Pre-excitation syndrome: Difference between revisions
No edit summary |
|||
| Line 1: | Line 1: | ||
{{CMG}} | {{CMG}}, Dr. Shivam Singla, M.B.B.S | ||
{{EH}} | {{EH}} | ||
| Line 15: | Line 15: | ||
* They found the association of these conditions with a small risk of sudden cardiac death | * They found the association of these conditions with a small risk of sudden cardiac death | ||
* Incidence 0.1 – 3.0 per 1000 | * Incidence 0.1 – 3.0 per 1000 | ||
*LGL syndrome is rare Man > woman. The commonest type of tacchyarrhythmias= AVRT (80%) frequency of PSVT is increased with age (10/100 in 20-40 yo VS 36/100 in >60 yo) In patients with history of recurrent tacchyarrhythmia, prognosis is still good; SCD is only 0.1% (rare) | |||
<br /> | |||
== Risk Factors[edit | edit source] == | == Risk Factors[edit | edit source] == | ||
| Line 37: | Line 39: | ||
*In [[Wolff-Parkinson-White syndrome|WPW]] syndrome which is a type of pre-excitation syndrome the abnormal conduction pathways are called [[Bundle of Kent]] or AV bypass tract. | *In [[Wolff-Parkinson-White syndrome|WPW]] syndrome which is a type of pre-excitation syndrome the abnormal conduction pathways are called [[Bundle of Kent]] or AV bypass tract. | ||
*The accessory pathways facilitates formation of [[Tachyarrhythmias]] by mainly forming reentry circuit , termed as <u>AVRT</u>. Even | *The accessory pathways facilitates formation of [[Tachyarrhythmias]] by mainly forming reentry circuit , termed as <u>AVRT</u> (80%). Even in cases of direct conduction through the accessory pathways from A to V ( Bypassing AV node) there can be resultant formation of [[Tachyarrhythmia|Tachyarrhythmias]], seen most frequently in condition of A. Fib with RVR. | ||
| Line 98: | Line 100: | ||
* May result in variation in ventricular morphology | * May result in variation in ventricular morphology | ||
* Reentry tachycardia typically has LBBB morphology | * Reentry tachycardia typically has LBBB morphology | ||
== Clinical Features[edit | edit source] == | == Clinical Features[edit | edit source] == | ||
*People with Pre- Excitation syndromes | *People with Pre- Excitation syndromes may be asymptomatic , however the individual may experience following symptoms | ||
**'''Palpitations''' | **'''Palpitations''' | ||
**'''Dizziness''' or lightheadedness. | **'''Dizziness''' or lightheadedness. | ||
Revision as of 12:27, 3 June 2020
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1], Dr. Shivam Singla, M.B.B.S
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview[edit | edit source]
Pre-excitation syndrome is a condition where the the ventricles of the heart become depolarized too early, which leads to their partially premature contraction. Normally, the atria (chambers taking venous blood) and the ventriculi (chambers pro-pulsing blood towards organs) are electrically isolated, and only electrical passage exists at "atrioventricular node". In all pre-excitation syndromes, there is at least one more conductive pathway is present. Physiologically, the electrical depolarization wave 'waits' in atrioventricular node to allow atria contract before ventriculi. However, there is no such property exists in abnormal pathway, so electrical stimulus passes to ventricle by this tracts far before normal atrioventricular-his system, and ventricles are depolarized (excited) before (pre-) normal conduction system. The term pre-excitation derives from this condition.
It is usually caused by a secondary conduction pathway (other than the bundle of His)
Epidemiology and Demographics[edit | edit source]
- First described by Louis Wolff, John Parkinson and Paul Dudley White in 1930
- They found the association of these conditions with a small risk of sudden cardiac death
- Incidence 0.1 – 3.0 per 1000
- LGL syndrome is rare Man > woman. The commonest type of tacchyarrhythmias= AVRT (80%) frequency of PSVT is increased with age (10/100 in 20-40 yo VS 36/100 in >60 yo) In patients with history of recurrent tacchyarrhythmia, prognosis is still good; SCD is only 0.1% (rare)
Risk Factors[edit | edit source]
- High risk population for sudden cardiac death in Wolff-Parkinson-White syndrome include:
- Policemen
- Sports player/Athletes
- Firemen
- Air pilots Risk factors for the development of atrial fibrillation in WPW syndrome include:
- Gender- Male
- Age (Peak age 30-50 yrs)
- Past history of syncope
Pathophysiology [edit | edit source]
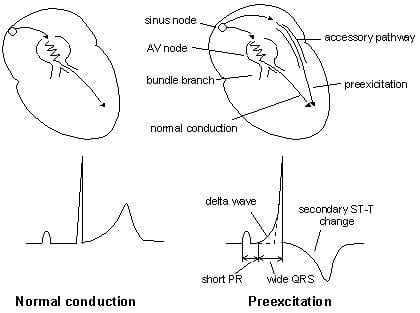
Pathophysiology of Pre-Excitation syndromes
- Pre-excitation refers to the early activation of the ventricles as a result of impulses bypassing the AV node via an accessory pathway. The latter are abnormal conduction pathways formed during cardiac development. These can conduct impulses either
- towards ventricles (Anterograde conduction, rarely seen) ,
- Away from the ventricles (Retrograde conduction, in approx 15%),
- in both the directions ( Majority of cases).
- In WPW syndrome which is a type of pre-excitation syndrome the abnormal conduction pathways are called Bundle of Kent or AV bypass tract.
- The accessory pathways facilitates formation of Tachyarrhythmias by mainly forming reentry circuit , termed as AVRT (80%). Even in cases of direct conduction through the accessory pathways from A to V ( Bypassing AV node) there can be resultant formation of Tachyarrhythmias, seen most frequently in condition of A. Fib with RVR.
