Pulmonic regurgitation pathophysiology
|
Pulmonic regurgitation Microchapters |
|
Diagnosis |
|---|
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Aravind Kuchkuntla, M.B.B.S[2], Aysha Anwar, M.B.B.S[3], Javaria Anwer M.D.[4]
Overview
Pulmonary valve is located at the junction of the right ventricular outflow tract and pulmonary artery. Three equal-sized, semilunar cusps or leaflets make up the pulmonary valve. Pulmonary valve opens during right ventricular systole and closes during right ventricular diastole. Pulmonary regurgitation (PR) may be caused by an acquired alteration in the valvular morphology, idiopathic dilatation of the pulmonary artery (IDPA), pulmonic valve ring dilatation, congenital absence or malformation of the valve, and increasing regurgitation causing right ventricular volume overload. The pathophysiologic mechanism of pulmonic regurgitation includes right ventricular overload resulting in the right ventricular remodeling and progressive decline in function. The rate of decline in right ventricular systolic function is affected by associated conditions such as peripheral pulmonary artery stenosis and pulmonary hypertension which further increase the severity of pulmonary regurgitation. Among patients with severe PR, the gene expression pattern of GRK2 and β2-adrenoceptor (molecular markers of cardiac dysfunction) has been reported to be altered. Isolated PR is uncommon and is usually demonstrated with other valvular abnormalities or in certain conditions. Conditions associated include TOF, rheumatic heart disease and syphilis. On gross pathology vegetative lesions on the pulmonic valve leaflets may be observed among patients with acquired alteration in the valvular leaflet morphology.
Pathophysiology
Anatomy of and physiology of pulmonic valve
- Location: Pulmonary valve is located at the junction of the right ventricular outflow tract and pulmonary artery. Pulmonic valve lies anterior and superior to the aortic valve at third intercostal space level. Infundibulum of the right ventricle separates it from tricuspid valve.[1]

- Structure: Three equal sized, semilunar cusps or leaflets make up the pulmonary valve. Based on the corresponding aortic valve, the cusps are named right, left and anterior.[2] [2]
- The three cusps are joined by commissures and the cusps are thinner when compared to the aortic valve, due to a low pressure in the right ventricle.[2]
- Histologically, the pulmonary valve consists of stratified extracellular matrix compartments. The layers constitute fibrosa, spongiosa and ventricularis.[3]
- The diameter of pulmonic valve is demonstrated to be closely related to the body size. For adult men (>17 years age) mean pulmonary valve diameter is 26.2 +/- 2.3 mm and 23.9 +/- 2.2 mm for adult women.[4]
- Physiology: The right ventricle delivers the received blood entirely to the pulmonary circulation every beat, maintaining optimum pressure.[5] Pulmonary valve opens during right ventricular systole allowing the deoxygenated blood to be delivered to the lungs. [2] During the right ventricular diastole the pulmonary valves close completely to prevent regurgitation (back flow) of the blood into the right ventricle.[2]
- The closure of the pulmonic valve contributes to the P2 component of the second heart sound (S2).
Pathogenesis
The pathogenesis of pulmonic regurgitation involves the following mechanisms:[6][7]
Dynamics of regurgitation
- The diastolic pressure difference between main pulmonary artery (MPA and right ventricle (RV) is usually very small and steers the pulmonic regurgitation. The right ventricular stiffness due to right ventricular hypertrophy (such as in Tetralogy of Fallot and fibrosis) increases the ventricular diastolic pressure. Increased ventricular diastolic pressure decreases the gradient causing regurgitation. A slight increase in the intrathoracic pressure (such as among ventilated patients) can accentuate PR considerably.[8]
- Along with diastolic pressure difference between right ventricle and pulmonary artery, the degree/ severity/ volume of regurgitant jet is dependent on:[9][10]
- Size/ area of the regurgitant orifice
- Afterload of the right ventricle/ capacitance of pulmonary arteries
- Right ventricle diastolic compliance
- Duration of right ventricular diastole
- Torricelli principle sums up some of the factors influencing regurgitant volume:[10]
PR volume = regurgitant orifice area · constant · diastolic time · mean diastolic pressure difference between the MPA and RV.(P2−P1)0.5.
