Orthostatic hypotension: Difference between revisions
Aditya Ganti (talk | contribs) |
|||
| (115 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
{{SI}} | {{SI}} | ||
{{CMG}}; {{AE}} {{S.G.}}; {{Norina Usman}} | {{CMG}}; {{AE}} {{Mitra}}; {{S.G.}}; {{Norina Usman}} | ||
{{SK}} Postural hypotension; orthostatic intolerance; head rush; dizzy spell | {{SK}} Postural hypotension; orthostatic intolerance; head rush; dizzy spell | ||
==Overview== | ==Overview== | ||
[[Orthostatic hypotension]] or [[postural hypotension]] is defined as a reduction of [[systolic blood pressure]] of at least 20 mm Hg or 10 mm Hg in [[diastolic blood pressure]] within 3 minutes of standing. A similar fall during [[head-up tilt test]] at 60 degrees also defines [[orthostatic hypotension]]. [[Orthostatic hypotension]] may be asymptomatic or may cause symptoms of [[lightheadedness]], [[dizziness]], [[blurred vision]] or [[cognitive impairment]]. It may have acute or chronic causes. Management of [[orthostatic hypotension]] may be challenging, in particular in patients with [[orthostatic hypotension]] and concomitant [[supine]] [[hypertension]]. <ref name="pmid14705758">{{cite journal| author=Bradley JG, Davis KA| title=Orthostatic hypotension. | journal=Am Fam Physician | year= 2003 | volume= 68 | issue= 12 | pages= 2393-8 | pmid=14705758 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14705758 }} </ref><ref name="pmid1592445">{{cite journal| author=Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS| title=Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group. | journal=Hypertension | year= 1992 | volume= 19 | issue= 6 Pt 1 | pages= 508-19 | pmid=1592445 | doi=10.1161/01.hyp.19.6.508 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1592445 }} </ref><ref name="pmid9109468">{{cite journal| author=Ooi WL, Barrett S, Hossain M, Kelley-Gagnon M, Lipsitz LA| title=Patterns of orthostatic blood pressure change and their clinical correlates in a frail, elderly population. | journal=JAMA | year= 1997 | volume= 277 | issue= 16 | pages= 1299-304 | pmid=9109468 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9109468 }} </ref> | |||
==Classification== | |||
[[ | *Based on the underlying [[pathophysiology]] correlated to a postural drop in [[blood pressure]], orthostatic hypotension can be classified into: | ||
'''Initial orthostatic hypotension (iOH)''' | '''Initial orthostatic hypotension (iOH)''' | ||
*It is most common in healthy adolescents | *It is most common in healthy adolescents | ||
*It is demarcated as a brief BP decrease of >40 mmHg systolic or >20 mmHg diastolic with symptomatic [[cerebral hypoperfusion]] within five to fifteen seconds after standing, typically | *It is demarcated as a brief BP decrease of >40 mmHg systolic or >20 mmHg diastolic with symptomatic [[cerebral hypoperfusion]] within five to fifteen seconds after standing, typically resolved by twenty seconds. | ||
'''Neurogenic orthostatic hypotension (nOH)''' | '''Neurogenic orthostatic hypotension (nOH)''' | ||
*In [[Neurogenic orthostatic hypotension]], the [[sympathetic]] [[noradrenergic]] nerves continually fail to facilitate the reflexive cardiovascular responses essential to sustain blood pressure in response to orthostatic stress. | *In [[Neurogenic orthostatic hypotension]], the [[sympathetic]] [[noradrenergic]] nerves continually fail to facilitate the reflexive cardiovascular responses essential to sustain blood pressure in response to orthostatic stress. | ||
*It is described as a constant BP decrease of >20 mmHg systolic or >10 mmHg diastolic, without or with symptoms, within three minutes of head-up tilt or standing. | *It is described as a constant [[BP]] decrease of >20 mmHg systolic or >10 mmHg diastolic, without or with symptoms, within three minutes of head-up tilt or standing. | ||
'''Delayed orthostatic hypotension (dOH)''' | '''Delayed orthostatic hypotension (dOH)''' | ||
[[Delayed orthostatic hypotension]] (dOH) is demarcated as a fall in blood pressure that accomplishes neurogenic orthostatic hypotension criteria but ensues after three minutes. | *[[Delayed orthostatic hypotension]] (dOH) is demarcated as a fall in blood pressure that accomplishes neurogenic orthostatic hypotension criteria but ensues after three minutes. | ||
'''Neurally mediated syncope (vOH)''' | '''Neurally mediated syncope (vOH)''' | ||
It is also recognized as vasodepressor or [[vasovagal syncope]], | *It is also recognized as vasodepressor or [[vasovagal syncope]], it involves a [[paroxysmal]] extraction of [[sympathetic]] [[vasopressor]] tone, frequently during prolonged standing, in patients with an effective [[autonomic nervous system]]. | ||
'''Cardiovascular orthostatic hypotension (cOH)''' | '''Cardiovascular orthostatic hypotension (cOH)''' | ||
[[Cardiovascular orthostatic hypotension]] occurs from intravascular [[hypovolemia]] or reduced cardiac output along with compensatory [[tachycardia]]. | *[[Cardiovascular orthostatic hypotension]] occurs from intravascular [[hypovolemia]] or reduced [[cardiac output]] along with compensatory [[tachycardia]]. | ||
'''Orthostatic pseudohypotension (pOH)''' | '''Orthostatic pseudohypotension (pOH)''' | ||
It is stated as apparent orthostatic hypotension when baseline supine blood pressure is raised, which may be due to a short time at rest to create a valid baseline, related recumbent [[hypertension]], or fluctuation of baseline blood pressure with labile [[hypertension]]<ref name="pmidhttps://doi.org/10.1007/s10286-016-0382-6">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=https://doi.org/10.1007/s10286-016-0382-6 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref name="pmid17199559">{{cite journal| author=Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME| title=Initial orthostatic hypotension: review of a forgotten condition. | journal=Clin Sci (Lond) | year= 2007 | volume= 112 | issue= 3 | pages= 157-65 | pmid=17199559 | doi=10.1042/CS20060091 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17199559 }} </ref><ref name="pmid21431947">{{cite journal| author=Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I | display-authors=etal| title=Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. | journal=Clin Auton Res | year= 2011 | volume= 21 | issue= 2 | pages= 69-72 | pmid=21431947 | doi=10.1007/s10286-011-0119-5 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21431947 }} </ref><ref name="pmid19390349">{{cite journal| author=Wieling W, Schatz IJ| title=The consensus statement on the definition of orthostatic hypotension: a revisit after 13 years. | journal=J Hypertens | year= 2009 | volume= 27 | issue= 5 | pages= 935-8 | pmid=19390349 | doi=10.1097/HJH.0b013e32832b1145 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19390349 }} </ref> | *It is stated as apparent [[orthostatic hypotension]] when baseline supine [[blood pressure]] is raised, which may be due to a short time at rest to create a valid baseline, related recumbent [[hypertension]], or fluctuation of baseline blood pressure with labile [[hypertension]] <ref name="pmidhttps://doi.org/10.1007/s10286-016-0382-6">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=https://doi.org/10.1007/s10286-016-0382-6 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref name="pmid17199559">{{cite journal| author=Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME| title=Initial orthostatic hypotension: review of a forgotten condition. | journal=Clin Sci (Lond) | year= 2007 | volume= 112 | issue= 3 | pages= 157-65 | pmid=17199559 | doi=10.1042/CS20060091 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17199559 }} </ref><ref name="pmid21431947">{{cite journal| author=Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I | display-authors=etal| title=Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. | journal=Clin Auton Res | year= 2011 | volume= 21 | issue= 2 | pages= 69-72 | pmid=21431947 | doi=10.1007/s10286-011-0119-5 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21431947 }} </ref><ref name="pmid19390349">{{cite journal| author=Wieling W, Schatz IJ| title=The consensus statement on the definition of orthostatic hypotension: a revisit after 13 years. | journal=J Hypertens | year= 2009 | volume= 27 | issue= 5 | pages= 935-8 | pmid=19390349 | doi=10.1097/HJH.0b013e32832b1145 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19390349 }} </ref> | ||
==Pathophysiology== | ==Pathophysiology== | ||
*In standing position, | *In the standing position, 500 to 1000 mL of [[blood]] pools in the [[lower extremities]] and [[splanchnic circulation]], causing a rapid decline in [[venous return]] to the heart. | ||
*Decreased [[ventricular filling pressures]] lower [[cardiac output]] and systemic [[blood pressure]]. <ref name="pmid2674714">{{cite journal| author=Lipsitz LA| title=Orthostatic hypotension in the elderly. | journal=N Engl J Med | year= 1989 | volume= 321 | issue= 14 | pages= 952-7 | pmid=2674714 | doi=10.1056/NEJM198910053211407 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=2674714 }} </ref><ref name="pmid7791382">{{cite journal| author=Low PA, Opfer-Gehrking TL, McPhee BR, Fealey RD, Benarroch EE, Willner CL | display-authors=etal| title=Prospective evaluation of clinical characteristics of orthostatic hypotension. | journal=Mayo Clin Proc | year= 1995 | volume= 70 | issue= 7 | pages= 617-22 | pmid=7791382 | doi=10.4065/70.7.617 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7791382 }} </ref><ref name="pmid11093411">{{cite journal| author=Zaqqa M, Massumi A| title=Neurally mediated syncope. | journal=Tex Heart Inst J | year= 2000 | volume= 27 | issue= 3 | pages= 268-72 | pmid=11093411 | doi= | pmc=101078 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11093411 }} </ref><ref name="pmid7746371">{{cite journal| author=Mathias CJ| title=Orthostatic hypotension: causes, mechanisms, and influencing factors. | journal=Neurology | year= 1995 | volume= 45 | issue= 4 Suppl 5 | pages= S6-11 | pmid=7746371 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7746371 }} </ref><ref name="pmid1475949">{{cite journal| author=Hollister AS| title=Orthostatic hypotension. Causes, evaluation, and management. | journal=West J Med | year= 1992 | volume= 157 | issue= 6 | pages= 652-7 | pmid=1475949 | doi= | pmc=1022100 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=1475949 }} </ref> | |||
*[[Baroreceptors]] located mainly in the [[aorta]] and [[carotid arteries]] are very sensitive to fluctuations in blood pressure. A fall in [[blood pressure]] decreases the stretching of [[baroreceptors]], thus decreasing their firing. The decreased firing of [[baroreceptors]] increases [[sympathetic]] and decreases [[parasympathetic]] outflow. | |||
* | *This compensatory reflex increases [[heart rate]], [[contractility]] and [[peripheral vascular resistance]] (i.e., both arteriolar and venous [[vasoconstriction]]). These changes result in increased [[venous return]] and increased [[cardiac output]], and limit the decline in [[blood pressure]]. This compensatory reflex is known as [[baroreflex]]. | ||
*Any disruption in this pathway can cause a significant decline in [[blood pressure]] upon standing (i.e., [[orthostatic hypotension]]), causing symptoms of cerebral hypoperfusion including [[nausea]], [[dizziness]], [[headache]], [[lightheadedness]], [[blurred vision]], and impaired [[cognition]]. | |||
*Although many pathologic causes may alter this normal physiologic response to standing, the most common pathophysiologic mechanisms include: | |||
**[[Autonomic dysfunction]] affecting the [[baroreflex]] (i.e. baroreflex dysfunction) | |||
**[[Volume depletion]] | |||
**Adverse effects of certain [[medications]] | |||
[[Image:barereflex.jpg|center|1000px|]] | |||
==Causes== | ==Causes== | ||
==== | Common causes of [[orthostsic hypotension]] include: <ref name="Jiang-2005">{{cite journal | author=Jiang W, Davidson JR. | title=Antidepressant therapy in patients with ischemic heart disease. | journal=Am Heart J | year=2005 | volume=150 | issue=5 | pages=871-81 | id=PMID 16290952}}</ref><ref name="Delini-Stula-1999">{{cite journal | author=Delini-Stula A, Baier D, Kohnen R, Laux G, Philipp M, Scholz HJ. | title=Undesirable blood pressure changes under naturalistic treatment with moclobemide, a reversible MAO-A inhibitor--results of the drug utilization observation studies. | journal=Pharmacopsychiatry | year=1999 | volume=32 | issue=2 | pages=61-7 | id=PMID 10333164}}</ref><ref name="Jones-2002">{{cite journal | author=Jones RT. | title=Cardiovascular system effcts of marijuana. | journal=J Clin Pharmacol | year=2002 | volume=42 | issue=11 Suppl | pages=58S-63S | id=PMID 12412837}}</ref><ref name="pmid1898124">{{cite journal |vauthors=Hohmann M, Künzel W |title=Orthostatic hypotension and birthweight |journal=Arch. Gynecol. Obstet. |volume=248 |issue=4 |pages=181–9 |date=1991 |pmid=1898124 |doi=10.1007/bf02390357 |url=}}</ref> | ||
