Ropinirole
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Vignesh Ponnusamy, M.B.B.S. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Ropinirole is a dopamine agonist that is FDA approved for the {{{indicationType}}} of parkinson’s disease (PD) and primary restless legs syndrome (RLS). Common adverse reactions include nausea, somnolence, dizziness, syncope, asthenic condition, viral infection, leg edema, vomiting, and dyspepsia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Parkinson's Disease
- Dosing Information
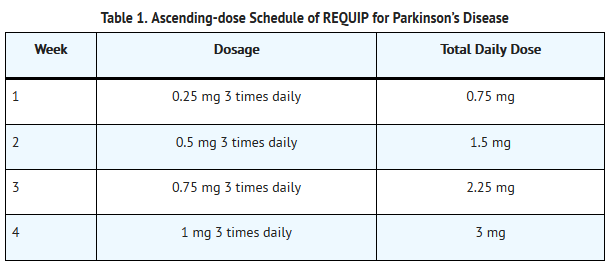
- The recommended starting dose for Parkinson’s disease is 0.25 mg three times daily. Based on individual patient therapeutic response and tolerability, if necessary, the dose should then be titrated with weekly increments as described in Table 1. After Week 4, if necessary, the daily dose may be increased by 1.5 mg/day on a weekly basis up to a dose of 9 mg/day, and then by up to 3 mg/day weekly up to a maximum recommended total daily dose of 24 mg/day (8 mg three times daily). Doses greater than 24 mg/day have not been tested in clinical trials.
- REQUIP should be discontinued gradually over a 7-day period in patients with Parkinson’s disease. The frequency of administration should be reduced from three times daily to twice daily for 4 days. For the remaining 3 days, the frequency should be reduced to once daily prior to complete withdrawal of REQUIP.
- Renal Impairment
- No dose adjustment is necessary in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). The recommended initial dose of ropinirole for patients with end-stage renal disease on hemodialysis is 0.25 mg three times a day. Further dose escalations should be based on tolerability and need for efficacy. The recommended maximum total daily dose is 18 mg/day in patients receiving regular dialysis. Supplemental doses after dialysis are not required. The use of REQUIP in patients with severe renal impairment without regular dialysis has not been studied.
Restless leg syndrome
- Dosing Information
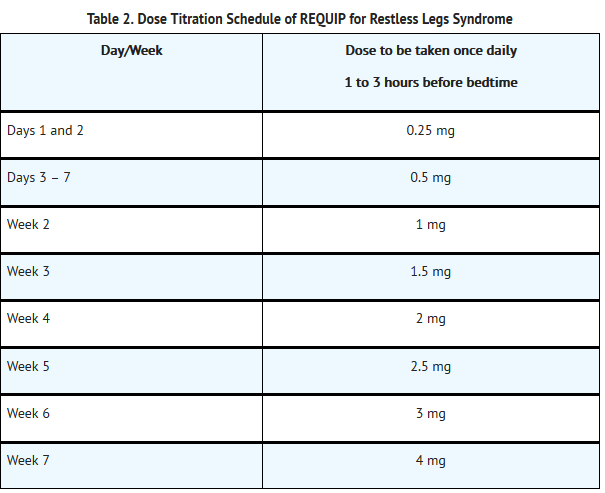
- The recommended adult starting dose for RLS is 0.25 mg once daily 1 to 3 hours before bedtime. After 2 days, if necessary, the dose can be increased to 0.5 mg once daily, and to 1 mg once daily at the end of the first week of dosing, then as shown in Table 2 as needed to achieve efficacy. Titration should be based on individual patient therapeutic response and tolerability, up to a maximum recommended dose of 4 mg daily. For RLS, the safety and effectiveness of doses greater than 4 mg once daily have not been established.
- In clinical trials of patients treated for RLS with doses up to 4 mg once daily, REQUIP was discontinued without a taper.
- Renal Impairment
- No dose adjustment is necessary in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). The recommended initial dose of ropinirole for patients with end-stage renal disease on hemodialysis is 0.25 mg once daily. Further dose escalations should be based on tolerability and need for efficacy. The recommended maximum total daily dose is 3 mg/day in patients receiving regular dialysis. Supplemental doses after dialysis are not required. The use of REQUIP in patients with severe renal impairment without regular dialysis has not been studied.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ropinirole in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ropinirole in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Ropinirole in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Ropinirole in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Ropinirole in pediatric patients.
Contraindications
- REQUIP is contraindicated in patients known to have a hypersensitivity/allergic reaction (including urticaria, angioedema, rash, pruritus) to ropinirole or to any of the excipients.
Warnings
Precautions
- Falling Asleep during Activities of Daily Living and Somnolence
- Patients treated with REQUIP have reported falling asleep while engaged in activities of daily living, including driving or operating machinery, which sometimes resulted in accidents. Although many of these patients reported somnolence while on REQUIP, some perceived that they had no warning signs, such as excessive drowsiness, and believed that they were alert immediately prior to the event. Some have reported these events more than 1 year after initiation of treatment.
- In controlled clinical trials, somnolence was commonly reported in patients receiving REQUIP and was more frequent in Parkinson's disease (up to 40% REQUIP, 6% placebo) than in Restless Legs Syndrome (12% REQUIP, 6% placebo).
- It has been reported that falling asleep while engaged in activities of daily living usually occurs in a setting of preexisting somnolence, although patients may not give such a history. For this reason, prescribers should reassess patients for drowsiness or sleepiness, especially since some of the events occur well after the start of treatment. Prescribers should also be aware that patients may not acknowledge drowsiness or sleepiness until directly questioned about drowsiness or sleepiness during specific activities.
- Before initiating treatment with REQUIP, patients should be advised of the potential to develop drowsiness and specifically asked about factors that may increase the risk with REQUIP such as concomitant sedating medications, the presence of sleep disorders (other than RLS), and concomitant medications that increase ropinirole plasma levels (e.g., ciprofloxacin). If a patient develops significant daytime sleepiness or episodes of falling asleep during activities that require active participation (e.g., driving a motor vehicle, conversations, eating), REQUIP should ordinarily be discontinued. If a decision is made to continue REQUIP, patients should be advised to not drive and to avoid other potentially dangerous activities. There is insufficient information to establish that dose reduction will eliminate episodes of falling asleep while engaged in activities of daily living.
- Syncope
- Syncope, sometimes associated with bradycardia, was observed in association with ropinirole in both patients with Parkinson’s disease and patients with RLS. In controlled clinical trials in patients with Parkinson’s disease, syncope was observed more frequently in patients receiving REQUIP than in patients receiving placebo (early Parkinson’s disease without L-dopa: REQUIP 12%, placebo 1%; advanced Parkinson’s disease: REQUIP 3%, placebo 2%). Syncope was reported in 1% of patients treated with REQUIP for RLS in 12-week, placebo-controlled clinical trials compared with 0.2% of patients treated with placebo. Most cases occurred more than 4 weeks after initiation of therapy with REQUIP, and were usually associated with a recent increase in dose.
- Because the trials of REQUIP excluded patients with significant cardiovascular disease, patients with significant cardiovascular disease should be treated with caution.
- Approximately 4% of patients with Parkinson’s disease enrolled in Phase 1 trials had syncope following a 1-mg dose of REQUIP. In two trials in patients with RLS that used a forced-titration regimen and orthostatic challenge with intensive blood pressure monitoring, 2% of RLS patients treated with REQUIP compared with 0% of patients receiving placebo reported syncope.
