Heart sounds
| Heart sounds | |
 | |
|---|---|
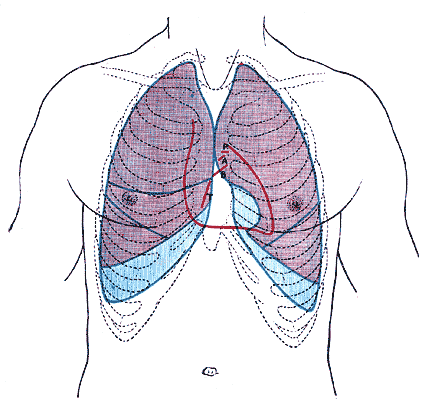
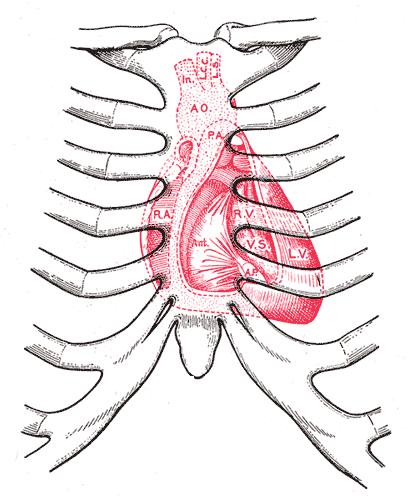
| Front of thorax, showing surface relations of bones, lungs (purple), pleura (blue), and heart (red outline). Heart valves are labeled with "B", "T", "A", and "P". First heart sound: caused by atrioventricular valves - Bicuspid/Mitral (B) and Tricuspid (T). Second heart sound caused by semilunar valves -- Aortic (A) and Pulmonary/Pulmonic (P). |
|
WikiDoc Resources for Heart sounds |
|
Articles |
|---|
|
Most recent articles on Heart sounds Most cited articles on Heart sounds |
|
Media |
|
Powerpoint slides on Heart sounds |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Heart sounds at Clinical Trials.gov Clinical Trials on Heart sounds at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Heart sounds
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Heart sounds Discussion groups on Heart sounds Patient Handouts on Heart sounds Directions to Hospitals Treating Heart sounds Risk calculators and risk factors for Heart sounds
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Heart sounds |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Overview
The heart sounds are the noises (sound) generated by the beating heart and the resultant flow of blood through it. This is also called a heartbeat. In cardiac auscultation, an examiner uses a stethoscope to listen for these sounds, which provide important information about the condition of the heart.
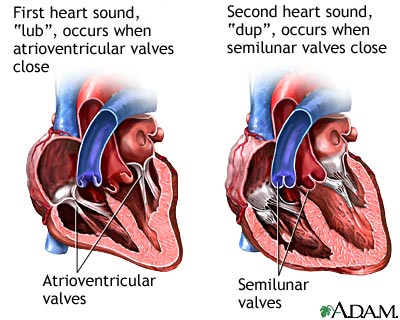
In healthy adults, there are two normal heart sounds often described as a lub and a dub (or dup), that occur in sequence with each heart beat. These are the first heart sound (S1) and second heart sound (S2), produced by the closure of the AV valves and semilunar valves respectively. In addition to these normal sounds, a variety of other sounds may be present including heart murmurs and adventitious sounds.
Heart murmurs are generated by turbulent flow of blood, which may occur inside or outside the heart. Murmurs may be physiological (benign) or pathological (abnormal). Abnormal murmurs can be caused by stenosis restricting the opening of a heart valve, causing turbulence as blood flows through it. Valve insufficiency (or regurgitation) allows backflow of blood when the incompetent valve is supposed to be closed. Different murmurs are audible in different parts of the cardiac cycle, depending on the cause of the murmur.
Normal heart sounds
{{#ev:youtube|xS3jX1FYG-M}}
{{#ev:youtube|NeMJXMSkA7g}}
First heart tone S1, the "lub"(components M1 and T1)
The first heart tone, or S1, is caused by the sudden block of reverse blood flow due to closure of the atrioventricular valves, mitral and tricuspid, at the beginning of ventricular contraction, or systole. When the pressure in the ventricles rises above the pressure in the atria, venous blood flow entering the ventricles is pushed back toward the atria, catching the valve leaflets, closing the inlet valves and preventing regurgitation of blood from the ventricles back into the atria. The S1 sound results from reverberation within the blood associated with the sudden block of flow reversal by the valves. [1]
Second heart tone S2 the "dub"(components A2 and P2)
The second heart tone, or S2, is caused by the sudden block of reversing blood flow due to closure of the aortic valve and pulmonary valve at the end of ventricular systole, i.e beginning of ventricular diastole. As the left ventricle empties, its pressure falls below the pressure in the aorta, aortic blood flow quickly reverses back toward the left ventricle, catching the aortic valve leaflets and is stopped by aortic (outlet) valve closure. Similarly, as the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonary (outlet) valve closes. The S2 sound results from reverberation within the blood associated with the sudden block of flow reversal.