{| class="wikitable" | |||
**[[ | |+ | ||
**[[ | |- | ||
| align="center" style="background: #4479BA; color: #FFFFFF " |'''Causes of [[orthostatic hypotension]]''' | |||
* | |- | ||
**[[ | |'''[[Cardiac diseases]]''' | ||
**[[ | |- | ||
** | | | ||
**[[ | *[[Myocardial ischemia]]/[[Myocardial infarction]] | ||
*[[ | |- | ||
**[[ | | | ||
**[[ | *[[Cardiac arrhythmias]] | ||
* | |- | ||
| | |||
*[[Congestive heart failure]] | |||
|- | |||
| | |||
**[[ | *[[Myocarditis]]/[[pericarditis]] | ||
**[[ | |- | ||
**[[ | | | ||
*[[Valvular heart diseases]] | |||
|- | |||
|'''[[Intravascular volume depletion]]''' | |||
|- | |||
| | |||
*[[Anemia]] | |||
|- | |||
| | |||
*[[Blood loss]] | |||
|- | |||
| | |||
*[[Dehydration]] | |||
|- | |||
| | |||
*[[Diuretics]] | |||
|- | |||
|'''[[Venous pooling]]/[[venous vasodilation]]''' | |||
|- | |||
| | |||
*[[Prolonged bed rest]] | |||
|- | |||
| | |||
*[[Pregnancy]] | |||
|- | |||
| | |||
*[[Venous insufficiency]]/[[Varicosities]] | |||
|- | |||
|'''[[Autonomic nervous system disorders]]''' | |||
|- | |||
| | |||
*Primary: | |||
**Pure autonomic failure | |||
**[[Multiple system atrophy]] | |||
|- | |||
| | |||
*Secondary: | |||
**[[Diabetes]] | |||
**[[Amyloidosis]] | |||
**[[Sarcoidosis]] | |||
**[[Renal failure]] | |||
|- | |||
|'''Endocrine''' | |||
|- | |||
| | |||
*[[Adrenal insufficiency]] | |||
|- | |||
| | |||
*[[Diabetes insipidus]] | |||
|- | |||
| | |||
*[[Hyperglycemia]] (acute) | |||
|- | |||
| | |||
*[[Hypoaldosteronism]] | |||
|- | |||
| | |||
*[[Hypokalemia]] | |||
|- | |||
| | |||
*[[Hypothyroidism]] | |||
|- | |||
| | |||
*[[Pheochromocytoma]] | |||
|- | |||
|'''[[Medications]]''' | |||
|- | |||
|'''Miscellaneous''' | |||
|- | |||
| | |||
*[[AIDS]] | |||
|- | |||
| | |||
*[[Anxiety]] or [[panic disorder]] | |||
|- | |||
| | |||
*[[Eating disorders]] | |||
|- | |||
| | |||
*[[Postprandial hypotension]] | |||
|- | |||
|} | |||
{| | |||
|- | |||
|} | |||
{| class="wikitable" | |||
|+ | |||
| colspan="2" rowspan="2" align="center" style="background: #4479BA; color: #FFFFFF " |'''Medication-induced [[Orthostatic Hypotension]]''' | |||
|+ | |||
|+ | |||
| colspan="1" rowspan="1" |'''[[Vasodilation]] through [[Alpha-1]] blockade''' | |||
| colspan="1" rowspan="1" | | |||
*[[Alpha-1 blockers]]: | |||
**[[Terazosin]] | |||
**[[Prazosin]] | |||
**[[Doxazosin]] | |||
*[[Antipsychotics]]: | |||
**[[Perphenazine oral|Perphenazine]] | **[[Perphenazine oral|Perphenazine]] | ||
**[[Risperidone]] | **[[Risperidone]] | ||
**[[Thioridazine hydrochloride]] | **[[Thioridazine hydrochloride]] | ||
**[[ | **[[Clozapine]] | ||
**[[ | **[[zotepine]] | ||
**[[ | **[[Olanzapine]] | ||
**[[ | **[[Fluphenazine (patient information)|Fluphenazine]] | ||
**[[ | *[[Antihistamines]] | ||
**[[ | *[[Antidepressants]]: | ||
**[[ | **[[Trazodone]] | ||
**[[ | **[[Tricyclic antidepressants]] ([[TCA]]s) | ||
**[[ | **[[Serotonin norepinephrine reuptake inhibitors]] ([[SNRI]]s): | ||
**[[Nitrates]] | ***[[Venlafaxine]] | ||
**[[ | ***[[Duloxetine]] | ||
**[[ | **[[Monoamine oxidase inhibitors]] | ||
**[[ | |- | ||
| colspan="1" rowspan="1" |'''[[Vasodilation]] (Others)''' | |||
**[[ | | colspan="1" rowspan="1" | | ||
*[[ACE Inhibitor]]s | |||
*[[ARBs]] | |||
*[[Dihydropyridine]] [[calcium channel blockers]] | |||
*[[Hydralazine]] | |||
*[[Nitrates]] | |||
*[[Phosphodiesterase inhibitors]]: | |||
**[[Sildenafil]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Volume depletion''' | |||
| colspan="1" rowspan="1" | | |||
*[[Diuretics]]: | |||
**[[Ethacrynic acid (patient information)|Ethacrynic Acid]] | |||
**[[Hydrochlorothiazide (patient information)|Hydrochlorothiazide]] | |||
**[[Furosemide]] | |||
*[[SGLT-2 inhibitors]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Sympathetic blockade''' | |||
| colspan="1" rowspan="1" | | |||
*[[Ganglionic blocking agents]] | |||
*[[Beta Blockers]]: | |||
**[[Propranolol]] | |||
*[[Clonidine]] | |||
|- | |||
| colspan="1" rowspan="1" |'''[[Dopamin agonists]] and other anti-Parkinsonian medications''' | |||
| colspan="1" rowspan="1" | | |||
*[[Dopamine agonists]] | |||
**[[Bromocriptine]] | |||
**[[Pramipexole]] | **[[Pramipexole]] | ||
**[[Ropinirole]] | **[[Ropinirole]] | ||
*[[Levodopa]] | |||
*[[Monoamine oxidase inhibitor]]s: | |||
**[[Selegiline]] | |||
**[[Rasagiline]] | |||
*[[COMT inhibitors]]: | |||
**[[Entacapone (patient information)|Entacapone]] | |||
|- | |||
| colspan="1" rowspan="1" |'''Others''' | |||
| colspan="1" rowspan="1" | | |||
*[[Alcohol]] | |||
*[[Apomorphine hydrochloride]] | |||
*[[Cidofovir]] | |||
*[[Iloperidone]] | |||
*[[Loxapine]] | |||
*[[Niacin]] | |||
*[[Pergolide]] | |||
*[[Ritonavir]] | |||
*[[Rotigotine]] | |||
*[[Narcotics]]: | |||
**[[Opiates]]: [[Morhine]] | |||
*[[Sedative-hypnotics]]: | |||
**[[Tempazepam]] | |||
*[[Muscle relaxants]]: | |||
**[[Tizanidine]] | |||
*[[Thiothixene]] | |||
*[[Tiagabine]] | |||
*Chemotherapeutic agents: | |||
*[[Vincristine]] | |||
*[[Vinblastine]] | |||
|- | |||
|} | |||
==Differentiating Orthostatic Hypotension from Other Diseases== | ==Differentiating Orthostatic Hypotension from Other Diseases== | ||
Orthostatic hypotension must be differentiated from [[neurogenic syncope]], [[cardiogenic syncope]], [[situational syncope]], [[multiple system atrophy]] with orthostatic hypotension, [[neurally mediated hypotension]], [[postural orthostatic tachycardia syndrome]] (POTS) and [[vasovagal syncope]]<ref name="pmid25498732">{{cite journal| author=Poewe W, Seppi K, Fitzer-Attas CJ, Wenning GK, Gilman S, Low PA | display-authors=etal| title=Efficacy of rasagiline in patients with the parkinsonian variant of multiple system atrophy: a randomised, placebo-controlled trial. | journal=Lancet Neurol | year= 2015 | volume= 14 | issue= 2 | pages= 145-52 | pmid=25498732 | doi=10.1016/S1474-4422(14)70288-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25498732 }} </ref><ref name="pmid15875516">{{cite journal| author=Brignole M| title=Neurally-mediated syncope. | journal=Ital Heart J | year= 2005 | volume= 6 | issue= 3 | pages= 249-55 | pmid=15875516 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15875516 }} </ref><ref name="pmid24630686">{{cite journal| author=Trahair LG, Horowitz M, Jones KL| title=Postprandial hypotension: a systematic review. | journal=J Am Med Dir Assoc | year= 2014 | volume= 15 | issue= 6 | pages= 394-409 | pmid=24630686 | doi=10.1016/j.jamda.2014.01.011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24630686 }} </ref><ref name="pmid26198889">{{cite journal| author=Garland EM, Celedonio JE, Raj SR| title=Postural Tachycardia Syndrome: Beyond Orthostatic Intolerance. | journal=Curr Neurol Neurosci Rep | year= 2015 | volume= 15 | issue= 9 | pages= 60 | pmid=26198889 | doi=10.1007/s11910-015-0583-8 | pmc=4664448 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26198889 }} </ref><ref name="pmid28375909">{{cite journal| author=Cheshire WP| title=Syncope. | journal=Continuum (Minneap Minn) | year= 2017 | volume= 23 | issue= 2, Selected Topics in Outpatient Neurology | pages= 335-358 | pmid=28375909 | doi=10.1212/CON.0000000000000444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28375909 }} </ref><ref name="pmid3528810">{{cite journal| author=Dohrmann ML, Cheitlin MD| title=Cardiogenic syncope. Seizure versus syncope. | journal=Neurol Clin | year= 1986 | volume= 4 | issue= 3 | pages= 549-62 | pmid=3528810 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3528810 }} </ref><ref name="pmid21160608">{{cite journal| author=Aydin MA, Salukhe TV, Wilke I, Willems S| title=Management and therapy of vasovagal syncope: A review. | journal=World J Cardiol | year= 2010 | volume= 2 | issue= 10 | pages= 308-15 | pmid=21160608 | doi=10.4330/wjc.v2.i10.308 | pmc=2998831 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21160608 }} </ref> | Orthostatic hypotension must be differentiated from [[neurogenic syncope]], [[cardiogenic syncope]], [[situational syncope]], [[multiple system atrophy]] with orthostatic hypotension, [[neurally mediated hypotension]], [[postural orthostatic tachycardia syndrome]] (POTS) and [[vasovagal syncope]] <ref name="pmid25498732">{{cite journal| author=Poewe W, Seppi K, Fitzer-Attas CJ, Wenning GK, Gilman S, Low PA | display-authors=etal| title=Efficacy of rasagiline in patients with the parkinsonian variant of multiple system atrophy: a randomised, placebo-controlled trial. | journal=Lancet Neurol | year= 2015 | volume= 14 | issue= 2 | pages= 145-52 | pmid=25498732 | doi=10.1016/S1474-4422(14)70288-1 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=25498732 }} </ref><ref name="pmid15875516">{{cite journal| author=Brignole M| title=Neurally-mediated syncope. | journal=Ital Heart J | year= 2005 | volume= 6 | issue= 3 | pages= 249-55 | pmid=15875516 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=15875516 }} </ref><ref name="pmid24630686">{{cite journal| author=Trahair LG, Horowitz M, Jones KL| title=Postprandial hypotension: a systematic review. | journal=J Am Med Dir Assoc | year= 2014 | volume= 15 | issue= 6 | pages= 394-409 | pmid=24630686 | doi=10.1016/j.jamda.2014.01.011 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24630686 }} </ref><ref name="pmid26198889">{{cite journal| author=Garland EM, Celedonio JE, Raj SR| title=Postural Tachycardia Syndrome: Beyond Orthostatic Intolerance. | journal=Curr Neurol Neurosci Rep | year= 2015 | volume= 15 | issue= 9 | pages= 60 | pmid=26198889 | doi=10.1007/s11910-015-0583-8 | pmc=4664448 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26198889 }} </ref><ref name="pmid28375909">{{cite journal| author=Cheshire WP| title=Syncope. | journal=Continuum (Minneap Minn) | year= 2017 | volume= 23 | issue= 2, Selected Topics in Outpatient Neurology | pages= 335-358 | pmid=28375909 | doi=10.1212/CON.0000000000000444 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28375909 }} </ref><ref name="pmid3528810">{{cite journal| author=Dohrmann ML, Cheitlin MD| title=Cardiogenic syncope. Seizure versus syncope. | journal=Neurol Clin | year= 1986 | volume= 4 | issue= 3 | pages= 549-62 | pmid=3528810 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=3528810 }} </ref><ref name="pmid21160608">{{cite journal| author=Aydin MA, Salukhe TV, Wilke I, Willems S| title=Management and therapy of vasovagal syncope: A review. | journal=World J Cardiol | year= 2010 | volume= 2 | issue= 10 | pages= 308-15 | pmid=21160608 | doi=10.4330/wjc.v2.i10.308 | pmc=2998831 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21160608 }} </ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
! rowspan="2" |Disease | ! rowspan="2" align="center" style="background: #4479BA; color: #FFFFFF " |Disease | ||
! colspan="12" |History and Physical Examination | ! colspan="12" align="center" style="background: #4479BA; color: #FFFFFF " |History and Physical Examination | ||
! | ! align="center" style="background: #4479BA; color: #FFFFFF " | | ||
! colspan="4" |Diagnostic approach | ! colspan="4" align="center" style="background: #4479BA; color: #FFFFFF " |Diagnostic approach | ||
|- | |- | ||
!Lightheadedness | ! align="center" style="background: #4479BA; color: #FFFFFF " |Lightheadedness | ||
!Fatigue | ! align="center" style="background: #4479BA; color: #FFFFFF " |Fatigue | ||
!Autonomic symptoms | ! align="center" style="background: #4479BA; color: #FFFFFF " |Autonomic symptoms | ||
!Fever | ! align="center" style="background: #4479BA; color: #FFFFFF " |Fever | ||
!Nausea/vomiting | ! align="center" style="background: #4479BA; color: #FFFFFF " |Nausea/vomiting | ||
!Diminished Vision | ! align="center" style="background: #4479BA; color: #FFFFFF " |Diminished Vision | ||
!Dizziness | ! align="center" style="background: #4479BA; color: #FFFFFF " |Dizziness | ||
!Slurred Speech | ! align="center" style="background: #4479BA; color: #FFFFFF " |Slurred Speech | ||