- In Phase 1 trials including healthy volunteers, the incidence of syncope was 2%. Of note, 1 subject with syncope developed hypotension, bradycardia, and sinus arrest; the subject recovered spontaneously without intervention.
- Hypotension/Orthostatic Hypotension
- Dopamine agonists in clinical trials and clinical experience appear to impair the systemic regulation of blood pressure, with resulting orthostatic hypotension, especially during dose escalation. In addition, patients with Parkinson’s disease appear to have an impaired capacity to respond to a postural challenge. For these reasons, patients should be monitored for signs and symptoms of orthostatic hypotension, especially during dose escalation, and patients should be informed of the risk for syncope and hypotension.
- Although the clinical trials were not designed to systematically monitor blood pressure, there were individual reported cases of orthostatic hypotension in early Parkinson’s disease (without L-dopa) in patients treated with REQUIP. Most of these cases occurred more than 4 weeks after initiation of therapy with REQUIP and were usually associated with a recent increase in dose.
- In 12-week, placebo-controlled trials of patients with RLS, the adverse event orthostatic hypotension was reported by 4 of 496 patients (0.8%) treated with REQUIP compared with 2 of 500 patients (0.4%) receiving placebo.
- In two Phase 2 studies in patients with RLS, 14 of 55 patients (25%) receiving REQUIP experienced an adverse event of hypotension or orthostatic hypotension compared with none of the 27 patients receiving placebo. In these studies, 11 of the 55 patients (20%) receiving REQUIP and 3 of the 26 patients (12%) who had post-dose blood pressure assessments following placebo, experienced an orthostatic blood pressure decrease of at least 40 mm Hg systolic and/or at least 20 mm Hg diastolic.
- In Phase 1 trials of REQUIP with healthy volunteers who received single doses on morethan one occasion without titration, 7% had documented symptomatic orthostatic hypotension. These episodes appeared mainly at doses above 0.8 mg and these doses are higher than the starting doses recommended for patients with either Parkinson’s disease or with RLS. In most of these individuals, the hypotension was accompanied by bradycardia but did not develop into syncope.
- Although dizziness is not a specific manifestation of hypotension or orthostatic hypotension, patients with hypotension or orthostatic hypotension frequently reported dizziness. In controlled clinical trials, dizziness was a common adverse reaction in patients receiving REQUIP and was more frequent in patients with Parkinson’s disease or with RLS receiving REQUIP than in patients receiving placebo (early Parkinson’s disease without L-dopa: REQUIP 40%, placebo 22%; advanced Parkinson’s disease: REQUIP 26%, placebo 16%; RLS: REQUIP 11%, placebo 5%). Dizziness of sufficient severity to cause trial discontinuation of REQUIP was 4% in patients with early Parkinson’s disease without L-dopa, 3% in patients with advanced Parkinson’s disease, and 1% in patients with RLS.
- Hallucinations/Psychotic-like Behavior
- In double-blind, placebo-controlled, early-therapy trials in patients with Parkinson’s disease who were not treated with L-dopa, 5.2% (8 of 157) of patients treated with REQUIP reported hallucinations, compared with 1.4% of patients on placebo (2 of 147). Among those patients receiving both REQUIP and L-dopa in advanced Parkinson’s disease studies, 10.1% (21 of 208) were reported to experience hallucinations, compared with 4.2% (5 of 120) of patients treated with placebo and L-dopa.
- The incidence of hallucination was increased in elderly patients (i.e., older than 65 years) treated with extended-release REQUIP.
- Postmarketing reports indicate that patients may experience new or worsening mental status and behavioral changes, which may be severe, including psychotic-like behavior during treatment with REQUIP or after starting or increasing the dose of REQUIP. Other drugs prescribed to improve the symptoms of Parkinson’s disease can have similar effects on thinking and behavior. This abnormal thinking and behavior can consist of one or more of a variety of manifestations including paranoid ideation, delusions, hallucinations, confusion, psychotic-like behavior, disorientation, aggressive behavior, agitation, and delirium.
- Patients with a major psychotic disorder should ordinarily not be treated with REQUIP because of the risk of exacerbating the psychosis. In addition, certain medications used to treat psychosis may exacerbate the symptoms of Parkinson’s disease and may decrease the effectiveness of REQUIP.
- Dyskinesia
- REQUIP may potentiate the dopaminergic side effects of L-dopa and may cause and/or exacerbate pre-existing dyskinesia in patients treated with L-dopa for Parkinson’s disease. In double-blind, placebo-controlled trials in advanced Parkinson’s disease, dyskinesia was much more common in patients treated with REQUIP than in those treated with placebo. Among those patients receiving both REQUIP and L-dopa in advanced Parkinson’s disease trials, 34% were reported to experience dyskinesia, compared with 13% of patients treated with placebo. Decreasing the dose of the dopaminergic drug may ameliorate this adverse reaction.
- Impulse Control/Compulsive Behaviors
- Case reports suggest that patients can experience intense urges to gamble, increased sexual urges, intense urges to spendmoney, binge or compulsive eating, and/or other intense urges, and the inability to control these urges while taking one or more of the medications, including REQUIP, that increase central dopaminergic tone and that are generally used for the treatment of Parkinson’s disease and RLS. In some cases, although not all, these urges were reported to have stopped when the dose was reduced or the medication was discontinued. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to specifically ask patients or their caregivers about the development of new or increased gambling urges, sexual urges, uncontrolled spending, binge or compulsive eating, or other urges while being treated with REQUIP. Physiciansshould consider dose reduction or stopping the medication if a patient develops such urges while taking REQUIP.
- Withdrawal-emergent Hyperpyrexia and Confusion
- A symptom complex resembling the neuroleptic malignant syndrome (characterized by elevated temperature, muscular rigidity, altered consciousness, and autonomic instability), with no other obvious etiology, has been reported in association with rapid dose reduction, withdrawal of, or changes in dopaminergic therapy. Therefore, it is recommended that the dose be tapered at the end of treatment with REQUIP for Parkinson’s disease as a prophylactic measure.
- Melanoma
- Epidemiological studies have shown that patients with Parkinson’s disease have a higher risk (2- to approximately 6-fold higher) of developing melanoma than the general population. Whether the increased risk observed was due to Parkinson’s disease or other factors, such as drugs used to treat Parkinson’s disease, is unclear.
- For the reasons stated above, patients and providers are advised to monitor for melanomas frequently and on a regular basis when using REQUIP for any indication. Ideally, periodic skin examinations should be performed by appropriately qualified individuals (e.g., dermatologists).
- Augmentation and Early-morning Rebound in Restless Legs Syndrome
- Reports in the literature indicate treatment of RLS with dopaminergic medications can result in recurrence of symptoms in the early morning hours, referred to as rebound. Augmentation has also been described during therapy for RLS. Augmentation refers to the earlier onset of symptoms in the evening (or even the afternoon), increase in symptoms, and spread of symptoms to involve other extremities. Rebound refers to new onset of symptoms in the early morning hours. Augmentation and/or early-morning rebound have been observed in a postmarketing trial. If augmentation or early-morning rebound occurs, the use of REQUIP should be reviewed and dosage adjustment or discontinuation of treatment should be considered.
