Lenalidomide
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Rabin Bista, M.B.B.S. [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: EMBRYO-FETAL TOXICITY, HEMATOLOGIC TOXICITY, AND VENOUS AND ARTERIAL THROMBOEMBOLISM :
See full prescribing information for complete Boxed Warning.
Embryo-Fetal Toxicity:
Hematologic Toxicity (Neutropenia and Thrombocytopenia):
Venous and Arterial Thromboembolism:
|
Overview
Lenalidomide is a Immune Modulator that is FDA approved for the treatment of Multiple myeloma(MM), Transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes (MDS), Mantle cell lymphoma (MCL). There is a Black Box Warning for this drug as shown here. Common adverse reactions include fatigue, neutropenia, constipation, diarrhea, muscle cramp, anemia, pyrexia, peripheral edema, nausea, back pain, upper respiratory tract infection, dyspnea, dizziness, thrombocytopenia, tremor and rash.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Indications
Multiple Myeloma
- REVLIMID in combination with dexamethasone is indicated for the treatment of patients with multiple myeloma (MM) who have received at least one prior therapy.
Myelodysplastic Syndromes
- REVLIMID is indicated for the treatment of patients with transfusion-dependent anemia due to low- or intermediate-1-risk myelodysplastic syndromes (MDS) associated with a deletion 5q cytogenetic abnormality with or without additional cytogenetic abnormalities.
Mantle Cell Lymphoma
- REVLIMID is indicated for the treatment of patients with mantle cell lymphoma (MCL) whose disease has relapsed or progressed after two prior therapies, one of which included bortezomib.
Limitations of Use
- REVLIMID is not indicated and is not recommended for the treatment of patients with CLL outside of controlled clinical trials
Dosage
Multiple Myeloma
- The recommended starting dose of REVLIMID is 25 mg once daily on Days 1-21 of repeated 28-day cycles. The recommended dose of dexamethasone is 40 mg once daily on Days 1-4, 9-12, and 17-20 of each 28-day cycle for the first 4 cycles of therapy and then 40 mg once daily orally on Days 1-4 every 28 days. Treatment is continued or modified based upon clinical and laboratory findings.
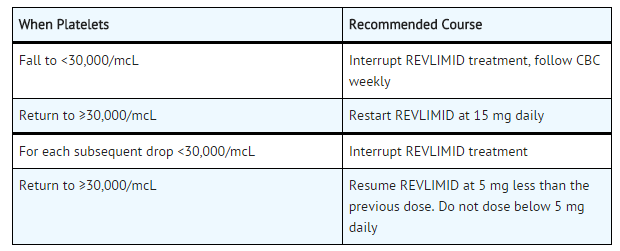
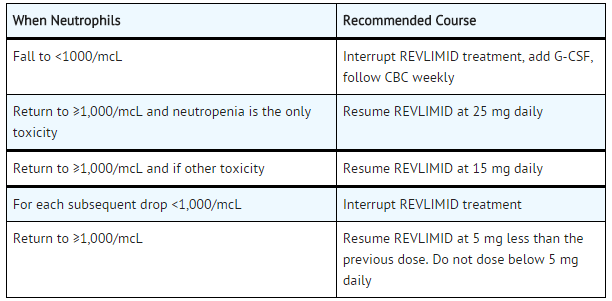
Dose Adjustments for Hematologic Toxicities During Multiple Myeloma Treatment
- Dose modification guidelines, as summarized below, are recommended to manage Grade 3 or 4 neutropenia or thrombocytopenia or other Grade 3 or 4 toxicity judged to be related to REVLIMID.
=Platelet counts=
=Thrombocytopenia in MM=
=Absolute Neutrophil counts (ANC)=
=Neutropenia in MM=
=Other Grade 3 / 4 Toxicities in MM=
- For other Grade 3/4 toxicities judged to be related to REVLIMID, hold treatment and restart at the physician's discretion at next lower dose level when toxicity has resolved to ≤ Grade 2.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lenalidomide in adult patients.
Non–Guideline-Supported Use
- Chronic lymphoid leukemia, Relapsed or refractory[1][2]
- Multiple myeloma, In combination with dexamethasone, first-line therapy[3][4]
- Myelofibrosis[5]
- Non-Hodgkin's lymphoma, Aggressive disease, relapsed or refractory[6]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Use of Lenalidomide in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lenalidomide in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lenalidomide in pediatric patients.
Contraindications
Pregnancy
- REVLIMID can cause fetal harm when administered to a pregnant female. Limb abnormalities were seen in the offspring of monkeys that were dosed with lenalidomide during organogenesis. This effect was seen at all doses tested. Due to the results of this developmental monkey study, and lenalidomide’s structural similarities to thalidomide, a known human teratogen, lenalidomide is contraindicated in females who are pregnant. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to the fetus
Allergic Reactions
- REVLIMID is contraindicated in patients who have demonstrated hypersensitivity (e.g., angioedema, Stevens-Johnson syndrome, toxic epidermal necrolysis) to lenalidomide
Warnings
|
WARNING: EMBRYO-FETAL TOXICITY, HEMATOLOGIC TOXICITY, AND VENOUS AND ARTERIAL THROMBOEMBOLISM :
See full prescribing information for complete Boxed Warning.
Embryo-Fetal Toxicity:
Hematologic Toxicity (Neutropenia and Thrombocytopenia):
Venous and Arterial Thromboembolism:
|
Embryo-Fetal Toxicity
- REVLIMID is a thalidomide analogue and is contraindicated for use during pregnancy. Thalidomide is a known human teratogen that causes life-threatening human birth defects or embryo-fetal death. An embryo-fetal development study in monkeys indicates that lenalidomide produced malformations in the offspring of female monkeys who received the drug during pregnancy, similar to birth defects observed in humans following exposure to thalidomide during pregnancy.
- REVLIMID is only available through the REVLIMID REMS™ program (formerly known as the “RevAssist® program”)
Females of Reproductive Potential
- Females of reproductive potential must avoid pregnancy for at least 4 weeks before beginning REVLIMID therapy, during therapy, during dose interruptions and for at least 4 weeks after completing therapy.
- Females must commit either to abstain continuously from heterosexual sexual intercourse or to use two methods of reliable birth control, beginning 4 weeks prior to initiating treatment with REVLIMID, during therapy, during dose interruptions and continuing for 4 weeks following discontinuation of REVLIMID therapy.
- Two negative pregnancy tests must be obtained prior to initiating therapy. The first test should be performed within 10-14 days and the second test within 24 hours prior to prescribing REVLIMID therapy and then weekly during the first month, then monthly thereafter in women with regular menstrual cycles or every 2 weeks in women with irregular menstrual cycles.
Males
- Lenalidomide is present in the semen of patients receiving the drug. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking REVLIMID and for up to 28 days after discontinuing REVLIMID, even if they have undergone a successful vasectomy. Male patients taking REVLIMID must not donate sperm.
Blood Donation
- Patients must not donate blood during treatment with REVLIMID and for 1 month following discontinuation of the drug because the blood might be given to a pregnant female patient whose fetus must not be exposed to REVLIMID.
REVLIMID REMS™ program
- Because of the embryo-fetal risk, REVLIMID is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS), the REVLIMID REMS™ program (formerly known as the “RevAssist®” program).
- Required components of the REVLIMID REMS™ program include the following:
- Prescribers must be certified with the REVLIMID REMS™ program by enrolling and complying with the REMS requirements.
- Patients must sign a Patient-Physician agreement form and comply with the REMS requirements. In particular, female patients of reproductive potential who are not pregnant must comply with the pregnancy testing and contraception requirements and males must comply with contraception requirements.
- Pharmacies must be certified with the REVLIMID REMS™ program, must only dispense to patients who are authorized to receive REVLIMID and comply with REMS requirements.
- Further information about the REVLIMID REMS™ program is available at www.celgeneriskmanagement.com or by telephone at 1-888-423-5436.
Hematologic Toxicity
- REVLIMID can cause significant neutropenia and thrombocytopenia. Patients taking REVLIMID for MDS should have their complete blood counts monitored weekly for the first 8 weeks and at least monthly thereafter. Patients taking REVLIMID for MM should have their complete blood counts monitored every 2 weeks for the first 12 weeks and then monthly thereafter. Patients taking REVLIMID for MCL should have their complete blood counts monitored weekly for the first cycle (28 days), every 2 weeks during cycles 2-4, and then monthly thereafter. Patients may require dose interruption and/or dose reduction.
- Grade 3 or 4 hematologic toxicity was seen in 80% of patients enrolled in the MDS study. In the 48% of patients who developed Grade 3 or 4 neutropenia, the median time to onset was 42 days (range, 14-411 days), and the median time to documented recovery was 17 days (range, 2-170 days). In the 54% of patients who developed Grade 3 or 4 thrombocytopenia, the median time to onset was 28 days (range, 8-290 days), and the median time to documented recovery was 22 days (range, 5-224 days.
- In the pooled MM trials Grade 3 and 4 hematologic toxicities were more frequent in patients treated with the combination of REVLIMID and dexamethasone than in patients treated with dexamethasone alone.
- In the MCL trial, Grade 3 or 4 neutropenia was reported in 43% of the patients. Grade 3 or 4 thrombocytopenia was reported in 28% of the patients.
Venous and Arterial Thromboembolism
- Venous thromboembolic events (deep venous thrombosis and pulmonary embolism) and arterial thromboses are increased in patients treated with REVLIMID. A significantly increased risk of DVT (7.4%) and of PE (3.7%) occurred in patients with multiple myeloma who were treated with REVLIMID and dexamethasone therapy compared to patients treated in the placebo and dexamethasone group (3.1% and 0.9%) in clinical trials with varying use of anticoagulant therapies.