!Tachycardia | ! align="center" style="background: #4479BA; color: #FFFFFF " |Tachycardia | ||
!Altered mentation | ! align="center" style="background: #4479BA; color: #FFFFFF " |Altered mentation | ||
!Loss of Consciousness | ! align="center" style="background: #4479BA; color: #FFFFFF " |Loss of Consciousness | ||
!Weakness | ! align="center" style="background: #4479BA; color: #FFFFFF " |Weakness | ||
!Neurological Deficit | ! align="center" style="background: #4479BA; color: #FFFFFF " |Neurological Deficit | ||
!Labs and CSF findings | ! align="center" style="background: #4479BA; color: #FFFFFF " |Labs and CSF findings | ||
!ECG | ! align="center" style="background: #4479BA; color: #FFFFFF " |ECG | ||
!CT/MRI | ! align="center" style="background: #4479BA; color: #FFFFFF " |CT/MRI | ||
!Gold standard test | ! align="center" style="background: #4479BA; color: #FFFFFF " |Gold standard test | ||
|- | |- | ||
|'''Multiple system atrophy with orthostatic hypotension''' | |'''Multiple system atrophy with orthostatic hypotension''' | ||
| Line 141: | Line 302: | ||
| - | | - | ||
|Atrophy of brain stem and cerebellum | |Atrophy of brain stem and cerebellum | ||
|Clinical | | | ||
*Clinical assessment | |||
|- | |- | ||
|'''Neurally mediated hypotension''' | |'''Neurally mediated hypotension''' | ||
| Line 160: | Line 322: | ||
| - | | - | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|Clinical | | | ||
*Clinical assessment | |||
|- | |- | ||
| | |''''Postural Orthostatic Tachycardia Syndrome (POTS)''' | ||
| + | | + | ||
| + | | + | ||
| Line 179: | Line 342: | ||
| + | | + | ||
|<nowiki>-</nowiki> | |<nowiki>-</nowiki> | ||
|Clinical | | | ||
*Clinical assessment | |||
|- | |- | ||
|'''Neurologic syncope''' | |'''Neurologic syncope''' | ||
| Line 198: | Line 362: | ||
| - | | - | ||
| - | | - | ||
|Clinical assessment | | | ||
*Clinical assessment | |||
|- | |- | ||
|'''Cardiac syncope''' | |'''Cardiac syncope''' | ||
| Line 217: | Line 382: | ||
| + | | + | ||
| - | | - | ||
|ECG | | | ||
*[[ECG]] | |||
*[[Holter monitor]] | |||
*[[Echocardiography]] | |||
|- | |- | ||
|'''Situational syncope''' | |'''Situational syncope''' | ||
| Line 236: | Line 404: | ||
| - | | - | ||
| - | | - | ||
|Clinical assessment syncope occurs during defecation, micturition or coughing | | | ||
*Clinical assessment syncope occurs during defecation, micturition, or coughing | |||
|- | |- | ||
|'''Vasovagal syncope (also known as cardio-neurogenic syncope)''' | |'''Vasovagal syncope (also known as cardio-neurogenic syncope)''' | ||
| Line 255: | Line 424: | ||
| + | | + | ||
| - | | - | ||
|ECG | | | ||
*[[ECG]] | |||
*[[Echocardiogram]] | |||
*[[Exercise stress testing|Exercise stress test]] | |||
|} | |} | ||
==Epidemiology and Demographics== | ==Epidemiology and Demographics== | ||
| Line 324: | Line 434: | ||
'''Incidence''' | '''Incidence''' | ||
*The approximation of orthostatic hypotension‐associated hospitalization is 36 per 100,000 adults, and the rate can be as high as 233 per 100,000 patients >75 years of age<ref name="pmid28713844">{{cite journal| author=Palma JA, Kaufmann H| title=Epidemiology, Diagnosis, and Management of [[Neurogenic Orthostatic Hypotension]]. | journal=Mov Disord Clin Pract | year= 2017 | volume= 4 | issue= 3 | pages= 298-308 | pmid=28713844 | doi=10.1002/mdc3.12478 | pmc=5506688 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28713844 }} </ref> | *The approximation of orthostatic hypotension‐associated hospitalization is 36 per 100,000 adults, and the rate can be as high as 233 per 100,000 patients >75 years of age. <ref name="pmid28713844">{{cite journal| author=Palma JA, Kaufmann H| title=Epidemiology, Diagnosis, and Management of [[Neurogenic Orthostatic Hypotension]]. | journal=Mov Disord Clin Pract | year= 2017 | volume= 4 | issue= 3 | pages= 298-308 | pmid=28713844 | doi=10.1002/mdc3.12478 | pmc=5506688 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=28713844 }} </ref> | ||
'''Prevalence''' | '''Prevalence''' | ||
| Line 330: | Line 440: | ||
*The overall prevalence of [[orthostatic hypotension]] depends on age as it increases with age in the general population. | *The overall prevalence of [[orthostatic hypotension]] depends on age as it increases with age in the general population. | ||
*The [[prevalence]] ranges from 5% in patients <50 years of age to 30% in those >70 years of age. | *The [[prevalence]] ranges from 5% in patients <50 years of age to 30% in those >70 years of age. | ||
*It is ~20% in > 65-year-old patients<ref name="pmid26271068">{{cite journal| author=Ricci F, De Caterina R, Fedorowski A| title=Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment. | journal=J Am Coll Cardiol | year= 2015 | volume= 66 | issue= 7 | pages= 848-860 | pmid=26271068 | doi=10.1016/j.jacc.2015.06.1084 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26271068 }} </ref><ref name="pmid18368301">{{cite journal| author=Low PA| title=Prevalence of orthostatic hypotension. | journal=Clin Auton Res | year= 2008 | volume= 18 Suppl 1 | issue= | pages= 8-13 | pmid=18368301 | doi=10.1007/s10286-007-1001-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18368301 }} </ref> | *It is ~20% in >65-year-old patients. <ref name="pmid26271068">{{cite journal| author=Ricci F, De Caterina R, Fedorowski A| title=Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment. | journal=J Am Coll Cardiol | year= 2015 | volume= 66 | issue= 7 | pages= 848-860 | pmid=26271068 | doi=10.1016/j.jacc.2015.06.1084 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26271068 }} </ref><ref name="pmid18368301">{{cite journal| author=Low PA| title=Prevalence of orthostatic hypotension. | journal=Clin Auton Res | year= 2008 | volume= 18 Suppl 1 | issue= | pages= 8-13 | pmid=18368301 | doi=10.1007/s10286-007-1001-3 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18368301 }} </ref> | ||
'''Age''' | '''Age''' | ||
*Orthostatic Hypotension is commonly seen in individuals older than 50 years of age. | *[[Orthostatic Hypotension]] is commonly seen in individuals older than 50 years of age. | ||
'''Gender''' | '''Gender''' | ||
*Orthostatic hypotension affects men and women equally. | *[[Orthostatic hypotension]] affects men and women equally. | ||
==Risk Factors== | ==Risk Factors== | ||
Common [[Risk factor|risk factors]] in the development of orthostatic hypotension include:<ref name="ArnoldShibao2013">{{cite journal|last1=Arnold|first1=Amy C.|last2=Shibao|first2=Cyndya|title=Current Concepts in Orthostatic Hypotension Management|journal=Current Hypertension Reports|volume=15|issue=4|year=2013|pages=304–312|issn=1522-6417|doi=10.1007/s11906-013-0362-3}}</ref><ref name="CanobbioWarnes2017">{{cite journal|last1=Canobbio|first1=Mary M.|last2=Warnes|first2=Carole A.|last3=Aboulhosn|first3=Jamil|last4=Connolly|first4=Heidi M.|last5=Khanna|first5=Amber|last6=Koos|first6=Brian J.|last7=Mital|first7=Seema|last8=Rose|first8=Carl|last9=Silversides|first9=Candice|last10=Stout|first10=Karen|title=Management of Pregnancy in Patients With Complex Congenital Heart Disease: A Scientific Statement for Healthcare Professionals From the American Heart Association|journal=Circulation|volume=135|issue=8|year=2017|issn=0009-7322|doi=10.1161/CIR.0000000000000458}}</ref> | Common [[Risk factor|risk factors]] in the development of orthostatic hypotension include: <ref name="ArnoldShibao2013">{{cite journal|last1=Arnold|first1=Amy C.|last2=Shibao|first2=Cyndya|title=Current Concepts in Orthostatic Hypotension Management|journal=Current Hypertension Reports|volume=15|issue=4|year=2013|pages=304–312|issn=1522-6417|doi=10.1007/s11906-013-0362-3}}</ref><ref name="CanobbioWarnes2017">{{cite journal|last1=Canobbio|first1=Mary M.|last2=Warnes|first2=Carole A.|last3=Aboulhosn|first3=Jamil|last4=Connolly|first4=Heidi M.|last5=Khanna|first5=Amber|last6=Koos|first6=Brian J.|last7=Mital|first7=Seema|last8=Rose|first8=Carl|last9=Silversides|first9=Candice|last10=Stout|first10=Karen|title=Management of Pregnancy in Patients With Complex Congenital Heart Disease: A Scientific Statement for Healthcare Professionals From the American Heart Association|journal=Circulation|volume=135|issue=8|year=2017|issn=0009-7322|doi=10.1161/CIR.0000000000000458}}</ref> | ||
*[[Age]] (>65) | *[[Age]] (>65) | ||
*[[Medication|Medications]] | *[[Medication|Medications]] | ||
*[[ | *[[Autonomic neuropathies]], such as[[Parkinson's Disease|Parkinson's disease]], [[diabetes]] | ||
*[[Volume depletion]] | |||
*[[Postpartum period]] | *[[Postpartum period]] | ||
*[[Prolong bedrest]]. | *[[Prolong bedrest]]. | ||
| Line 352: | Line 463: | ||
==Screening== | ==Screening== | ||
*Orthostatic hypotension | *Orthostatic hypotension screening consists of [[blood pressure]] measurements in [[supine]] (or sitting) and [[standing position]] during clinical consultations. <ref name="pmid30418320">{{cite journal| author=Cremer A, Rousseau AL, Boulestreau R, Kuntz S, Tzourio C, Gosse P| title=Screening for orthostatic hypotension using home blood pressure measurements. | journal=J Hypertens | year= 2019 | volume= 37 | issue= 5 | pages= 923-927 | pmid=30418320 | doi=10.1097/HJH.0000000000001986 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=30418320 }} </ref> | ||
==Natural History, Complications, and Prognosis== | ==Natural History, Complications, and Prognosis== | ||
====Natural History==== | ====Natural History==== | ||
*The symptoms of orthostatic hypotension mainly develop in the elderly, and start with generalized symptoms of [[dizziness]], [[lightheadedness]], or [[syncope]] and less frequently with [[headache]], [[leg buckling]], or [[chest pain]]<ref name="pmid28846238">{{cite journal| author=| title=StatPearls | journal= | year= 2020 | volume= | issue= | pages= | pmid=28846238 | doi= | pmc= | url= }} </ref><ref name="pmid14705758">{{cite journal| author=Bradley JG, Davis KA| title=Orthostatic hypotension. | journal=Am Fam Physician | year= 2003 | volume= 68 | issue= 12 | pages= 2393-8 | pmid=14705758 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14705758 }} </ref> | *The symptoms of orthostatic hypotension mainly develop in the elderly, and start with generalized symptoms of [[dizziness]], [[lightheadedness]], or [[syncope]] and less frequently with [[headache]], [[leg buckling]], or [[chest pain]] <ref name="pmid28846238">{{cite journal| author=| title=StatPearls | journal= | year= 2020 | volume= | issue= | pages= | pmid=28846238 | doi= | pmc= | url= }} </ref><ref name="pmid14705758">{{cite journal| author=Bradley JG, Davis KA| title=Orthostatic hypotension. | journal=Am Fam Physician | year= 2003 | volume= 68 | issue= 12 | pages= 2393-8 | pmid=14705758 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14705758 }} </ref> | ||
====Complications==== | ====Complications==== | ||
Common [[Complication (medicine)|complications]] of orthostatic hypotension include:<ref name="pmid21438868">{{cite journal |vauthors=Romero-Ortuno R, Cogan L, Foran T, Kenny RA, Fan CW |title=Continuous noninvasive orthostatic blood pressure measurements and their relationship with orthostatic intolerance, falls, and frailty in older people |journal=J Am Geriatr Soc |volume=59 |issue=4 |pages=655–65 |date=April 2011 |pmid=21438868 |doi=10.1111/j.1532-5415.2011.03352.x |url=}}</ref><ref name="RicciFedorowski2015">{{cite journal|last1=Ricci|first1=Fabrizio|last2=Fedorowski|first2=Artur|last3=Radico|first3=Francesco|last4=Romanello|first4=Mattia|last5=Tatasciore|first5=Alfonso|last6=Di Nicola|first6=Marta|last7=Zimarino|first7=Marco|last8=De Caterina|first8=Raffaele|title=Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies|journal=European Heart Journal|volume=36|issue=25|year=2015|pages=1609–1617|issn=0195-668X|doi=10.1093/eurheartj/ehv093}}</ref> | Common [[Complication (medicine)|complications]] of orthostatic hypotension include: <ref name="pmid21438868">{{cite journal |vauthors=Romero-Ortuno R, Cogan L, Foran T, Kenny RA, Fan CW |title=Continuous noninvasive orthostatic blood pressure measurements and their relationship with orthostatic intolerance, falls, and frailty in older people |journal=J Am Geriatr Soc |volume=59 |issue=4 |pages=655–65 |date=April 2011 |pmid=21438868 |doi=10.1111/j.1532-5415.2011.03352.x |url=}}</ref><ref name="RicciFedorowski2015">{{cite journal|last1=Ricci|first1=Fabrizio|last2=Fedorowski|first2=Artur|last3=Radico|first3=Francesco|last4=Romanello|first4=Mattia|last5=Tatasciore|first5=Alfonso|last6=Di Nicola|first6=Marta|last7=Zimarino|first7=Marco|last8=De Caterina|first8=Raffaele|title=Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies|journal=European Heart Journal|volume=36|issue=25|year=2015|pages=1609–1617|issn=0195-668X|doi=10.1093/eurheartj/ehv093}}</ref> | ||
