may include maculopapular rash, petechial rash, abdominal pain and joint pain. | |
| Rickettsialpox | Overlapping symptoms with secondary syphilis may include flu-like illness including fever, chills, weakness and muscle pain but the most distinctive symptom is the rash that breaks out, spanning the person's entire body. | |
| Kawasaki disease | Commonly presents with high and persistent fever, red mucous membranes in mouth, "strawberry tongue", swollen lymph nodes and skin rash in early disease, with peeling off of the skin of the hands, feet and genital area | |
| Yaws | Tropical infection of the skin, bones and joints caused by the spirochete bacterium Treponema pertenue | |
| Stevens-Johnson syndrome | Symptoms may include fever, sore throat and fatigue. Commonly presents ulcers and other lesions in the mucous membranes, almost always in the mouth and lips but also in the genital and anal regions. | |
| Tertiary | Brain tumour | Findings which may overlap with neurosyphilis include headache,seizures, visual changes and personality changes.[8] |
| Other causes of seizures | Neurosyphilitic disease can present with seizures and must be differentiated from other causes of seizures. | |
| Other causes of stroke[9] | Presents as weakness, sensory loss, gait abnormality and cranial nerve damage. | |
| Meningococcemia | Rash, petechiae, headache, confusion, and stiff neck, high fever, mental status changes, nausea and vomiting.[10] | |
| Multiple sclerosis | May presents as changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty in moving, difficulties with coordination and balance (ataxia), problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis, or diplopia), fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology (mainly depression).[23] | |
| Other causes of meningitis][8][11] | Such as bacterial, fungal and viral meningitis. It commonly presents with headache, nuchal rigidity, fever, petechiae and altered mental status. | |
| Psychosis | Presents as hallucinations, delusions, auditory hallucinations, and flat or blunted affect and emotion, poverty of speech (alogia), anhedonia, and lack of motivation.[24] | |
| Vasculitides | Cardiovasular syphilis may present as aortitis and aortic aneurysm. Overlapping symptoms with other vasculitis may include back pain, fever, abdominal pain, chest pain, shortness of breath, fatigue, arm and leg weakness, lightheadedness, dizziness, fainting, and headaches.[25][13][14] | |
| Other causes of congestive heart failure | Presenting symptoms include dizziness, dyspnea on ordinary exertion or greater shortness of breath with usual activities, fainting, fatigue, hemoptysis or frothy sputum, nocturia or urination during the night, nocturnal cough, orthopnea or sleeping on pillows, palpitations or extra heart beats, paroxysmal nocturnal dyspnea or awakening at night with shortness of breath, shortness of breath, syncope or passing out and weakness. | |
| Other causes of glomerulonephritis | May presents as blood in the urine (dark, rust-colored, or brown urine), foamy urine (due to excess protein in the urine), swelling (edema) of the face, eyes, ankles, feet, legs, or abdomen. | |