- Myocardial infarction (1.7%) and stroke (CVA) (2.3%) are increased in patients with multiple myeloma who were treated with REVLIMID and dexamethasone therapy compared to patients treated with placebo and dexamethasone (0.6%, and 0.9%) in clinical trials. Patients with known risk factors, including prior thrombosis, may be at greater risk and actions should be taken to try to minimize all modifiable factors (e.g. hyperlipidemia, hypertension, smoking)
- In controlled clinical trials that did not use concomitant thromboprophylaxis, 21.5% overall thrombotic events (Standardized MedDRA Query Embolic and Thrombotic events) occurred in patients with refractory and relapsed multiple myeloma who were treated with REVLIMID and dexamethasone compared to 8.3% thrombosis in patients treated with placebo and dexamethasone. The median time to first thrombosis event was 2.7 months. Thromboprophylaxis is recommended. The regimen of thromboprophylaxis should be based on an assessment of the patient’s underlying risks. Instruct patients to report immediately any signs and symptoms suggestive of thrombotic events. ESAs and estrogens may further increase the risk of thrombosis and their use should be based on a benefit-risk decision in patients receiving REVLIMID.
Increased Mortality in Patients with CLL
- In a prospective randomized (1:1) clinical trial in the first line treatment of patients with chronic lymphocytic leukemia, single agent REVLIMID therapy increased the risk of death as compared to single agent chlorambucil. In an interim analysis, there were 34 deaths among 210 patients on the REVLIMID treatment arm compared to 18 deaths among 211 patients in the chlorambucil treatment arm, and hazard ratio for overall survival was 1.92 [95% CI: 1.08 – 3.41], consistent with a 92% increase in the risk of death. The trial was halted for safety in July 2013.
- Serious adverse cardiovascular reactions, including atrial fibrillation, myocardial infarction, and cardiac failure occurred more frequently in the REVLIMID treatment arm. REVLIMID is not indicated and not recommended for use in CLL outside of controlled clinical trials.
Second Primary Malignancies
- Patients with multiple myeloma treated with lenalidomide in studies including melphalan and stem cell transplantation had a higher incidence of second primary malignancies, particularly acute myelogenous leukemia (AML) and Hodgkin lymphoma, compared to patients in the control arms who received similar therapy but did not receive lenalidomide. Monitor patients for the development of second malignancies. Take into account both the potential benefit of lenalidomide and the risk of second primary malignancies when considering treatment with lenalidomide.
Hepatotoxicity
- Hepatic failure, including fatal cases, has occurred in patients treated with lenalidomide in combination with dexamethasone. In clinical trials, 15% of patients experienced hepatotoxicity (with hepatocellular, cholestatic and mixed characteristics); 2% of patients with multiple myeloma and 1% of patients with myelodysplasia had serious hepatotoxicity events. The mechanism of drug-induced hepatotoxicity is unknown. Pre-existing viral liver disease, elevated baseline liver enzymes, and concomitant medications may be risk factors. Monitor liver enzymes periodically. Stop REVLIMID upon elevation of liver enzymes. After return to baseline values, treatment at a lower dose may be considered.
Allergic Reactions
- Angioedema and serious dermatologic reactions including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have been reported. These events can be fatal. Patients with a prior history of Grade 4 rash associated with thalidomide treatment should not receive REVLIMID. REVLIMID interruption or discontinuation should be considered for Grade 2-3 skin rash. REVLIMID must be discontinued for angioedema, Grade 4 rash, exfoliative or bullous rash, or if SJS or TEN is suspected and should not be resumed following discontinuation for these reactions.
- REVLIMID capsules contain lactose. Risk-benefit of REVLIMID treatment should be evaluated in patients with lactose intolerance.
Tumor Lysis Syndrome
- Fatal instances of tumor lysis syndrome have been reported during treatment with lenalidomide. The patients at risk of tumor lysis syndrome are those with high tumor burden prior to treatment. These patients should be monitored closely and appropriate precautions taken.
Tumor Flare Reaction
- Tumor flare reaction has occurred during investigational use of lenalidomide for CLL and lymphoma, and is characterized by tender lymph node swelling, low grade fever, pain and rash. REVLIMID is not indicated and not recommended for use in CLL outside of controlled clinical trials.
- Monitoring and evaluation for tumor flare reaction (TFR) is recommended in patients with MCL. Tumor flare reaction may mimic progression of disease (PD). In the MCL trial, 13/134 (10%) of subjects experienced TFR; all reports were Grade 1 or 2 in severity. All of the events occurred in cycle 1 and one patient developed TFR again in cycle 11. Lenalidomide may be continued in patients with Grade 1 and 2 TFR without interruption or modification, at the physician’s discretion. Patients with Grade 1 and 2 TFR may also be treated with corticosteroids, non-steroidal anti-inflammatory drugs (NSAIDs) and/or narcotic analgesics for management of TFR symptoms. In patients with Grade 3 or 4 TFR, it is recommended to withhold treatment with lenalidomide until TFR resolves to ≤ Grade 1. Patients with Grade 3 or 4 TFR may be treated for management of symptoms per the guidance for treatment of Grade 1 and 2 TFR.
Adverse Reactions
Clinical Trials Experience
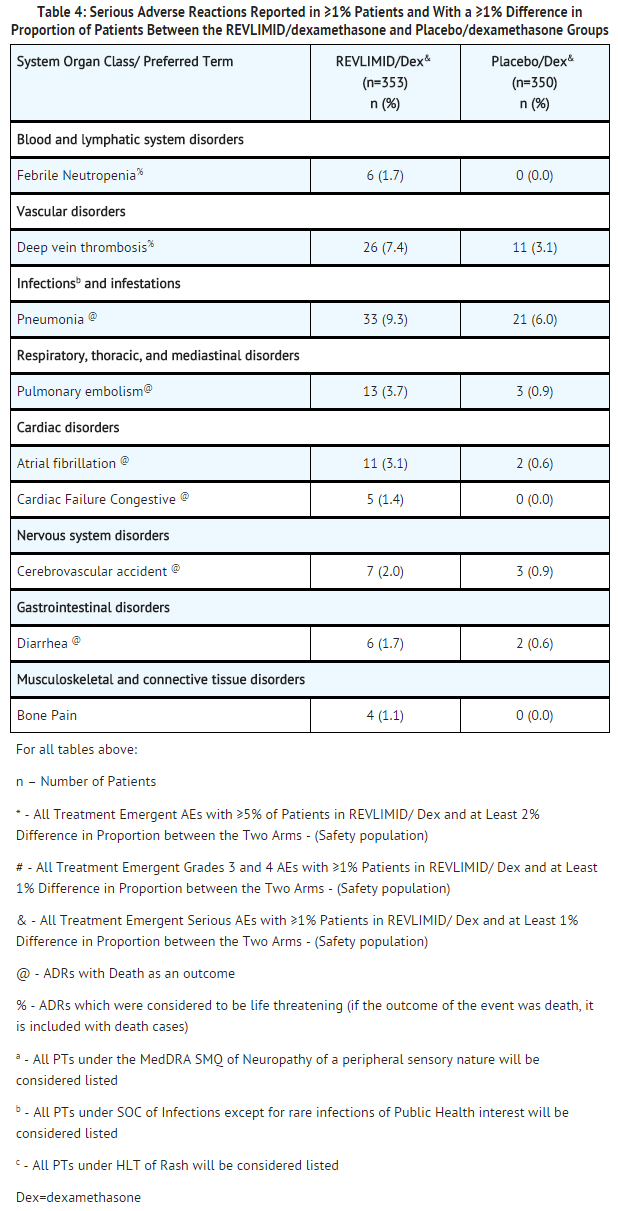
Clinical Trials Experience in Multiple Myeloma
- Data were evaluated from 703 patients in two studies who received at least one dose of REVLIMID/dexamethasone (353 patients) or placebo/dexamethasone (350 patients).
- In the REVLIMID/dexamethasone treatment group, 269 patients (76%) had at least one dose interruption with or without a dose reduction of REVLIMID compared to 199 patients (57%) in the placebo/dexamethasone treatment group. Of these patients who had one dose interruption with or without a dose reduction, 50% in the REVLIMID/dexamethasone treatment group had at least one additional dose interruption with or without a dose reduction compared to 21% in the placebo/dexamethasone treatment group. Most adverse events and Grade 3/4 adverse events were more frequent in patients who received the combination of REVLIMID/dexamethasone compared to placebo/dexamethasone.
- TABLES 2, 3, and 4 summarize the adverse reactions reported for REVLIMID/dexamethasone and placebo/dexamethasone groups.
- Median duration of exposure among patients treated with REVLIMID/dexamethasone was 44 weeks while median duration of exposure among patients treated with placebo/dexamethasone was 23 weeks. This should be taken into consideration when comparing frequency of adverse events between two treatment groups REVLIMID/dexamethasone vs. placebo/dexamethasone.
Venous and Arterial Thromboembolism
- Deep vein thrombosis (DVT) was reported as a serious (7.4%) or severe (8.2%) adverse drug reaction at a higher rate in the REVLIMID/dexamethasone group compared to 3.1 % and 3.4% in the placebo/dexamethasone group, respectively. Discontinuations due to DVT adverse reactions were reported at comparable rates between groups.
- Pulmonary embolism (PE) was reported as a serious adverse drug reaction including Grade 3/4 (3.7%) at a higher rate in the REVLIMID/dexamethasone group compared to 0.9% in the placebo/dexamethasone group. Discontinuations due to PE adverse reactions were reported at comparable rates between groups.
- Myocardial infarction was reported as a serious (1.7%) or severe (1.7%) adverse drug reaction at a higher rate in the REVLIMID/dexamethasone group compared to 0.6 % and 0.6% respectively in the placebo/dexamethasone group. Discontinuation due to MI (including acute) adverse reactions was 0.8% in REVLIMID/dexamethasone group and none in the placebo/dexamethasone group.
- Stroke (CVA) was reported as a serious (2.3%) or severe (2.0%) adverse drug reaction in the REVLIMID/dexamethasone group compared to 0.9% and 0.9% respectively in the placebo/dexamethasone group. Discontinuation due to stroke (CVA) was 1.4% in REVLIMID/ dexamethasone group and 0.3% in the placebo/dexamethasone group.
