Panobinostat
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Martin Nino [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
FATAL AND SERIOUS TOXICITIES: SEVERE DIARRHEA AND CARDIAC TOXICITIES
See full prescribing information for complete Boxed Warning.
Severe diarrhea occurred in 25% of Panobinostat treated patients. Monitor for symptoms, institute anti-diarrheal treatment, interrupt Panobinostat and then reduce dose or discontinue Panobinostat. Severe and fatal cardiac ischemic events, severe arrhythmias, and ECG changes have occurred in patients receiving Panobinostat. Arrhythmias may be exacerbated by electrolyte abnormalities. Obtain ECG and electrolytes at baseline and periodically during treatment as clinically indicated. |
Overview
Panobinostat is a histone deacetylase inhibitor that is FDA approved for the treatment of patients with multiple myeloma (in combination with bortezomib and dexamethasone) who have received at least 2 prior regimens, including bortezomib and an immunomodulatory agent. There is a Black Box Warning for this drug as shown here. Common adverse reactions include diarrhea, fatigue, nausea, peripheral edema, decreased appetite, pyrexia, and vomiting (≥20%).
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Panobinostat, a histone deacetylase inhibitor, in combination with bortezomib and dexamethasone, is indicated for the treatment of patients with multiple myeloma who have received at least 2 prior regimens, including bortezomib and an immunomodulatory agent. This indication is approved under accelerated approval based on progression free survival. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.
Dosage
- Recommended Dosing
- The recommended starting dose of Panobinostat is 20 mg, taken orally once every other day for 3 doses per week in Weeks 1 and 2 of each 21-day cycle for up to 8 cycles. Consider continuing treatment for an additional 8 cycles for patients with clinical benefit who do not experience unresolved severe or medically significant toxicity. The total duration of treatment may be up to 16 cycles (48 weeks). Panobinostat is administered in combination with bortezomib and dexamethasone as shown in Table 1 and Table 2.
- The recommended dose of bortezomib is 1.3 mg/m2 given as an injection. The recommended dose of dexamethasone is 20 mg taken orally per scheduled day, on a full stomach.
- Table 1: Recommended Dosing Schedule of Panobinostat in Combination with Bortezomib and Dexamethasone During Cycles 1 to 8
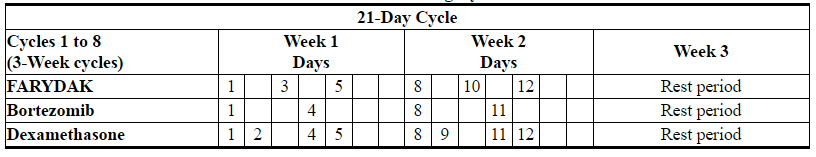
FARYDAK: Panobinostat's Brand name
- Table 2: Recommended Dosing Schedule of Panobinostat in Combination with Bortezomib and Dexamethasone During Cycles 9 to 16

FARYDAK: Panobinostat's Brand name
- Dose Adjustments and Modifications for Toxicity
- Dose and/or schedule modification of Panobinostat may be required based on toxicity. Management of adverse drug reactions may require treatment interruption and/or dose reductions. If dose reduction is required, the dose of Panobinostat should be reduced in increments of 5 mg (i.e., from 20 mg to 15 mg, or from 15 mg to 10 mg). If the dosing of Panobinostat is reduced below 10 mg given 3 times per week, discontinue Panobinostat. Keep the same treatment schedule (3-week treatment cycle) when reducing dose. The table also lists Bortezomib (BTZ) dose modification procedures from the clinical trials.
- Table 3: Dose Modifications for Most Common Toxicities

FARYDAK: Panobinostat's Brand name
- Interrupt or reduce the dose of Panobinostat in patients who have thrombocytopenia, neutropenia or anemia according to instructions in Table 3. For patients with severe thrombocytopenia, consider platelet transfusions. Discontinue Panobinostat treatment if thrombocytopenia does not improve despite the recommended treatment modifications or if repeated platelet transfusions are required.
- In the event of Grade 3 or 4 neutropenia, consider dose reduction and/or the use of growth factors (e.g., G-CSF). Discontinue Panobinostat if neutropenia does not improve despite dose modifications, colony-stimulating factors, or in case of severe infection.
- Gastrointestinal Toxicity
- Gastrointestinal toxicity is common in patients treated with Panobinostat. Patients who experience diarrhea, nausea, or vomiting may require treatment interruption or dose reduction (Table 3). At the first sign of abdominal cramping, loose stools, or onset of diarrhea, patients should be treated with anti-diarrheal medication (e.g., loperamide). Consider and administer prophylactic anti-emetics as clinically indicated.
- Other Adverse Drug Reactions
- For patients experiencing Grade 3/4 adverse drug reactions other than thrombocytopenia, neutropenia, or gastrointestinal toxicity, the recommendation is the following:
- CTC Grade 2 toxicity recurrence and CTC Grade 3 and 4 - omit the dose until recovery to CTC Grade 1 or less and restart treatment at a reduced dose
- CTC Grade 3 or 4 toxicity recurrence, a further dose reduction may be considered once the adverse events have resolved to CTC Grade 1 or less.
- Dose Modifications for Use in Hepatic Impairment
- Reduce the starting dose of Panobinostat to 15 mg in patients with mild hepatic impairment and 10 mg in patients with moderate hepatic impairment. Avoid use in patients with severe hepatic impairment. Monitor patients frequently for adverse events and adjust dose as needed for toxicity.
- Dose Modifications for Use with Strong CYP3A Inhibitors
- Reduce the starting dose of Panobinostat to 10 mg when coadministered with strong CYP3A inhibitors (e.g., boceprevir, clarithromycin, conivaptan, indinavir, itraconazole, ketoconazole, lopinavir/ritonavir).