Acquired alteration in the valvular morphology[11][10]
- The most common cause of PR is post repair of TOF to relieve right ventricle outflow tract (RVOT) obstruction. The valvular lesion is thought to be due to the disruption of pulmonary valve's morphological integrity. In a TOF patient even after the RVOT obstruction relief, the right ventricle (RV) is hypertrophied and pulmonary arteries are usually hypoplastic, both demonstrating low compliance. Among children, tachycardia leads to shorter duration diastoles.
Regurgitation is avoided despite large regurgitation orifice due to Torricelli principle. Progressively, an increased size and capacitance of central pulmonary ateries and right ventricular dilatation occurs due to increased RV stroke volume. The changes described progress with age accompanied by a longer duration of diastole and decreased heart rate. This progressively leads to an increase in the degree of PR.
- The development of pulmonic regurgitation due to tophus valvular vegetations has been reported in a case. The patient reported had long-standing cyanotic congenital heart disease and developed hyperuricemia secondary to polycythemia. The possible mechanism of development of the vegetations involved hemodynamic valvular trauma in the setting of sustained hyperuricemia and subsequent dystrophic calcification at primary tophus lesion.

Idiopathic dilatation of the pulmonary artery (IDPA)[12][13][14]
- The exact pathogenesis of dilatation of the pulmonary artery is not fully understood. The demonstration of the disease among pediatric population signals the congenital nature of the etiology. Main pulmonary artery and the origin of its right and left main pulmonary arteries are majorly affected. It is thought that pulmonary artery dilatation is mediated by the unequal division of truncus arteriosus communis. Other proposed mechanisms include maldevelopment of the whole pulmonary tree and the association of hypoplastic aorta with dilated.

Pulmonary valve ring dilatation[16]
A study utilized pulsed doppler echocardiography and cineangiography to identify the significance of pulmonic valve ring dimensions in the development of PR. It reported the ratio of sagittal to the transverse diameter of the pulmonic valve ring to be greater among patients with PR. In patients with PAH the study also demonstrated greater dilatation of the sagittal diameter of the pulmonic valve ring than pulmonary sinus diameter. In the light of the results, the etiology of PR was attributed to the distortion of pulmonic valve ring.
Congenital absence or malformation of the valve[17][12][13][18]
- Absent pulmonary valve syndrome (APVS) is rare and involves developmental abnormality and dysplasia or absolute absence of pulmonary valve cusps. A variable degree of dilatation/aneurysm of the main pulmonary artery always accompanies the disorder.
- It is thought that the development of pulmonary artery aneurysm is mediated by either the congenital weakness or cystic medial degeneration of the pulmonary artery walls. An association between cystic medial degeneration and increased hemodynamic forces then leads to aneurysm formation. Pulmonary artery aneurysms have been associated with structural cardiac and vascular abnormalities, vasculitis, and infection (such as syphilis).
- The pathogenesis of Fallot type (APVS) involves either agenesis of ductus arteriosus or post pulmonary stenotic dilatation due to increased stroke volume.
- Quuadricuspid pulmonary valve is rare but may cause PR. Thick valvular leaflets with decreased mobility without complete closure during diastole may lead to the development of PR.[19]
Increasing regurgitation causing right ventricular volume overload[9]
- Patients with pulmonic regurgitation (PR) develop chronic right ventricular overload resulting in right ventricular remodeling and progressive decline in function. The rate of decline in right ventricular systolic function is also affected by associated conditions such as peripheral pulmonary artery stenosis and pulmonary hypertension which accentuates PR. Among patients with increased pulmonary artery pressure from dysfunction of left ventricle or residual pulmonary artery stenosis the severity of PR is increased. Progressive dilation of the right ventricle results in functional tricuspid regurgitation and increases the risk of developing arrhythmias.
Genetics
- ADAMTS19 has been identified as a novel causative gene for autosomal recessive cardiac valve disease. ADAMTS is a disintegrin and metalloproteinase with thrombospondin motifs protein family. All patients demonstrated anomalies of the aortic and/or pulmonary heart valves, such as thickening of valve leaflets, stenosis and insufficiency.[20][21]
- Among patients with severe pulmonary regurgitation (PR), the gene expression pattern of GRK2 and β2-adrenoceptor ( molecular markers of cardiac dysfunction) has been reported to be altered. The lymphocyte expression of described adrenoceptors and kinases demonstrates neurohumoral changes in heart failure.[22]
- 25% cases of absent pulmonary valve syndrome (APVS) are associated with chromosomal anomalies such as Trisomy 21, Trisomy 13, chromosome 6 and 7 deletions.[23]
- 22q11 micro-deletion has been shown to be associated with 25% cases of APVS.[24]
Associated conditions
Isolated PR is uncommon and is usually demonstrated with other valvular abnormalities or in certain conditions. The most important conditions/diseases associated with PR include:
- TOF: Surgical repair of pulmonic stenosis associated with TOF may lead to PR. Post TOF repair, PR is a common complication.
