Differentiating crohn's disease from other diseases

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor(s)-in-Chief: Aditya Ganti M.B.B.S. [2]
Overview
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
Differentiating Crohn's Disease from other Diseases
The most common disease that mimics the symptoms of Crohn's disease is ulcerative colitis, as both are inflammatory bowel diseases that can affect the colon with similar symptoms. It is important to differentiate these diseases, since the course of the diseases and treatments may be different. In some cases, however, it may not be possible to tell the difference, in which case the disease is classified as indeterminate colitis.
| Crohn's disease | Ulcerative colitis | |
|---|---|---|
| Terminal ileum involvement | Commonly | Seldom |
| Colon involvement | Usually | Always |
| Rectum involvement | Seldom | Usually[1] |
| Involvement around the anus | Common[2] | Seldom |
| Bile duct involvement | No increase in rate of primary sclerosing cholangitis | Higher rate[3] |
| Distribution of Disease | Patchy areas of inflammation (Skip lesions) | Continuous area of inflammation[1] |
| Endoscopy | Deep geographic and serpiginous (snake-like) ulcers | Continuous ulcer |
| Depth of inflammation | May be transmural, deep into tissues[2] | Shallow, mucosal |
| Fistulae | Common[2] | Seldom |
| Stenosis | Common | Seldom |
| Autoimmune disease | Widely regarded as an autoimmune disease | No consensus |
| Cytokine response | Associated with Th1 | Vaguely associated with Th2 |
| Granulomas on biopsy | Can have granulomas[2] | Granulomas uncommon[1] |
| Surgical cure | Often returns following removal of affected part | Usually cured by removal of colon |
| Smoking | Higher risk for smokers | Lower risk for smokers[1] |
Oral lesioins of Crohn's disease must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
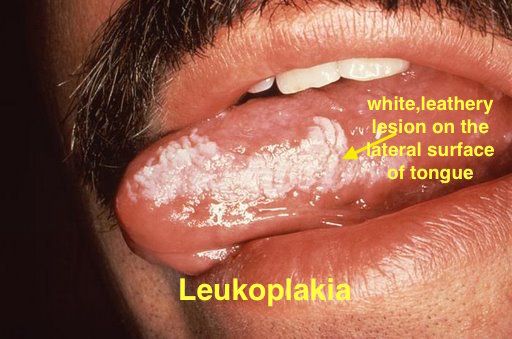 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
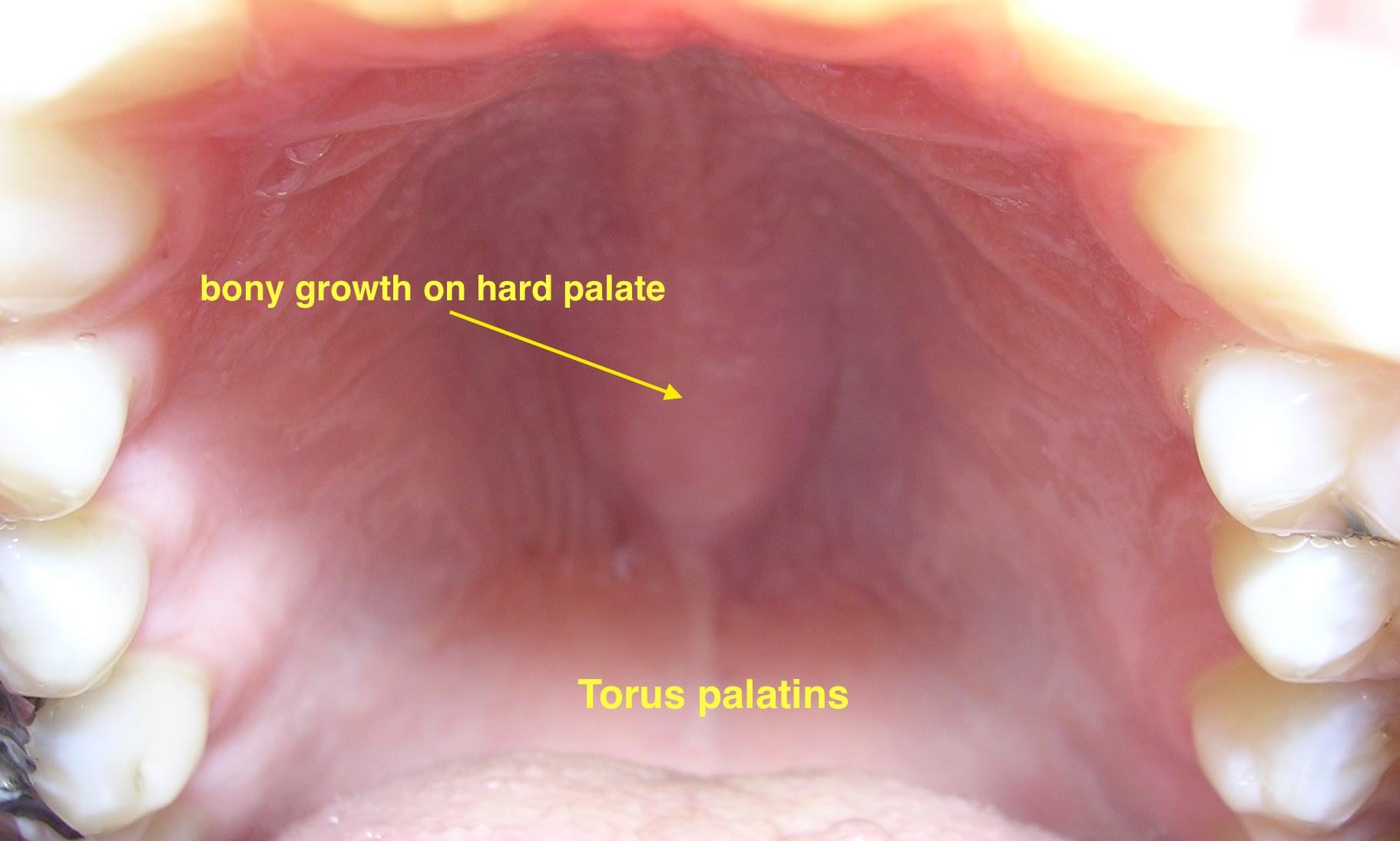 | ||||
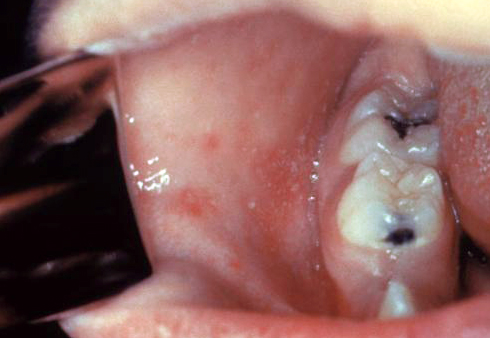
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[6] |
|
|
|
 | ||
| Coxsackie virus |
|
|
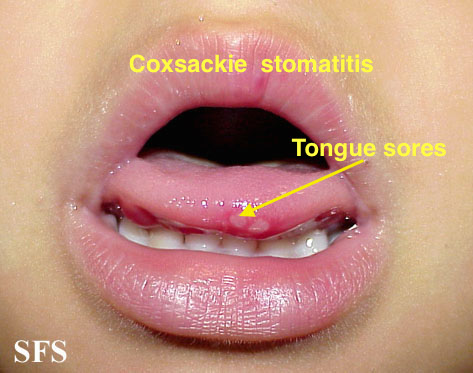
| |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