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Panobinostat in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Panobinostat in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
The safety and efficacy of Panobinostat in children has not been established.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Panobinostat in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Panobinostat in pediatric patients.
Contraindications
None
Warnings
|
FATAL AND SERIOUS TOXICITIES: SEVERE DIARRHEA AND CARDIAC TOXICITIES
See full prescribing information for complete Boxed Warning.
Severe diarrhea occurred in 25% of Panobinostat treated patients. Monitor for symptoms, institute anti-diarrheal treatment, interrupt Panobinostat and then reduce dose or discontinue Panobinostat. Severe and fatal cardiac ischemic events, severe arrhythmias, and ECG changes have occurred in patients receiving Panobinostat. Arrhythmias may be exacerbated by electrolyte abnormalities. Obtain ECG and electrolytes at baseline and periodically during treatment as clinically indicated. |
Severe diarrhea occurred in 25% of patients treated with Panobinostat. Diarrhea of any grade occurred in 68% of patients treated with Panobinostat compared to 42% of patients in the control arm. Diarrhea can occur at any time. Monitor patient hydration status and electrolyte blood levels, including potassium, magnesium and phosphate, at baseline and weekly (or more frequently as clinically indicated) during therapy and correct to prevent dehydration and electrolyte disturbances. Initiate anti-diarrheal medication at the onset of diarrhea. Interrupt Panobinostat at the onset of moderate diarrhea (4 to 6 stools per day). Ensure that patients initiating therapy with Panobinostat have anti-diarrheal medications on hand.
Cardiac Toxicities
Severe and fatal cardiac ischemic events, as well as severe arrhythmias, and electrocardiogram (ECG) changes occurred in patients receiving Panobinostat. Arrhythmias occurred in 12% of patients receiving Panobinostat, compared to 5% of patients in the control arm. Cardiac ischemic events occurred in 4% of patients treated with Panobinostat compared with 1% of patients in the control arm. Do not initiate Panobinostat treatment in patients with history of recent myocardial infarction or unstable angina.
Electrocardiographic abnormalities such as ST-segment depression and T-wave abnormalities also occurred more frequently in patients receiving Panobinostat compared to the control arm: 22% versus 4% and 40% versus 18%, respectively. Panobinostat may prolong cardiac ventricular repolarization (QT interval). Do not initiate treatment with Panobinostat in patients with a QTcF >450 msec or clinically significant baseline ST-segment or T-wave abnormalities. Arrhythmias may be exacerbated by electrolyte abnormalities. If during treatment with Panobinostat, the QTcF increases to ≥480 msec, interrupt treatment. Correct any electrolyte abnormalities. If QT prolongation does not resolve, permanently discontinue treatment with Panobinostat.
Obtain ECG at baseline and periodically during treatment as clinically indicated. Monitor electrolytes during treatment with Panobinostat and correct abnormalities as clinically indicated.
Fatal and serious hemorrhage occurred during treatment with Panobinostat. In the clinical trial in patients with relapsed multiple myeloma, 5 patients receiving Panobinostat compared to 1 patient in the control arm died due to a hemorrhagic event. All 5 patients had grade ≥3 thrombocytopenia at the time of the event. Grade 3/4 hemorrhage was reported in 4% of patients treated with the Panobinostat arm and 2% of patients in the control arm.
Panobinostat causes myelosuppression, including severe thrombocytopenia, neutropenia and anemia. In the clinical trial in patients with relapsed multiple myeloma, 67% of patients treated with Panobinostat developed Grade 3 to 4 thrombocytopenia compared with 31% in the control arm. Thrombocytopenia led to treatment interruption and or dose modification in 31% of patients receiving Panobinostat compared to 11% of patients in the control arm. For patients receiving Panobinostat, 33% required platelet transfusion compared to 10% of patients in the control arm.
Severe neutropenia occurred in 34% of patients treated with Panobinostat, compared to 11% of patients in the control arm. Neutropenia led to treatment interruption and or dose modification in 10% of patients receiving Panobinostat. The use of granulocyte-colony stimulating factor (G-CSF) was higher in patients treated with Panobinostat compared to the control arm, 13% compared to 4%, respectively.
Obtain a baseline CBC and monitor the CBC weekly during treatment (or more frequently if clinically indicated). Dose modifications are recommended for Myelosuppression. Monitor CBCs more frequently in patients over 65 years of age due to the increased frequency of myelosuppression in these patients.
Infections
Localized and systemic infections, including pneumonia, bacterial infections, invasive fungal infections, and viral infections have been reported in patients taking Panobinostat. Severe infections occurred in 31% of patients (including 10 deaths) treated with Panobinostat compared with 24% of patients (including 6 deaths) in the control arm. Infections of all grades occurred at a similar rate between arms. Panobinostat treatment should not be initiated in patients with active infections. Monitor patients for signs and symptoms of infections during treatment; if a diagnosis of infection is made, institute appropriate anti-infective treatment promptly and consider interruption or discontinuation of Panobinostat.
Hepatic dysfunction, primarily elevations in aminotransferases and total bilirubin, occurred in patients treated with Panobinostat. Liver function should be monitored prior to treatment and regularly during treatment. If abnormal liver function tests are observed dose adjustments may be considered and the patient should be followed until values return to normal or pretreatment levels.
Embryo-Fetal Toxicity
Panobinostat can cause fetal harm when administered to a pregnant woman. Panobinostat was teratogenic in rats and rabbits. If Panobinostat is used during pregnancy, or if the patient becomes pregnant while taking Panobinostat, the patient should be apprised of the potential hazard to the fetus.
Advise females of reproductive potential to avoid becoming pregnant while taking Panobinostat. Advise sexually-active females of reproductive potential to use effective contraception while taking Panobinostat and for at least 3 months after the last dose of Panobinostat.