- Marfan syndrome: Dilatation of pulmonary artery root is one of the established diagnostic criteria of Marfan syndrome.[25] Although other valvular regurgitations are common in Marfan syndrome, pulmonic regurgitation is also possible.
- Rheumatic heart disease: The disease is uncommon among developed countries but developing countries still share the burden of the disease.[26][27]
- Syphilis: Although a rare cause, pulmonary artery dilatation and PAH may be caused by tertiary syphilis. Given the prognostic implications and available treatments, early detection of PAH.[28] Being a sexually transmitted disease (STD), it is important to screen the patient for other STDs.
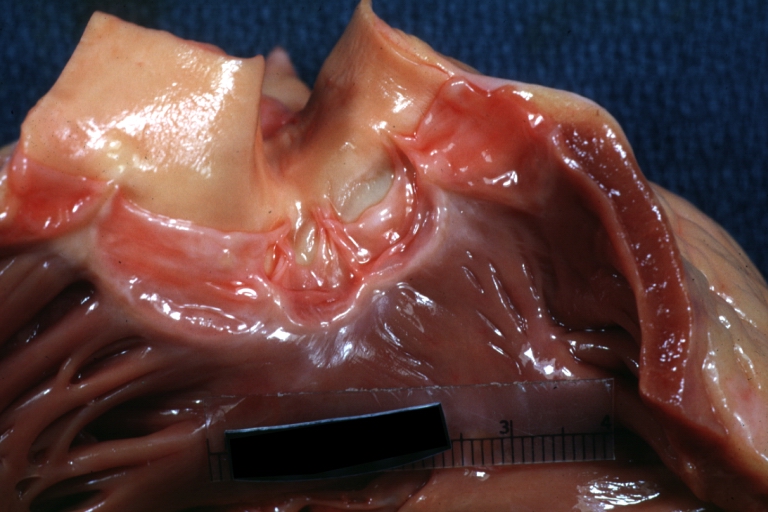
Gross pathology
- On gross pathology vegetative lesions on the pulmonic valve leaflets may be observed among patients with acquired alteration in the valvular leaflet morphology.[11]
Microscopic pathology
- On polarized light microscopy of the material taken from the pulmonic valve, negatively birefringent crystals may be observed in acquired alteration in the valvular leaflet morphology.[11]
References
- ↑ Maganti K, Rigolin VH, Sarano ME, Bonow RO (2010). "Valvular heart disease: diagnosis and management". Mayo Clin Proc. 85 (5): 483–500. doi:10.4065/mcp.2009.0706. PMC 2861980. PMID 20435842.
- ↑ Jump up to: 2.0 2.1 2.2 2.3 2.4 Schmoldt A, Benthe HF, Haberland G, Felt V, Nedvídková J, Hynie S, Mosinger B, Vavrinková M, Järvisalo J, Saris NE (September 1975). "Digitoxin metabolism by rat liver microsomes". Biochem. Pharmacol. 24 (17): 1639–41. doi:10.1016/0006-2952(75)90009-x. PMC 5922622. PMID 10.
- ↑ Combs MD, Yutzey KE (August 2009). "Heart valve development: regulatory networks in development and disease". Circ. Res. 105 (5): 408–21. doi:10.1161/CIRCRESAHA.109.201566. PMC 2777683. PMID 19713546.
- ↑ Capps SB, Elkins RC, Fronk DM (May 2000). "Body surface area as a predictor of aortic and pulmonary valve diameter". J. Thorac. Cardiovasc. Surg. 119 (5): 975–82. doi:10.1016/S0022-5223(00)70092-4. PMID 10788818.
- ↑ Pinsky MR (September 2016). "The right ventricle: interaction with the pulmonary circulation". Crit Care. 20: 266. doi:10.1186/s13054-016-1440-0. PMC 5018168. PMID 27613549.