* | *Symptomatic orthostatic hypotension may cause falling. <ref name="pmid23265229">{{cite journal| author=van Hateren KJ, Kleefstra N, Blanker MH, Ubink-Veltmaat LJ, Groenier KH, Houweling ST | display-authors=etal| title=Orthostatic hypotension, diabetes, and falling in older patients: a cross-sectional study. | journal=Br J Gen Pract | year= 2012 | volume= 62 | issue= 603 | pages= e696-702 | pmid=23265229 | doi=10.3399/bjgp12X656838 | pmc=3459777 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23265229 }} </ref> <ref name="pmid21391928">{{cite journal| author=Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P | display-authors=etal| title=Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. | journal=J Am Geriatr Soc | year= 2011 | volume= 59 | issue= 3 | pages= 383-9 | pmid=21391928 | doi=10.1111/j.1532-5415.2011.03317.x | pmc=3306056 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21391928 }} </ref> | ||
** | **The risk of recurrent falls is particularly higher in frail, older adults. | ||
* | *According to various studies, [[orthostatic hypotension]] may be a [[risk factor]] for: <ref name="pmid20698925">{{cite journal| author=Fedorowski A, Hedblad B, Engström G, Gustav Smith J, Melander O| title=Orthostatic hypotension and long-term incidence of atrial fibrillation: the Malmö Preventive Project. | journal=J Intern Med | year= 2010 | volume= 268 | issue= 4 | pages= 383-9 | pmid=20698925 | doi=10.1111/j.1365-2796.2010.02261.x | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20698925 }} </ref> <ref name="pmid23675460">{{cite journal| author=Xin W, Lin Z, Li X| title=Orthostatic hypotension and the risk of congestive heart failure: a meta-analysis of prospective cohort studies. | journal=PLoS One | year= 2013 | volume= 8 | issue= 5 | pages= e63169 | pmid=23675460 | doi=10.1371/journal.pone.0063169 | pmc=3652866 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23675460 }} </ref> <ref name="pmid20651699">{{cite journal| author=Fedorowski A, Engström G, Hedblad B, Melander O| title=Orthostatic hypotension predicts incidence of heart failure: the Malmö preventive project. | journal=Am J Hypertens | year= 2010 | volume= 23 | issue= 11 | pages= 1209-15 | pmid=20651699 | doi=10.1038/ajh.2010.150 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20651699 }} </ref> <ref name="pmid20458003">{{cite journal| author=Fagard RH, De Cort P| title=Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly. | journal=Hypertension | year= 2010 | volume= 56 | issue= 1 | pages= 56-61 | pmid=20458003 | doi=10.1161/HYPERTENSIONAHA.110.151654 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=20458003 }} </ref> <ref name="pmid23216860">{{cite journal| author=Fedorowski A, Melander O| title=Syndromes of orthostatic intolerance: a hidden danger. | journal=J Intern Med | year= 2013 | volume= 273 | issue= 4 | pages= 322-35 | pmid=23216860 | doi=10.1111/joim.12021 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23216860 }} </ref> <ref name="pmid9826316">{{cite journal| author=Masaki KH, Schatz IJ, Burchfiel CM, Sharp DS, Chiu D, Foley D | display-authors=etal| title=Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program. | journal=Circulation | year= 1998 | volume= 98 | issue= 21 | pages= 2290-5 | pmid=9826316 | doi=10.1161/01.cir.98.21.2290 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=9826316 }} </ref> | ||
**Cardiovascular and all-cause mortality | |||
* | **Cardiovascular events | ||
**[[ | **[[Congestive heart failure]] | ||
** | **[[Atrial fibrillation]] | ||
**Cognitive decline or [[dementia]] | |||
**[[Anxiety]], [[depression]], and impaired quality of life | |||
====Prognosis==== | ====Prognosis==== | ||
*Depending on the underlying | *Depending on the underlying cause of [[orthostatic hypotension]], the prognosis may vary. | ||
==Diagnosis== | |||
==Diagnostic study of choice== | ===Diagnostic study of choice=== | ||
*[[Orthostatic vitals]] are the best diagnostic tests that are simple and easy to perform in a clinical setting. | *[[Orthostatic vitals]] are the best diagnostic tests that are simple and easy to perform in a clinical setting. <nowiki></ref></nowiki><ref name="pmid21431947">{{cite journal| author=Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I | display-authors=etal| title=Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. | journal=Clin Auton Res | year= 2011 | volume= 21 | issue= 2 | pages= 69-72 | pmid=21431947 | doi=10.1007/s10286-011-0119-5 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=21431947 }} </ref><ref name="pmid19390349">{{cite journal| author=Wieling W, Schatz IJ| title=The consensus statement on the definition of orthostatic hypotension: a revisit after 13 years. | journal=J Hypertens | year= 2009 | volume= 27 | issue= 5 | pages= 935-8 | pmid=19390349 | doi=10.1097/HJH.0b013e32832b1145 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19390349 }} </ref> | ||
*[[Blood pressure]] and [[heart rate]] should be measured within 2-5 minutes of standing after a 5-minute period of supine rest. | |||
** The optimal time to check standing blood pressure varies<ref name="pmid37668347">{{cite journal| author=Petriceks AH, Appel LJ, Miller ER, Mitchell CM, Schrack JA, Mukamal KJ | display-authors=etal| title=Timing of orthostatic hypotension and its relationship with falls in older adults. | journal=J Am Geriatr Soc | year= 2023 | volume= 71 | issue= 12 | pages= 3711-3720 | pmid=37668347 | doi=10.1111/jgs.18573 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=37668347 }} </ref> | |||
*[[Orthostatic hypotension]] is diagnosed when there is: | |||
**At least a 20 mmHg decline in [[systolic blood pressure]] | |||
**At least 10 mmHg decline in [[diastolic blood pressure]] | |||
*The absence of the normal rise in [[heart rate]] on standing is a diagnostic clue to the presence of [[autonomic dysfunction]]; however, an increased [[heart rate]] cannot exclude autonomic failure. | |||
===History and Symptoms=== | ===History and Symptoms=== | ||
*Symptoms are | *When evaluating a patient with [[orthostatic hypotension]], the following features in history may provide a clue to the diagnosis: <ref name="pmid17904451">{{cite journal| author=Gupta V, Lipsitz LA| title=Orthostatic hypotension in the elderly: diagnosis and treatment. | journal=Am J Med | year= 2007 | volume= 120 | issue= 10 | pages= 841-7 | pmid=17904451 | doi=10.1016/j.amjmed.2007.02.023 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17904451 }} </ref> | ||
*Symptoms | *Use of certain medications known to cause [[orthostatic hypotension]]. | ||
*Recent history of [[volume depletion]] (such as [[fever]], [[fluid restriction]], [[vomiting]], [[diarrhea]], [[hemorrhage]]) | |||
*Medical history of common diseases causing [[orthostatic hypotension]], such as [[congestive heart failure]], [[diabetes]], [[Parkinson's disease]], [[malignancie]]s. | |||
*History of [[alcohol]] consumption | |||
*Particular attention should be made to the presence of neurologic symptoms (e.g., [[parkinsonism]], [[ataxia]], [[peripheral neuropathy]]) or symptoms of [[autonomic dysfunction]] (e.g. abnormal [[pupillary response]], chronic [[constipation]], [[erectile dysfunction]], [[urinary incontinence]]) | |||
*Symptoms of [[orthostatic hypotension]] are prominent immediately upon standing, might improve in sitting position, and disappear in the supine position (i.e., postural symptoms). <ref name="pmid26879239">{{cite journal| author=Palma JA, Norcliffe-Kaufmann L, Kaufmann H| title=An orthostatic hypotension mimic: The inebriation-like syndrome in Parkinson disease. | journal=Mov Disord | year= 2016 | volume= 31 | issue= 4 | pages= 598-600 | pmid=26879239 | doi=10.1002/mds.26516 | pmc=4833617 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26879239 }} </ref><ref name="pmid18256396">{{cite journal| author=Freeman R| title=Clinical practice. Neurogenic orthostatic hypotension. | journal=N Engl J Med | year= 2008 | volume= 358 | issue= 6 | pages= 615-24 | pmid=18256396 | doi=10.1056/NEJMcp074189 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18256396 }} </ref> | |||
*Symptoms may also be seen in association with meals, exercise, and prolonged standing | |||
*Symptoms are due to cerebral [[hypoperfusion]] | |||
*Symptoms usually last for few minutes | |||
*The most common symptoms are [[lightheadedness]] and [[dizziness]] upon standing. | |||
*Other symptoms include: | |||
:*Generalized [[weakness]] | :*Generalized [[weakness]] | ||
:*[[Headache]] | :*[[Headache]] | ||
:*Blurred or dimmed [[eye|vision]] (possibly to the point of momentary [[blindness]]) | :*Blurred or dimmed [[eye|vision]] (possibly to the point of momentary [[blindness]]) | ||
:*[[Fatigue]] | :*[[Fatigue]] | ||
:*[[Cognition|Cognitive]] | :*[[Cognition|Cognitive]] impairment | ||
:*[[ | :*[[Loss of consciousness]] ([[syncope]]) may be seen in severe cases | ||
===Physical Examination=== | ===Physical Examination=== | ||
Common physical examination findings of orthostatic hypotension include checking the blood pressure, pulse, and symptoms while having the patient in the standing and sitting position<ref name="pmid23569093">{{cite journal |vauthors=Stewart JM |title=Common syndromes of orthostatic intolerance |journal=Pediatrics |volume=131 |issue=5 |pages=968–80 |date=May 2013 |pmid=23569093 |pmc=3639459 |doi=10.1542/peds.2012-2610 |url=}}</ref> | Common physical examination findings of orthostatic hypotension include checking the [[blood pressure]], pulse, and symptoms while having the [[patient]] in the standing and sitting position. <ref name="pmid23569093">{{cite journal |vauthors=Stewart JM |title=Common syndromes of orthostatic intolerance |journal=Pediatrics |volume=131 |issue=5 |pages=968–80 |date=May 2013 |pmid=23569093 |pmc=3639459 |doi=10.1542/peds.2012-2610 |url=}}</ref> | ||
===Laboratory Findings=== | |||
There are no diagnostic laboratory findings associated with orthostatic hypotension. While the definitive diagnosis of orthostatic hypotension is made clinically, other tests contribute to understanding the [[risks]] of disease and may provide clues to the selection of [[treatment]] options. These tests include those that access the underlying [[cause]] that may be altered in patients suffering from [[orthostatic hypotension]] | There are no diagnostic laboratory findings associated with orthostatic hypotension. While the definitive diagnosis of orthostatic hypotension is made clinically, other tests contribute to understanding the [[risks]] of disease and may provide clues to the selection of [[treatment]] options. <ref name="pmid17904451">{{cite journal| author=Gupta V, Lipsitz LA| title=Orthostatic hypotension in the elderly: diagnosis and treatment. | journal=Am J Med | year= 2007 | volume= 120 | issue= 10 | pages= 841-7 | pmid=17904451 | doi=10.1016/j.amjmed.2007.02.023 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17904451 }} </ref> | ||
These tests include those that access the underlying [[cause]] that may be altered in patients suffering from [[orthostatic hypotension]]. | |||
*[[CBC]] | *[[CBC]] | ||
| Line 409: | Line 537: | ||
*[[TSH]] | *[[TSH]] | ||
===Electrocardiogram=== | |||
An [[ECG]] may be helpful in the diagnosis of orthostatic hypotension. | An [[ECG]] may be helpful in the diagnosis of cardiovascular causes of [[orthostatic hypotension]]. | ||
===X-ray=== | |||
There are no [[x-ray]] findings associated with orthostatic hypotension. | |||
===Echocardiography=== | |||
===== | Echocardiography may be helpful in the diagnosis of [[orthostatic hypotension]]. Findings on an [[echocardiography]] diagnostic of [[orthostatic hypotension]] include cardiac structural changes such as [[left ventricular hypertrophy]], development of [[diastolic dysfunction]], and decreased right chamber volume. <ref name="pmid26643688">{{cite journal| author=Magnusson M, Holm H, Bachus E, Nilsson P, Leosdottir M, Melander O | display-authors=etal| title=Orthostatic Hypotension and Cardiac Changes After Long-Term Follow-Up. | journal=Am J Hypertens | year= 2016 | volume= 29 | issue= 7 | pages= 847-52 | pmid=26643688 | doi=10.1093/ajh/hpv187 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=26643688 }} </ref> | ||