Advise sexually active men to use condoms while on treatment and for 6 months after their last dose of Panobinostat.
Adverse Reactions
Clinical Trials Experience
The following adverse reactions are described in detail in other sections of the label:
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data reflect subject exposure to Panobinostat from a clinical trial, in which 758 subjects with relapsed multiple myeloma received Panobinostat in combination with bortezomib and dexamethasone or placebo in combination with bortezomib and dexamethasone (referred to as the control arm). The median duration of exposure to Panobinostat was 5 months with 16% of patients exposed to study treatment for ≥48 weeks.
Serious adverse events (SAEs) occurred in 60% of patients in the Panobinostat, bortezomib, and dexamethasone compared to 42% of patients in the control arm. The most frequent (≥5%) treatment-emergent SAEs reported for patients treated with Panobinostat were pneumonia (18%), diarrhea, (11%), thrombocytopenia (7%), fatigue (6%), and sepsis (6%).
Adverse reactions that led to discontinuation of Panobinostat occurred in 36% of patients. The most common adverse reactions leading to treatment discontinuations were diarrhea, fatigue, and pneumonia.
Deaths occurred in 8% of patients in the Panobinostat arm versus 5% on the control arm. The most frequent causes of death were infection and hemorrhage.
Table 4 summarizes the adverse reactions occurring in at least 10% of patients with ≥ 5% greater incidence in the Panobinostat arm, and Table 5 summarizes the treatment-emergent laboratory abnormalities.
- Table 4: Adverse Reactions (≥10% Incidence and ≥5% Greater Incidence in Panobinostat-Arm) in Patients with Multiple Myeloma
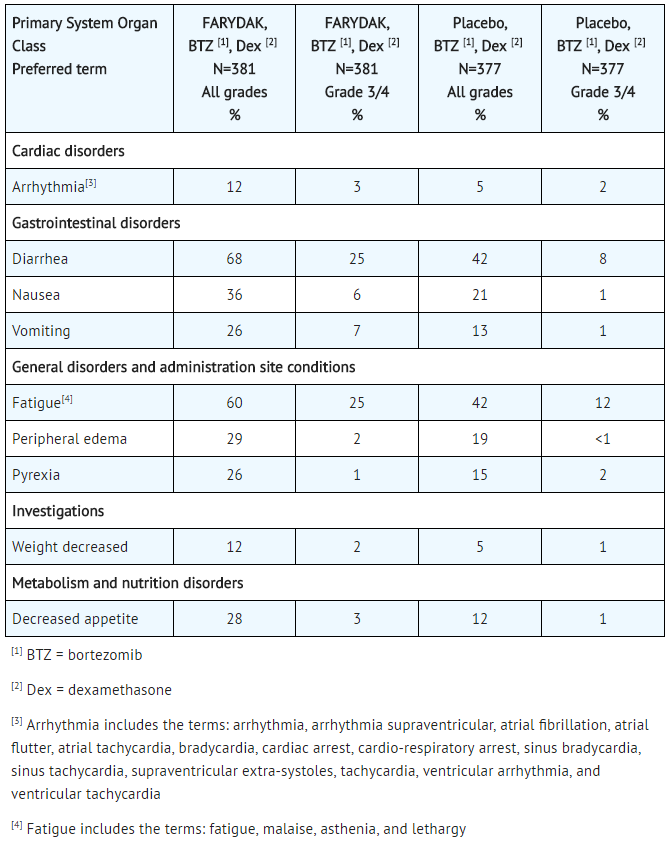
FARYDAK: Panobinostat's Brand name
Other Adverse Reactions
Other notable adverse drug reactions of Panobinostat not described above, which were either clinically significant, or occurred with a frequency less than 10% but had a frequency in the Panobinostat arm greater than 2% over the control arm in the multiple myeloma clinical trial are listed below:
- Infections and infestations: hepatitis B.
- Endocrine disorders: hypothyroidism.
- Metabolism and nutrition disorders: hyperglycemia, dehydration, fluid retention, hyperuricemia, hypomagnesemia.
- Cardiac disorders: palpitations.
- Vascular disorders: hypotension, hypertension, orthostatic hypotension.
- Respiratory, thoracic and mediastinal disorders: cough, dyspnea, respiratory failure, rales, wheezing.
- Gastrointestinal disorders: abdominal pain, dyspepsia, gastritis, cheilitis,abdominal distension,dry mouth, flatulence, colitis, gastrointestinal pain.
- Musculoskeletal and connective tissue disorders: joint swelling.
- Renal and urinary disorders: renal failure, urinary incontinence.
- General disorders and administration site conditions: chills.
- Investigations: blood urea increased, glomerular filtration rate decreased, blood alkaline phosphatase increased.
- Psychiatric disorders: insomnia.