- Fibrotic Complications
- Cases of retroperitoneal fibrosis, pulmonary infiltrates, pleural effusion, pleural thickening, pericarditis, and cardiac valvulopathy have been reported in some patients treated with ergot-derived dopaminergic agents. While these complications may resolve when the drug is discontinued, complete resolution does not always occur.
- Although these adverse reactions are believed to be related to the ergoline structure of these compounds, whether other, non-ergot‑derived dopamine agonists such as ropinirole can cause them is unknown.
- Cases of possible fibrotic complications, including pleural effusion, pleural fibrosis, interstitial lung disease, and cardiac valvulopathy have been reported in the development program and postmarketing experience for ropinirole. While the evidence is not sufficient to establish a causal relationship between ropinirole and these fibrotic complications, a contribution of ropinirole cannot be excluded.
- Retinal Pathology
- Retinal degeneration was observed in albino rats in the 2-year carcinogenicity study at all doses tested (equivalent to 0.6 to 20 times the maximum recommended human dose [MRHD] for Parkinson’s disease [24 mg/day] on a mg/m2 basis), but was statistically significant at the highest dose (50 mg/kg/day). Retinal degeneration was not observed in a 3-month study in pigmented rats, in a 2-year carcinogenicity study in albino mice, or in 1‑year studies in monkeys or albino rats. The significance of this effect for humans has not been established but involves disruption of a mechanism that is universally present in vertebrates (e.g., disk shedding).
- Ocular electroretinogram (ERG) assessments were conducted during a 2-year, double-blind, multicenter, flexible dose, L-dopa-controlled clinical trial of ropinirole in patients with Parkinson’s disease; 156 patients (78 on ropinirole, mean dose: 11.9 mg/day, and 78 on L-dopa, mean dose: 555.2 mg/day) were evaluated for evidence of retinal dysfunction through electroretinograms. There was no clinically meaningful difference between the treatment groups in retinal function over the duration of the trial.
- Binding to Melanin
- Ropinirole binds to melanin-containing tissues (i.e., eyes, skin) in pigmented rats. After a single dose, long-term retention of drug was demonstrated, with a half-life in the eye of 20 days
Adverse Reactions
Clinical Trials Experience
- Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug (or of another development program of a different formulation of the same drug) and may not reflect the rates observed in practice.
- Parkinson’s Disease
- During the premarketing development of REQUIP, patients received REQUIP either without L-dopa (early Parkinson’s disease trials) or as concomitant therapy with L-dopa (advanced Parkinson’s disease trials). Because these two populations may have differential risks for various adverse reactions, this section will in general present adverse reaction data for these two populations separately.
- Early Parkinson’s Disease (without L-dopa)
- In the double-blind, placebo-controlled trials in patients with early-stage Parkinson’s disease, the most commonly observed adverse reactions in patients treated with REQUIP (incidence at least 5% greater than placebo) were nausea, somnolence, dizziness, syncope, asthenic condition (i.e., asthenia, fatigue, and/or malaise), viral infection, leg edema, vomiting, and dyspepsia.
- Approximately 24% of patients treated with REQUIP who participated in the double-blind, placebo-controlled early Parkinson’s disease (without L-dopa) trials discontinued treatment due to adverse reactions compared with 13% of patients who received placebo. The most common adverse reactions in patients treated with REQUIP (incidence at least 2% greater than placebo) of sufficient severity to cause discontinuation were nausea and dizziness.
- Table 3 lists treatment-emergent adverse reactions that occurred in at least 2% of patients with early Parkinson’s disease (without L-dopa) treated with REQUIP participating in the double-blind, placebo-controlled trials and were numerically more common than the incidence for placebo-treated patients. In these trials, either REQUIP or placebo was used as early therapy (i.e., without L-dopa).
- aPatients may have reported multiple adverse reactions during the trial or at discontinuation; thus, patients may be included in more than one category.
- b Asthenic condition (i.e., asthenia, fatigue, and/or malaise).
- Advanced Parkinson’s Disease (with L-dopa)
- In the double-blind, placebo-controlled trials in patients with advanced-stage Parkinson’s disease, the most commonly observed adverse reactions in patients treated with REQUIP (incidence at least 5 % greater than placebo) were dyskinesia, somnolence, nausea, dizziness, confusion, hallucinations, increased sweating, and headache.
- Approximately 24% of patients who received REQUIP in the double-blind, placebo-controlled advanced Parkinson’s disease (with L-dopa) trials discontinued treatment due to adverse reactions compared with 18% of patients who received placebo. The most common adverse reaction in patients treated with REQUIP (incidence at least 2% greater than placebo) of sufficient severity to cause discontinuation was dizziness.
- Table 4 lists treatment-emergent adverse reactions that occurred in at least 2% of patients with advanced Parkinson’s disease (with L-dopa) treated with REQUIP who participated in the double-blind, placebo-controlled trials and were numerically more common than the incidence for placebo-treated patients. In these trials, either REQUIP or placebo was used as an adjunct to L-dopa.
- aPatients may have reported multiple adverse reactions during the trial or at discontinuation; thus, patients may be included in more than one category.
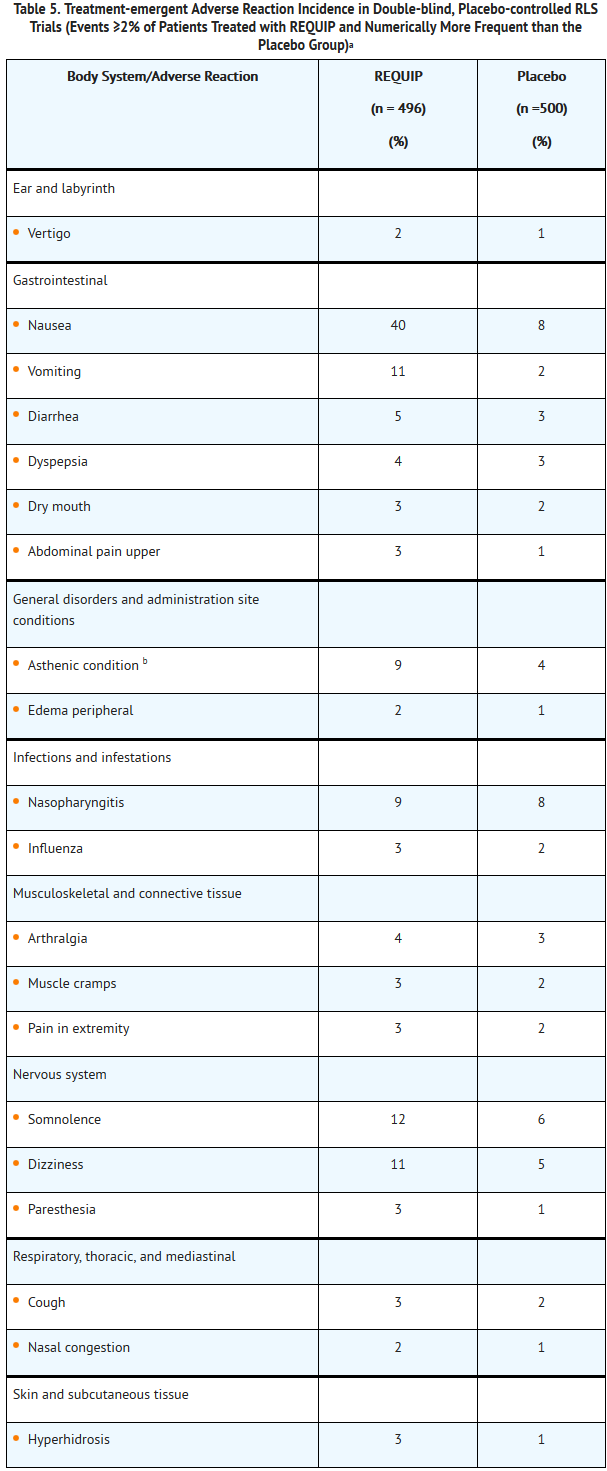
- Restless Legs Syndrome
- In the double-blind, placebo-controlledtrials in patients with RLS, the most commonly observed adverse reactions in patients treated with REQUIP (incidence at least 5% greater than placebo) were nausea, vomiting, somnolence, dizziness, and asthenic condition (i.e., asthenia, fatigue, and/or malaise).