Other Adverse Reactions
- In these clinical studies of REVLIMID in patients with multiple myeloma, the following adverse drug reactions (ADRs) not described above that occurred at ≥1% rate and of at least twice of the placebo percentage rate were reported:
Blood and lymphatic system disorders
Cardiac disorders
Endocrine disorders
Eye disorders
Gastrointestinal disorders
General disorders and administration site conditions
Investigations
- liver function tests abnormal
- alanine aminotransferase increased
Nervous system disorders
Psychiatric disorders
Reproductive system and breast disorders
Respiratory, thoracic and mediastinal disorders
Skin and subcutaneous tissue disorders
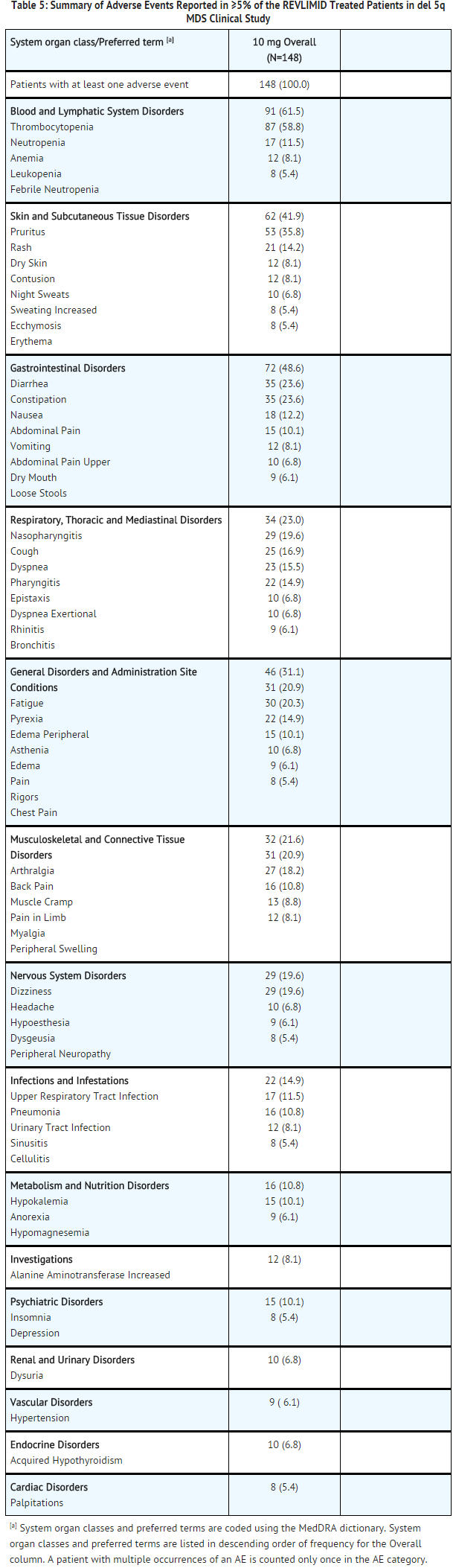
Clinical Trials Experience in Myelodysplastic Syndromes
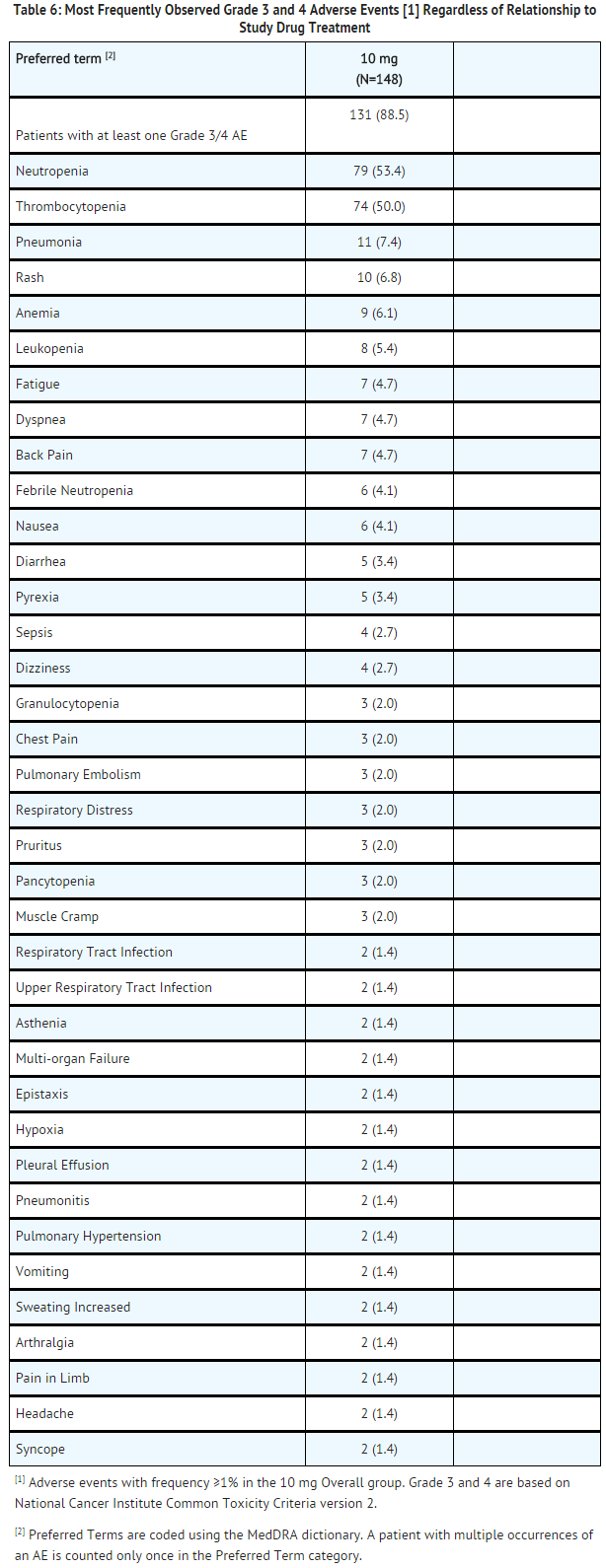
- A total of 148 patients received at least 1 dose of 10 mg REVLIMID in the del 5q MDS clinical study. At least one adverse event was reported in all of the 148 patients who were treated with the 10 mg starting dose of REVLIMID. The most frequently reported adverse events were related to blood and lymphatic system disorders, skin and subcutaneous tissue disorders, gastrointestinal disorders, and general disorders and administrative site conditions.
- Thrombocytopenia (61.5%; 91/148) and neutropenia (58.8%; 87/148) were the most frequently reported adverse events. The next most common adverse events observed were diarrhea (48.6%; 72/148), pruritus (41.9%; 62/148), rash (35.8%; 53/148) and fatigue (31.1%; 46/148). Table 5 summarizes the adverse events that were reported in ≥ 5% of the REVLIMID treated patients in the del 5q MDS clinical study. TABLE 6 summarizes the most frequently observed Grade 3 and Grade 4 adverse reactions regardless of relationship to treatment with REVLIMID. In the single-arm studies conducted, it is often not possible to distinguish adverse events that are drug-related and those that reflect the patient’s underlying disease.
- In other clinical studies of REVLIMID in MDS patients, the following serious adverse events (regardless of relationship to study drug treatment) not described in TABLE 5 or 6 were reported:
Blood and lymphatic system disorders
- warm type hemolytic anemia
- splenic infarction
- bone marrow depression
- coagulopathy
- hemolysis
- hemolytic anemia
- refractory anemia
Cardiac disorders
- cardiac failure congestive
- atrial fibrillation
- angina pectoris
- cardiac arrest
- cardiac failure
- cardio-respiratory arrest
- cardiomyopathy
- myocardial infarction
- myocardial ischemia
- atrial fibrillation aggravated
- bradycardia
- cardiogenic shock
- pulmonary edema
- supraventricular arrhythmia
- tachyarrhythmia
- ventricular dysfunction
Ear and labyrinth disorders
Endocrine disorders
Gastrointestinal disorders
- gastrointestinal hemorrhage
- colitis ischemic
- intestinal perforation
- rectal hemorrhage
- colonic polyp
- diverticulitis
- dysphagia
- gastritis
- gastroenteritis
- gastroesophageal reflux disease
- obstructive inguinal hernia
- irritable bowel syndrome
- melena
- pancreatitis due to biliary obstruction
- pancreatitis
- perirectal abscess
- small intestinal obstruction
- upper gastrointestinal hemorrhage
General disorders and administration site conditions
- disease progression
- fall
- abnormal gait
- intermittent pyrexia
- nodule
- rigors
- sudden death
Hepatobiliary disorders
Immune system disorders
Infections and infestations
- infection
- bacteremia
- central line infection
- clostridial infection
- ear infection
- Enterobacter sepsis
- fungal infection
- herpes viral infection NOS
- influenza,
- kidney infection
- Klebsiella sepsis
- lobar pneumonia
- localized infection
- oral infection
- Pseudomonas infection
- septic shock
- sinusitis acute
- sinusitis
- Staphylococcal infection
- urosepsis
Injury, poisoning and procedural complications
- femur fracture
- transfusion reaction
- cervical vertebral fracture
- femoral neck fracture
- fractured pelvis
- hip fracture
- overdose
- post procedural hemorrhage
- rib fracture
- road traffic accident
- spinal compression fracture
Investigations
- blood creatinine increased
- hemoglobin decreased
- liver function tests abnormal
- troponin I increased
Metabolism and nutrition disorders
Musculoskeletal and connective tissue disorders
- arthritis
- arthritis aggravated
- gouty arthritis
- neck pain
- chondrocalcinosis pyrophosphate
Neoplasms benign, malignant and unspecified
- acute leukemia
- acute myeloid leukemia
- bronchoalveolar carcinoma
- lung cancer metastatic
- lymphoma
- prostate cancer metastatic
Nervous system disorders
- cerebrovascular accident
- aphasia
- cerebellar infarction
- cerebral infarction
- depressed level of consciousness
- dysarthria
- migraine
- spinal cord compression
- subarachnoid hemorrhage
- transient ischemic attack
Psychiatric disorders
- confusional state
Renal and urinary disorders
- renal failure
- hematuria
- renal failure acute
- azotemia
- calculus ureteric
- renal mass
Reproductive system and breast disorders
Respiratory, thoracic and mediastinal disorders
- bronchitis
- chronic obstructive airways disease exacerbated
- respiratory failure
- dyspnea exacerbated
- interstitial lung disease
- lung infiltration
- wheezing
Skin and subcutaneous tissue disorders
Vascular system disorders
- deep vein thrombosis
- hypotension
- aortic disorder
- ischemia
- thrombophlebitis superficial
- thrombosis
Clinical Trials Experience in Mantle Cell Lymphoma
- In the MCL trial, a total of 134 patients received at least 1 dose of REVLIMID. Their median age was 67 (range 43-83) years, 128/134 (96%) were Caucasian, 108/134 (81%) were males and 82/134 (61%) had duration of MCL for at least 3 years.