- Table 5: Treatment-emergent Laboratory Abnormalities (≥10% Incidence and ≥5% Greater Incidence in Panobinostat-arm) in Patients with Multiple Myeloma
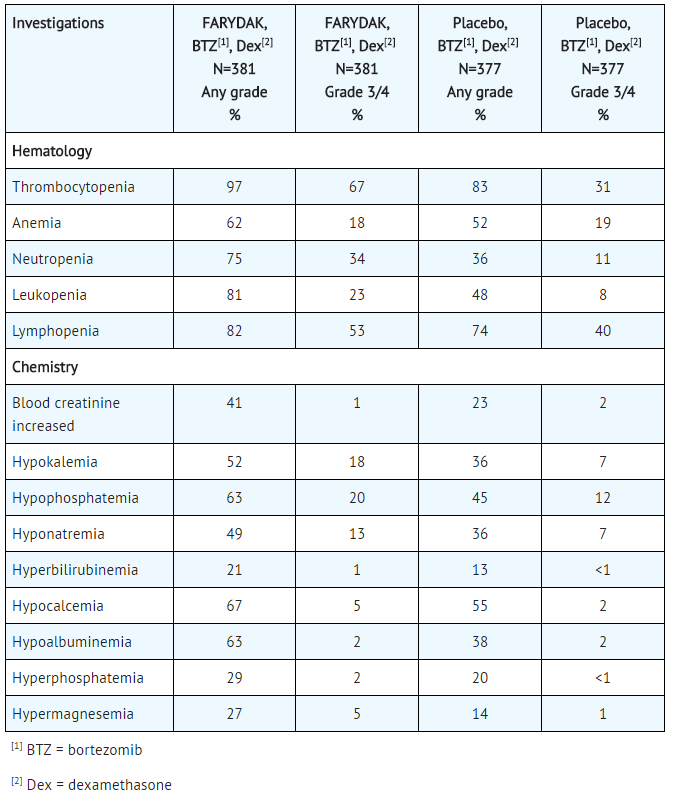
FARYDAK: Panobinostat's Brand name
Grade 1 to Grade 4 asthenic conditions (fatigue, malaise, asthenia, and lethargy) were reported in 60% of the patients in the Panobinostat arm compared to 42% of patients in the control arm. Grade ≥3 asthenic conditions were reported in 25% of the patients in the Panobinostat arm compared to 12% of patients in the control arm. Asthenic conditions led to treatment discontinuation in 6% of patients in the Panobinostat arm versus 3% of patients in the control arm.
The prespecified sub-group upon which the efficacy and safety of Panobinostat was based had a similar adverse reaction profile to the entire safety population of patients treated with Panobinostat, bortezomib, and dexamethasone.
Postmarketing Experience
There is limited information regarding Panobinostat Postmarketing Experience in the drug label.
Drug Interactions
Panobinostat is a CYP3A substrate and inhibits CYP2D6. Panobinostat is a P-glycoprotein (P-gp) transporter system substrate.
Agents that May Increase Panobinostat Blood Concentrations
- Reduce dose to 10 mg when coadministered with strong CYP3A inhibitors (e.g., boceprevir, clarithromycin, conivaptan, indinavir, itraconazole, ketoconazole, lopinavir/ritonavir, nefazodone, nelfinavir, posaconazole, ritonavir, saquinavir, telaprevir, telithromycin, voriconazole). Instruct patients to avoid star fruit, pomegranate or pomegranate juice, and grapefruit or grapefruit juice because these foods are known to inhibit CYP3A enzymes.
Agents that May Decrease Panobinostat Plasma Concentrations
- CYP3A Inducers: Coadministration of Panobinostat with strong CYP3A inducers was not evaluated in vitro or in a clinical trial however, a reduction in panobinostat exposure is likely. An approximately 70% decrease in the systemic exposure of panobinostat in the presence of strong inducers of CYP3A was observed in simulations using mechanistic models. Therefore, the concomitant use of strong CYP3A inducers should be avoided.
Agents whose Plasma Concentrations May be Increased by Panobinostat
- CYP2D6 Substrates: Panobinostat increased the median Cmax and AUC of a sensitive substrate of CYP2D6 by approximately 80% and 60%, respectively; however this was highly variable. Avoid coadministrating Panobinostat with sensitive CYP2D6 substrates (i.e., atomoxetine, desipramine, dextromethorphan,metoprolol, nebivolol, perphenazine, tolterodine, and venlafaxine) or CYP2D6 substrates that have a narrow therapeutic index (i.e., thioridazine, pimozide). If concomitant use of CYP2D6 substrates is unavoidable, monitor patients frequently for adverse reactions.
Drugs that Prolong QT interval
- Concomitant use of anti-arrhythmic medicines (including, but not limited to amiodarone, disopyramide, procainamide, quinidine and sotalol) and other drugs that are known to prolong the QT interval (including, but not limited to chloroquine, halofantrine, clarithromycin, methadone, moxifloxacin, bepridil and pimozide) is not recommended. Anti-emetic drugs with known QT prolonging risk, such as dolasetron, ondansetron, and tropisetron can be used with frequent ECG monitoring.
Use in Specific Populations
Pregnancy
- Risk Summary
- Panobinostat can cause fetal harm when administered to a pregnant woman. Panobinostat was teratogenic in rats and rabbits. If Panobinostat is used during pregnancy or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to the fetus.
- Data
- Animal Data
- In embryofetal development studies, panobinostat was administered orally 3 times per week during the period of organogenesis to pregnant rats (30, 100, and 300 mg/kg) and rabbits (10, 40, and 80 mg/kg). In rats, maternal toxicity including death was observed at doses greater than or equal to 100 mg/kg/day. Embryofetal toxicities occurred at 30 mg/kg (the only dose with live fetuses) and consisted of fetal malformations and anomalies, such as cleft palate, short tail, extra presacral vertebrae, and extra ribs. The dose of 30 mg/kg resulted in exposures (AUCs) approximately 3-fold the human exposure at the human dose of 20 mg. In rabbits, maternal toxicity including death was observed at doses greater than or equal to 80 mg/kg. Increased pre- and/or post-implantation loss occurred at all doses tested. Embryofetal toxicities included decreased fetal weights at doses greater than or equal to 40 mg/kg and malformations (absent digits, cardiac interventricular septal defects, aortic arch interruption, missing gallbladder, and irregular ossification of skull) at 80 mg/kg. The dose of 40 mg/kg in rabbits results in systemic exposure approximately 4-fold the human exposure and the dose of 80 mg/kg results in exposure 7-fold the human exposure, at the human dose of 20 mg.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Panobinostat in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Panobinostat during labor and delivery.
Nursing Mothers
It is not known whether Panobinostat is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse drug reactions in nursing infants, decide whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
The safety and efficacy of Panobinostat in children has not been established.
Geriatic Use
In clinical trials of Panobinostat in patients with multiple myeloma, 42% of patients were 65 years of age or older.