Splitting of the second heart sound
{{#ev:youtube|5tBk1XuEyuM}}
Physiologic Splitting
During inspiration, negative intrathoracic pressure causes increased blood return into the right side of the heart, yet some slowing of emptying from the left side. The increased blood volume in the right ventricle causes the pulmonary valve to stay open longer during ventricular systole. This causes an increased delay in the P2 component of S2 relative to the A2 component. This is defined as physiologic splitting of S2. During expiration, the positive intrathoracic pressure causes decreased blood return to the right side of the heart. The reduced volume in the right ventricle allows the pulmonary valve to close earlier at the end of ventricular systole, causing P2 to occur earlier, and "closer" to A2. It is physiological to hear a "splitting" of the second heart tone in younger people, during inspiration and in the "pulmonary area", i.e. the 2nd ICS (intercostal space) at the left edge of the sternum. During expiration, the interval between the two components normally shortens and the S2 sounds becomes merged.
Persistent Splitting
Persistent splitting of S2 is seen in right bundle branch block (RBBB) and pulmonary hypertension. Because of the delayed activation of the right heart in RBBB the pulmonary valve closure is delayed causing a split in the second heart sound which is persistent in both inspiration and expiration.
Paradoxical Splitting
This phenomenon is seen in left bundle branch block (LBBB), aortic stenosis, severe heart failure and hypertrophic cardiomyopathy. Delayed activation of the left ventricle and in turn delayed closure of the aortic valve causes the pulmonic component of the second heart sound to occur before the aortic component. This split is better appreciated while expiration than during inspiration.
Fixed Splitting
If this splitting does not vary with inspiration, it is termed "fixed split S2" and is usually due to an atrial septal defect (ASD) or ventricular septal defect (VSD). The ASD or VSD creates a left to right shunt that increases the blood flow to the right side of the heart, thereby causing the pulmonic valve to close later than the aortic valve independent of inspiration/expiration.
Loud P2
Pulmonary hypertension is the most common cause of a loud P2. When the pulmonary artery pressures are more than 50 mm Hg a loud pulmonic component of S2 is heard in the left second intercostal space (pulmonic area). Pulmonary hypertension is also a caiuse of persistent splitting of S2.
Extra heart sounds
Infrequently extra heart sounds are heard in both normal and abnormal situations. A gallop rhythm refers to a (usually abnormal) rhythm of the heart on auscultation. The normal heart rhythm contains two audible sounds, called S1 and S2, giving the well-known "lub-dub" rhythm. They are caused by the closing of valves in the heart. A gallop rhythm contains another sound, called S3 or S4, dependent upon where in the cycle this added sound comes; it can also contain both of these sounds.
Third heart sound S3
Rarely, there may be a third heart sound S3. S3 (or third heart sound) is the name of the vibration which occurs during early diastole, shortly after the second heart sound S2, giving a rhythm much like the cadence in the word 'Kentucky'. It can be a normal finding in people under 40 years of age, but over this age is usually a sign of heart failure. It is usually low-pitched and difficult to hear, and is best heard with the bell of the stethoscope. An S3 rhythm is also known as ventricular gallop. The third heart sound or protodiastolic sound is not of valvular origin, as it occurs at the beginning of diastole just after S2. This sound occurs when the left ventricle is not very compliant, and at the beginning of diastole the rush of blood into the left ventricle suddenly is halted, resulting in a vibration of the ventricle and surrounding structures.
The third heart sound is normal in children and young adults, but disappears before middle age. Abnormal reemergence of this sound late in life indicates a pathological state, often a sign of a failing left ventricle as in dilated congestive heart failure (CHF). This sound is called a protodiastolic gallop or ventricular gallop, a type of gallop rhythm.
Pathophysiology and Etiology
It is caused by the sudden slowing of blood rushing in from the atrium into the ventricle as it is relaxing.
Differential Diagnosis of Causes of an S3
It is associated with heart failure, caused by conditions which have:
Rapid ventricular filling
- Mitral regurgitation - this is when one of the heart valves that usually stops blood going from the left ventricle to the left atria fails, allowing blood into the atria during systole. This means they will be overfilled when they come to contract, leading to the rapid ventricular filling.
- Elevated left atrial and left ventricular filling pressures, usually a result of a stiffened and dilated left ventricle
- Ventricular septal defect - this is a hole in the wall between the two ventricles, which allows rapid filling from the other ventricle.
- Elevated atrial pressure
- High-output states
Poor Left Ventricular Function
- Post-MI - the death of tissue in the ventricular wall due to loss of blood supply causes areas which do not move as well, if at all (hypokinetic and akinetic), meaning they do not relax quickly enough so the ventricular filling is relatively too quick.