- Table 7 summarizes the most frequently observed adverse reactions regardless of relationship to treatment with REVLIMID. Across the 134 patients treated in this study, median duration of treatment was 95 days (1-1002 days). Seventy-eight patients (58%) received 3 or more cycles of therapy, 53 patients (40%) received 6 or more cycles, and 26 patients (19%) received 12 or more cycles. Seventy-six patients (57%) underwent at least one dose interruption due to adverse events, and 51 patients (38%) underwent at least one dose reduction due to adverse events. Twenty-six patients (19%) discontinued treatment due to adverse events.
- The following adverse events which have occurred in other indications and not described above have been reported (5-10%) in patients treated with REVLIMID monotherapy for mantle cell lymphoma.
General disorders and administration site conditions
- Chills
Musculoskeletal and connective tissue disorders
- Pain in extremity
- Nervous system disorders
- Dysguesia
- headache
- peripheral neuropathy
Infections and infestations
Skin and subcutaneous tissue disorders
- Dry skin
- night sweats
- The following serious adverse events not described above and reported in 2 or more patients treated with REVLIMID monotherapy for mantle cell lymphoma.
Respiratory, Thoracic and Mediastinal Disorders
Infections and Infestations
Neoplasms benign, malignant and unspecified (incl cysts and polyps)
Cardiac Disorder
Postmarketing Experience
- The following adverse drug reactions have been identified from the worldwide post-marketing experience with REVLIMID: Allergic conditions (angioedema, SJS, TEN), tumor lysis syndrome (TLS) and tumor flare reaction (TFR), pneumonitis, hepatic failure, including fatality, toxic hepatitis, cytolytic hepatitis, cholestatic hepatitis, and mixed cytolytic/cholestatic hepatitis and transient abnormal liver laboratory tests. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Cases of hypothyroidism and hyperthyroidism have also been reported. Optimal control of thyroid function is recommended before start of treatment. Baseline and ongoing monitoring of thyroid function is recommended.
Drug Interactions
- Results from human in vitro studies show that REVLIMID is neither metabolized by nor inhibits or induces the cytochrome P450 pathway suggesting that lenalidomide is not likely to cause or be subject to P450-based metabolic drug interactions.
- In vitro studies demonstrated that REVLIMID is not a substrate of human breast cancer resistance protein (BCRP), multidrug resistance protein (MRP) transporters MRP1, MRP2, or MRP3, organic anion transporters (OAT) OAT1 and OAT3, organic anion transporting polypeptide 1B1 (OATP1B1 or OATP2), organic cation transporters (OCT) OCT1 and OCT2, multidrug and toxin extrusion protein (MATE) MATE1, and organic cation transporters novel (OCTN) OCTN1 and OCTN2.
- In vitro, lenalidomide is a substrate, but is not an inhibitor of P-glycoprotein (P-gp).
Digoxin
- When digoxin was co-administered with multiple doses of REVLIMID (10 mg/day) the digoxin Cmax and AUC0-∞ were increased by 14%. Periodic monitoring of digoxin plasma levels, in accordance with clinical judgment and based on standard clinical practice in patients receiving this medication, is recommended during administration of REVLIMID.
Warfarin
- Co-administration of multiple dose REVLIMID (10 mg) with single dose warfarin (25 mg) had no effect on the pharmacokinetics of total lenalidomide or R- and S-warfarin. Expected changes in laboratory assessments of PT and INR were observed after warfarin administration, but these changes were not affected by concomitant REVLIMID administration. It is not known whether there is an interaction between dexamethasone and warfarin. Close monitoring of PT and INR is recommended in multiple myeloma patients taking concomitant warfarin.
Concomitant Therapies That May Increase the Risk of Thrombosis
- Erythropoietic agents, or other agents that may increase the risk of thrombosis, such as estrogen containing therapies, should be used with caution after making a benefit-risk assessment in patients receiving REVLIMID
Use in Specific Populations
Pregnancy
Risk Summary
- REVLIMID can cause embryo-fetal harm when administered to a pregnant female and is contraindicated during pregnancy. REVLIMID is a thalidomide analogue.
- Thalidomide is a human teratogen, inducing a high frequency of severe and life-threatening birth defects such as amelia (absence of limbs), phocomelia (short limbs), hypoplasticity of the bones, absence of bones, external ear abnormalities (including anotia, micropinna, small or absent external auditory canals), facial palsy, eye abnormalities (anophthalmos, microphthalmos), and congenital heart defects. Alimentary tract, urinary tract, and genital malformations have also been documented and mortality at or shortly after birth has been reported in about 40% of infants.
- Lenalidomide caused thalidomide-type limb defects in monkey offspring. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, the patient should be apprised of the potential hazard to a fetus.
- If pregnancy does occur during treatment, immediately discontinue the drug. Under these conditions, refer patient to an obstetrician/gynecologist experienced in reproductive toxicity for further evaluation and counseling. Any suspected fetal exposure to REVLIMID must be reported to the FDA via the MedWatch program at 1-800-FDA-1088 and also to Celgene Corporation at 1-888-423-5436.
Animal data
- In an embryo-fetal developmental toxicity study in monkeys, teratogenicity, including thalidomide-like limb defects, occurred in offspring when pregnant monkeys received oral lenalidomide during organogenesis. Exposure (AUC) in monkeys at the lowest dose was 0.17 times the human exposure at the maximum recommended human dose (MRHD) of 25 mg. Similar studies in pregnant rabbits and rats at 20 times and 200 times the MRHD respectively, produced embryo lethality in rabbits and no adverse reproductive effects in rats.
- In a pre- and post-natal development study in rats, animals received lenalidomide from organogenesis through lactation. The study revealed a few adverse effects on the offspring of female rats treated with lenalidomide at doses up to 500 mg/kg (approximately 200 times the human dose of 25 mg based on body surface area). The male offspring exhibited slightly delayed sexual maturation and the female offspring had slightly lower body weight gains during gestation when bred to male offspring. As with thalidomide, the rat model may not adequately address the full spectrum of potential human embryo-fetal developmental effects for lenalidomide.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lenalidomide in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Lenalidomide during labor and delivery.
Nursing Mothers
It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for adverse reactions in nursing infants from lenalidomide, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- Safety and effectiveness in pediatric patients below the age of 18 have not been established.
Geriatic Use
- REVLIMID has been used in multiple myeloma (MM) clinical trials in patients up to 86 years of age.
- Of the 703 MM patients who received study treatment in Studies 1 and 2, 45% were age 65 or over while 12% of patients were age 75 and over. The percentage of patients age 65 or over was not significantly different between the REVLIMID/dexamethasone and placebo/dexamethasone groups. Of the 353 patients who received REVLIMID/dexamethasone, 46% were age 65 and over. In both studies, patients > 65 years of age were more likely than patients ≤ 65 years of age to experience DVT, pulmonary embolism, atrial fibrillation, and renal failure following use of REVLIMID. No differences in efficacy were observed between patients over 65 years of age and younger patients.
- REVLIMID has been used in del 5q MDS clinical trials in patients up to 95 years of age.
- Of the 148 patients with del 5q MDS enrolled in the major study, 38% were age 65 and over, while 33% were age 75 and over. Although the overall frequency of adverse events (100%) was the same in patients over 65 years of age as in younger patients, the frequency of serious adverse events was higher in patients over 65 years of age than in younger patients (54% vs. 33%). A greater proportion of patients over 65 years of age discontinued from the clinical studies because of adverse events than the proportion of younger patients (27% vs.16%). No differences in efficacy were observed between patients over 65 years of age and younger patients.
- REVLIMID has been used in a mantle cell lymphoma (MCL) clinical trial in patients up to 83 years of age. Of the 134 patients with MCL enrolled in the MCL trial, 63% were age 65 and over, while 22% of patients were age 75 and over. The overall frequency of adverse events was similar in patients over 65 years of age and in younger patients (98% vs. 100%). The overall incidence of grade 3 and 4 adverse events was also similar in these 2 patient groups (79% vs. 78%, respectively). The frequency of serious adverse events was higher in patients over 65 years of age than in younger patients (55% vs. 41%). No differences in efficacy were observed between patients over 65 years of age and younger patients.
- Since elderly patients are more likely to have decreased renal function, care should be taken in dose selection. Monitor renal function.
Gender
There is no FDA guidance on the use of Lenalidomide with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lenalidomide with respect to specific racial populations.
Renal Impairment
- Since lenalidomide is primarily excreted unchanged by the kidney, adjustments to the starting dose of REVLIMID are recommended to provide appropriate drug exposure in patients with moderate (CLcr 30-60 mL/min) or severe renal impairment (CLcr < 30 mL/min) and in patients on dialysis
Hepatic Impairment
- No dedicated study has been conducted in patients with hepatic impairment. The elimination of unchanged lenalidomide is predominantly by the renal route.