Classification[edit | edit source]
| Type | Conduction pathway | PR interval | QRS interval | Delta wave? |
| Wolff-Parkinson-White syndrome | Bundle of Kent (atria to ventricles) | short | long | yes |
| Lown-Ganong-Levine syndrome | "James bundle" (atria to bundle of His) | short | normal | no |
| Mahaim-type | Mahaim fibers | normal | long |
WPW Syndrome
WPW is a combination of presence of congenital accessory pathways along with episodic tachyarrhythmias. Here the accessory pathways are reffered to as Bundle of Kent or AV bypass tracts.
The features of pre excitation are subtle, intermittent and are aggravated by increase in vagal tone ( Valsalva maneuver, AV blockage by drugs).
- ECG Features of WPW
- Shortened PR interval (Less than 120ms)
- Delta wave – slow/slurring in the rise of initial portion of the QRS
- Widening of QRS complex
- ST Segment and T wave discordant changes – i.e. in the opposite direction to the major component of the QRS complex
- WPW is mainly categorized as type A or B.
- Type A: positive delta wave in all precordial leads with R/S > 1 in V1
- Type B: negative delta wave in leads V1 and V2
Lown-Ganong-Levine (LGL) Syndrome
Here the Accessory pathway are composed of James fibres.
ECG features:
- PR interval <120ms
- Normal QRS morphology
The important point to be noted is that this tern is not relevant or shouldn't be used in the absence of paroxysmal tachycardia. Its existence is disputed and it may not exist.
Mahaim-Type Pre-excitation
Right sided accessory pathways connecting either AV node to ventricles, fascicles to ventricles, or atria to fascicles
ECG features:
- Sinus rhythm ECG may be normal
- May result in variation in ventricular morphology
- Reentry tachycardia typically has LBBB morphology
Clinical Features[edit | edit source]
- People with Pre- Excitation syndromes may be asymptomatic , however the individual may experience following symptoms
- Palpitations
- Dizziness or lightheadedness.
- Shortness of breath.
- Chest pain
- Fatigue.
- Anxiety.
- Fainting
- Difficulty breathing
Diagnosis and Treatment [edit | edit source]
Atrioventricular Reentry Tachycardia's (AVRT)
AVRT is a form of PSVT. Reentry circuit results from the combination of signal transduction from normal conduction system and accessory pathway.
- During tachyarrythmias, the accessory pathway forms part of the reentry circuit that results in the disappearance of features of tachyarrythmias..
- AVRT are further divided into
- Orthodromic or Antidromic conduction based on ECG morphology and direction of formation of re-entry circuit.
1) AVRT with Orthodromic Conduction
In this the anterograde conduction occurs via the AV node and retrograde conduction occurs via accessory pathway.
ECG features of AVRT with orthodromic conduction
- Rate usually 200 – 300 bpm
- P waves may be buried in QRS complex or retrograde
- QRS Complex usually <120 ms unless pre-existing bundle branch block, or rate-related aberrant conduction
- QRS Alternans – phasic variation in QRS amplitude associated with AVNRT and AVRT, distinguished from electrical alterns by a normal QRS amplitude
- T wave inversion common
- ST segment depression
Treatment Of Orthodromic AVRT:- Hemodynamically Unstable patients( Low BP, Altered mental state, pulmonary edema)- Synchronized DC Cardioversion. In patients who are hemodynamically stable- Vagal maneuvers, Adenosine, CCB and DC cardioversion as a last resort only if patient not responding to medical therapy.
2) AVRT with Antidromic Conduction
In this the anterograde conduction occurs via the accessory pathway and retrograde conduction via the AV node. Occurring only in app. 5% of patients with WPW.
ECG features are:
- Rate usually 200 – 300 bpm.
- Wide QRS complexes due to abnormal accessory pathway ventricular depolarisation.
- Due to wide complex, Commonly mistaken for Ventricular Tachycardia.
Treatment of antidromic AVRT: Hemodynamically unstable patients:- Urgent synchronized DC cardio version. Hemodynamically stable patients:- Amiodarone, procainamide or ibutilide.
3) Atrial Fib/Atrial Flutter in WPW
- In 20% of the patients WPW Atrial fibrillation can occur and in approx 7% of patients with WPW atrial flutter can occur. Accessory pathways plays major role by allowing the rapid conduction of impulses directly to the ventricles without involving AV node, in extreme cases may lead to VT or VF.
ECG features
- Rate > 200 bpm
- Irregular rhythm
- Wide QRS complexes due to abnormal ventricular depolarisation via accessory pathway
- QRS Complexes change in shape and morphology
- Axis remains stable unlike Polymorphic VT
- Atrial Flutter presents with same features as atrial fibrillation in WPW except rhythm is regular and commonly mistaken for VT
Treatment of AF with WPW:- Hemodynamically unstable patients: Urgent synchronized DC cardioversion. Hemodynamically stable patients:- Procainamide or ibutilide. Caution: Adenosine, CCB, Beta blockers results in increase in conduction via accessory pathway which results in worsening of condition with possible degeneration into VT or VF
Differentiating from other Diseases[edit | edit source]
- Pre-Excitation syndrome must be differentiated from other diseases. The conditions that needs to be ruled out while making the diagnosis are:
- Atrial Flutter
- Atrial Fibrillation
- Atrioventricular Nodal Reentry Tachycardia
- Atrial Tachycardia
- Ventricular Tachycardia
- Paroxysmal Supraventricular Tachycardia
- Ebstein Anomaly
- Genetics of Glycogen-Storage Disease Type I
- Genetics of Glycogen-Storage Disease Type II (Pompe Disease)
- Lown-Ganong-Levine Syndrome
- Syncope
- Danon Disease