- Approximately 5% of patients treated with REQUIP who participated in the double-blind, placebo-controlled trials in the treatment of RLS discontinued treatment due to adverse reactions compared with 4% of patients who received placebo. The most common adverse reaction in patients treated with REQUIP (incidence at least 2% greater than placebo) of sufficient severity to cause discontinuation was nausea.
- Table 5 lists treatment-emergent adverse reactions that occurred in at least 2% of patients with RLS treated with REQUIP participating in the 12-week, double-blind, placebo-controlled trials and were numerically more common than the incidence for placebo-treated patients.
- aPatients may have reported multiple adverse reactions during the trial or at discontinuation; thus, patients may be included in more than one category.
- b Asthenic condition (i.e., asthenia, fatigue, and/or malaise).
Postmarketing Experience
There is limited information regarding Postmarketing Experience of Ropinirole in the drug label.
Drug Interactions
- CYP1A2 Inhibitors and Inducers
- In vitro metabolism studies showed that CYP1A2 is the major enzyme responsible for the metabolism of ropinirole. There is thus the potential for inducers or inhibitors of this enzyme to alter the clearance of ropinirole. Therefore, if therapy with a drug known to be a potent inducer or inhibitor of CYP1A2 is stopped or started during treatment with REQUIP, adjustment of the dose of REQUIP may be required. Coadministration of ciprofloxacin, an inhibitor of CYP1A2, increases the AUC and Cmax of ropinirole. Cigarette smoking is expected to increase the clearance of ropinirole since CYP1A2 is known to be induced by smoking.
- Estrogens
- Population pharmacokinetic analysis revealed that higher doses of estrogens (usually associated with hormone replacement therapy [HRT]) reduced the clearance of ropinirole. Starting or stopping HRT may require adjustment of dosage of REQUIP.
- Dopamine Antagonists
- Because ropinirole is a dopamine agonist, it is possible that dopamine antagonists such as neuroleptics (e.g., phenothiazines, butyrophenones, thioxanthenes) or metoclopramide may reduce the efficacy of REQUIP.
Use in Specific Populations
Pregnancy
- Pregnancy Category C
- There are no adequate and well-controlled studies in pregnant women. In animal reproduction studies, ropinirole has been shown to have adverse effects on embryo-fetal development, including teratogenic effects. REQUIP should be used during pregnancy only if the potential benefit outweighs the potential risk to the fetus.
- Oral treatment of pregnant rats with ropinirole during organogenesis resulted in decreased fetal body weight, increased fetal death, and digital malformations at 24, 36, and 60 times, respectively, the maximum recommended human dose (MRHD) for Parkinson’s disease (24 mg/day) on a mg/m2 basis. The combined oral administration of ropinirole at 8 times the MRHD and a clinically relevant dose of L‑dopa to pregnant rabbits during organogenesis produced a greater incidence and severity of fetal malformations (primarily digit defects) than were seen in the offspring of rabbits treated with L-dopa alone. No effect on fetal development was observed in rabbits when ropinirole was administered alone at an oral dose 16 times the MRHD on a mg/m2 basis. In a perinatal-postnatal study in rats, impaired growth and development of nursing offspring and altered neurological development of female offspring were observed when dams were treated with 4 times the MRHD on a mg/m2 basis.
- Australian Drug Evaluation Committee (ADEC) Pregnancy Category
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Ropinirole in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Ropinirole during labor and delivery.
Nursing Mothers
- Ropinirole inhibits prolactin secretion in humans and could potentially inhibit lactation. Ropinirole has been detected in rat milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when REQUIP is administered to a nursing woman.
Pediatric Use
- Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
- Dose adjustment is not necessary in elderly (65 years and older) patients, as the dose of REQUIP is individually titrated to clinical therapeutic response and tolerability. Pharmacokinetic trials conducted in patients demonstrated that oral clearance of ropinirole is reduced by 15% in patients older than 65 years compared with younger patients.
- In clinical trials of extended-release ropinirole for Parkinson’s disease, 387 patients were 65 years and older and 107 patients were 75 years and older. Among patients receiving extended-release ropinirole, hallucination was more common in elderly patients (10%) compared with non-elderly patients (2%). The incidence of overall adverse reactions increased with increasing age for both patients receiving extended-release ropinirole and placebo.
Gender
There is no FDA guidance on the use of Ropinirole with respect to specific gender populations.
Race
There is no FDA guidance on the use of Ropinirole with respect to specific racial populations.
Renal Impairment
- No dose adjustment is necessary in patients with moderate renal impairment (creatinine clearance of 30 to 50 mL/min). For patients with end-stage renal disease on hemodialysis, a reduced maximum dose is recommended.
- The use of REQUIP in patients with severe renal impairment (creatinine clearance less than 30 mL/min) without regular dialysis has not been studied.
Hepatic Impairment
- The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Ropinirole in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Ropinirole in patients who are immunocompromised.
Administration and Monitoring
Administration
- Oral
Monitoring
There is limited information regarding Monitoring of Ropinirole in the drug label.
IV Compatibility
There is limited information regarding IV Compatibility of Ropinirole in the drug label.
Overdosage
Acute Overdose
Signs and Symptoms
- The symptoms of overdose with REQUIP are generally related to its dopaminergic activity.
- In the Parkinson’s disease program, there have been patients who accidentally or intentionally took more than their prescribed dose of ropinirole. The largest overdose reported with ropinirole in clinical trials was 435 mg taken over a 7-day period (62.1 mg/day). Of patients who received a dose greater than 24 mg/day, reported symptoms included adverse events commonly reported during dopaminergic therapy (nausea, dizziness), as well as visual hallucinations, hyperhidrosis, claustrophobia, chorea, palpitations, asthenia, and nightmares. Additional symptoms reported for doses of 24 mg or less or for overdoses of unknown amount included vomiting, increased coughing, fatigue, syncope, vasovagal syncope, dyskinesia, agitation, chest pain, orthostatic hypotension, somnolence, and confusional state.
Management
- General supportive measures are recommended. Vital signs should be maintained, if necessary.
Chronic Overdose
There is limited information regarding Chronic Overdose of Ropinirole in the drug label.