Females of Reproductive Potential and Males
- REVLIMID can cause fetal harm when administered during pregnancy. Females of reproductive potential must avoid pregnancy 4 weeks before therapy, while taking REVLIMID, during dose interruptions and for at least 4 weeks after completing therapy.
Females
- Females of reproductive potential must commit either to abstain continuously from heterosexual sexual intercourse or to use two methods of reliable birth control simultaneously (one highly effective form of contraception – tubal ligation, IUD, hormonal (birth control pills, injections, hormonal patches, vaginal rings or implants) or partner’s vasectomy and one additional effective contraceptive method – male latex or synthetic condom, diaphragm or cervical cap. Contraception must begin 4 weeks prior to initiating treatment with REVLIMID, during therapy, during dose interruptions and continuing for 4 weeks following discontinuation of REVLIMID therapy. Reliable contraception is indicated even where there has been a history of infertility, unless due to hysterectomy. Females of reproductive potential should be referred to a qualified provider of contraceptive methods, if needed.
- Females of reproductive potential must have 2 negative pregnancy tests before initiating REVLIMID. The first test should be performed within 10-14 days, and the second test within 24 hours prior to prescribing REVLIMID. Once treatment has started and during dose interruptions, pregnancy testing for females of reproductive potential should occur weekly during the first 4 weeks of use, then pregnancy testing should be repeated every 4 weeks in females with regular menstrual cycles. If menstrual cycles are irregular, the pregnancy testing should occur every 2 weeks. Pregnancy testing and counseling should be performed if a patient misses her period or if there is any abnormality in her menstrual bleeding. REVLIMID treatment must be discontinued during this evaluation.
Males
- Lenalidomide is present in the semen of males who take REVLIMID. Therefore, males must always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking REVLIMID, during dose interruptions and for up to 28 days after discontinuing REVLIMID, even if they have undergone a successful vasectomy. Male patients taking REVLIMID must not donate sperm
Immunocompromised Patients
There is no FDA guidance one the use of Lenalidomide in patients who are immunocompromised.
Administration and Monitoring
Administration
- REVLIMID should be taken orally at about the same time each day, either with or without food. REVLIMID capsules should be swallowed whole with water. The capsules should not be opened, broken, or chewed.
Monitoring
- Patients on therapy for del 5q myelodysplastic syndromes should have their complete blood counts monitored weekly for the first 8 weeks of therapy and at least monthly thereafter.
- Monitor for and advise patients about signs and symptoms of thromboembolism.
- Monitor patients at risk of Tumor Lysis Syndromes (i.e., those with high tumor burden) and take appropriate precautions
- monitor liver function
IV Compatibility
There is limited information regarding IV Compatibility of Lenalidomide in the drug label.
Overdosage
- There is no specific experience in the management of lenalidomide overdose in patients; although in dose-ranging studies, some patients were exposed to up to 150 mg and in single-dose studies, some patients were exposed to up to 400 mg.
- In studies, the dose-limiting toxicity was essentially hematological. In the event of overdose, supportive care is advised.
Pharmacology
| |
| |
Lenalidomide
| |
| Systematic (IUPAC) name | |
| (RS)-3-(4-Amino-1-oxo 1,3-dihydro-2H-isoindol- 2-yl)piperidine-2,6-dione | |
| Identifiers | |
| CAS number | |
| ATC code | L04 |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 259.261 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 30% |
| Metabolism | Undetermined |
| Half life | 3 h |
| Excretion | Renal (67% unchanged) |
| Therapeutic considerations | |
| Pregnancy cat. |
X(US) |
| Legal status |
[[Prescription drug|Template:Unicode-only]](US) |
| Routes | Oral |
Mechanism of Action
- Lenalidomide is an analogue of thalidomide with immunomodulatory, antiangiogenic, and antineoplastic properties. Lenalidomide inhibits proliferation and induces apoptosis of certain hematopoietic tumor cells including multiple myeloma, mantle cell lymphoma, and del (5q) myelodysplastic syndromes in vitro. Lenalidomide causes a delay in tumor growth in some in vivo nonclinical hematopoietic tumor models including multiple myeloma. Immunomodulatory properties of lenalidomide include activation of T cells and natural killer (NK) cells, increased numbers of NKT cells, and inhibition of pro-inflammatory cytokines (e.g., TNF-α and IL-6) by monocytes. In multiple myeloma cells, the combination of lenalidomide and dexamethasone synergizes the inhibition of cell proliferation and the induction of apoptosis.
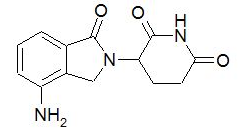
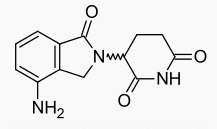
Structure
- REVLIMID, a thalidomide analogue, is an immunomodulatory agent with antiangiogenic and antineoplastic properties. The chemical name is 3-(4-amino-1-oxo 1,3-dihydro-2H-isoindol-2-yl) piperidine-2,6-dione and it has the following chemical structure:
Pharmacodynamics
- The effect of lenalidomide on the QTc interval was evaluated in 60 healthy male subjects in a randomized, thorough QT study with placebo and positive controls. At a dose two times the maximum recommended dose, lenalidomide does not prolong the QTc interval to any clinically relevant extent. The largest upper bound of the 2-sided 90% CI for the mean differences between lenalidomide and placebo was below 10 ms.
Pharmacokinetics
Absorption
- Lenalidomide is rapidly absorbed following oral administration. Following single and multiple doses of REVLIMID in patients with MM or MDS the maximum plasma concentrations occurred between 0.5 and 6 hours post-dose. The single and multiple dose pharmacokinetic disposition of lenalidomide is linear with AUC and Cmax values increasing proportionally with dose. Multiple dosing at the recommended dose-regimen does not result in drug accumulation.
- Systemic exposure (AUC) of lenalidomide in MM and MDS patients with normal or mild renal function (CLcr ≥ 60 mL/min) is approximately 60% higher as compared to young healthy male subjects.
- Administration of a single 25 mg dose of REVLIMID with a high-fat meal in healthy subjects reduces the extent of absorption, with an approximate 20% decrease in AUC and 50% decrease in Cmax. In the trials where the efficacy and safety were established for REVLIMID, the drug was administered without regard to food intake. REVLIMID can be administered with or without food.
- Population pharmacokinetic analyses show that the oral absorption rate of lenalidomide in patients with MCL is similar to that observed in patients with MM or MDS.
Distribution
- In vitro (14C)-lenalidomide binding to plasma proteins is approximately 30%.
Metabolism=
- Lenalidomide -undergoes limited metabolism. Unchanged lenalidomide is the predominant circulating component in humans. Two identified metabolites are hydroxy-lenalidomide and N-acetyl-lenalidomide; each constitutes less than 5% of parent levels in circulation.
Elimination
- Elimination is primarily renal. Following a single oral administration of [14C]-lenalidomide (25 mg) to healthy subjects, approximately 90% and 4% of the radioactive dose is eliminated within ten days in urine and feces, respectively. Approximately 82% of the radioactive dose is excreted as lenalidomide in the urine within 24 hours. Hydroxy-lenalidomide and N-acetyl-lenalidomide represent 4.59% and 1.83% of the excreted dose, respectively. The renal clearance of lenalidomide exceeds the glomerular filtration rate.
- The mean half-life of lenalidomide is 3 hours in healthy subjects and 3 to 5 hours in patients with MM, MDS or MCL.
Effect of Dexamethasone
- Co-administration of single or multiple doses of dexamethasone (40 mg) has no clinically relevant effect on the multiple dose pharmacokinetics of REVLIMID (25 mg).
Specific Populations
Patients with Renal Impairment
- The pharmacokinetics of lenalidomide were studied in patients with renal impairment due to nonmalignant conditions. In this study, 5 patients with mild renal impairment (creatinine clearance 57-74 mL/min), 6 patients with moderate renal impairment (creatinine clearance 33-46 mL/min), 6 patients with severe renal impairment (creatinine clearance 17-29 mL/min), and 6 patients with end stage renal disease requiring dialysis were administered a single oral 25-mg dose of REVLIMID. As a control group comparator, 7 healthy subjects of similar age with normal renal function (creatinine clearance 83-145 mL/min) were also administered a single oral 25-mg dose of REVLIMID. As creatinine clearance decreased from mild to severe impairment, half-life increased and drug clearance decreased linearly. Patients with moderate and severe renal impairment had a 3-fold increase in half-life and a 66% to 75% decrease in drug clearance compared to healthy subjects. Patients on hemodialysis (n=6) given a single, 25-mg dose of lenalidomide has an approximate 4.5-fold increase in half-life and an 80% decrease in drug clearance compared to healthy subjects. Approximately 40% of the administered dose was removed from the body during a single dialysis session.
- In MM patients, those patients with mild renal impairment had an AUC 56% greater than those with normal renal function.
- Adjustment of the starting dose of REVLIMID is recommended in patients with moderate or severe (CLcr < 60 mL/min) renal impairment and in patients on dialysis.
Elderly Patients
- No dedicated clinical studies have been conducted to evaluate pharmacokinetics of lenalidomide in the elderly. Population pharmacokinetic analyses included patients with ages ranging from 39 to 85 years old and show that age does not influence the disposition of lenalidomide.
Patients with Hepatic Disease
- Population pharmacokinetic analyses included patients with mild hepatic impairment (N = 16, total bilirubin >1 to ≤ 1.5 x ULN or AST > ULN) and show that mild hepatic impairment does not influence the disposition of lenalidomide. There are no data available for patients with moderate to severe hepatic impairment.
Pediatric
- No pharmacokinetic data are available in patients below the age of 18 years.
Other Intrinsic Factors
- Population pharmacokinetic analyses show that body weight (33-135 kg), gender, race, and type of hematological malignancies (MM, MDS or MCL) do not have a clinically relevant effect on lenalidomide clearance in adult patients.