- Dilated cardiomyopathy - the ventricular walls are abnormal for a variety of reasons, and become thin and stiff so do not relax well.
- Hypertrophic obstructive cardiomyopathy
- Cardiomegaly of a variety of causes
In conditions affecting the pericardium or diseases that primarily affect the heart muscle (restrictive cardiomyopathies) a similar sound can be heard, but is usually more high-pitched and is called a 'pericardial knock'.
The S3 can also be confused with a widely split S2, or a mitral opening snap, but these sounds are typically of much higher pitch and occur closer to the onset of S2.
Treatment
The gallop rhythm itself does not need to be treated; the underlying cause requires correction; depending on the etiology the gallop rhythm may resolve following treatment.
Fourth heart sound S4
S4 (or fourth heart sound) occurs just before S1 (thus right at the end of one whole cycle), giving a cadence like the word 'Tennessee'. It is never normal. If the problem lies with the left ventricle, the gallop rhythm will be heard best at the cardiac apex (the point of the two ventricles). It will become more apparent with exercise, with the patient lying on their left-hand side, or with the patient holding expiration. If the culprit is the right ventricle, the abnormal rhythm will be most evident on the lower left hand side of the sternum, and will get louder with exercise and quick, deep inspiration [2]. The fourth heart sound S4 is sometimes audible in healthy children, but when audible in an adult is called a presystolic gallop or atrial gallop. This gallop is a sign of a pathologic state, usually a failing left ventricle. This sound occurs just after atrial contraction ("atrial kick") and is the sound of blood being forced into a stiff/hypertrophic left ventricle. The combined presence of S3 and S4 is a quadruple gallop. At rapid heart rates, S3 and S4 may merge to produce a summation gallop.
Pathophysiology and Etiology
It is caused by the atria contracting forcefully in an effort to overcome an abnormally-stiff ventricle.
Differential Diagnosis of Causes of an S4
The S4 rhythm is associated with disorders that increases the stiffness of the ventricle, including:
- Long-standing hypertension
- Aortic stenosis
- Overload of the ventricle
- Fibrosis of the ventricle
- Left ventricular hypertrophy
- Coronary Artery Disease
- Hypertrophic Cardiomyopathy
- Pulmonary Hypertension
Treatment
Again, the rhythm itself does not require treatment; the underlying cause of ventricular stiffness or dysfunction does.
If a fast heart rate (tachycardia) is present along and S3 and S4 both occur, the rate may become high enough so that the distinction between the two sounds is lost, and they summate into a single sound.
Abnormal sounds
Aortic area, pulmonic area, tricuspid area and mitral area are the area where we auscultate the heart. Heart murmurs are produced as a result of turbulent flow of blood, turbulence sufficient to produce audible noise. They usually are heard as a whooshing sound. The term murmur only refers to a sound believed to originating within blood flow through or near the heart; rapid blood velocity is necessary to produce a murmur. Though not fully reliable, soft murmurs are less likely to reflect a serious, if any, health problem; loud murmurs essentially always reflect a problem. Yet most heart problems do not produce any murmur and most valve problems also do not produce an audible murmur.
The following paragraphs overview the murmurs most commonly heard in adults, adults who do not have major congenital heart abnormalities.
- Regurgitation through the mitral valve is by far the most commonly heard murmur, sometimes fairly loud to a practiced ear, even though the volume of regurgitant blood flow may be quite small. Yet, though often obvious, probably about 20% of cases of mitral regurgitation, though obvious using echocardiography visualization, do not produce an audible murmur.
- Stenosis of the aortic valve is typically the next most commonly heart murmur, a systolic ejection murmur. This is more common in older adults or in those individuals having a two, not a three leaflet aortic valve.
- Regurgitation through the aortic valve, if marked, is sometimes audible to a practiced ear with a high quality, especially electronically amplified, stethoscope. Generally, this is a very rarely heard murmur, even though aortic valve regurgitation is not so rare. Aortic regurgition, though obvious using echocardiography visualization, usually does not produce an audible murmur.
- Stenosis of the mitral valve, if severe, also rarely produces an audible, low frequency soft rumbling murmur, best recognized by a practiced ear using a high quality, especially electronically amplified, stethoscope.
- Either regurgitation through, or stenosis of, the tricuspid or pulmonary valves essentially never produces audible murmurs.