| Other causes of arthritis | Gummatous lesions of syphilis in joints may present as joint pains and stiffness. | |
| Other causes of lymphadenitis | May present as fever, myalgia, weight loss, and lymph node enlargement.[15] | |
| Other causes of hepatitis | Common presenting symptoms may include dark urine, fatigue, weight loss, fever usually low-grade, itching, jaundice (yellowing of the skin or eyes), loss of appetite, nausea and vomiting.[16] | |
| Other causes of nephrotic syndrome | Presents as proteinuria, edema, weight gain, fatigue and dyspnea. | |
| Other causes of uveitis | Symptoms of uveitis include eye pain, eye redness, and photophobia. Intermediate, posterior, and panuveitis commonly present with floaters, blurry vision, and impaired vision.[15][17] |
Differentiating secondary syphilis from other diseases
- Secondary siphilis should be differentiated from other diseases causing erythamosquamous rash. the differentials include the following:
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[26] |
|
|
||
| Pityriasis rosea[27] |
|
|
||
| Pityriasis lichenoides chronica |
|
|
||
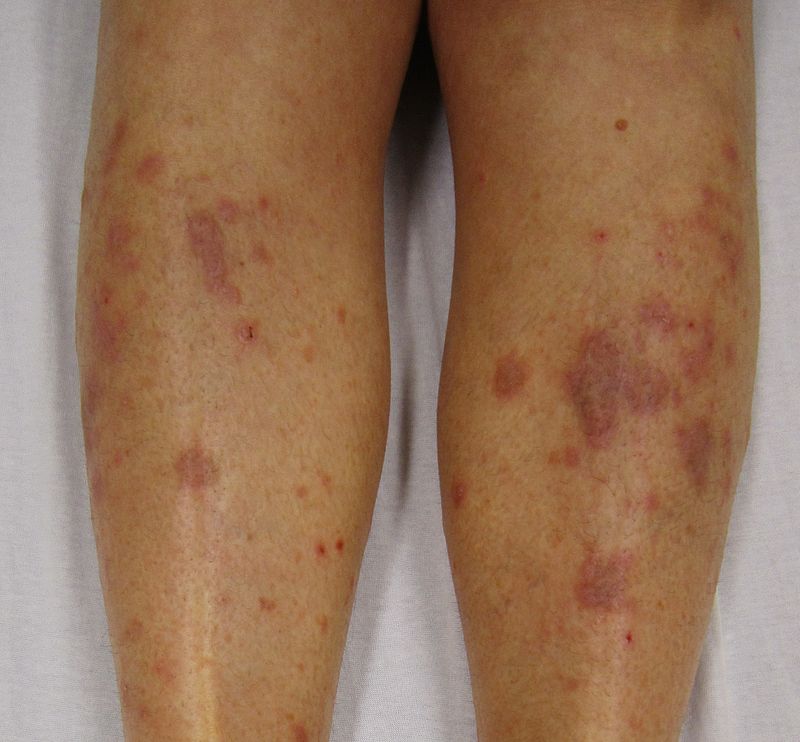
| Nummular dermatitis[30] |
|
|
|
|
| Secondary syphilis[31] |
|
|||
| Bowen’s disease[32] |
|
|
||
| Exanthematous pustulosis[34] |
|
|
||
| Hypertrophic lichen planus[36] |
|
|
|
|
| Sneddon–Wilkinson disease[38] |
|
|
||
| Small plaque parapsoriasis[42] |
|
|
|
|
| Intertrigo[44] |
|
|
||
| Langerhans cell histiocytosis[45] |
|
|
|
|
| Tinea manuum/pedum/capitis[49] |
|
|
|
|
| Seborrheic dermatitis |
|
|
Syphilitic oral lesions must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
| |||
| Leukoplakia |
|
|
|
|
| |
| Melanoma |
|
|
|
|
| |
| Fordyce spots |
|
|
|
|
| |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
| ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
| ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[54] |
|
|
|
| ||
| Coxsackie virus |
|
|
| |||
| Chicken pox |
|
|
|
|
| |
| Measles |
|
|
|
| ||
References
- ↑ 1.0 1.1 Carlson JA, Dabiri G, Cribier B, Sell S (2011). "The immunopathobiology of syphilis: the manifestations and course of syphilis are determined by the level of delayed-type hypersensitivity". Am J Dermatopathol. 33 (5): 433–60. doi:10.1097/DAD.0b013e3181e8b587. PMC 3690623. PMID 21694502.
- ↑ 2.0 2.1 2.2 2.3 Fatahzadeh M, Schwartz RA (2007). "Human herpes simplex virus infections: epidemiology, pathogenesis, symptomatology, diagnosis, and management". J. Am. Acad. Dermatol. 57 (5): 737–63, quiz 764–6. doi:10.1016/j.jaad.2007.06.027. PMID 17939933.
- ↑ 3.0 3.1 3.2 O'Farrell N (2002). "Donovanosis". Sexually Transmitted Infections. 78 (6): 452–7. PMC 1758360. PMID 12473810.
- ↑ 4.0 4.1 4.2 Coovadia YM, Kharsany A, Hoosen A (1985). "The microbial aetiology of genital ulcers in black men in Durban, South Africa". Genitourin Med. 61 (4): 266–9. PMC 1011828. PMID 2991120.
- ↑ 5.0 5.1 5.2 Mabey D, Peeling RW (2002). "Lymphogranuloma venereum". Sexually Transmitted Infections. 78 (2): 90–2. PMC 1744436. PMID 12081191.