Pharmacology

| |
Ropinirole
| |
| Systematic (IUPAC) name | |
| 4-[2-(dipropylamino)ethyl]-1,3-dihydro-2H-indol-2-one | |
| Identifiers | |
| CAS number | |
| ATC code | N04 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 260.375 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | 50%[1] |
| Metabolism | Hepatic (CYP1A2)[1] |
| Half life | 5-6 hours[1] |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
C |
| Legal status |
Template:Unicode Prescription only |
| Routes | Oral |
Mechanism of Action
- Ropinirole is a non-ergoline dopamine agonist. The precise mechanism of action of ropinirole as a treatment for Parkinson’s disease is unknown, although it is thought to be related to its ability to stimulate dopamine D2 receptors within the caudate-putamen in the brain. The precise mechanism of action of ropinirole as a treatment for Restless Legs Syndrome is unknown, although it is thought to be related to its ability to stimulate dopamine receptors.
Structure
- REQUIP contains ropinirole, a non-ergoline dopamine agonist, as the hydrochloride salt. The chemical name of ropinirole hydrochloride is 4-[2-(dipropylamino)ethyl]-1,3-dihydro-2H-indol-2-one and the empirical formula is C16H24N2O•HCl. The molecular weight is 296.84 (260.38 as the free base).
- Ropinirole hydrochloride is a white to yellow solid with a melting range of 243° to 250°C and a solubility of 133 mg/mL in water.
- Each pentagonal film-coated TILTAB® tablet with beveled edges contains 0.29 mg, 0.57 mg, 1.14 mg, 2.28 mg, 3.42 mg, 4.56 mg , or 5.70 mg ropinirole hydrochloride equivalent to ropinirole, 0.25 mg, 0.5 mg, 1 mg, 2 mg, 3 mg, 4 mg, or 5 mg. Inactive ingredients consist of croscarmellose sodium, hydrous lactose, magnesium stearate, microcrystalline cellulose, and one or more of the following: carmine, FD&C Blue No. 2 aluminum lake, FD&C Yellow No. 6 aluminum lake, hypromellose, iron oxides, polyethylene glycol, polysorbate 80, titanium dioxide.
Pharmacodynamics
- Clinical experience with dopamine agonists, including ropinirole, suggests an association with impaired ability to regulate blood pressure with resulting orthostatic hypotension, especially during dose escalation. In some patients in clinical trials, blood pressure changes were associated with the emergence of orthostatic symptoms, bradycardia, and, in one case in a healthy volunteer, transient sinus arrest with syncope.
- The mechanism of orthostatic hypotension induced by ropinirole is presumed to be due to a D2-mediated blunting of the noradrenergic response to standing and subsequent decrease in peripheral vascular resistance. Nausea is a common concomitant symptom of orthostatic signs and symptoms.
- At oral doses as low as 0.2 mg, ropinirole suppressed serum prolactin concentrations in healthy male volunteers.
- Ropinirole had no dose-related effect on ECG wave form and rhythm in young, healthy, male volunteers in the range of 0.01 to 2.5 mg.
- Ropinirole had no dose- or exposure-related effect on mean QT intervals in healthy male and female volunteers titrated to doses up to 4 mg/day. The effect of ropinirole on QTc intervals at higher exposures achieved either due to drug interactions, hepatic impairment, or at higher doses has not been systematically evaluated.
Pharmacokinetics
- Ropinirole displayed linear kinetics over the dosing range of 1 to 8 mg three times daily. Steady-state concentrations are expected to be achieved within 2 days of dosing. Accumulation upon multiple dosing is predictive from single dosing.
- Absorption
- Ropinirole is rapidly absorbed after oral administration, reaching peak concentration in approximately 1 to 2 hours. In clinical trials, more than 88% of a radiolabeled dose was recovered in urine and the absolute bioavailability was 45% to 55%, indicating approximately 50% first-pass effect.
- Relative bioavailability from a tablet compared with an oral solution is 85%. Food does not affect the extent of absorption of ropinirole, although its Tmax is increased by 2.5 hours and its Cmax is decreased by approximately 25% when the drug is taken with a high-fat meal.
- Distribution
- Ropinirole is widely distributed throughout the body, with an apparent volume of distribution of 7.5 L/kg. It is up to 40% bound to plasma proteins and has a blood-to-plasma ratio of 1:1.
- Metabolism
- Ropinirole is extensively metabolized by the liver. The major metabolic pathways are N-despropylation and hydroxylation to form the inactive N-despropyl metabolite and hydroxy metabolites. The N-despropyl metabolite is converted to carbamyl glucuronide, carboxylic acid, and N-despropyl hydroxy metabolites. The hydroxy metabolite of ropinirole is rapidly glucuronidated.
- In vitro studies indicate that the major cytochrome P450 enzyme involved in the metabolism of ropinirole is CYP1A2, an enzyme known to be induced by smoking and omeprazole and inhibited by, for example, fluvoxamine, mexiletine, and the older fluoroquinolones such as ciprofloxacin and norfloxacin.
- Elimination
- The clearance of ropinirole after oral administration is 47 L/h and its elimination half-life is approximately 6 hours. Less than 10% of the administered dose is excreted as unchanged drug in urine. N-despropyl ropinirole is the predominant metabolite found in urine (40%), followed by the carboxylic acid metabolite (10%), and the glucuronide of the hydroxy metabolite (10%).
- Drug Interactions
- Digoxin: Coadministration of REQUIP (2 mg three times daily) with digoxin (0.125 to 0.25 mg once daily) did not alter the steady-state pharmacokinetics of digoxin in 10 patients.
- Theophylline: Administration of theophylline (300 mg twice daily, a substrate of CYP1A2) did not alter the steady-state pharmacokinetics of ropinirole (2 mg three times daily) in 12 patients with Parkinson’s disease. REQUIP (2 mg three times daily) did not alter the pharmacokinetics of theophylline (5 mg/kg IV) in 12 patients with Parkinson’s disease.
- Ciprofloxacin: Coadministration of ciprofloxacin (500 mg twice daily), an inhibitor of CYP1A2, with REQUIP (2 mg three times daily) increased ropinirole AUC by 84% on average and Cmax by 60% (n = 12 patients).
- Estrogens: Population pharmacokinetic analysis revealed that estrogens (mainly ethinylestradiol: intake 0.6 to 3 mg over 4-month to 23-year period) reduced the oral clearance of ropinirole by 36% in 16 patients.
- L-dopa: Coadministration of carbidopa + L-dopa (10/100 mg twice daily) with REQUIP (2 mg three times daily) had no effect on the steady-state pharmacokinetics of ropinirole (n = 28 patients). Oral administration of REQUIP 2 mg three times daily increased mean steady-state Cmax of L-dopa by 20%, but its AUC was unaffected (n = 23 patients).
- Commonly Administered Drugs: Population analysis showed that commonly administered drugs, e.g., selegiline, amantadine, tricyclic antidepressants, benzodiazepines, ibuprofen, thiazides, antihistamines, and anticholinergics, did not affect the clearance of ropinirole. An in vitro study indicates that ropinirole is not a substrate for P-gp. Ropinirole and its circulating metabolites do not inhibit or induce P450 enzymes; therefore, ropinirole is unlikely to affect the pharmacokinetics of other drugs by a P450 mechanism.
- Specific Populations
- Because therapy with REQUIP is initiated at a low dose and gradually titrated upward according to clinical tolerability to obtain the optimum therapeutic effect, adjustment of the initial dose based on gender, weight, or age is not necessary.