Patients over 65 years of age had a higher frequency of selected adverse events and of discontinuation of treatment due to adverse events. In patients over 65 years of age, the incidence of deaths not related to disease progression was 9% in patients ≥65 years of age compared to 5 % in patients <65.
In the randomized clinical trial in patients with relapsed multiple myeloma, no major differences in effectiveness were observed in older patients compared to younger patients. Adverse reactions leading to permanent discontinuation occurred in 45% of patients ≥65 years of age in the Panobinostat treatment arm compared to 30% of patients <65 years age in the Panobinostat treatment arm. Monitor for toxicity more frequently in patients over 65 years of age, especially for gastrointestinal toxicity, myelosuppression, and cardiac toxicity.
Gender
There is no FDA guidance on the use of Panobinostat with respect to specific gender populations.
Race
There is no FDA guidance on the use of Panobinostat with respect to specific racial populations.
Renal Impairment
Mild (creatinine clearance (CrCl) ≥50 to <80 mL/min) to severe renal impairment (CrCl <30 mL/min) did not impact the plasma exposure of panobinostat. Panobinostat has not been studied in patients with end stage renal disease (ESRD) or patients on dialysis. The dialyzability of panobinostat is unknown.
Hepatic Impairment
The safety and efficacy of Panobinostat in patients with hepatic impairment has not been evaluated.
In a pharmacokinetic trial, patients with mild (bilirubin ≤1xULN and AST >1xULN, or bilirubin >1.0 to 1.5x ULN and any AST) or moderate (bilirubin >1.5x to 3.0x ULN, any AST) hepatic impairment (NCI-ODWG criteria) had increased AUC of panobinostat by 43% and 105%, respectively. Reduce the starting dose of Panobinostat in patients with mild or moderate hepatic impairment. Avoid use in patients with severe hepatic impairment. Monitor patients with hepatic impairment frequently for adverse events.
Females of Reproductive Potential and Males
Embryofetal toxicity including malformations occurred in embryofetal development studies in rats.
Pregnancy Testing
Perform pregnancy testing in women of childbearing potential prior to starting treatment with Panobinostat and intermittently during treatment with Panobinostat.
- Females
- Panobinostat can cause fetal harm. Advise females of reproductive potential to avoid becoming pregnant while taking Panobinostat. Advise sexually-active females of reproductive potential to use effective contraception while taking Panobinostat and for at least 3 months after the last dose of Panobinostat. Advise patients to contact their healthcare provider if they become pregnant, or if pregnancy is suspected, while taking Panobinostat.
- Males
- Advise sexually active men to use condoms while on treatment and for at least 6 months after their last dose of Panobinostat.
Immunocompromised Patients
There is no FDA guidance one the use of Panobinostat in patients who are immunocompromised.
Administration and Monitoring
Administration
- Panobinostat should be taken orally once on each scheduled day at about the same time, either with or without food
- Panobinostat capsules should be swallowed whole with a cup of water. Do not open, crush, or chew the capsules
- If a dose is missed it can be taken up to 12 hours after the specified dose time. If vomiting occurs the patient should not repeat the dose, but should take the next usual scheduled dose.
- Counsel patients on the correct dosing schedule, technique of administration of Panobinostat, and when to take Panobinostat if dosing adjustments are made.
Monitoring
Prior to the start of Panobinostat treatment and during treatment, monitoring should include:
- Complete Blood Count (CBC): Obtain a CBC before initiating treatment. Verify that the baseline platelet count is at least 100 x 109/L and the baseline absolute neutrophil count (ANC) is at least 1.5 x 109/L. Monitor the CBC weekly (or more often as clinically indicated) during treatment.
- ECG: Perform an ECG prior to the start of therapy and repeat periodically during treatment as clinically indicated. Verify that the QTcF is less than 450 msec prior to initiation of treatment with Panobinostat. If during treatment with Panobinostat, the QTcF increases to ≥480 msec, interrupt treatment. Correct any electrolyte abnormalities. If QT prolongation does not resolve, permanently discontinue treatment with Panobinostat. During the clinical trial, ECGs were performed at baseline and prior to initiation of each cycle for the first 8 cycles.
- Serum Electrolytes: Obtain electrolytes, including potassium and magnesium, at baseline and monitor during therapy. Correct abnormal electrolyte values before treatment. During the trial, monitoring was conducted prior to the start of each cycle, at Day 11 of cycles 1 to 8, and at the start of each cycle for cycles 9 to 16.
For additional information please refer to the bortezomib and dexamethasone prescribing information.
IV Compatibility
There is limited information regarding the compatibility of Panobinostat and IV administrations.
Overdosage
There is limited experience with overdosage. Expect exaggeration of adverse reactions observed during the clinical trial, including hematologic and gastrointestinal reactions such as thrombocytopenia, pancytopenia, diarrhea, nausea, vomiting and anorexia. Monitor cardiac status including ECGs, and assess and correct electrolytes. Consider platelet transfusions for thrombocytopenic bleeding. It is not known if Panobinostat is dialyzable.
Pharmacology
Mechanism of Action
Panobinostat is a histone deacetylase (HDAC) inhibitor that inhibits the enzymatic activity of HDACs at nanomolar concentrations. HDACs catalyze the removal of acetyl groups from the lysine residues of histones and some non-histone proteins. Inhibition of HDAC activity results in increased acetylation of histone proteins, an epigenetic alteration that results in a relaxing of chromatin, leading to transcriptional activation. In vitro, panobinostat caused the accumulation of acetylated histones and other proteins, inducing cell cycle arrest and/or apoptosis of some transformed cells. Increased levels of acetylated histones were observed in xenografts from mice that were treated with panobinostat. Panobinostat shows more cytotoxicity towards tumor cells compared to normal cells.