- ↑ Khavandi, Ali (2014). Essential revision notes for the cardiology KBA. Oxford: Oxford University Press. ISBN 978-0199654901.
- ↑ Khavandi, Ali (2014). Essential revision notes for the cardiology KBA. Oxford: Oxford University Press. ISBN 978-0199654901.
- ↑ Chaturvedi RR, Redington AN (2007). "Pulmonary regurgitation in congenital heart disease". Heart. 93 (7): 880–9. doi:10.1136/hrt.2005.075234. PMC 1994453. PMID 17569817.
- ↑ Jump up to: 9.0 9.1 Bigdelian H, Mardani D, Sedighi M (2015). "The Effect of Pulmonary Valve Replacement (PVR) Surgery on Hemodynamics of Patients Who Underwent Repair of Tetralogy of Fallot (TOF)". J Cardiovasc Thorac Res. 7 (3): 122–5. doi:10.15171/jcvtr.2015.26. PMC 4586599. PMID 26430501.
- ↑ Jump up to: 10.0 10.1 10.2 10.3 Geva T (January 2011). "Repaired tetralogy of Fallot: the roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support". J Cardiovasc Magn Reson. 13: 9. doi:10.1186/1532-429X-13-9. PMC 3036629. PMID 21251297.
- ↑ Jump up to: 11.0 11.1 11.2 Curtiss, E I; Miller, T R; Shapiro, L S (1983). "Pulmonic regurgitation due to valvular tophi". Circulation. 67 (3): 699–701. doi:10.1161/01.CIR.67.3.699. ISSN 0009-7322.
- ↑ Jump up to: 12.0 12.1 Malviya A, Jha PK, Kalita JP, Saikia MK, Mishra A (2017). "Idiopathic dilatation of pulmonary artery: A review". Indian Heart J. 69 (1): 119–124. doi:10.1016/j.ihj.2016.07.009. PMC 5319124. PMID 28228295.
- ↑ Jump up to: 13.0 13.1 Sharma RK, Talwar D, Gupta SK, Bansal S (2016). "Idiopathic dilatation of pulmonary artery". Lung India. 33 (6): 675–677. doi:10.4103/0970-2113.192869. PMC 5112830. PMID 27891002.
- ↑ Segall, S.; Ritter, I. I.; Hwang, W. (1950). "A Case of Marked Dilatation of the Pulmonary Arterial Tree Associated with Mitral Stenosis". Circulation. 1 (4): 777–781. doi:10.1161/01.CIR.1.4.777. ISSN 0009-7322.
- ↑ Deb, Subrato J.; Zehr, Kenton J.; Shields, Raymond C. (2005). "Idiopathic Pulmonary Artery Aneurysm". The Annals of Thoracic Surgery. 80 (4): 1500–1502. doi:10.1016/j.athoracsur.2004.04.011. ISSN 0003-4975.
- ↑ Tsuneyoshi H, Hara K, Takeuchi H, Kashida M, Yamaguchi T, Toide H, Toda E, Machii K (December 1985). "[Pulmonary regurgitation with special reference to the shape of the pulmonary valve ring: a pulsed Doppler and angiographic study]". J Cardiogr (in Japanese). 15 (4): 1145–56. PMID 3841897.
- ↑ Bouzas, Beatriz; Kilner, Philip J.; Gatzoulis, Michael A. (2005). "Pulmonary regurgitation: not a benign lesion". European Heart Journal. 26 (5): 433–439. doi:10.1093/eurheartj/ehi091. ISSN 0195-668X.
- ↑ Deb SJ, Zehr KJ, Shields RC (October 2005). "Idiopathic pulmonary artery aneurysm". Ann. Thorac. Surg. 80 (4): 1500–2. doi:10.1016/j.athoracsur.2004.04.011. PMID 16181901.
- ↑ Kotani A, Nakagawa K, Yamamoto T, Hirano Y, Kimura H, Yamada S, Ikawa H, Ishikawa K (June 2002). "[Quadricuspid pulmonary valve with valvular stenosis and regurgitation identified by transthoracic echocardiography: a case report]". J Cardiol (in Japanese). 39 (6): 313–9. PMID 12094521.