- Age
- Oral clearance of ropinirole is reduced by 15% in patients older than 65 years compared with younger patients. Dosage adjustment is not necessary in the elderly (older than 65 years), as the dose of ropinirole is to be individually titrated to clinical response.
- Gender
- Female and male patients showed similar clearance.
- Race
- The influence of race on the pharmacokinetics of ropinirole has not been evaluated.
- Cigarette Smoking
- Smoking is expected to increase the clearance of ropinirole since CYP1A2 is known to be induced by smoking. In a trial in patients with RLS, smokers (n = 7) had an approximately 30% lower Cmax and a 38% lower AUC than did nonsmokers (n = 11) when those parameters were normalized for dose.
- Renal Impairment
- Based on population pharmacokinetic analysis, no difference was observed in the pharmacokinetics of ropinirole in subjects with moderate renal impairment (creatinine clearance between 30 to 50 mL/min) compared with an age-matched population with creatinine clearance above 50 mL/min. Therefore, no dosage adjustment is necessary in patients with moderate renal impairment.
- A trial of ropinirole in subjects with end-stage renal disease on hemodialysis has shown that clearance of ropinirole was reduced by approximately 30%. The recommended maximum dose should be lower in these patients.
- The use of ropinirole in subjects with severe renal impairment (creatinine clearance less than 30 mL/min) without regular dialysis has not been studied.
- Hepatic Impairment
- The pharmacokinetics of ropinirole have not been studied in patients with hepatic impairment. Because ropinirole is extensively metabolized by the liver, these patients may have higher plasma levels and lower clearance of ropinirole than patients with normal hepatic function.
- Other Diseases
- Population pharmacokinetic analysis revealed no change in the clearance of ropinirole in patients with concomitant diseases such as hypertension, depression, osteoporosis/arthritis, and insomnia compared with patients with Parkinson’s disease only.
Nonclinical Toxicology
- Carcinogenesis
- Two-year carcinogenicity studies of ropinirole were conducted in mice at oral doses of 5, 15, and 50 mg/kg/day and in rats at oral doses of 1.5, 15, and 50 mg/kg/day.
- In rats, there was an increase in testicular Leydig cell adenomas at all doses tested. The lowest dose tested (1.5 mg/kg/day) is less than the MRHD for Parkinson’s disease (24 mg/day) on a mg/m2 basis. The endocrine mechanisms believed to be involved in the production of these tumors in rats are not considered relevant to humans.
- In mice, there was an increase in benign uterine endometrial polyps at a dose of 50 mg/kg/day. The highest dose not associated with this finding (15 mg/kg/day) is three times the MRHD on a mg/m2 basis.
- Mutagenesis
- Ropinirole was not mutagenic or clastogenic in in vitro (Ames, chromosomal aberration in human lymphocytes, mouse lymphoma tk) assays or in the in vivo mouse micronucleus test.
- Impairment of Fertility
- When administered to female rats prior to and during mating and throughout pregnancy, ropinirole caused disruption of implantation at oral doses of 20 mg/kg/day (8 times the MRHD on a mg/m2 basis) or greater. This effect in rats is thought to be due to the prolactin-lowering effect of ropinirole. In rat studies using a low oral dose (5 mg/kg) during the prolactin-dependent phase of early pregnancy (gestation days 0 to 8), ropinirole did not affect female fertility at oral doses up to 100 mg/kg/day (40 times the MRHD on a mg/m2 basis). No effect on male fertility was observed in rats at oral doses up to 125 mg/kg/day (50 times the MRHD on a mg/m2 basis).
Clinical Studies
- Parkinson’s Disease
- The effectiveness of REQUIP in the treatment of Parkinson’s disease was evaluated in a multinational drug development program consisting of 11 randomized, controlled trials. Four trials were conducted in patients with early Parkinson’s disease and no concomitant levodopa (L-dopa) and seven trials were conducted in patients with advanced Parkinson’s disease with concomitant L-dopa.
- Three placebo‑controlled trials provide evidence of effectiveness of REQUIP in the management of patients with Parkinson’s disease who were and were not receiving concomitant L-dopa. Two of these three trials enrolled patients with early Parkinson’s disease (without L-dopa) and one enrolled patients receiving L-dopa.
- In these trials a variety of measures were used to assess the effects of treatment (e.g., the Unified Parkinson’s Disease Rating Scale [UPDRS], Clinical Global Impression [CGI] scores, patient diaries recording time “on” and “off,” tolerability of L-dopa dose reductions).
- In both trials of patients with early Parkinson’s disease (without L-dopa), the motor component (Part III) of the UPDRS was the primary outcome assessment. The UPDRS is a multi-item rating scale intended to evaluate mentation (Part I), activities of daily living (Part II), motor performance (Part III), and complications of therapy (Part IV). Part III of the UPDRS contains 14 items designed to assess the severity of the cardinal motor findings in patients with Parkinson’s disease (e.g., tremor, rigidity, bradykinesia, postural instability) scored for different body regions and has a maximum (worst) score of 108. In the trial of patients with advanced Parkinson’s disease (with L-dopa), both reduction in percent awake time spent “off” and the ability to reduce the daily use of L-dopa were assessed as a combined endpoint and individually.
- Trials in Patients with Early Parkinson’s Disease (without L-dopa)
- Trial 1 was a 12-week multicenter trial in which 63 patients with idiopathic Parkinson’s disease receiving concomitant anti-Parkinson medication (but not L-dopa) were enrolled and 41 were randomized to REQUIP and 22 to placebo. Patients had a mean disease duration of approximately 2 years. Patients were eligible for enrollment if they presented with bradykinesia and at least tremor, rigidity, or postural instability. In addition, they must have been classified as Hoehn & Yahr Stage I-IV. This scale, ranging from I = unilateral involvement with minimal impairment to V = confined to wheelchair or bed, is a standard instrument used for staging patients with Parkinson’s disease. The primary outcome measure in this trial was the proportion of patients experiencing a decrease (compared with baseline) of at least 30% in the UPDRS motor score.
- Patients were titrated for up to 10 weeks, starting at 0.5 mg twice daily, with weekly increments of 0.5 mg twice daily to a maximum of 5 mg twice daily. Once patients reached their maximally tolerated dose (or 5 mg twice daily), they were maintained on that dose through 12 weeks. The mean dose achieved by patients at trial endpoint was 7.4 mg/day. Mean baseline UPDRS motor score was 18.6 for patients treated with REQUIP and 19.9 for patients treated with placebo. At the end of 12 weeks, the percentage of responders was greater on REQUIP than on placebo and the difference was statistically significant (Table 6).