- ↑ 6.0 6.1 Workowski, KA.; Berman, S.; Workowski, KA.; Bauer, H.; Bachman, L.; Burstein, G.; Eckert, L.; Geisler, WM.; Ghanem, K. (2010). "Sexually transmitted diseases treatment guidelines, 2010". MMWR Recomm Rep. 59 (RR-12): 1–110. PMID 21160459. Unknown parameter
|month=ignored (help) - ↑ 7.0 7.1 F. G. Bruins, F. J. A. van Deudekom & H. J. C. de Vries (2015). "Syphilitic condylomata lata mimicking anogenital warts". BMJ (Clinical research ed.). 350: h1259. PMID 25784708.
- ↑ 8.0 8.1 8.2 8.3 Berger JR, Dean D (2014). "Neurosyphilis". Handb Clin Neurol. 121: 1461–72. doi:10.1016/B978-0-7020-4088-7.00098-5. PMID 24365430.
- ↑ 9.0 9.1 Hotson JR (1981). "Modern neurosyphilis: a partially treated chronic meningitis". West J Med. 135 (3): 191–200. PMC 1273113. PMID 7340118.
- ↑ 10.0 10.1 Lukehart SA, Hook EW, Baker-Zander SA, Collier AC, Critchlow CW, Handsfield HH (1988). "Invasion of the central nervous system by Treponema pallidum: implications for diagnosis and treatment". Ann Intern Med. 109 (11): 855–62. PMID 3056164.
- ↑ 11.0 11.1 Simon RP (1985). "Neurosyphilis". Arch Neurol. 42 (6): 606–13. PMID 3890813.
- ↑ Suresh E (2006). "Diagnostic approach to patients with suspected vasculitis". Postgrad Med J. 82 (970): 483–8. doi:10.1136/pgmj.2005.042648. PMC 2585712. PMID 16891436.
- ↑ 13.0 13.1 Sapira JD (1981 Apr). ""Quincke, de Musset, Duroziez, and Hill: some aortic regurgitations"". South Med J. 74 (4): 459–67. Check date values in:
|date=(help) - ↑ 14.0 14.1 Pugh PJ, Grech ED (2002). "Images in clinical medicine. Syphilitic aortitis". N Engl J Med. 346 (9): 676. doi:10.1056/NEJMicm010343. PMID 11870245.
- ↑ 15.0 15.1 15.2 J. Deschenes, C. D. Seamone & M. G. Baines (1992). "Acquired ocular syphilis: diagnosis and treatment". Annals of ophthalmology. 24 (4): 134–138. PMID 1590633. Unknown parameter
|month=ignored (help) - ↑ 16.0 16.1 Young MF, Sanowski RA, Manne RA (1992). "Syphilitic hepatitis". Journal of Clinical Gastroenterology. 15 (2): 174–6. PMID 1401840.
- ↑ 17.0 17.1 T. F. Jr Schlaegel & S. F. Kao (1982). "A review (1970-1980) of 28 presumptive cases of syphilitic uveitis". American journal of ophthalmology. 93 (4): 412–414. PMID 7072806. Unknown parameter
|month=ignored (help) - ↑ Baron, Samuel (1996). Medical microbiology. Galveston, Tex: University of Texas Medical Branch at Galveston. ISBN 0-9631172-1-1.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
- ↑ Baron, Samuel (1996). Medical microbiology. Galveston, Tex: University of Texas Medical Branch at Galveston. ISBN 0-9631172-1-1.
- ↑ Mandell, Gerald (2010). Mandell, Douglas, and Bennett's principles and practice of infectious diseases. Philadelphia, PA: Churchill Livingstone/Elsevier. ISBN 978-0-443-06839-3.
- ↑ Kang, Jin Han. "Febrile Illness with Skin Rashes." Infection & chemotherapy 47.3 (2015): 155-166.
- ↑ Scolding N (2001). "The differential diagnosis of multiple sclerosis". Journal of Neurology, Neurosurgery, and Psychiatry. 71 Suppl 2: ii9–15. PMC 1765571. PMID 11701778.
- ↑ Friedrich F, Geusau A, Greisenegger S, Ossege M, Aigner M (2009). "Manifest psychosis in neurosyphilis". General Hospital Psychiatry. 31 (4): 379–81. doi:10.1016/j.genhosppsych.2008.09.010. PMID 19555800.
- ↑ K. Doi, T. Kasaba & Y. Kosaka (1989). "[A comparative study of the depressive effects of halothane and isoflurane on medullary respiratory neurons in cats]". Masui. The Japanese journal of anesthesiology. 38 (11): 1427–1437. PMID 2585712. Unknown parameter
|month=ignored (help) - ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.