Nonclinical Toxicology
Carcinogenesis, mutagenesis, impairment of fertility
- Carcinogenicity studies with lenalidomide have not been conducted.
- Lenalidomide was not mutagenic in the bacterial reverse mutation assay (Ames test) and did not induce chromosome aberrations in cultured human peripheral blood lymphocytes, or mutations at the thymidine kinase (tk) locus of mouse lymphoma L5178Y cells. Lenalidomide did not increase morphological transformation in Syrian Hamster Embryo assay or induce micronuclei in the polychromatic erythrocytes of the bone marrow of male rats.
- A fertility and early embryonic development study in rats, with administration of lenalidomide up to 500 mg/kg (approximately 200 times the human dose of 25 mg, based on body surface area) produced no parental toxicity and no adverse effects on fertility.
Clinical Studies
Multiple Myeloma
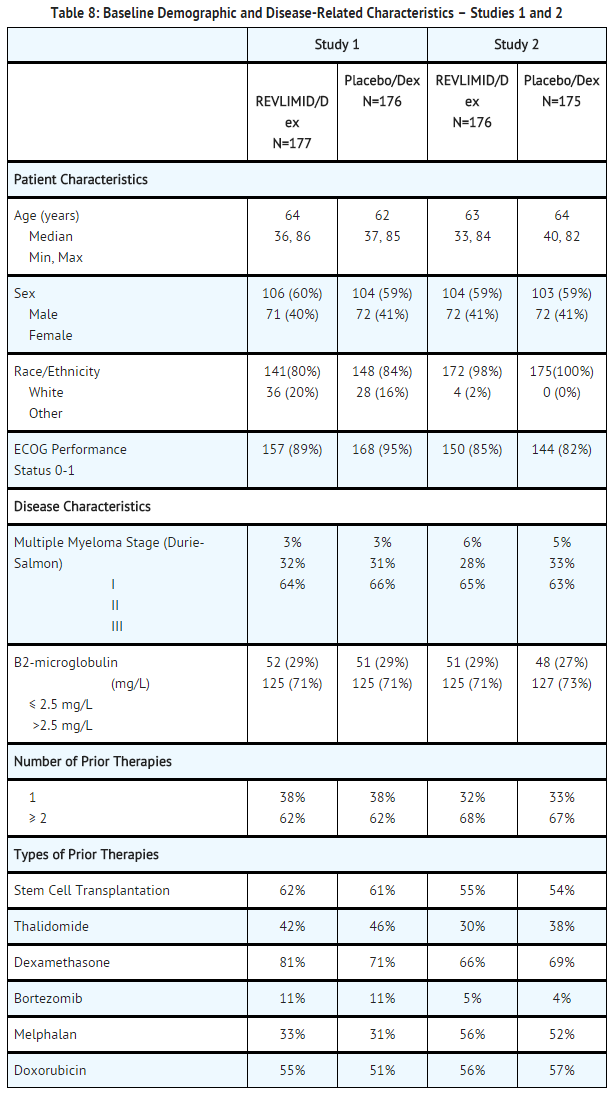
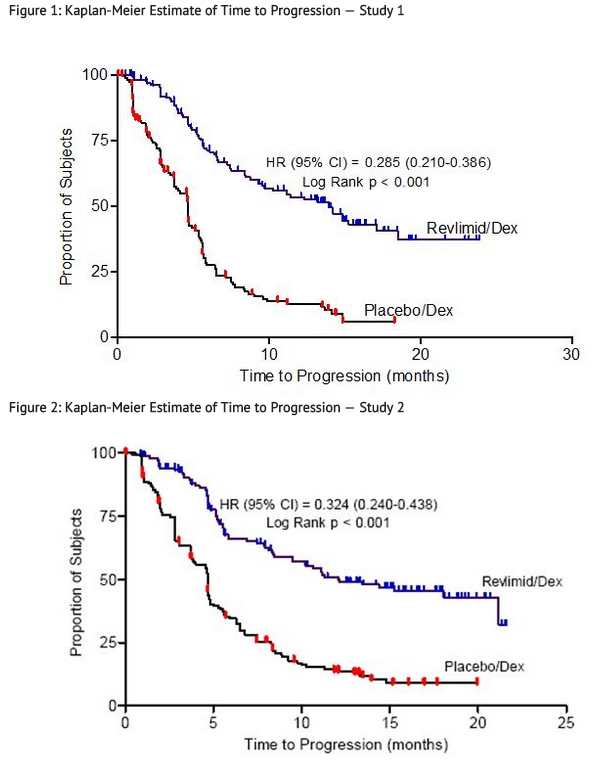
- Two randomized studies (Studies 1 and 2) were conducted to evaluate the efficacy and safety of REVLIMID. These multicenter, multinational, double-blind, placebo-controlled studies compared REVLIMID plus oral pulse high-dose dexamethasone therapy to dexamethasone therapy alone in patients with multiple myeloma who had received at least one prior treatment. These studies enrolled patients with absolute neutrophil counts (ANC) ≥ 1000/mm3, platelet counts ≥ 75,000/mm3, serum creatinine ≤ 2.5 mg/dL, serum SGOT/AST or SGPT/ALT ≤ 3 x upper limit of normal (ULN), and serum direct bilirubin ≤ 2 mg/dL
- In both studies, patients in the REVLIMID/dexamethasone group took 25 mg of REVLIMID orally once daily on Days 1 to 21 and a matching placebo capsule once daily on Days 22 to 28 of each 28-day cycle. Patients in the placebo/dexamethasone group took 1 placebo capsule on Days 1 to 28 of each 28-day cycle. Patients in both treatment groups took 40 mg of dexamethasone orally once daily on Days 1 to 4, 9 to 12, and 17 to 20 of each 28-day cycle for the first 4 cycles of therapy.
- The dose of dexamethasone was reduced to 40 mg orally once daily on Days 1 to 4 of each 28-day cycle after the first 4 cycles of therapy. In both studies, treatment was to continue until disease progression.
- In both studies, dose adjustments were allowed based on clinical and laboratory findings. Sequential dose reductions to 15 mg daily, 10 mg daily and 5 mg daily were allowed for toxicity [see Dosage and Administration (2.1)].
- Table 8 summarizes the baseline patient and disease characteristics in the two studies. In both studies, baseline demographic and disease-related characteristics were comparable between the REVLIMID/dexamethasone and placebo/dexamethasone groups.
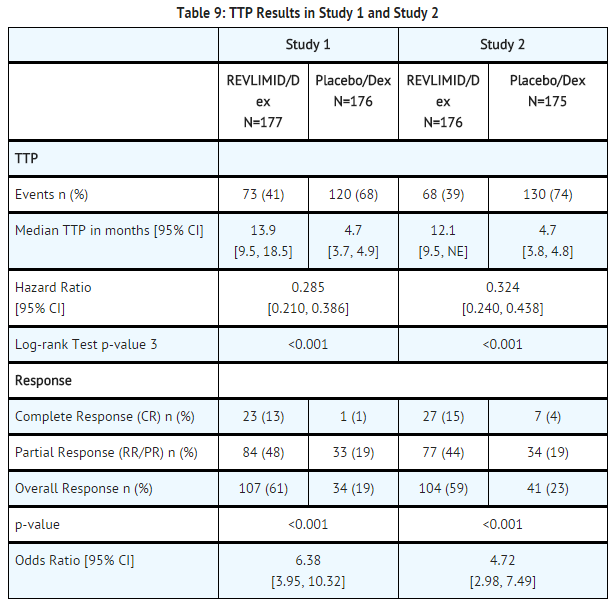
- The primary efficacy endpoint in both studies was time to progression (TTP). TTP was defined as the time from randomization to the first occurrence of progressive disease.
- Preplanned interim analyses of both studies showed that the combination of REVLIMID/dexamethasone was significantly superior to dexamethasone alone for TTP. The studies were unblinded to allow patients in the placebo/dexamethasone group to receive treatment with the REVLIMID/dexamethasone combination. For both studies, the extended follow-up survival data with crossovers were analyzed. In study 1, the median survival time was 39.4 months (95%CI: 32.9, 47.4) in REVLIMID/dexamethasone group and 31.6 months (95%CI: 24.1, 40.9) in placebo/dexamethasone group, with a hazard ratio of 0.79 (95% CI: 0.61-1.03). In study 2, the median survival time was 37.5 months (95%CI: 29.9, 46.6) in REVLIMID/dexamethasone group and 30.8 months (95%CI: 23.5, 40.3) in placebo/dexamethasone group, with a hazard ratio of 0.86 (95% CI: 0.65-1.14).