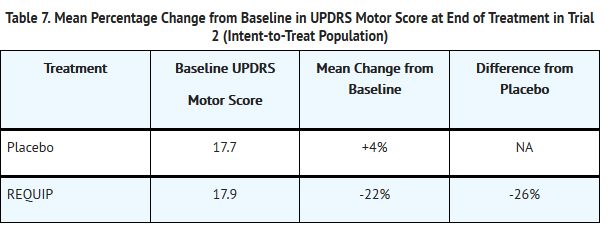
- Trial 2 in patients with early Parkinson’s disease (without L-dopa) was a double‑blind, randomized, placebo-controlled, 6-month trial. In this trial, 241 patients were enrolled and 116 were randomized to REQUIP and 125 to placebo. Patients were essentially similar to those in the trial described above; concomitant use of selegiline was allowed, but patients were not permitted to use anticholinergics or amantadine during the trial. Patients had a mean disease duration of 2 years and limited (not more than a 6-week period) or no prior exposure to L-dopa. The starting dosage of REQUIP in this trial was 0.25 mg three times daily. The dosage was titrated at weekly intervals by increments of 0.25 mg three times daily to a dosage of 1 mg three times daily. Further titrations at weekly intervals were at increments of 0.5 mg three times daily up to a dosage of 3 mg three times daily, and then weekly at increments of 1 mg three times daily. Patients were to be titrated to a dosage of at least 1.5 mg three times daily and then to their maximally tolerated dosage, up to a maximum of 8 mg three times daily. The mean dose attained in patients at trial endpoint was 15.7 mg/day.
- The primary measure of effectiveness was the mean percent reduction (improvement) from baseline in the UPDRS motor score. At the end of the 6-month trial, patients treated with REQUIP showed improvement in motor score compared with placebo and the difference was statistically significant (Table 7).
- Trial in Patients with Advanced Parkinson’s Disease (with L-dopa)
- Trial 3 was a double-blind, randomized, placebo-controlled, 6-month trial that randomized 149 patients (Hoehn & Yahr II‑IV) who were not adequately controlled on L-dopa. Ninety-five patients were randomized to REQUIP and 54 were randomized to placebo. Patients in this trial had a mean disease duration of approximately 9 years, had been exposed to L-dopa for approximately 7 years, and had experienced “on-off” periods with L-dopa therapy. Patients previously receiving stable doses of selegiline, amantadine, and/or anticholinergic agents could continue on these agents during the trial. Patients were started at a dosage of 0.25 mg three times daily of REQUIP and titrated upward by weekly intervals until an optimal therapeutic response was achieved. The maximum dosage of trial medication was 8 mg three times daily. All patients had to be titrated to at least a dosage of 2.5 mg three times daily. Patients could then be maintained on this dosage level or higher for the remainder of the trial. Once a dosage of 2.5 mg three times daily was achieved, patients underwent a mandatory reduction in their L-dopa dosage, to be followed by additional mandatory reductions with continued escalation of the dosage of REQUIP. Reductions in the dosage of l-dopa were also allowed if patients experienced adverse reactions that the investigator considered related to dopaminergic therapy. The mean dose attained at trial endpoint was 16.3 mg/day. The primary outcome was the proportion of responders, defined as patients who were able both to achieve a decrease (compared with baseline) of at least 20% in their L-dopa dosage and a decrease of at least 20% in the proportion of the time awake in the “off” condition (a period of time during the day when patients are particularly immobile), as determined by subject diary. In addition, the mean change in “off” time from baseline and the percent change from baseline in daily L-dopa dosage were examined.
- At the end of 6 months, the percentage of responders was greater on REQUIP than on placebo and the difference was statistically significant (Table 8).
- Based on the protocol-mandated reductions in L-dopa dosage with escalating doses of REQUIP, patients treated with REQUIP had a 19.4% mean reduction in L-dopa dosage while patients treated with placebo had a 3% reduction. Mean daily L-dopa dosage at baseline was 759 mg for patients treated with REQUIP and 843 mg for patients treated with placebo.
- The mean number of daily “off” hours at baseline was 6.4 hours for patients treated with REQUIP and 7.3 hours for patients treated with placebo. At the end of the 6-month trial, there was a mean reduction of 1.5 hours of “off” time in patients treated with REQUIP and a mean reduction of 0.9 hours of “off” time in patients treated with placebo, resulting in a treatment difference of 0.6 hours of “off” time.
- Restless Legs Syndrome
- The effectiveness of REQUIP in the treatment of RLS was demonstrated in randomized, double-blind, placebo-controlled trials in adults diagnosed with RLS using the International Restless Legs Syndrome Study Group diagnostic criteria. Patients were required to have a history of a minimum of 15 RLS episodes/month during the previous month and a total score of ≥15 on the International RLS Rating Scale (IRLS scale) at baseline. Patients with RLS secondary to other conditions (e.g., pregnancy, renal failure, anemia) were excluded. All trials employed flexible dosing, with patients initiating therapy at 0.25 mg REQUIP once daily. Patients were titrated based on clinical response and tolerability over 7 weeks to a maximum of 4 mg once daily. All doses were taken between 1 and 3 hours before bedtime.
- A variety of measures were used to assess the effects of treatment, including the IRLS scale and Clinical Global Impression-Global Improvement (CGI-I) scores. The IRLS scale contains 10 items designed to assess the severity of sensory and motor symptoms, sleep disturbance, daytime somnolence, and impact on activities of daily living and mood associated with RLS. The range of scores is 0 to 40, with 0 being absence of RLS symptoms and 40 the most severe symptoms. Three of the controlled trials utilized the change from baseline in the IRLS scale at the Week 12 endpoint as the primary efficacy outcome.
- Three hundred eighty patients were randomized to receive REQUIP (n = 187) or placebo (n = 193) in a US trial (RLS-1); 284 were randomized to receive either REQUIP (n = 146) or placebo (n = 138) in a multinational trial (excluding US) (RLS-2); and 267 patients were randomized to REQUIP (n = 131) or placebo (n = 136) in a multinational trial (including US) (RLS-3). Across the three trials, the mean duration of RLS was 16 to 22 years (range: 0 to 65 years), mean age was approximately 54 years (range: 18 to 79 years), and approximately 61% were women. The mean dose at Week 12 was approximately 2 mg/day for the three trials.
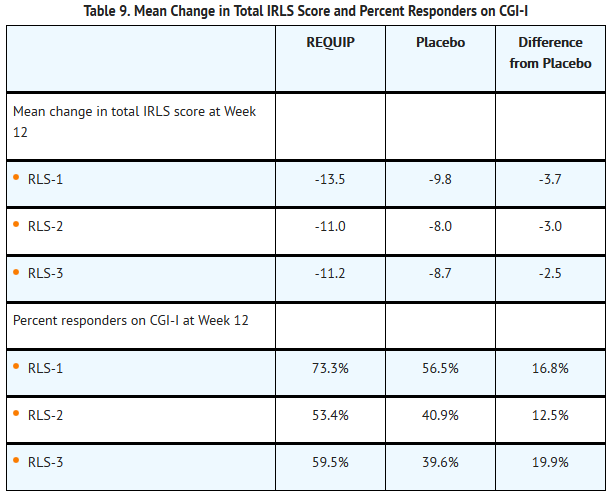
- At baseline, mean total IRLS score was 22.0 for REQUIP and 21.6 for placebo in RLS-1, was 24.4 for REQUIP and 25.2 for placebo in RLS-2, and was 23.6 for REQUIP and 24.8 for placebo in RLS-3. In all three trials, a statistically significant difference between the treatment group receiving REQUIP and the treatment group receiving placebo was observed at Week 12 for both the mean change from baseline in the IRLS scale total score and the percentage of patients rated as responders (much improved or very much improved) on the CGI-I (see Table 9).