Structure
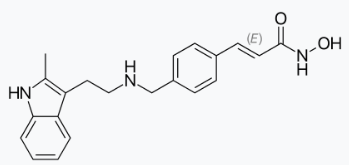
Panobinostat lactate is a histone deacetylase inhibitor.
The chemical name of panobinostat lactate is 2-Hydroxypropanoic acid, compd. with 2-(E)-N-hydroxy-3-[4-[([2-(2-methyl-1H-indol-3-yl)ethyl]amino)methyl]phenyl]-2-propenamide (1:1).
The structural formula is:

Panobinostat lactate anhydrous is a white to slightly yellowish or brownish powder. The molecular formula is C21H23N3O2•C3H6O3 (lactate); its molecular weight is 439.51 (as a lactate), equivalent to 349.43 (free base). Panobinostat lactate anhydrous is light sensitive. Panobinostat lactate anhydrous is both chemically and thermodynamically a stable crystalline form with no polymorphic behavior. Panobinostat free base is not chiral and shows no specific optical rotation. Panobinostat lactate anhydrous is slightly soluble in water. Solubility of panobinostat lactate anhydrous is pH-dependent, with the highest solubility in buffer pH 3.0 (citrate).
Panobinostat capsules contain 10 mg, 15 mg, or 20 mg panobinostat free base (equivalent to 12.58 mg, 18.86 mg, and 25.15 mg respectively of panobinostat lactate). The inactive ingredients are magnesium stearate, mannitol, microcrystalline cellulose and pregelatinized starch. The capsules contain gelatin, FD&C Blue 1 (10 mg capsules), yellow iron oxide (10 mg and 15 mg capsules), red iron oxide (15 mg and 20 mg capsules) and titanium dioxide.
Pharmacodynamics
Panobinostat may prolong cardiac ventricular repolarization (QT interval). In the randomized multiple myeloma trial, QTc prolongation with values between 451 msec to 480 msec occurred in 10.8% of Panobinostat treated patients. Events with values of 481 msec to 500 msec occurred in 1.3% of Panobinostat treated patients. A maximum QTcF increase from baseline of between 31 msec and 60 msec was reported in 14.5% of Panobinostat treated patients. A maximum QTcF increase from baseline of >60 msec was reported in 0.8% of Panobinostat treated patients. No episodes of QTcF prolongation >500 msec have been reported with the dose of 20 mg Panobinostat in the randomized multiple myeloma trial conducted in combination with bortezomib and dexamethasone. Pooled clinical data from over 500 patients treated with single agent Panobinostat in multiple indications and at different dose levels has shown that the incidence of CTC Grade 3 QTc prolongation (QTcF >500 msec) was approximately 1% overall and 5% or more at a dose of 60 mg or higher.
Pharmacokinetics
The absolute oral bioavailability of Panobinostat is approximately 21%. Peak concentrations of panobinostat are observed within 2 hours (Tmax) of oral administration in patients with advanced cancer. Panobinostat exhibits an approximate dose proportional increase in both Cmax and AUC over the dosing range.
Plasma panobinostat Cmax and AUC(0–48) were approximately 44% and 16% lower compared to fasting conditions, respectively, following ingestion of an oral Panobinostat dose 30 minutes after a high-fat meal by 36 patients with advanced cancer. The median Tmax was also delayed by 2.5 hours in these patients.
The aqueous solubility of panobinostat is pH dependent, with higher pH resulting in lower solubility. Coadministration of Panobinostat with drugs that elevate the gastric pH was not evaluated in vitro or in a clinical trial; however, altered panobinostat absorption was not observed in simulations using physiologically-based pharmacokinetic (PBPK) models.
Panobinostat is approximately 90% bound to human plasma proteins in vitro and is independent of concentration. Panobinostat is a P-gp substrate.
Panobinostat is extensively metabolized. Pertinent metabolic pathways involved in the biotransformation of panobinostat are reduction, hydrolysis, oxidation, and glucuronidation processes. The fraction metabolized through CYP3A accounts for approximately 40% of the total hepatic panobinostat elimination. In vitro, additional contributions from the CYP2D6 and CYP2C19 pathways are minor. In vitro, UGT1A1, UGT1A3, UGT1A7, UGT1A8, UGT1A9, and UGT2B4 contribute to the glucuronidation of panobinostat.
Elimination
Twenty-nine percent to 51% of administered radioactivity is excreted in urine and 44% to 77% in the feces after a single oral dose of [14C] panobinostat in 4 patients with advanced cancer. Unchanged panobinostat accounted for <2.5% of the dose in urine and <3.5% of the dose in feces with the remainder consisting of metabolites.
An oral clearance (CL/F) and terminal elimination half-life (t1/2) of approximately 160 L/hr and 37 hours, respectively, was estimated using a population based pharmacokinetic (pop-PK) model in patients with advanced cancer. An inter-subject variability 65% on the clearance estimate was also reported. Up to 2-fold accumulation was observed with chronic oral dosing in patients with advanced cancer.
Specific Populations
- Population pharmacokinetic (PK) analyses of Panobinostat indicated that body surface area, gender, age, and race do not have a clinically meaningful influence on clearance.
- Hepatic Impairment: The effect of hepatic impairment on the pharmacokinetics of panobinostat was evaluated in a phase 1 study in 24 patients with advanced cancer with varying degrees of hepatic impairment. In patients with NCI-CTEP class mild (i.e., Group B) and moderate (i.e., Group C) hepatic impairment, AUC(0-inf) increased 43% and 105% compared to the group with normal hepatic function, respectively. The relative change in Cmax followed a similar pattern. The effect of severe hepatic impairment was indeterminate in this study due to the small sample size (n=1). A dose modification is recommended for patients with mild and moderate hepatic impairment.