===CT scan=== | |||
A CT scan may be helpful in the diagnosis of [[orthostatic hypotension]]. Findings on a CT scan diagnostic of [[orthostatic hypotension]] include the presence of a [[cerebral tumor]] or [[communicating hydrocephalus]]. <ref name="pmid23180176">{{cite journal| author=Metzler M, Duerr S, Granata R, Krismer F, Robertson D, Wenning GK| title=Neurogenic orthostatic hypotension: pathophysiology, evaluation, and management. | journal=J Neurol | year= 2013 | volume= 260 | issue= 9 | pages= 2212-9 | pmid=23180176 | doi=10.1007/s00415-012-6736-7 | pmc=3764319 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=23180176 }} </ref> | |||
===== | ===MRI=== | ||
A brain [[MRI]] may be helpful in the diagnosis of [[orthostatic hypotension]]. Findings on a [[MRI]] suggestive of [[orthostatic hypotension]] include: | |||
[[MRI]] | |||
*[[Neurodegenerative disorder]] | *[[Neurodegenerative disorder]] | ||
*[[Stroke]] | *[[Stroke]] | ||
===Other Imaging Findings=== | |||
There are no other diagnostic studies associated with [[orthostatic hypotension]]. | |||
===Other Diagnostic Studies=== | |||
There are no other diagnostic studies associated with [[orthostatic hypotension]]. | |||
==Treatment== | ==Treatment== | ||
| Line 444: | Line 575: | ||
*Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension. | *Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension. | ||
{{familytree/start}} | {{familytree/start}} | ||
{{familytree | | | | | | | | | | | | | | | | A01 | | | | | |A01=Drop of systolic BP > 20 mmHg (30 for hypertensive patients)}} | {{familytree | | | | | | | | | | | | | | | | A01 | | | | | |A01=Drop of systolic BP > 20 mmHg (30 for [[hypertensive]] [[patients]])}} | ||
{{familytree | | | | | | | | | | | | | | | | |!| | | | | | | | }} | {{familytree | | | | | | | | | | | | | | | | |!| | | | | | | | }} | ||
{{familytree | | | | | | | | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | {{familytree | | | | | | | | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| }} | ||
| Line 452: | Line 583: | ||
and follow-up}} | and follow-up}} | ||
{{familytree | | | | | | | | | |!| | | | | | | | | }} | {{familytree | | | | | | | | | |!| | | | | | | | | }} | ||
{{familytree | | | | | | | | | E01 | | | | | | | |E01= | {{familytree | | | | | | | | | E01 | | | | | | | |E01=Persistence of symptoms}} | ||
{{familytree | | | | | | | | | |!| | | | | | | | | }} | {{familytree | | | | | | | | | |!| | | | | | | | | }} | ||
{{familytree | | | | | | | | | E01 | | | | | | | |E01=Pharmacological Treatment}} | {{familytree | | | | | | | | | E01 | | | | | | | |E01=Pharmacological Treatment}} | ||
| Line 458: | Line 589: | ||
{{familytree | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| | }} | {{familytree | | |,|-|-|-|-|-|-|^|-|-|-|-|-|-|.| | }} | ||
{{familytree | | |!| | | | | | | | | | | | | |!| | }} | {{familytree | | |!| | | | | | | | | | | | | |!| | }} | ||
{{familytree | | E01 | | | | | | | | | | | | E02 | | |E01=No supine hypertension or chronic heart failure|E02=Supine hypertension or chronic heart failure: }} | {{familytree | | E01 | | | | | | | | | | | | E02 | | |E01=No supine [[hypertension]] or chronic [[heart failure]]|E02=Supine hypertension or chronic [[heart failure]]: }} | ||
{{familytree | | |!| | | | | | | | | | | | | |!| | }} | {{familytree | | |!| | | | | | | | | | | | | |!| | }} | ||
{{familytree | | E01 | | | | | | | | | | | | E02 | | E01= Fludrocortisone<br>Midodrine|E02=Midodrine}} | {{familytree | | E01 | | | | | | | | | | | | E02 | | E01= [[Fludrocortisone]]<br>[[Midodrine]]|E02=[[Midodrine]]}} | ||
{{familytree/end}} | {{familytree/end}} | ||
===Non Pharmacological Therapy=== | ===Non-Pharmacological Therapy=== | ||
*Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension.<ref name="Singer-2003">{{cite journal | author=Singer W, Opfer-Gehrking TL, McPhee BR, Hilz MJ, Bharucha AE, Low PA. | title=Acetylcholinesterase inhibition: a novel approach in the treatment of neurogenic orthostatic hypotension. | journal=J Neurol Neurosurg Psychiatry | year=2003 | volume=74 | issue=9 | pages=1294-8 | id=PMID 12933939}}</ref><ref name="FigueroaBasford2010">{{cite journal|last1=Figueroa|first1=J. J.|last2=Basford|first2=J. R.|last3=Low|first3=P. A.|title=Preventing and treating orthostatic hypotension: As easy as A, B, C|journal=Cleveland Clinic Journal of Medicine|volume=77|issue=5|year=2010|pages=298–306|issn=0891-1150|doi=10.3949/ccjm.77a.09118}}</ref><ref name="FreemanAbuzinadah2018">{{cite journal|last1=Freeman|first1=Roy|last2=Abuzinadah|first2=Ahmad R.|last3=Gibbons|first3=Christopher|last4=Jones|first4=Pearl|last5=Miglis|first5=Mitchell G.|last6=Sinn|first6=Dong In|title=Orthostatic Hypotension|journal=Journal of the American College of Cardiology|volume=72|issue=11|year=2018|pages=1294–1309|issn=07351097|doi=10.1016/j.jacc.2018.05.079}}</ref><ref name="FreemanAbuzinadah20182">{{cite journal|last1=Freeman|first1=Roy|last2=Abuzinadah|first2=Ahmad R.|last3=Gibbons|first3=Christopher|last4=Jones|first4=Pearl|last5=Miglis|first5=Mitchell G.|last6=Sinn|first6=Dong In|title=Orthostatic Hypotension|journal=Journal of the American College of Cardiology|volume=72|issue=11|year=2018|pages=1294–1309|issn=07351097|doi=10.1016/j.jacc.2018.05.079}}</ref><ref name="pmid/10.1016/j.jacc.2015.06.1084">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=/10.1016/j.jacc.2015.06.1084 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref name="pmid14705758">{{cite journal| author=Bradley JG, Davis KA| title=Orthostatic hypotension. | journal=Am Fam Physician | year= 2003 | volume= 68 | issue= 12 | pages= 2393-8 | pmid=14705758 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14705758 }} </ref><ref name="pmid10071663">{{cite journal| author=Carlson JE| title=Assessment of orthostatic blood pressure: measurement technique and clinical applications. | journal=South Med J | year= 1999 | volume= 92 | issue= 2 | pages= 167-73 | pmid=10071663 | doi=10.1097/00007611-199902000-00002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10071663 }} </ref> | *Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension.<ref name="Singer-2003">{{cite journal | author=Singer W, Opfer-Gehrking TL, McPhee BR, Hilz MJ, Bharucha AE, Low PA. | title=Acetylcholinesterase inhibition: a novel approach in the treatment of neurogenic orthostatic hypotension. | journal=J Neurol Neurosurg Psychiatry | year=2003 | volume=74 | issue=9 | pages=1294-8 | id=PMID 12933939}}</ref><ref name="FigueroaBasford2010">{{cite journal|last1=Figueroa|first1=J. J.|last2=Basford|first2=J. R.|last3=Low|first3=P. A.|title=Preventing and treating orthostatic hypotension: As easy as A, B, C|journal=Cleveland Clinic Journal of Medicine|volume=77|issue=5|year=2010|pages=298–306|issn=0891-1150|doi=10.3949/ccjm.77a.09118}}</ref><ref name="FreemanAbuzinadah2018">{{cite journal|last1=Freeman|first1=Roy|last2=Abuzinadah|first2=Ahmad R.|last3=Gibbons|first3=Christopher|last4=Jones|first4=Pearl|last5=Miglis|first5=Mitchell G.|last6=Sinn|first6=Dong In|title=Orthostatic Hypotension|journal=Journal of the American College of Cardiology|volume=72|issue=11|year=2018|pages=1294–1309|issn=07351097|doi=10.1016/j.jacc.2018.05.079}}</ref><ref name="FreemanAbuzinadah20182">{{cite journal|last1=Freeman|first1=Roy|last2=Abuzinadah|first2=Ahmad R.|last3=Gibbons|first3=Christopher|last4=Jones|first4=Pearl|last5=Miglis|first5=Mitchell G.|last6=Sinn|first6=Dong In|title=Orthostatic Hypotension|journal=Journal of the American College of Cardiology|volume=72|issue=11|year=2018|pages=1294–1309|issn=07351097|doi=10.1016/j.jacc.2018.05.079}}</ref><ref name="pmid/10.1016/j.jacc.2015.06.1084">{{cite journal| author=Schmoldt A, Benthe HF, Haberland G| title=Digitoxin metabolism by rat liver microsomes. | journal=Biochem Pharmacol | year= 1975 | volume= 24 | issue= 17 | pages= 1639-41 | pmid=/10.1016/j.jacc.2015.06.1084 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10 }} </ref><ref name="pmid14705758">{{cite journal| author=Bradley JG, Davis KA| title=Orthostatic hypotension. | journal=Am Fam Physician | year= 2003 | volume= 68 | issue= 12 | pages= 2393-8 | pmid=14705758 | doi= | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=14705758 }} </ref><ref name="pmid10071663">{{cite journal| author=Carlson JE| title=Assessment of orthostatic blood pressure: measurement technique and clinical applications. | journal=South Med J | year= 1999 | volume= 92 | issue= 2 | pages= 167-73 | pmid=10071663 | doi=10.1097/00007611-199902000-00002 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=10071663 }} </ref> | ||
*Cessation of orthostatic hypotension inducing drugs such as [[ | *Cessation of orthostatic hypotension inducing [[drugs]] such as [[anti-hypertensives]]s in patients with a mean [[blood pressure]] below target value is recommended. | ||
*Avoidance of certain factors that aggravate hypotension such as heat, alcohol intake. | *Avoidance of certain factors that aggravate hypotension such as heat, and alcohol intake. | ||
*Consumption of large meals induces [[splanchnic]] [[vasodilation]] thereby resulting in hypotension [[postprandially]]. | *Consumption of large meals induces [[splanchnic]] [[vasodilation]] thereby resulting in hypotension [[postprandially]]. | ||
**Fractionated meals are recommended in patients with postprandial symptoms. | **Fractionated meals are recommended in patients with postprandial symptoms. | ||
| Line 474: | Line 605: | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
!Non-Pharmacological methods | ! align="center" style="background: #4479BA; color: #FFFFFF " |Non-Pharmacological methods | ||
!Mechanism of alleviating hypotension | ! align="center" style="background: #4479BA; color: #FFFFFF " |Mechanism of alleviating hypotension | ||
!Recommendations | ! align="center" style="background: #4479BA; color: #FFFFFF " |Recommendations | ||
|- | |- | ||
|Elastic stockings | |Elastic stockings | ||
| Line 485: | Line 616: | ||
*Leg compression alone is not considered effective. | *Leg compression alone is not considered effective. | ||
**Due to the minor venous capacitance of legs relative to the abdomen. | **Due to the minor venous capacitance of legs relative to the abdomen. | ||
*Separate abdominal and leg compression is recommended to avoid patient | *Separate abdominal and leg compression is recommended to avoid patient discomfort. | ||
|- | |- | ||
|Physical Maneuvers | |Physical Maneuvers | ||
| Line 492: | Line 623: | ||
| | | | ||
*Contraction of a group of muscles | *Contraction of a group of muscles | ||
*Leg | *Leg crossing | ||
*Toe raising | *Toe raising | ||
*Bending at the waist | *Bending at the waist | ||
| Line 498: | Line 629: | ||
|Head up tilt sleeping | |Head up tilt sleeping | ||
| | | | ||
*Enhance orthostatic tolerance upon the first | *Enhance orthostatic tolerance upon the first morning rise | ||
| | | | ||
*Results in reduction in supine hypertension, pressure-natriuresis | *Results in reduction in supine hypertension, pressure-natriuresis | ||
| Line 521: | Line 652: | ||
===Medical Therapy=== | ===Medical Therapy=== | ||