Myelodysplastic Syndromes (MDS) with a Deletion 5q Cytogenetic Abnormality
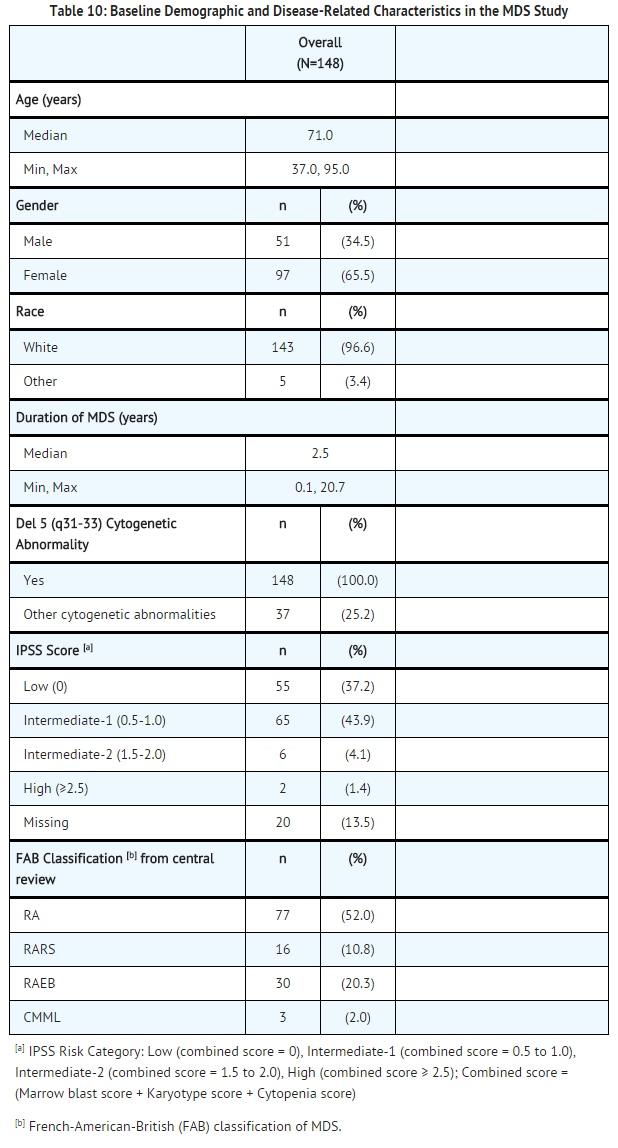
- The efficacy and safety of REVLIMID were evaluated in patients with transfusion-dependent anemia in low- or intermediate-1- risk MDS with a 5q (q31-33) cytogenetic abnormality in isolation or with additional cytogenetic abnormalities, at a dose of 10 mg once daily or 10 mg once daily for 21 days every 28 days in an open-label, single-arm, multi-center study. The major study was not designed nor powered to prospectively compare the efficacy of the 2 dosing regimens. Sequential dose reductions to 5 mg daily and 5 mg every other day, as well as dose delays, were allowed for toxicity.
- This major study enrolled 148 patients who had RBC transfusion dependent anemia. RBC transfusion dependence was defined as having received ≥ 2 units of RBCs within 8 weeks prior to study treatment. The study enrolled patients with absolute neutrophil counts (ANC) ≥ 500/mm3, platelet counts ≥ 50,000/mm3, serum creatinine ≤ 2.5 mg/dL, serum SGOT/AST or SGPT/ALT ≤ 3 x upper limit of normal (ULN), and serum direct bilirubin ≤ 2 mg/dL. Granulocyte colony-stimulating factor was permitted for patients who developed neutropenia or fever in association with neutropenia. Baseline patient and disease-related characteristics are summarized in Table 10.
- The frequency of RBC transfusion independence was assessed using criteria modified from the International Working Group (IWG) response criteria for MDS. RBC transfusion independence was defined as the absence of any RBC transfusion during any consecutive “rolling” 56 days (8 weeks) during the treatment period.
- Transfusion independence was seen in 99/148 (67%) patients (95% CI [59, 74]). The median duration from the date when RBC transfusion independence was first declared (i.e., the last day of the 56-day RBC transfusion-free period) to the date when an additional transfusion was received after the 56-day transfusion-free period among the 99 responders was 44 weeks (range of 0 to >67 weeks). Ninety percent of patients who achieved a transfusion benefit did so by completion of three months in the study.
- RBC transfusion independence rates were unaffected by age or gender.
- The dose of REVLIMID was reduced or interrupted at least once due to an adverse event in 118 (79.7%) of the 148 patients; the median time to the first dose reduction or interruption was 21 days (mean, 35.1 days; range, 2-253 days), and the median duration of the first dose interruption was 22 days (mean, 28.5 days; range, 2-265 days). A second dose reduction or interruption due to adverse events was required in 50 (33.8%) of the 148 patients. The median interval between the first and second dose reduction or interruption was 51 days (mean, 59.7 days; range, 15-205 days) and the median duration of the second dose interruption was 21 days (mean, 26 days; range, 2-148 days).
Mantle Cell Lymphoma
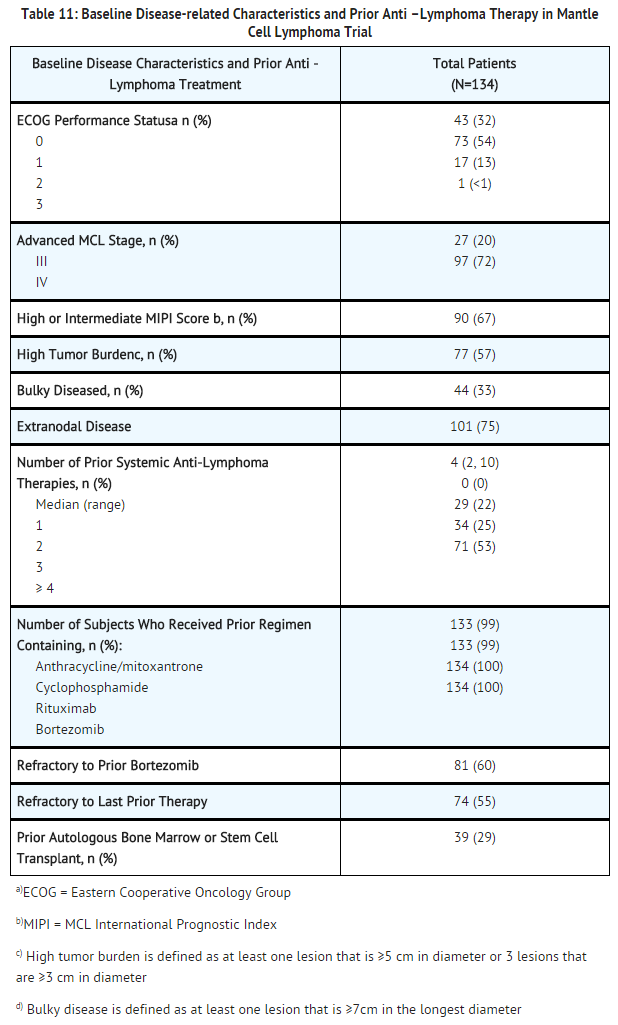
- A multicenter, single-arm, open-label trial of single-agent lenalidomide was conducted to evaluate the safety and efficacy of lenalidomide in patients with mantle cell lymphoma who have relapsed after or were refractory to bortezomib or a bortezomib-containing regimen. Patients with a creatinine clearance >60 mL/min were given lenalidomide at a dose of 25 mg once daily for 21 days every 28 days. Patients with a creatinine clearance ≥30 mL/min and <60 mL/min were given lenalidomide at a dose of 10 mg once daily for 21 days every 28 days. Treatment was continued until disease progression, unacceptable toxicity, or withdrawal of consent.
- The trial included patients who were at least 18 years of age with biopsy-proven MCL with measurable disease by CT scan. Patients were required to have received prior treatment with an anthracycline or mitoxantrone, cyclophosphamide, rituximab, and bortezomib, alone or in combination. Patients were required to have documented refractory disease (defined as without any response of PR or better during treatment with bortezomib or a bortezomib-containing regimen), or relapsed disease (defined as progression within one year after treatment with bortezomib or a bortezomib-containing regimen). At enrollment patients were to have an absolute neutrophil counts (ANC) ≥1500/ mm3, platelet counts ≥ 60,000/mm3, serum SGOT/AST or SGPT/ALT ≤3x upper limit of normal (ULN) unless there was documented evidence of liver involvement by lymphoma, serum total bilirubin ≤1.5 x ULN except in cases of Gilbert’s syndrome or documented liver involvement by lymphoma, and calculated creatinine clearance (Cockcroft-Gault formula) ≥30 mL/min.
- The median age was 67 years (43-83), 81% were male and 96% were Caucasian. The table below summarizes the baseline disease-related characteristics and prior anti-lymphoma therapy in the Mantle Cell Lymphoma trial.
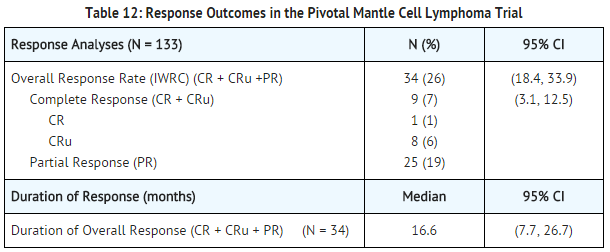
- The efficacy endpoints in the MCL trial were overall response rate (ORR) and duration of response (DOR). Response was determined based on review of radiographic scans by an independent review committee according to a modified version of the International Workshop Lymphoma Response Criteria (Cheson, 1999). The DOR is defined as the time from the initial response (at least PR) to documented disease progression. The efficacy results for the MCL population were based on all evaluable patients who received at least one dose of study drug and are presented in Table 12. The median time to response was 2.2 months (range 1.8 to 13 months).