- Renal Impairment: The effect of renal impairment on the pharmacokinetics of panobinostat was assessed in a phase 1 trial of 37 patients with advanced cancer and varying degrees of renal impairment. Panobinostat AUC(0–inf) in the mild, moderate and severe renal impairment groups were 64%, 99% and 59%, of the normal group, respectively. The relative change in Cmax followed a similar pattern.
Drug Interactions:
- Strong CYP3A Inhibitors: Coadministration of a single 20 mg Panobinostat dose with ketoconazole (200 mg twice daily for 14 days) increased the Cmax and AUC(0–48) of panobinostat by 62% and 73% respectively, compared to when Panobinostat was given alone in 14 patients with advanced cancer. Tmax was unchanged. A modified starting dose is recommended.
- Strong CYP3A Inducers: The human oxidative metabolism of panobinostat via the cytochrome P450 system primarily involves CYP3A isozymes. Simulations using PBPK models, predicted an approximately 70% decrease in the systemic exposure of panobinostat in the presence of strong inducers of CYP3A. Avoid coadministration of Panobinostat with strong CYP3A inducers.
- CYP2D6 Substrates: Coadministration of a single 60 mg dextromethorphan (DM) dose with Panobinostat (20 mg once per day, on Days 3, 5, and 8) increased the Cmax and AUC(0–∞) of DM by 20% to 200% and 20% to 130% (interquartile ranges), respectively, compared to when DM was given alone in 14 patients with advanced cancer. These DM exposures were extremely variable (CV% >150%). Avoid coadministration of Panobinostat with sensitive CYP2D6 substrates or CYP2D6 substrates that have a narrow therapeutic index.
- In vitro studies with CYP or UDPglucuronosyltransferase (UGT) substrates: Panobinostat inhibits CYP2D6, CYP2C19 and CYP3A4 (time-dependent), but does not inhibit CYP1A2, CYP2C8, CYP2C9, and CYP2E. Panobinostat does not induce CYP1A1/2, CYP2B6, CYP2C8/9/19, CYP3A and UGT1A1.
- In vitro studies with drug transporter system substrates: Panobinostat inhibits OAT3, OCT1, OCT2, OATP1B1 and OATP1B3, but does not inhibit P-gp and breast cancer resistant protein (BCRP), or OAT1. Panobinostat does not induce P-gp and multidrug resistance protein 2 (MRP2) transporters.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with panobinostat.
Panobinostat was mutagenic in the Ames assay, and caused endo-reduplication (increased number of chromosomes) in human peripheral blood lymphocytes in vitro and DNA damage in an in vitro COMET assay in mouse lymphoma L5178Y cells.
Panobinostat may impair male and female fertility. In an oral fertility study conducted in rats, 10, 30, or 100 mg/kg doses of panobinostat were administered to females 3 times weekly (Days 1, 3, and 5) for 2 weeks prior to mating, then during the mating period, and on gestation Days 0, 3, and 6. An increase in early resorption and/or post-implantation loss in female rats were observed at doses ≥10 mg/kg. Number of pregnancies was reduced at doses ≥30 mg/kg. Prostate atrophy accompanied by reduced secretory granules, and testicular degeneration, oligospermia and increased epididymal debris were observed in repeated dose oral toxicity studies in dogs, e.g., in the 4-week study at the dose of 1.5 mg/kg. These effects were not completely reversed following a 4-week nondosing period.
Animal Toxicology and/or Pharmacology
Adverse findings observed in animals and not reported (or reported with low incidence) in patients treated with panobinostat include thyroid, bone marrow, and skin findings. Thyroid hormone changes in oral studies in rats and dogs included decreases in triodothyronine (T3), tetraiodothyronine (T4) and thyroid stimulating hormone (TSH). Histopathology changes of the thyroid included decreases in follicular colloid and epithelial vacuolation, and increases in thyroid follicular hypertrophy. A benign thyroid follicular cell adenoma was also seen in 1 rat in the 26-week study. Bone marrow findings in one or both species included hyperostosis, plasmacytosis, increased number of granulocytic cells, and presence of abnormal cytoplasmic granulation. Osseous metaplasia of the lung and skin hyperplasia and papilloma were observed in dogs in the 39-week study.
Clinical Studies
Relapsed Multiple Myeloma
The efficacy and safety of Panobinostat in combination with bortezomib and dexamethasone was evaluated in a randomized, double-blind, placebo-controlled, multicenter study in patients with relapsed multiple myeloma who had received 1 to 3 prior lines of therapy.
Patients received bortezomib (1.3 mg/m2 injected intravenously) with dexamethasone (20 mg) in addition to Panobinostat 20 mg (or placebo), taken orally every other day, for 3 doses per week in Weeks 1 and 2 of each 21-day cycle. Treatment was administered for a maximum of 16 cycles (48 weeks).
A total of 768 patients were randomized in a 1:1 ratio to receive either the combination of Panobinostat, bortezomib, dexamethasone (n=387) or placebo, bortezomib, dexamethasone (n=381), stratified by prior use of bortezomib and the number of prior lines of anti-myeloma therapy. Demographics and baseline disease characteristics were balanced between arms. The median age was 63 years (range 28 to 84); 42% of patients were older than 65 years; 53% of patients were male; Caucasians comprised 65% of the study population, Asians 30%, and blacks 3%. The ECOG performance status was 0 to 1 in 93% of patients. The median number of prior therapies was 1; 48% of patients received 2 or 3 prior lines of therapy. More than half (57%) of the patients had prior stem cell transplantation. The most common prior antineoplastic therapies were corticosteroids (90%), melphalan (80%), thalidomide (53%), cyclophosphamide (47%), bortezomib (44%), and lenalidomide (19%). The median duration of follow-up was 29 months in both arms.