*Pharmacological: Some drugs that are used in the treatment of orthostatic hypotension include [[fludrocortisone]] (Florinef), [[erythropoietin]], [[midodrine]] and [[Pyridostigmine bromide]] (Mestinon)<ref name="pmid19422980">{{cite journal| author=Benditt DG, Nguyen JT| title=Syncope: therapeutic approaches. | journal=J Am Coll Cardiol | year= 2009 | volume= 53 | issue= 19 | pages= 1741-51 | pmid=19422980 | doi=10.1016/j.jacc.2008.12.065 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19422980 }} </ref><ref name="pmid24697914">{{cite journal| author=Wieling W, van Dijk N, Thijs RD, de Lange FJ, Krediet CT, Halliwill JR| title=Physical countermeasures to increase orthostatic tolerance. | journal=J Intern Med | year= 2015 | volume= 277 | issue= 1 | pages= 69-82 | pmid=24697914 | doi=10.1111/joim.12249 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24697914 }} </ref><ref name="pmid18420158">{{cite journal| author=Low PA, Singer W| title=Management of neurogenic orthostatic hypotension: an update. | journal=Lancet Neurol | year= 2008 | volume= 7 | issue= 5 | pages= 451-8 | pmid=18420158 | doi=10.1016/S1474-4422(08)70088-7 | pmc=2628163 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420158 }} </ref><ref name="pmid17346129">{{cite journal| author=Maule S, Papotti G, Naso D, Magnino C, Testa E, Veglio F| title=Orthostatic hypotension: evaluation and treatment. | journal=Cardiovasc Hematol Disord Drug Targets | year= 2007 | volume= 7 | issue= 1 | pages= 63-70 | pmid=17346129 | doi=10.2174/187152907780059029 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17346129 }} </ref> | *Pharmacological: Some drugs that are used in the treatment of orthostatic hypotension include [[fludrocortisone]] (Florinef), [[erythropoietin]], [[midodrine]] and [[Pyridostigmine bromide]] (Mestinon) <ref name="pmid19422980">{{cite journal| author=Benditt DG, Nguyen JT| title=Syncope: therapeutic approaches. | journal=J Am Coll Cardiol | year= 2009 | volume= 53 | issue= 19 | pages= 1741-51 | pmid=19422980 | doi=10.1016/j.jacc.2008.12.065 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19422980 }} </ref><ref name="pmid24697914">{{cite journal| author=Wieling W, van Dijk N, Thijs RD, de Lange FJ, Krediet CT, Halliwill JR| title=Physical countermeasures to increase orthostatic tolerance. | journal=J Intern Med | year= 2015 | volume= 277 | issue= 1 | pages= 69-82 | pmid=24697914 | doi=10.1111/joim.12249 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=24697914 }} </ref><ref name="pmid18420158">{{cite journal| author=Low PA, Singer W| title=Management of neurogenic orthostatic hypotension: an update. | journal=Lancet Neurol | year= 2008 | volume= 7 | issue= 5 | pages= 451-8 | pmid=18420158 | doi=10.1016/S1474-4422(08)70088-7 | pmc=2628163 | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18420158 }} </ref><ref name="pmid17346129">{{cite journal| author=Maule S, Papotti G, Naso D, Magnino C, Testa E, Veglio F| title=Orthostatic hypotension: evaluation and treatment. | journal=Cardiovasc Hematol Disord Drug Targets | year= 2007 | volume= 7 | issue= 1 | pages= 63-70 | pmid=17346129 | doi=10.2174/187152907780059029 | pmc= | url=https://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=17346129 }} </ref> | ||
===Initial Therapy=== | ===Initial Therapy=== | ||
| Line 532: | Line 663: | ||
**Patients should not take droxidopa within four to five hours of bedtime in order to limit supine hypertension. | **Patients should not take droxidopa within four to five hours of bedtime in order to limit supine hypertension. | ||
=== | ===Second-line Therapy=== | ||
*Preferred regimen (1): [[Erythropoietin]] is administered SC or IV at doses between 25 to 75 units/kg three times a week. | *Preferred regimen (1): [[Erythropoietin]] is administered SC or IV at doses between 25 to 75 units/kg three times a week. | ||
*Preferred regimen (1): [[Methylxanthine]] caffeine 100 to 250 mg three times a day with meals. | *Preferred regimen (1): [[Methylxanthine]] caffeine 100 to 250 mg three times a day with meals. | ||
*Preferred regimen (1): [[Pyridostigmine]] initiated at a dose of 30 mg three times daily, up to a maximum dose of 90 mg three times daily. | *Preferred regimen (1): [[Pyridostigmine]] initiated at a dose of 30 mg three times daily, up to a maximum dose of 90 mg three times daily. | ||
*Preferred regimen (1): [[Non-steroidal anti-inflammatory drug| | *Preferred regimen (1): [[Non-steroidal anti-inflammatory drug|Non-steroidal anti-inflammatory drugs]] are rarely effective as monotherapy | ||
**They can supplement treatment with fludrocortisone or a sympathomimetic agent. | **They can supplement treatment with fludrocortisone or a sympathomimetic agent. | ||
=== | ===Third-line Therapy=== | ||
*Preferred regimen (1): [[Atomoxetine]] | *Preferred regimen (1): [[Atomoxetine]] | ||
| Line 556: | Line 687: | ||
*A. Abdominal compression: Wear an abdominal binder when out of bed | *A. Abdominal compression: Wear an abdominal binder when out of bed | ||
*B. A bolus of water/elevate | *B. A bolus of water/elevate bed: On bad days, drink two 8-ounce glasses of cold water prior to prolonged standing and sleep with the head of the bed raised about 4 inches | ||
*C. [[Counter-maneuvers]]: While standing, contract the lower abdominal muscles for about 30 seconds | *C. [[Counter-maneuvers]]: While standing, contract the lower abdominal muscles for about 30 seconds | ||
*D. Drugs: Midodrine, Pyridostigmine, or Fludrocortisone can be used to elevate blood pressure (acknowledge any medications currently taken that can lower blood pressure) | *D. [[Drugs]]: [[Midodrine]], [[Pyridostigmine]], or [[Fludrocortisone]] can be used to elevate [[blood pressure]] (acknowledge any [[medications]] currently taken that can lower [[blood pressure]]) | ||
*E. Education & Exercise: Note any symptoms that indicate a fall in blood pressure while standing, recognize conditions that lower blood pressure (i.e. heavy metals, temperature changes, exercise, change in position) | *E. Education & Exercise: Note any symptoms that indicate a fall in [[blood pressure]] while standing, recognize conditions that lower [[blood pressure]] (i.e. heavy metals, temperature changes, exercise, change in position) | ||
*F. Fluids: Stay hydrated | *F. Fluids: Stay hydrated | ||
==References== | ==References== | ||
{{Reflist|2}} | {{Reflist|2}} | ||
[[Category:Cardiology]] | |||
{{Circulatory system pathology}} | {{Circulatory system pathology}} | ||
[[nl:Orthostatische hypotensie]] | |||
[[es:Hipotensión ortostática]] | [[es:Hipotensión ortostática]] | ||
[[fr:Hypotension orthostatique]] | [[fr:Hypotension orthostatique]] | ||
[[Category:Up-To-Date]] | |||
[[Category: | |||
Latest revision as of 05:20, 19 January 2024
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Mitra Chitsazan, M.D.[2]; Sogand Goudarzi, MD [3]; Norina Usman, M.B.B.S[4]
Synonyms and keywords: Postural hypotension; orthostatic intolerance; head rush; dizzy spell
Overview
Orthostatic hypotension or postural hypotension is defined as a reduction of systolic blood pressure of at least 20 mm Hg or 10 mm Hg in diastolic blood pressure within 3 minutes of standing. A similar fall during head-up tilt test at 60 degrees also defines orthostatic hypotension. Orthostatic hypotension may be asymptomatic or may cause symptoms of lightheadedness, dizziness, blurred vision or cognitive impairment. It may have acute or chronic causes. Management of orthostatic hypotension may be challenging, in particular in patients with orthostatic hypotension and concomitant supine hypertension. [1][2][3]
Classification
- Based on the underlying pathophysiology correlated to a postural drop in blood pressure, orthostatic hypotension can be classified into:
Initial orthostatic hypotension (iOH)
- It is most common in healthy adolescents
- It is demarcated as a brief BP decrease of >40 mmHg systolic or >20 mmHg diastolic with symptomatic cerebral hypoperfusion within five to fifteen seconds after standing, typically resolved by twenty seconds.
Neurogenic orthostatic hypotension (nOH)
- In Neurogenic orthostatic hypotension, the sympathetic noradrenergic nerves continually fail to facilitate the reflexive cardiovascular responses essential to sustain blood pressure in response to orthostatic stress.
- It is described as a constant BP decrease of >20 mmHg systolic or >10 mmHg diastolic, without or with symptoms, within three minutes of head-up tilt or standing.
Delayed orthostatic hypotension (dOH)
- Delayed orthostatic hypotension (dOH) is demarcated as a fall in blood pressure that accomplishes neurogenic orthostatic hypotension criteria but ensues after three minutes.
Neurally mediated syncope (vOH)
- It is also recognized as vasodepressor or vasovagal syncope, it involves a paroxysmal extraction of sympathetic vasopressor tone, frequently during prolonged standing, in patients with an effective autonomic nervous system.
Cardiovascular orthostatic hypotension (cOH)
- Cardiovascular orthostatic hypotension occurs from intravascular hypovolemia or reduced cardiac output along with compensatory tachycardia.
Orthostatic pseudohypotension (pOH)
- It is stated as apparent orthostatic hypotension when baseline supine blood pressure is raised, which may be due to a short time at rest to create a valid baseline, related recumbent hypertension, or fluctuation of baseline blood pressure with labile hypertension [4][5][6][7]
Pathophysiology
- In the standing position, 500 to 1000 mL of blood pools in the lower extremities and splanchnic circulation, causing a rapid decline in venous return to the heart.
- Decreased ventricular filling pressures lower cardiac output and systemic blood pressure. [8][9][10][11][12]
- Baroreceptors located mainly in the aorta and carotid arteries are very sensitive to fluctuations in blood pressure. A fall in blood pressure decreases the stretching of baroreceptors, thus decreasing their firing. The decreased firing of baroreceptors increases sympathetic and decreases parasympathetic outflow.
- This compensatory reflex increases heart rate, contractility and peripheral vascular resistance (i.e., both arteriolar and venous vasoconstriction). These changes result in increased venous return and increased cardiac output, and limit the decline in blood pressure. This compensatory reflex is known as baroreflex.
- Any disruption in this pathway can cause a significant decline in blood pressure upon standing (i.e., orthostatic hypotension), causing symptoms of cerebral hypoperfusion including nausea, dizziness, headache, lightheadedness, blurred vision, and impaired cognition.
- Although many pathologic causes may alter this normal physiologic response to standing, the most common pathophysiologic mechanisms include:
- Autonomic dysfunction affecting the baroreflex (i.e. baroreflex dysfunction)
- Volume depletion
- Adverse effects of certain medications
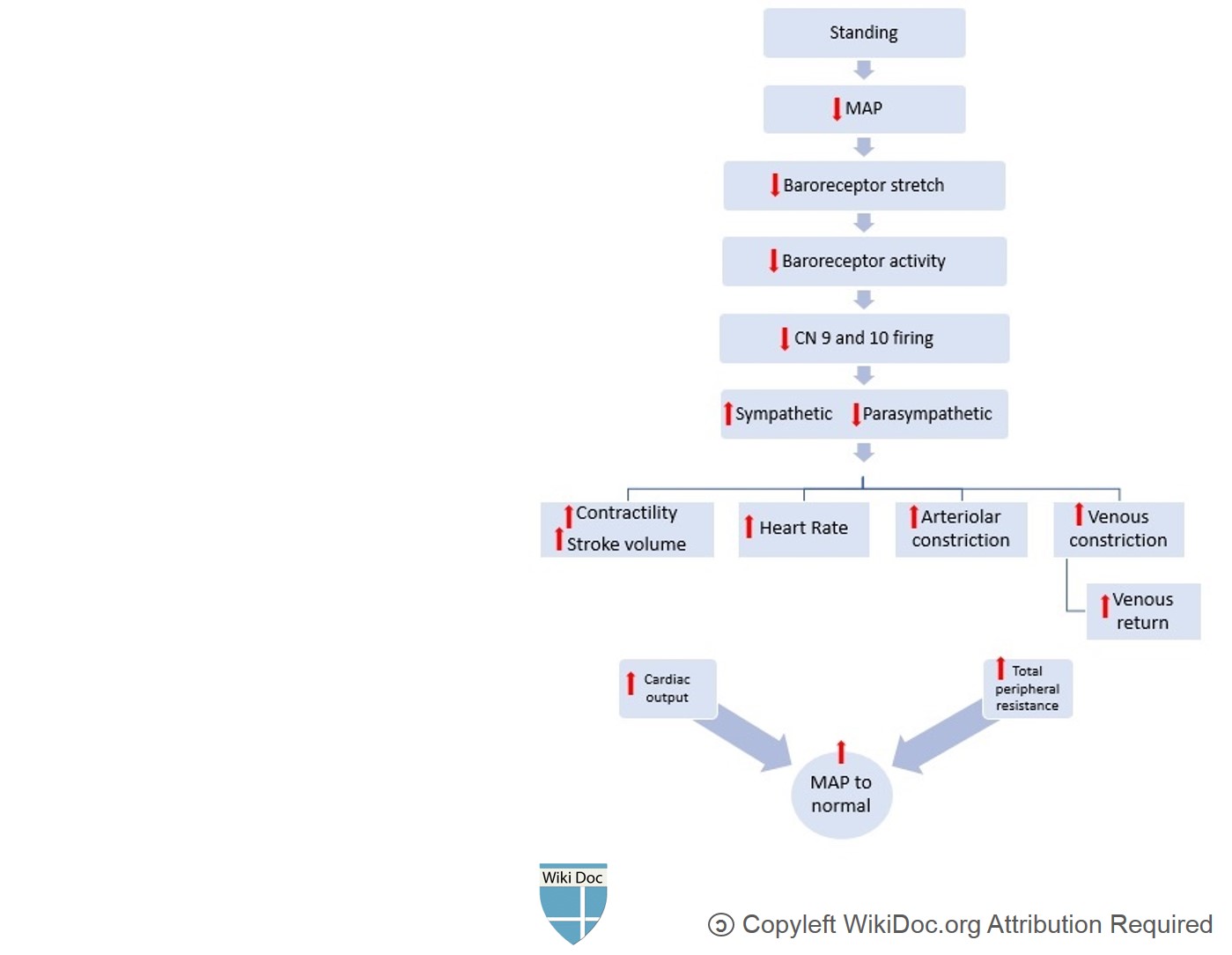
Causes
Common causes of orthostsic hypotension include: [13][14][15][16]
| Causes of orthostatic hypotension |
| Cardiac diseases |
| Intravascular volume depletion |
| Venous pooling/venous vasodilation |
| Autonomic nervous system disorders |
|
|
| Endocrine |
|
| Medications |
| Miscellaneous |
| Medication-induced Orthostatic Hypotension | |
| Vasodilation through Alpha-1 blockade | |
| Vasodilation (Others) | |
| Volume depletion | |
| Sympathetic blockade | |
| Dopamin agonists and other anti-Parkinsonian medications | |
| Others | |
Differentiating Orthostatic Hypotension from Other Diseases
Orthostatic hypotension must be differentiated from neurogenic syncope, cardiogenic syncope, situational syncope, multiple system atrophy with orthostatic hypotension, neurally mediated hypotension, postural orthostatic tachycardia syndrome (POTS) and vasovagal syncope [17][18][19][20][21][22][23]
| Disease | History and Physical Examination | Diagnostic approach | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lightheadedness | Fatigue | Autonomic symptoms | Fever | Nausea/vomiting | Diminished Vision | Dizziness | Slurred Speech | Tachycardia | Altered mentation | Loss of Consciousness | Weakness | Neurological Deficit | Labs and CSF findings | ECG | CT/MRI | Gold standard test | |
| Multiple system atrophy with orthostatic hypotension | + | + | + | - | - | + | + | + | - | + | - | + | + | - | - | Atrophy of brain stem and cerebellum |
|
| Neurally mediated hypotension | + | + | + | - | + | + | + | + | - | + | - | + | - | - | - | - |
|
| 'Postural Orthostatic Tachycardia Syndrome (POTS) | + | + | + | - | - | - | - | - | + | - | - | - | - | - | + | - |
|
| Neurologic syncope | + | - | + | - | + | +/- | + | - | - | - | + | +/- | - | - | - | - |
|
| Cardiac syncope | + | + | + | _ | + | + | + | + | + | +/- | + | + | - | - | + | - | |
| Situational syncope | + | + | + | - | + | + | + | +/- | +/- | +/- | + | +/- | - | - | - | - |
|
| Vasovagal syncope (also known as cardio-neurogenic syncope) | + | + | + | - | + | +/- | + | + | - | + | + | +/- | - | + | + | - | |
Epidemiology and Demographics
Incidence
- The approximation of orthostatic hypotension‐associated hospitalization is 36 per 100,000 adults, and the rate can be as high as 233 per 100,000 patients >75 years of age. [24]
Prevalence
- The overall prevalence of orthostatic hypotension depends on age as it increases with age in the general population.