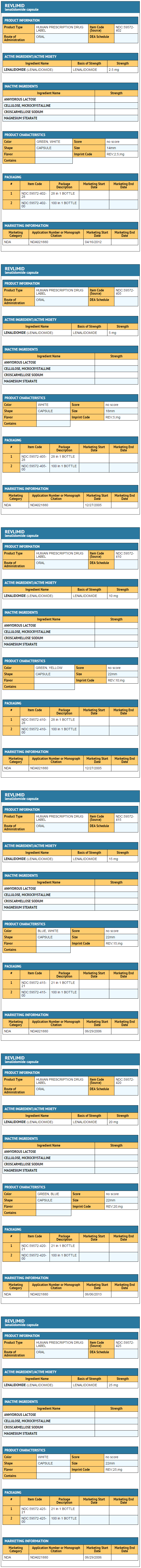
How Supplied
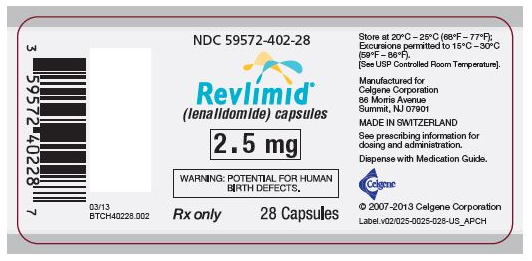
- White and blue-green opaque hard capsules imprinted “REV” on one half and “2.5 mg” on the other half in black ink:
- 2.5 mg bottles of 28 (NDC 59572-402-28)
- 2.5 mg bottles of 100 (NDC 59572-402-00)
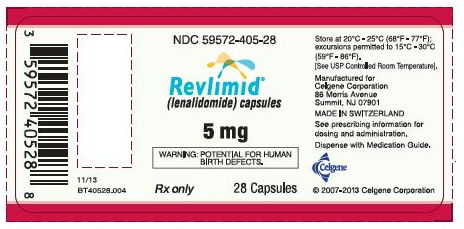
- White opaque capsules imprinted “REV” on one half and “5 mg” on the other half in black ink:
- 5 mg bottles of 28 (NDC 59572-405-28)
- 5 mg bottles of 100 (NDC 59572-405-00)
- Blue/green and pale yellow opaque capsules imprinted “REV” on one half and “10 mg” on the other half in black ink:
- 10 mg bottles of 28 (NDC 59572-410-28)
- 10 mg bottles of 100 (NDC 59572-410-00)
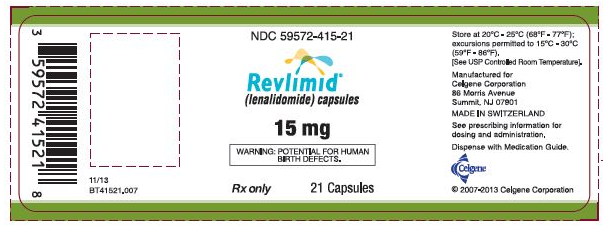
- Powder blue and white opaque capsules imprinted “REV” on one half and “15 mg” on the other half in black ink:
- 15 mg bottles of 21 (NDC 59572-415-21)
- 15 mg bottles of 100 (NDC 59572-415-00)
- Powder blue and blue-green opaque hard capsules imprinted “REV” on one half and “20 mg” on the other half in black ink.
- 20 mg bottles of 21 (NDC 59572-420-21)
- 20 mg bottles of 100 (NDC 59572-420-00)
- White opaque capsules imprinted “REV” on one half and “25 mg” on the other half in black ink:
- 25 mg bottles of 21 (NDC 59572-425-21)
- 25 mg bottles of 100 (NDC 59572-425-00)
Storage
- Store at 20°C - 25°C (68°F - 77°F); excursions permitted to 15°C - 30°C (59°F - 86°F) [See USP Controlled Room Temperature].
Handling and Disposal
- Care should be exercised in the handling of REVLIMID. REVLIMID capsules should not be opened or crushed. If powder from REVLIMID contacts the skin, wash the skin immediately and thoroughly with soap and water. If REVLIMID contacts the mucous membranes, flush thoroughly with water.
- Procedures for the proper handling and disposal of anticancer drugs should be considered. Several guidelines on the subject have been published.1
- Dispense no more than a 28-day supply.
Images
Drug Images
{{#ask: Page Name::Lenalidomide |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
Revlimid (lenalidomide) Capsules, 2.5 mg - 28 Count Bottle
Revlimid (lenalidomide) Capsules, 5 mg - 28 Count Bottle
Revlimid (lenalidomide) Capsules, 10 mg - 28 Count Bottle
Revlimid (lenalidomide) Capsules, 15 mg - 21 Count Bottle
Revlimid (lenalidomide) Capsules, 20 mg - 21 Count Bottle
Revlimid (lenalidomide) Capsules, 25 mg - 21 Count Bottle
Ingredients and Appearance
{{#ask: Label Page::Lenalidomide |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Embryo-Fetal Toxicity
- Advise patients that REVLIMID is contraindicated in pregnancy. REVLIMID is a thalidomide analog and can cause serious birth defects or death to a developing baby.
- Advise females of reproductive potential that they must avoid pregnancy while taking REVLIMID and for at least 4 weeks after completing therapy.
Initiate REVLIMID treatment in females of reproductive potential only following a negative pregnancy test.
- Advise females of reproductive potential of the importance of monthly pregnancy tests and the need to use two different forms of contraception including at least one highly effective form simultaneously during REVLIMID therapy, during dose interruption and for 4 weeks after she has completely finished taking REVLIMID. Highly effective forms of contraception other than tubal ligation include IUD and hormonal (birth control pills, injections, patch or implants) and a partner’s vasectomy. Additional effective contraceptive methods include latex or synthetic condom, diaphragm and cervical cap.
- Instruct patient to immediately stop taking REVLIMID and contact her doctor if she becomes pregnant while taking this drug, if she misses her menstrual period, or experiences unusual menstrual bleeding, if she stops taking birth control, or if she thinks FOR ANY REASON that she may be pregnant.
- Advise patient that if her doctor is not available, she can call 1-888-668-2528 for information on emergency contraception.
- Advise males to always use a latex or synthetic condom during any sexual contact with females of reproductive potential while taking REVLIMID and for up to 28 days after discontinuing REVLIMID, even if they have undergone a successful vasectomy.
- Advise male patients taking REVLIMID that they must not donate sperm.
All patients must be instructed to not donate blood while taking REVLIMID, during dose interruptions and for 1 month following discontinuation of REVLIMID.
REVLIMID REMS™ program
- Because of the risk of embryo-fetal toxicity, REVLIMID is only available through a restricted program called the REVLIMID REMS™ program (formerly known as the “RevAssist®” program).
- Patients must sign a Patient-Physician agreement form and comply with the requirements to receive REVLIMID. In particular, females of reproductive potential must comply with the pregnancy testing, contraception requirements and participate in monthly telephone surveys. Males must comply with the contraception requirements.
- REVLIMID is available only from pharmacies that are certified in REVLIMID REMS™ program. Provide patients with the telephone number and website for information on how to obtain the product.
Hematologic Toxicity
- Inform patients that REVLIMID is associated with significant neutropenia and thrombocytopenia.
Venous and Arterial Thromboembolism
- Inform patients of the risk of thrombosis including DVT, PE, MI, and stroke and to report immediately any signs and symptoms suggestive of these events for evaluation.
Increased Mortality in Patients with CLL
- Inform patients that REVLIMID had increased mortality in patients with CLL and serious adverse cardiovascular reactions, including atrial fibrillation, myocardial infarction, and cardiac failure [see Warning and Precautions (5.5)].
Second Primary Malignancies
- Inform patients of the potential risk of developing second primary malignancies during treatment with REVLIMID.
Hepatotoxicity
- Inform patients of the risk of hepatotoxicity, including hepatic failure and death, and to report any signs and symptoms associated with this event to their healthcare provider for evaluation.
Allergic Reactions
- Inform patients of the potential for allergic reactions including hypersensitivity, angioedema, Stevens Johnsons Syndrome, or toxic epidermal necrolysis if they had such a reaction to THALOMID and report symptoms associated with these events to their healthcare provider for evaluation.
Tumor Lysis Syndrome
- Inform patients of the potential risk of tumor lysis syndrome and to report any signs and symptoms associated with this event to their healthcare provider for evaluation.
Tumor Flare Reaction
- Inform patients of the potential risk of tumor flare reaction and to report any signs and symptoms associated with this event to their healthcare provider for evaluation.
Dosing Instructions
- Inform patients to take REVLIMID once daily at about the same time each day, either with or without food. The capsules should not be opened, broken, or chewed. REVLIMID should be swallowed whole with water.
- Instruct patients that if they miss a dose of REVLIMID, they may still take it up to 12 hours after the time they would normally take it. If more than 12 hours have elapsed, they should be instructed to skip the dose for that day. The next day, they should take REVLIMID at the usual time. Warn patients to not take 2 doses to make up for the one that they missed.
Precautions with Alcohol
- Alcohol-Lenalidomide interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Revlimid®[7]
Look-Alike Drug Names
There is limited information regarding Lenalidomide Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ Ferrajoli A, Lee BN, Schlette EJ, O'Brien SM, Gao H, Wen S; et al. (2008). "Lenalidomide induces complete and partial remissions in patients with relapsed and refractory chronic lymphocytic leukemia". Blood. 111 (11): 5291–7. doi:10.1182/blood-2007-12-130120. PMC 4082321. PMID 18334676.
- ↑ Chanan-Khan A, Miller KC, Musial L, Lawrence D, Padmanabhan S, Takeshita K; et al. (2006). "Clinical efficacy of lenalidomide in patients with relapsed or refractory chronic lymphocytic leukemia: results of a phase II study". J Clin Oncol. 24 (34): 5343–9. doi:10.1200/JCO.2005.05.0401. PMID 17088571.
- ↑ Zonder JA, Crowley J, Hussein MA, Bolejack V, Moore DF, Whittenberger BF; et al. (2010). "Lenalidomide and high-dose dexamethasone compared with dexamethasone as initial therapy for multiple myeloma: a randomized Southwest Oncology Group trial (S0232)". Blood. 116 (26): 5838–41. doi:10.1182/blood-2010-08-303487. PMC 3031379. PMID 20876454.
- ↑ Benboubker L, Dimopoulos MA, Dispenzieri A, Catalano J, Belch AR, Cavo M; et al. (2014). "Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma". N Engl J Med. 371 (10): 906–17. doi:10.1056/NEJMoa1402551. PMID 25184863.
- ↑ Jabbour E, Thomas D, Kantarjian H, Zhou L, Pierce S, Cortes J; et al. (2011). "Comparison of thalidomide and lenalidomide as therapy for myelofibrosis". Blood. 118 (4): 899–902. doi:10.1182/blood-2010-12-325589. PMC 4186644. PMID 21622644.
- ↑ Wiernik PH, Lossos IS, Tuscano JM, Justice G, Vose JM, Cole CE; et al. (2008). "Lenalidomide monotherapy in relapsed or refractory aggressive non-Hodgkin's lymphoma". J Clin Oncol. 26 (30): 4952–7. doi:10.1200/JCO.2007.15.3429. PMID 18606983.
- ↑ "Lenalidomide".