- Long-term maintenance of efficacy in the treatment of RLS was demonstrated in a 36‑week trial. Following a 24-week, single-blind treatment phase (flexible dosages of REQUIP of 0.25 to 4 mg once daily), patients who were responders (defined as a decrease of >6 points on the IRLS scale total score relative to baseline) were randomized in double-blind fashion to placebo or continuation of REQUIP for an additional 12 weeks. Relapse was defined as an increase of at least 6 points on the IRLS scale total score to a total score of at least 15, or withdrawal due to lack of efficacy. For patients who were responders at Week 24, the mean dose of REQUIP was 2 mg (range: 0.25 to 4 mg).Patientscontinued on REQUIP demonstrated a significantly lower relapse rate compared with patients randomized to placebo (32.6% versus 57.8%, P = 0.0156).
How Supplied
- Each pentagonal film-coated TILTAB® tablet with beveled edges contains ropinirole hydrochloride equivalent to the labeled amount of ropinirole as follows:
- 0.25 mg: white tablets imprinted with “SB” and “4890” in bottles of 100 (NDC 0007-4890-20)
- 0.5 mg: yellow tablets imprinted with “SB” and “4891” in bottles of 100 (NDC 0007-4891-20)
- 1 mg: green tablets imprinted with “SB” and “4892” in bottles of 100 (NDC 0007-4892-20)
- 2 mg: pale yellowish-pink tablets imprinted with “SB” and “4893” in bottles of 100 (NDC 0007-4893-20)
- 3 mg: pale to moderate reddish-purple tablets, imprinted with “SB” and “4895” in bottles of 100 (NDC 0007-4895-20)
- 4 mg: pale brown tablets imprinted with “SB” and “4896” in bottles of 100 (NDC 0007-4896-20)
- 5 mg: blue tablets imprinted with “SB” and “4894” in bottles of 100 (NDC 0007-4894-20)
- Storage
- Store at controlled room temperature 20° - 25°C (68° - 77°F) [see USP]. Protect from light and moisture. Close container tightly after each use.
Storage
There is limited information regarding Ropinirole Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Ropinirole |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Ropinirole |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
- Advise the patient to read the FDA-approved patient labeling (Patient Information).
- Dosing Instructions
- Instruct patients to take REQUIP only as prescribed. If a dose is missed, advise patients not to double their next dose. REQUIP can be taken with or without food.
- Ropinirole is the active ingredient in both REQUIP XL and REQUIP tablets (the immediate‑release formulation). Ask your patients if they are taking another medication containing ropinirole.
- Hypersensitivity/Allergic Reactions
- Advise patients about the potential for developing a hypersensitivity/allergic reaction including manifestations such as urticaria, angioedema, rash, and pruritus when taking any ropinirole product. Inform patients who experience these or similar reactions to immediately contact their healthcare professional.
- Falling Asleep during Activities of Daily Living and Somnolence
- Alert patients to the potential sedating effects caused by REQUIP, including somnolence and the possibility of falling asleep while engaged in activities of daily living. Because somnolence is a frequent adverse reaction with potentially serious consequences, patients should not drive a car, operate machinery, or engage in other potentially dangerous activities until they have gained sufficient experience with REQUIP to gauge whether or not it affects their mental and/or motor performance adversely. Advise patients that if increased somnolence or episodes of falling asleep during activities of daily living (e.g., conversations, eating, driving a motor vehicle, etc.) are experienced at any time during treatment, they should not drive or participate in potentially dangerous activities until they have contacted their physician.
- Advise patients of possible additive effects when patients are taking other sedating medications, alcohol, or other central nervous system depressants (e.g., benzodiazepines, antipsychotics, antidepressants, etc.) in combination with REQUIP or when taking a concomitant medication (e.g., ciprofloxacin) that increases plasma levels of ropinirole.
- Syncope and Hypotension/Orthostatic Hypotension
- Advise patients that they may experience syncope and may develop hypotension with or without symptoms such as dizziness, nausea, syncope, and sometimes sweating while taking REQUIP, especially if they are elderly. Hypotension and/or orthostatic symptoms may occur more frequently during initial therapy or with an increase in dose at any time (cases have been seen after weeks of treatment).Postural/orthostatic symptoms may be related to sitting up or standing. Accordingly, caution patients against standing rapidly after sitting or lying down, especially if they have been doing so for prolonged periods and especially at the initiation of treatment with REQUIP.
- Hallucinations/Psychotic-like Behavior
- Inform patients that they may experience hallucinations (unreal visions, sounds, or sensations), and that other psychotic-like behavior can occur while taking REQUIP. The elderly are at greater risk than younger patients with Parkinson’s disease. This risk is greater in patients who are taking REQUIP with L-dopa or taking higher doses of REQUIP and may also be further increased in patients taking any other drugs that increase dopaminergic tone. Tell patients to report hallucinations or psychotic-like behavior to their healthcare provider promptly should they develop.
- Inform patients that REQUIP may cause and/or exacerbate pre-existing dyskinesias.
- Impulse Control/Compulsive Behaviors
- Advise patients that they may experience impulse control and/or compulsive behaviors while taking one or more of the medications (including REQUIP) that increase central dopaminergic tone, that are generally used for the treatment of Parkinson’s disease. Advise patients to inform their physician or healthcare provider if they develop new or increased gambling urges, sexual urges, uncontrolled spending, binge or compulsive eating, or other urges while being treated with REQUIP. Physicians should consider dose reduction or stopping the medication if a patient develops such urges while taking REQUIP.
- Withdrawal-emergent Hyperpyrexia and Confusion
- Advise patients to contact their healthcare provider if they wish to discontinue REQUIP or decrease the dose of REQUIP.
- Melanoma
- Advise patients with Parkinson’s disease that they have a higher risk of developing melanoma. Advise patients to have their skin examined on a regular basis by a qualified healthcare provider (e.g., dermatologist) when using REQUIP for any indication.
- Augmentation and Rebound
- Inform patients with RLS that augmentation and/or rebound may occur after starting treatment with REQUIP.
- Nursing Mothers
- Because of the possibility that ropinirole may be excreted in breast milk, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother. Advise patients that REQUIP could inhibit lactation because ropinirole inhibits prolactin secretion.
- Pregnancy
- Because ropinirole has been shown to have adverse effects on embryo-fetal development, including teratogenic effects, in animals, and because experience in humans is limited, advise patients to notify their physician if they become pregnant or intend to become pregnant during therapy.
Precautions with Alcohol
- Alcohol-Ropinirole interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- REQUIP®[2]
Look-Alike Drug Names
- rOPINIRole hydrochloride® — risperiDONE®[3]
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 1.2 Tompson, Debra J.; et al. (2007). "Steady-State Pharmacokinetic Properties of a 24-Hour Prolonged-Release Formulation of Ropinirole: Results of Two Randomized Studies in Patients with Parkinson's Disease". Clinical Pharmacokinetics. 29 (12): 2654–66. doi:10.1016/j.clinthera.2007.12.010. PMID 18201581.
- ↑ "REQUIP ropinirole tablet, film coated".
- ↑ "http://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Ropinirole |Pill Name=No image.jpg |Drug Name= |Pill Ingred=|+sep=; |Pill Imprint= |Pill Dosage= |Pill Color=|+sep=; |Pill Shape= |Pill Size (mm)= |Pill Scoring= |Pill Image= |Drug Author= |NDC=
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole11.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole12.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole13.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole14.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole15.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole16.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole17.png
}}
{{#subobject:
|Label Page=Ropinirole |Label Name=Ropinirole18.png
}}