- The prevalence ranges from 5% in patients <50 years of age to 30% in those >70 years of age.
- It is ~20% in >65-year-old patients. [25][26]
Age
- Orthostatic Hypotension is commonly seen in individuals older than 50 years of age.
Gender
- Orthostatic hypotension affects men and women equally.
Risk Factors
Common risk factors in the development of orthostatic hypotension include: [27][28]
- Age (>65)
- Medications
- Autonomic neuropathies, such asParkinson's disease, diabetes
- Volume depletion
- Postpartum period
- Prolong bedrest.
Screening
- Orthostatic hypotension screening consists of blood pressure measurements in supine (or sitting) and standing position during clinical consultations. [29]
Natural History, Complications, and Prognosis
Natural History
- The symptoms of orthostatic hypotension mainly develop in the elderly, and start with generalized symptoms of dizziness, lightheadedness, or syncope and less frequently with headache, leg buckling, or chest pain [30][1]
Complications
Common complications of orthostatic hypotension include: [31][32]
- Symptomatic orthostatic hypotension may cause falling. [33] [34]
- The risk of recurrent falls is particularly higher in frail, older adults.
- According to various studies, orthostatic hypotension may be a risk factor for: [35] [36] [37] [38] [39] [40]
- Cardiovascular and all-cause mortality
- Cardiovascular events
- Congestive heart failure
- Atrial fibrillation
- Cognitive decline or dementia
- Anxiety, depression, and impaired quality of life
Prognosis
- Depending on the underlying cause of orthostatic hypotension, the prognosis may vary.
Diagnosis
Diagnostic study of choice
- Orthostatic vitals are the best diagnostic tests that are simple and easy to perform in a clinical setting. </ref>[6][7]
- Blood pressure and heart rate should be measured within 2-5 minutes of standing after a 5-minute period of supine rest.
- The optimal time to check standing blood pressure varies[41]
- Orthostatic hypotension is diagnosed when there is:
- At least a 20 mmHg decline in systolic blood pressure
- At least 10 mmHg decline in diastolic blood pressure
- The absence of the normal rise in heart rate on standing is a diagnostic clue to the presence of autonomic dysfunction; however, an increased heart rate cannot exclude autonomic failure.
History and Symptoms
- When evaluating a patient with orthostatic hypotension, the following features in history may provide a clue to the diagnosis: [42]
- Use of certain medications known to cause orthostatic hypotension.
- Recent history of volume depletion (such as fever, fluid restriction, vomiting, diarrhea, hemorrhage)
- Medical history of common diseases causing orthostatic hypotension, such as congestive heart failure, diabetes, Parkinson's disease, malignancies.
- History of alcohol consumption
- Particular attention should be made to the presence of neurologic symptoms (e.g., parkinsonism, ataxia, peripheral neuropathy) or symptoms of autonomic dysfunction (e.g. abnormal pupillary response, chronic constipation, erectile dysfunction, urinary incontinence)
- Symptoms of orthostatic hypotension are prominent immediately upon standing, might improve in sitting position, and disappear in the supine position (i.e., postural symptoms). [43][44]
- Symptoms may also be seen in association with meals, exercise, and prolonged standing
- Symptoms are due to cerebral hypoperfusion
- Symptoms usually last for few minutes
- The most common symptoms are lightheadedness and dizziness upon standing.
- Other symptoms include:
Physical Examination
Common physical examination findings of orthostatic hypotension include checking the blood pressure, pulse, and symptoms while having the patient in the standing and sitting position. [45]
Laboratory Findings
There are no diagnostic laboratory findings associated with orthostatic hypotension. While the definitive diagnosis of orthostatic hypotension is made clinically, other tests contribute to understanding the risks of disease and may provide clues to the selection of treatment options. [42] These tests include those that access the underlying cause that may be altered in patients suffering from orthostatic hypotension.
Electrocardiogram
An ECG may be helpful in the diagnosis of cardiovascular causes of orthostatic hypotension.
X-ray
There are no x-ray findings associated with orthostatic hypotension.
Echocardiography
Echocardiography may be helpful in the diagnosis of orthostatic hypotension. Findings on an echocardiography diagnostic of orthostatic hypotension include cardiac structural changes such as left ventricular hypertrophy, development of diastolic dysfunction, and decreased right chamber volume. [46]
CT scan
A CT scan may be helpful in the diagnosis of orthostatic hypotension. Findings on a CT scan diagnostic of orthostatic hypotension include the presence of a cerebral tumor or communicating hydrocephalus. [47]
MRI
A brain MRI may be helpful in the diagnosis of orthostatic hypotension. Findings on a MRI suggestive of orthostatic hypotension include:
Other Imaging Findings
There are no other diagnostic studies associated with orthostatic hypotension.
Other Diagnostic Studies
There are no other diagnostic studies associated with orthostatic hypotension.
Treatment
- Asymptomatic hypotension is a common finding in practice and does not require any treatment.
- There is no specific target blood pressure goals in the management of orthostatic hypotension.
- However, management is targeted to alleviate symptoms, prevention of future falls, and excessive supine hypertension.
- Management of orthostatic hypotension can be categorized into lifestyle modifications and medical therapy.
- Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension.
| Drop of systolic BP > 20 mmHg (30 for hypertensive patients) | |||||||||||||||||||||||||||||||||||||||||||||||||
| Symptomatic | Asymptomatic | ||||||||||||||||||||||||||||||||||||||||||||||||
| Non-pharmacological treatment | Observation and follow-up | ||||||||||||||||||||||||||||||||||||||||||||||||
| Persistence of symptoms | |||||||||||||||||||||||||||||||||||||||||||||||||
| Pharmacological Treatment | |||||||||||||||||||||||||||||||||||||||||||||||||
| No supine hypertension or chronic heart failure | Supine hypertension or chronic heart failure: | ||||||||||||||||||||||||||||||||||||||||||||||||
| Fludrocortisone Midodrine | Midodrine | ||||||||||||||||||||||||||||||||||||||||||||||||
Non-Pharmacological Therapy
- Education of the patient and non-pharmacological treatments are the cornerstone of treatment of orthostatic hypotension.[48][49][50][51][52][1][53]
- Cessation of orthostatic hypotension inducing drugs such as anti-hypertensivess in patients with a mean blood pressure below target value is recommended.
- Avoidance of certain factors that aggravate hypotension such as heat, and alcohol intake.
- Consumption of large meals induces splanchnic vasodilation thereby resulting in hypotension postprandially.
- Fractionated meals are recommended in patients with postprandial symptoms.
| Non-Pharmacological methods | Mechanism of alleviating hypotension | Recommendations |
|---|---|---|
| Elastic stockings |
|
|
| Physical Maneuvers |
|
|
| Head up tilt sleeping |
|
|
| Intravascular volume |
|
|
| Intake of cold water |
|
|
Medical Therapy
- Pharmacological: Some drugs that are used in the treatment of orthostatic hypotension include fludrocortisone (Florinef), erythropoietin, midodrine and Pyridostigmine bromide (Mestinon) [54][55][56][57]
Initial Therapy
- Preferred regimen (1): Fludrocortisone acetate at a dose of 0.1 mg per day, administered in the morning, which can eventually be increased up to 0.3 mg per day.
- Considered first-line regimen for hypotension in the absence of heart failure and supine hypertension
- Preferred regimen (2): Midodrine 2.5 to 10 mg three times a day.
- Max dose should not exceed 40 mg/day.
- Preferred regimen (2): Droxidopa starts at 100 mg and escalates to 600 mg three times per day.
- Patients should not take droxidopa within four to five hours of bedtime in order to limit supine hypertension.
Second-line Therapy
- Preferred regimen (1): Erythropoietin is administered SC or IV at doses between 25 to 75 units/kg three times a week.
- Preferred regimen (1): Methylxanthine caffeine 100 to 250 mg three times a day with meals.
- Preferred regimen (1): Pyridostigmine initiated at a dose of 30 mg three times daily, up to a maximum dose of 90 mg three times daily.
- Preferred regimen (1): Non-steroidal anti-inflammatory drugs are rarely effective as monotherapy
- They can supplement treatment with fludrocortisone or a sympathomimetic agent.
Third-line Therapy
- Preferred regimen (1): Atomoxetine
- Preferred regimen (1): Vasopressin analogs (desmopressin (DDAVP))
- Preferred regimen (1): Yohimbine a single dose of yohimbine (5.4 mg).
- Yohimbine has limited availability in the United States.
- Preferred regimen (1): Somatostatin subcutaneous doses range from 25 to 200 mcg.
- Preferred regimen (1): Ergotamine-caffeine (1 mg/100 mg) up to twice-daily dosing in patients with orthostatic hypotension.
- Preferred regimen (1): Metoclopramide and domperidone
Primary Prevention
Effective measures for the primary prevention of orthostatic hypotension include:
ABCDEF method
- A. Abdominal compression: Wear an abdominal binder when out of bed
- B. A bolus of water/elevate bed: On bad days, drink two 8-ounce glasses of cold water prior to prolonged standing and sleep with the head of the bed raised about 4 inches
- C. Counter-maneuvers: While standing, contract the lower abdominal muscles for about 30 seconds
- D. Drugs: Midodrine, Pyridostigmine, or Fludrocortisone can be used to elevate blood pressure (acknowledge any medications currently taken that can lower blood pressure)
- E. Education & Exercise: Note any symptoms that indicate a fall in blood pressure while standing, recognize conditions that lower blood pressure (i.e. heavy metals, temperature changes, exercise, change in position)
- F. Fluids: Stay hydrated
References
- ↑ 1.0 1.1 1.2 Bradley JG, Davis KA (2003). "Orthostatic hypotension". Am Fam Physician. 68 (12): 2393–8. PMID 14705758.
- ↑ Rutan GH, Hermanson B, Bild DE, Kittner SJ, LaBaw F, Tell GS (1992). "Orthostatic hypotension in older adults. The Cardiovascular Health Study. CHS Collaborative Research Group". Hypertension. 19 (6 Pt 1): 508–19. doi:10.1161/01.hyp.19.6.508. PMID 1592445.
- ↑ Ooi WL, Barrett S, Hossain M, Kelley-Gagnon M, Lipsitz LA (1997). "Patterns of orthostatic blood pressure change and their clinical correlates in a frail, elderly population". JAMA. 277 (16): 1299–304. PMID 9109468.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID https://doi.org/10.1007/s10286-016-0382-6 Check
|pmid=value (help). - ↑ Wieling W, Krediet CT, van Dijk N, Linzer M, Tschakovsky ME (2007). "Initial orthostatic hypotension: review of a forgotten condition". Clin Sci (Lond). 112 (3): 157–65. doi:10.1042/CS20060091. PMID 17199559.
- ↑ 6.0 6.1 Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I; et al. (2011). "Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome". Clin Auton Res. 21 (2): 69–72. doi:10.1007/s10286-011-0119-5. PMID 21431947.
- ↑ 7.0 7.1 Wieling W, Schatz IJ (2009). "The consensus statement on the definition of orthostatic hypotension: a revisit after 13 years". J Hypertens. 27 (5): 935–8. doi:10.1097/HJH.0b013e32832b1145. PMID 19390349.