- Other audible murmurs are associated with abnormal openings between the left ventricle and right heart or from the aortic or pulmonary arteries back into a lower pressure heart chamber.
| Gradations of Murmurs[3] | |
|---|---|
| Grade | Description |
| Grade 1 | Very faint, heard only after listener has "tuned in"; may not be heard in all positions. |
| Grade 2 | Quiet, but heard immediately after placing the stethoscope on the chest. |
| Grade 3 | Moderately loud. |
| Grade 4 | Loud, with palpable thrill. |
| Grade 5 | Very loud, with thrill. May be heard when stethoscope is partly off the chest. |
| Grade 6 | Very loud, with thrill. May be heard with stethoscope entirely off the chest. |
As noted, several different cardiac conditions can cause heart murmurs. However, the murmurs produced often change in complex ways with the severity of the cardiac disease. An astute physician can sometimes diagnose cardiac conditions with some accuracy based largely on the murmur, related physical examination and experience with the relative frequency of different heart conditions. However, with the advent of better quality and wider availability of echocardiography and other techniques, heart status can be recognized and quantified much more accurately than formerly possible with only a stethoscope, examination and experience.
Clicks: With the advent of newer, non-invasive imaging techniques, the origin of other, so-called adventitial sounds or "clicks" has been appreciated. These are short, high-pitched sounds. There are two types of clicks, ejection click and non-ejection click.
- Ejection clicks are caused by bicuspid aortic valve and bicuspid pulmonary valve early in the systole.
- Non-ejection clicks are seen in mitral valve prolapse, ventricular septal aneurysm, atrial septal aneurysm, cardiac tumors, pulmonary hypertension and systemic hypertension. Patients with mitral valve prolapse may have a mid-systolic click along with a murmur.
- The atrioventricular valves of patients with mitral stenosis may open with an opening snap on the beginning of diastole.
Rubs: Patients with pericarditis, an inflammation of the sac surrounding the heart (pericardium), may have an audible pericardial friction rub. This is a characteristic scratching, creaking, high-pitched sound emanating from the rubbing of both layers of inflammated pericardium. It is the loudest in systole, but can often be heard also at the beginning and at the end of diastole. It is very dependent on body position and breathing, and changes from hour to hour.
There are a number of interventions that can be performed that alter the intensity and characteristics of abnormal heart sounds. These interventions can be performed to differentiate the different heart sounds and obtain a diagnosis of the cardiac anomaly that causes the heart sound. (See Heart murmur#Interventions that change murmur sounds.)
Inhalation pressure also causes an increase in the venous blood return to the right side of the heart. Therefore, right-sided murmurs generally increase in intensity with inspiration. The increased volume of blood entering the right sided chambers of the heart restricts the amount of blood entering the left sided chambers of the heart. This causes left-sided murmurs to generally decrease in intensity during inspiration.
With expiration, the opposite haemodynamic changes occur. This means that left-sided murmurs generally increase in intensity with expiration. Having the patient lie supine and raising their legs up to a 45 degree angle facilitates an increase in venous return to the right side of the heart producing effects similar to inhalation-increased blood flow.
Surface anatomy
The opening and closing of the valves is usually much less loud than the sound of the blood rushing through the valve and "colliding" with the subsequent barrier. Because of this, auscultation to determine function of a valve is usually not performed at the position of the valve, but at a downstream position where the listener can best hear the blood colliding after the valve is closed.
| Pulmonary valve (to pulmonary trunk) | second intercostal space | left upper sternal border |
| Aortic valve (to aorta) | second intercostal space | right upper sternal border |
| Mitral valve (to left ventricle) | fifth intercostal space | lateral to left midclavicular line |
| Tricuspid valve (to right ventricle) | fourth intercostal space | lower left sternal border |
One can remember the positions of the sounds by the mnemonic "All The Presidents Men". [3]
- A - Aortic - Right second intercostal space
- T - Tricuspid - Left fourth intercostal space sternal border
- P - Pulmonic - Left second intercostal space sternal border
- M - Mitral - Fifth intercostal space lateral to left midclavicular line
Recording heart sounds
With the advent of electronic stethoscopes, it is now possible to conveniently record heart sounds. One electronic stethoscope provides a port to output stethoscope sounds to an external recording device, such as a notebook computer or MP3 recorder. The same connection can then be used to listen to the recordings through the stethoscope headphones, allowing for faithful reproduction of low-frequency murmurs and other heart sounds.
Related Chapters
- Physical examination
- Precordial examination
- Anatomy
- Pathophysiology
- Heart murmur
- Benign paediatric heart murmur
- Pulsatile Tinnitus - hearing a heartbeat sound in one or both ears
References
- ↑ "The Cardiovascular System." Bates, B. A Guide to Physical Examination and History Taking. 9h Ed. 2005.
- ↑ Tavel ME. The appearance of gallop rhythm after exercise stress testing. 'Clin Cardiol'. 1996 Nov;19(11):887-91
- ↑ "Cardiovascular Examination." Pitcher, J. Physical Examination Primer. McMaster University 2007.
External links
- Pubmed.com - journal article on diastolic gallop sounds