ST elevation myocardial infarction classification
| Myocardial infarction | |
 | |
|---|---|
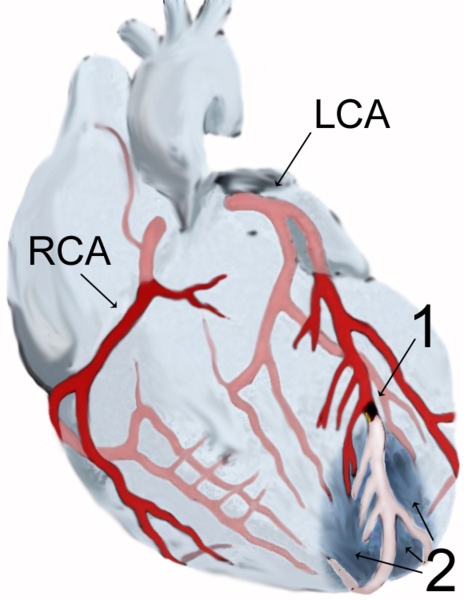
| Diagram of a myocardial infarction (2) of the tip of the anterior wall of the heart (an apical infarct) after occlusion (1) of a branch of the left coronary artery (LCA, right coronary artery = RCA). | |
| ICD-10 | I21-I22 |
| ICD-9 | 410 |
| DiseasesDB | 8664 |
| MedlinePlus | 000195 |
| eMedicine | med/1567 emerg/327 ped/2520 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editors-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Classification
Acute myocardial infarction is a type of acute coronary syndrome, which is most frequently (but not always) a manifestation of coronary artery disease. The acute coronary syndromes include ST segment elevation myocardial infarction (STEMI), non-ST segment elevation myocardial infarction (NSTEMI), and unstable angina (UA).
Depending on the location of the obstruction in the coronary circulation, different zones of the heart can become injured. Using the anatomical terms of location, one can describe anterior, inferior, lateral, apical and septal infarctions (and combinations, such as anteroinferior, anterolateral, and so on).[1] For example, an occlusion of the left anterior descending coronary artery will result in an anterior wall myocardial infarct.[2]
Another distinction is whether a MI is subendocardial, affecting only the inner third to one half of the heart muscle, or transmural, damaging (almost) the entire wall of the heart.[3] The inner part of the heart muscle is more vulnerable to oxygen shortage, because the coronary arteries run inward from the epicardium to the endocardium, and because the blood flow through the heart muscle is hindered by the heart contraction.[2]
The phrases transmural and subendocardial infarction used to be considered synonymous with Q-wave and non-Q-wave myocardial infarction respectively, based on the presence or absence of Q waves on the ECG. It has since been shown that there is no clear correlation between the presence of Q waves with a transmural infarction and the absence of Q waves with a subendocardial infarction,[4] but Q waves are associated with larger infarctions, while the lack of Q waves is associated with smaller infarctions. The presence or absence of Q-waves also has clinical importance,[5] with improved outcomes associated with a lack of Q waves.[6]
The phrase "massive heart attack" is not a recognized medical term.
See also
- acute coronary syndrome
- angina
- Cardiac arrest
- coronary thrombosis
- Hibernating myocardium
- Stunned myocardium
- Ventricular remodeling
References
- ↑ "Dorland's Illustrated Medical Dictionary". WB Saunders, an Elsevier imprint. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - ↑ 2.0 2.1 Rubin's Pathology - Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. 2001. p. 525. ISBN 0-7817-4733-3. Unknown parameter
|coauthors=ignored (help) - ↑ Rubin's Pathology - Clinicopathological Foundations of Medicine. Maryland: Lippincott Williams & Wilkins. 2001. pp. p. 545. ISBN 0-7817-4733-3. Unknown parameter
|coauthors=ignored (help) - ↑ Moon JC, De Arenaza DP, Elkington AG, Taneja AK, John AS, Wang D, Janardhanan R, Senior R, Lahiri A, Poole-Wilson PA, Pennell DJ. (2004). "The pathologic basis of Q-wave and non-Q-wave myocardial infarction: a cardiovascular magnetic resonance study". J Am Coll Cardiol. 44 (3): 554–60. PMID 15358019.
- ↑ Yang H, Pu M, Rodriguez D, Underwood D, Griffin BP, Kalahasti V, Thomas JD, Brunken RC (2004). "Ischemic and viable myocardium in patients with non-Q-wave or Q-wave myocardial infarction and left ventricular dysfunction: a clinical study using positron emission tomography, echocardiography, and electrocardiography". J Am Coll Cardiol. 43 (4): 592–8. PMID 14975469.
- ↑ Goodman SG, Langer A, Ross AM, Wildermann NM, Barbagelata A, Sgarbossa EB, Wagner GS, Granger CB, Califf RM, Topol EJ, Simoons ML, Armstrong PW. (1998). "Non-Q-wave versus Q-wave myocardial infarction after thrombolytic therapy: angiographic and prognostic insights from the global utilization of streptokinase and tissue plasminogen activator for occluded coronary arteries-I angiographic substudy. GUSTO-I Angiographic Investigators". Circulation. 97 (5): 444–50. PMID 9490238.
External links
- The MD TV: Comments on Hot Topics, State of the Art Presentations in Cardiovascular Medicine, Expert Reviews on Cardiovascular Research
- Clinical Trial Results: An up to dated resource of Cardiovascular Research
- Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack - based on information of the Framingham Heart Study, from the United States National Heart, Lung and Blood Institute
- Heart Attack - overview of resources from MedlinePlus.
- Heart Attack Warning Signals from the Heart and Stroke Foundation of Canada
- Regional PCI for STEMI Resource Center - Evidence based online resource center for the development of regional PCI networks for acute STEMI
- STEMI Systems - Articles, profiles, and reviews of the latest publications involved in STEMI care. Quarterly newsletter.
- American College of Cardiology (ACC) Door to Balloon (D2B) Initiative.
- American Heart Association's Heart Attack web site - Information and resources for preventing, recognizing and treating heart attack.