- ↑ Wünnemann, Florian; Ta-Shma, Asaf; Preuss, Christoph; Leclerc, Severine; van Vliet, Patrick Piet; Oneglia, Andrea; Thibeault, Maryse; Nordquist, Emily; Lincoln, Joy; Scharfenberg, Franka; Becker-Pauly, Christoph; Hofmann, Philipp; Hoff, Kirstin; Audain, Enrique; Kramer, Hans-Heiner; Makalowski, Wojciech; Nir, Amiram; Gerety, Sebastian S.; Hurles, Matthew; Comes, Johanna; Fournier, Anne; Osinska, Hanna; Robins, Jeffrey; Pucéat, Michel; Elpeleg, Orly; Hitz, Marc-Phillip; Andelfinger, Gregor (2019). "Loss of ADAMTS19 causes progressive non-syndromic heart valve disease". Nature Genetics. 52 (1): 40–47. doi:10.1038/s41588-019-0536-2. ISSN 1061-4036.
- ↑ Massadeh, Salam; Alhashem, Amal; Laar, Ingrid M.B.H.; Alhabshan, Fahad; Ordonez, Natalia; Alawbathani, Salem; Khan, Suliman; Kabbani, Mohamed S.; Chaikhouni, Farah; Sheereen, Atia; Almohammed, Iman; Alghamdi, Bader; Frohn‐Mulder, Ingrid; Ahmad, Salim; Beetz, Christian; Bauer, Peter; Wessels, Marja W.; Alaamery, Manal; Bertoli‐Avella, Aida M. (2020). "ADAMTS19
‐associated heart valve defects: Novel genetic variants consolidating a recognizable cardiac phenotype". Clinical Genetics. 98 (1): 56–63. doi:10.1111/cge.13760. ISSN 0009-9163. line feed character in
|title=at position 9 (help) - ↑ Rodríguez-Serrano M, Rueda Soriano J, Buendía Fuentes F, Osa Sáez AM, Montó Guillot F, D'Ocon Navaza P, Aguero J, Oliver E, Serrano F, Martínez-Dolz L (July 2019). "Changes in Adrenoceptor and GRK Expression in Patients With Chronic Pulmonary Regurgitation". Rev Esp Cardiol (Engl Ed). 72 (7): 569–576. doi:10.1016/j.rec.2018.05.030. PMID 30104167.
- ↑ Grewal DS, Chamoli SC, Saxena S (April 2014). "Absent pulmonary valve syndrome - Antenatal diagnosis". Med J Armed Forces India. 70 (2): 198–200. doi:10.1016/j.mjafi.2013.07.002. PMC 4017172. PMID 24843213.
- ↑ Volpe P, Paladini D, Marasini M, Buonadonna AL, Russo MG, Caruso G, Marzullo A, Arciprete P, Martinelli P, Gentile M (November 2004). "Characteristics, associations and outcome of absent pulmonary valve syndrome in the fetus". Ultrasound Obstet Gynecol. 24 (6): 623–8. doi:10.1002/uog.1729. PMID 15386602.
- ↑ Nollen GJ, van Schijndel KE, Timmermans J, Groenink M, Barentsz JO, van der Wall EE, Stoker J, Mulder BJ (May 2002). "Pulmonary artery root dilatation in Marfan syndrome: quantitative assessment of an unknown criterion". Heart. 87 (5): 470–1. doi:10.1136/heart.87.5.470. PMC 1767105. PMID 11997425.
- ↑ Eisenberg MJ (January 1993). "Rheumatic heart disease in the developing world: prevalence, prevention, and control". Eur. Heart J. 14 (1): 122–8. doi:10.1093/eurheartj/14.1.122. PMID 8432279.
- ↑ prasad, Arun; Kumar, Sanjeev; Kr Singh, Birendra; Kumari, Neelam (2017). "Mortality Due to Rheumatic Heart Disease in Developing World: A Preventable Problem". Journal of Clinical & Experimental Cardiology. 08 (03). doi:10.4172/2155-9880.1000503. ISSN 2155-9880.
- ↑ Raymond TE, Khabbaza JE, Yadav R, Tonelli AR (December 2014). "Significance of main pulmonary artery dilation on imaging studies". Ann Am Thorac Soc. 11 (10): 1623–32. doi:10.1513/AnnalsATS.201406-253PP. PMC 4298979. PMID 25406836.