- ↑ Lipsitz LA (1989). "Orthostatic hypotension in the elderly". N Engl J Med. 321 (14): 952–7. doi:10.1056/NEJM198910053211407. PMID 2674714.
- ↑ Low PA, Opfer-Gehrking TL, McPhee BR, Fealey RD, Benarroch EE, Willner CL; et al. (1995). "Prospective evaluation of clinical characteristics of orthostatic hypotension". Mayo Clin Proc. 70 (7): 617–22. doi:10.4065/70.7.617. PMID 7791382.
- ↑ Zaqqa M, Massumi A (2000). "Neurally mediated syncope". Tex Heart Inst J. 27 (3): 268–72. PMC 101078. PMID 11093411.
- ↑ Mathias CJ (1995). "Orthostatic hypotension: causes, mechanisms, and influencing factors". Neurology. 45 (4 Suppl 5): S6–11. PMID 7746371.
- ↑ Hollister AS (1992). "Orthostatic hypotension. Causes, evaluation, and management". West J Med. 157 (6): 652–7. PMC 1022100. PMID 1475949.
- ↑ Jiang W, Davidson JR. (2005). "Antidepressant therapy in patients with ischemic heart disease". Am Heart J. 150 (5): 871–81. PMID 16290952.
- ↑ Delini-Stula A, Baier D, Kohnen R, Laux G, Philipp M, Scholz HJ. (1999). "Undesirable blood pressure changes under naturalistic treatment with moclobemide, a reversible MAO-A inhibitor--results of the drug utilization observation studies". Pharmacopsychiatry. 32 (2): 61–7. PMID 10333164.
- ↑ Jones RT. (2002). "Cardiovascular system effcts of marijuana". J Clin Pharmacol. 42 (11 Suppl): 58S–63S. PMID 12412837.
- ↑ Hohmann M, Künzel W (1991). "Orthostatic hypotension and birthweight". Arch. Gynecol. Obstet. 248 (4): 181–9. doi:10.1007/bf02390357. PMID 1898124.
- ↑ Poewe W, Seppi K, Fitzer-Attas CJ, Wenning GK, Gilman S, Low PA; et al. (2015). "Efficacy of rasagiline in patients with the parkinsonian variant of multiple system atrophy: a randomised, placebo-controlled trial". Lancet Neurol. 14 (2): 145–52. doi:10.1016/S1474-4422(14)70288-1. PMID 25498732.
- ↑ Brignole M (2005). "Neurally-mediated syncope". Ital Heart J. 6 (3): 249–55. PMID 15875516.
- ↑ Trahair LG, Horowitz M, Jones KL (2014). "Postprandial hypotension: a systematic review". J Am Med Dir Assoc. 15 (6): 394–409. doi:10.1016/j.jamda.2014.01.011. PMID 24630686.
- ↑ Garland EM, Celedonio JE, Raj SR (2015). "Postural Tachycardia Syndrome: Beyond Orthostatic Intolerance". Curr Neurol Neurosci Rep. 15 (9): 60. doi:10.1007/s11910-015-0583-8. PMC 4664448. PMID 26198889.
- ↑ Cheshire WP (2017). "Syncope". Continuum (Minneap Minn). 23 (2, Selected Topics in Outpatient Neurology): 335–358. doi:10.1212/CON.0000000000000444. PMID 28375909.
- ↑ Dohrmann ML, Cheitlin MD (1986). "Cardiogenic syncope. Seizure versus syncope". Neurol Clin. 4 (3): 549–62. PMID 3528810.
- ↑ Aydin MA, Salukhe TV, Wilke I, Willems S (2010). "Management and therapy of vasovagal syncope: A review". World J Cardiol. 2 (10): 308–15. doi:10.4330/wjc.v2.i10.308. PMC 2998831. PMID 21160608.
- ↑ Palma JA, Kaufmann H (2017). "Epidemiology, Diagnosis, and Management of [[Neurogenic Orthostatic Hypotension]]". Mov Disord Clin Pract. 4 (3): 298–308. doi:10.1002/mdc3.12478. PMC 5506688. PMID 28713844. URL–wikilink conflict (help)
- ↑ Ricci F, De Caterina R, Fedorowski A (2015). "Orthostatic Hypotension: Epidemiology, Prognosis, and Treatment". J Am Coll Cardiol. 66 (7): 848–860. doi:10.1016/j.jacc.2015.06.1084. PMID 26271068.
- ↑ Low PA (2008). "Prevalence of orthostatic hypotension". Clin Auton Res. 18 Suppl 1: 8–13. doi:10.1007/s10286-007-1001-3. PMID 18368301.
- ↑ Arnold, Amy C.; Shibao, Cyndya (2013). "Current Concepts in Orthostatic Hypotension Management". Current Hypertension Reports. 15 (4): 304–312. doi:10.1007/s11906-013-0362-3. ISSN 1522-6417.
- ↑ Canobbio, Mary M.; Warnes, Carole A.; Aboulhosn, Jamil; Connolly, Heidi M.; Khanna, Amber; Koos, Brian J.; Mital, Seema; Rose, Carl; Silversides, Candice; Stout, Karen (2017). "Management of Pregnancy in Patients With Complex Congenital Heart Disease: A Scientific Statement for Healthcare Professionals From the American Heart Association". Circulation. 135 (8). doi:10.1161/CIR.0000000000000458. ISSN 0009-7322.
- ↑ Cremer A, Rousseau AL, Boulestreau R, Kuntz S, Tzourio C, Gosse P (2019). "Screening for orthostatic hypotension using home blood pressure measurements". J Hypertens. 37 (5): 923–927. doi:10.1097/HJH.0000000000001986. PMID 30418320.
- ↑ "StatPearls". 2020. PMID 28846238.
- ↑ Romero-Ortuno R, Cogan L, Foran T, Kenny RA, Fan CW (April 2011). "Continuous noninvasive orthostatic blood pressure measurements and their relationship with orthostatic intolerance, falls, and frailty in older people". J Am Geriatr Soc. 59 (4): 655–65. doi:10.1111/j.1532-5415.2011.03352.x. PMID 21438868.
- ↑ Ricci, Fabrizio; Fedorowski, Artur; Radico, Francesco; Romanello, Mattia; Tatasciore, Alfonso; Di Nicola, Marta; Zimarino, Marco; De Caterina, Raffaele (2015). "Cardiovascular morbidity and mortality related to orthostatic hypotension: a meta-analysis of prospective observational studies". European Heart Journal. 36 (25): 1609–1617. doi:10.1093/eurheartj/ehv093. ISSN 0195-668X.
- ↑ van Hateren KJ, Kleefstra N, Blanker MH, Ubink-Veltmaat LJ, Groenier KH, Houweling ST; et al. (2012). "Orthostatic hypotension, diabetes, and falling in older patients: a cross-sectional study". Br J Gen Pract. 62 (603): e696–702. doi:10.3399/bjgp12X656838. PMC 3459777. PMID 23265229.
- ↑ Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P; et al. (2011). "Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study". J Am Geriatr Soc. 59 (3): 383–9. doi:10.1111/j.1532-5415.2011.03317.x. PMC 3306056. PMID 21391928.
- ↑ Fedorowski A, Hedblad B, Engström G, Gustav Smith J, Melander O (2010). "Orthostatic hypotension and long-term incidence of atrial fibrillation: the Malmö Preventive Project". J Intern Med. 268 (4): 383–9. doi:10.1111/j.1365-2796.2010.02261.x. PMID 20698925.
- ↑ Xin W, Lin Z, Li X (2013). "Orthostatic hypotension and the risk of congestive heart failure: a meta-analysis of prospective cohort studies". PLoS One. 8 (5): e63169. doi:10.1371/journal.pone.0063169. PMC 3652866. PMID 23675460.
- ↑ Fedorowski A, Engström G, Hedblad B, Melander O (2010). "Orthostatic hypotension predicts incidence of heart failure: the Malmö preventive project". Am J Hypertens. 23 (11): 1209–15. doi:10.1038/ajh.2010.150. PMID 20651699.
- ↑ Fagard RH, De Cort P (2010). "Orthostatic hypotension is a more robust predictor of cardiovascular events than nighttime reverse dipping in elderly". Hypertension. 56 (1): 56–61. doi:10.1161/HYPERTENSIONAHA.110.151654. PMID 20458003.
- ↑ Fedorowski A, Melander O (2013). "Syndromes of orthostatic intolerance: a hidden danger". J Intern Med. 273 (4): 322–35. doi:10.1111/joim.12021. PMID 23216860.
- ↑ Masaki KH, Schatz IJ, Burchfiel CM, Sharp DS, Chiu D, Foley D; et al. (1998). "Orthostatic hypotension predicts mortality in elderly men: the Honolulu Heart Program". Circulation. 98 (21): 2290–5. doi:10.1161/01.cir.98.21.2290. PMID 9826316.
- ↑ Petriceks AH, Appel LJ, Miller ER, Mitchell CM, Schrack JA, Mukamal KJ; et al. (2023). "Timing of orthostatic hypotension and its relationship with falls in older adults". J Am Geriatr Soc. 71 (12): 3711–3720. doi:10.1111/jgs.18573. PMID 37668347 Check
|pmid=value (help). - ↑ 42.0 42.1 Gupta V, Lipsitz LA (2007). "Orthostatic hypotension in the elderly: diagnosis and treatment". Am J Med. 120 (10): 841–7. doi:10.1016/j.amjmed.2007.02.023. PMID 17904451.
- ↑ Palma JA, Norcliffe-Kaufmann L, Kaufmann H (2016). "An orthostatic hypotension mimic: The inebriation-like syndrome in Parkinson disease". Mov Disord. 31 (4): 598–600. doi:10.1002/mds.26516. PMC 4833617. PMID 26879239.
- ↑ Freeman R (2008). "Clinical practice. Neurogenic orthostatic hypotension". N Engl J Med. 358 (6): 615–24. doi:10.1056/NEJMcp074189. PMID 18256396.
- ↑ Stewart JM (May 2013). "Common syndromes of orthostatic intolerance". Pediatrics. 131 (5): 968–80. doi:10.1542/peds.2012-2610. PMC 3639459. PMID 23569093.
- ↑ Magnusson M, Holm H, Bachus E, Nilsson P, Leosdottir M, Melander O; et al. (2016). "Orthostatic Hypotension and Cardiac Changes After Long-Term Follow-Up". Am J Hypertens. 29 (7): 847–52. doi:10.1093/ajh/hpv187. PMID 26643688.
- ↑ Metzler M, Duerr S, Granata R, Krismer F, Robertson D, Wenning GK (2013). "Neurogenic orthostatic hypotension: pathophysiology, evaluation, and management". J Neurol. 260 (9): 2212–9. doi:10.1007/s00415-012-6736-7. PMC 3764319. PMID 23180176.
- ↑ Singer W, Opfer-Gehrking TL, McPhee BR, Hilz MJ, Bharucha AE, Low PA. (2003). "Acetylcholinesterase inhibition: a novel approach in the treatment of neurogenic orthostatic hypotension". J Neurol Neurosurg Psychiatry. 74 (9): 1294–8. PMID 12933939.
- ↑ Figueroa, J. J.; Basford, J. R.; Low, P. A. (2010). "Preventing and treating orthostatic hypotension: As easy as A, B, C". Cleveland Clinic Journal of Medicine. 77 (5): 298–306. doi:10.3949/ccjm.77a.09118. ISSN 0891-1150.
- ↑ Freeman, Roy; Abuzinadah, Ahmad R.; Gibbons, Christopher; Jones, Pearl; Miglis, Mitchell G.; Sinn, Dong In (2018). "Orthostatic Hypotension". Journal of the American College of Cardiology. 72 (11): 1294–1309. doi:10.1016/j.jacc.2018.05.079. ISSN 0735-1097.
- ↑ Freeman, Roy; Abuzinadah, Ahmad R.; Gibbons, Christopher; Jones, Pearl; Miglis, Mitchell G.; Sinn, Dong In (2018). "Orthostatic Hypotension". Journal of the American College of Cardiology. 72 (11): 1294–1309. doi:10.1016/j.jacc.2018.05.079. ISSN 0735-1097.
- ↑ Schmoldt A, Benthe HF, Haberland G (1975). "Digitoxin metabolism by rat liver microsomes". Biochem Pharmacol. 24 (17): 1639–41. PMID /10.1016/j.jacc.2015.06.1084 Check
|pmid=value (help). - ↑ Carlson JE (1999). "Assessment of orthostatic blood pressure: measurement technique and clinical applications". South Med J. 92 (2): 167–73. doi:10.1097/00007611-199902000-00002. PMID 10071663.
- ↑ Benditt DG, Nguyen JT (2009). "Syncope: therapeutic approaches". J Am Coll Cardiol. 53 (19): 1741–51. doi:10.1016/j.jacc.2008.12.065. PMID 19422980.
- ↑ Wieling W, van Dijk N, Thijs RD, de Lange FJ, Krediet CT, Halliwill JR (2015). "Physical countermeasures to increase orthostatic tolerance". J Intern Med. 277 (1): 69–82. doi:10.1111/joim.12249. PMID 24697914.
- ↑ Low PA, Singer W (2008). "Management of neurogenic orthostatic hypotension: an update". Lancet Neurol. 7 (5): 451–8. doi:10.1016/S1474-4422(08)70088-7. PMC 2628163. PMID 18420158.
- ↑ Maule S, Papotti G, Naso D, Magnino C, Testa E, Veglio F (2007). "Orthostatic hypotension: evaluation and treatment". Cardiovasc Hematol Disord Drug Targets. 7 (1): 63–70. doi:10.2174/187152907780059029. PMID 17346129.