The primary endpoint was progression-free survival (PFS), using modified European Bone Marrow Transplant Group (EBMT) criteria, as assessed by the investigators. In the overall trial population, the median PFS (95% CI) was 12 months (10.3, 12.9) in the Panobinostat, bortezomib, dexamethasone arm and 8.1 months (7.6, 9.2) in the placebo, bortezomib, dexamethasone arm, [HR: 0.63 (95% CI: 0.52, 0.76)]. At the time of interim analysis, overall survival was not statistically different between arms. The approval of Panobinostat was based upon the efficacy and safety in a prespecified subgroup analysis of 193 patients who had received prior treatment with both bortezomib and an immunomodulatory agent and a median of 2 prior therapies as the benefit:risk appeared to be greater in this more heavily pretreated population than in the overall trial population. Of these 193 patients, 76% of them had received ≥2 prior lines of therapy. The median PFS (95% CI) was 10.6 months (7.6, 13.8) in the Panobinostat, bortezomib, and dexamethasone arm and 5.8 months (4.4, 7.1) in the placebo, bortezomib, and dexamethasone arm [HR: 0.52 (0.36, 0.76)]. Efficacy results are summarized in Table 6 and the Kaplan- Meier curves for PFS are provided in Figure 1.
- Table 6: Efficacy Results from the Multiple Myeloma Trial in Patients who Received Prior Treatment with Bortezomib and an Immunomodulating Agent

FARYDAK: Panobinostat's Brand name
- Figure 1: Kaplan-Meier Plot of Progression-Free Survival in Patients with Multiple Myeloma who Received Prior Treatment with Both Bortezomib and an Immunomodulatory Agent

FARYDAK: Panobinostat's Brand name
In the subgroup of patients who had received prior treatment with both bortezomib and an immunomodulatory agent (n=193), the overall response rate using modified EBMT criteria was 59% in the Panobinostat, bortezomib, and dexamethasone arm and 41% in the placebo, bortezomib, and dexamethasone arm. Response rates are summarized in Table 7.
- Table 7: Response Rates

FARYDAK: Panobinostat's Brand name
How Supplied
- Panobinostat 10 mg (equivalent to 12.58 mg of panobinostat lactate): Size # 3 light green opaque capsule, radial markings on cap with black ink “LBH 10 mg” and two radial bands with black ink on body, containing white to almost white powder.
- Panobinostat 15 mg (equivalent to 18.86 mg of panobinostat lactate): Size #1 orange opaque capsule, radial markings on cap with black ink “LBH 15 mg” and two radial bands with black ink on body, containing white to off-white powder.
- Panobinostat 20 mg (equivalent to 25.15 mg of panobinostat lactate): Size #1 red opaque capsule, radial markings on cap with black ink “LBH 20 mg” and two radial bands with black ink on body, containing white to off-white powder.
Panobinostat capsules are packaged in PVC/PCTFE blister packs.
10 mg: Blister packs containing 6 capsules ………………………….…….NDC 0078-0650-06
15 mg: Blister packs containing 6 capsules ………………………….…….NDC 0078-0651-06
20 mg: Blister packs containing 6 capsules ………………………….…….NDC 0078-0652-06
Storage
Store at 20°C to 25°C (68°F to 77°F), excursions permitted between 15°C and 30°C (59°F and 86°F). Store blister pack in original carton to protect from light. Panobinostat capsules should not be opened, crushed, or chewed. Direct contact of the powder in Panobinostat capsules with the skin or mucous membranes should be avoided. If such contact occurs wash thoroughly. Personnel should avoid exposure to crushed and/or broken capsules.
Panobinostat is a cytotoxic drug. Follow special handling and disposal procedures.
Images
Drug Images
{{#ask: Page Name::Panobinostat |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel



{{#ask: Label Page::Panobinostat |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
- Dosing and Administration
- Instruct patients to take Panobinostat exactly as prescribed and not to change their dose or to stop taking Panobinostat unless they are told to do so by their healthcare provider. If a patient misses a dose, advise them to take their dose as soon possible and up to 12 hours after the specified dose time. If vomiting occurs advise the patient not to repeat the dose, but to take the next usual prescribed dose on schedule.
- Cardiac Toxicity/Electrocardiographic Changes
- Inform patients to report chest pain or discomfort, changes in heart beat (fast or slow), palpitations, lightheadedness, fainting, dizziness, blue discoloration of lips, shortness of breath, and swelling of lower limbs or skin as these may be warning signs of a heart problem.
- Bleeding Risk
- Inform patients that Panobinostat is associated with thrombocytopenia. Advise patients to contact their healthcare provider right away if they experience any signs of bleeding and inform patients that it might take longer than usual for them to stop bleeding. Advise patients of the need to monitor blood chemistry and hematology prior to the start of Panobinostat therapy and periodically thereafter.
- Infections
- Inform patients of the risk of neutropenia and severe and life-threatening infections. Instruct patients to contact their physician immediately if they develop a fever and/or any exhibit any signs of infection.
- Gastrointestinal Toxicities
- Inform patients that Panobinostat can cause severe nausea, vomiting and diarrhea which may require medication for treatment. Advise patients to contact their physician at the start of diarrhea, for persistent vomiting, or signs of dehydration. Inform patients to consult with their physicians prior to using medications with laxative properties.
- Pregnancy
- Inform patients that Panobinostat can cause fetal harm. Advise women of reproductive potential to avoid pregnancy while taking Panobinostat. Advise women of reproductive potential to use effective contraception while taking Panobinostat and for at least 3 months after the last dose of the drug.
- Advise sexually active men to use condoms while receiving Panobinostat and for at least 6 months following the last dose of the drug.
- Lactation
- Advise women not to breastfeed while taking Panobinostat.

Precautions with Alcohol
Alcohol-Panobinostat interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
FARYDAK®
Look-Alike Drug Names
There is limited information regarding Panobinostat Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.