The following table differentiates all the diseases presenting with abdominal pain, fever and lower gastrointestinal bleeding.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Abbreviations: RUQ= Right upper quadrant of the abdomen, LUQ= Left upper quadrant, LLQ= Left lower quadrant, RLQ= Right lower quadrant, LFT= Liver function test, SIRS= Systemic inflammatory response syndrome, ERCP= Endoscopic retrograde cholangiopancreatography, IV= Intravenous, N= Normal, AMA= Anti mitochondrial antibodies, LDH= Lactate dehydrogenase, GI= Gastrointestinal, CXR= Chest X ray, IgA= Immunoglobulin A, IgG= Immunoglobulin G, IgM= Immunoglobulin M, CT= Computed tomography, PMN= Polymorphonuclear cells, ESR= Erythrocyte sedimentation rate, CRP= C-reactive protein, TS= Transferrin saturation, SF= Serum Ferritin, SMA= Superior mesenteric artery, SMV= Superior mesenteric vein, ECG= Electrocardiogram
Differentiating Crohn's disease from other causes of abdominal pain and diarrhea
Crohn's disease must be differentiated from other causes of abdominal pain and diarrhea.
| Diseases | Clinical manifestations | Para-clinical findings | Gold standard | Additional findings | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms | Physical examination | ||||||||||||||||||||||||
| Lab Findings | Imaging | Histopathology | |||||||||||||||||||||||
| Abdominal pain | Diarrhea | Flushing | Dyspnea | Palpitations | Other symptoms | Wheezing | Telangiectasia | Hypotension | Tachycardia | Systolic murmur of tricuspid regurgitation | Other physical findings | Urinary 5-hydroxyindoleacetic acid (5-HIAA) | Serum Chromogranin A (CgA) | Other markers | Abdominal computed tomography (CT) | Abdominal MRI | Somatostatin receptor scintigraphy [SRS], or Octreoscan | Metaiodobenzylguanidine (MIBG) scintigraphy | Other diagnostic studies | Transthoracic echocardiography | |||||
| Carcinoid Syndrome[9][10][11][12][13][14][15][16][17] | Neuroendocrine tumor of midgut [18][19][20][21] | +
Mild |
+
|
+ | + | + |
Metastatic tumors in the liver: Right upper quadrant pain, hepatomegaly, and early satiety |
+ | +/- | +/- | + | + | - | + | + |
|
|
|
+
|
+ |
|
|
|
|
|
| Neuroendocrine tumor of lung[22][23][24][25] | + | + | + | + | + |
|
+ | +/- | +/- | + | + | - | + | + |
|
Sensitive for detection of liver metastases if present | + | + |
|
- | Typical low-grade:bland cells containing regular round nuclei with finely dispersed chromatin and inconspicuous small nucleoli.Mitotic figures are scarce and necrosis is absent.
Intermediate-grade atypical: presence of Neuroendocrine morphology and either necrosis or 2 to 10 mitoses per 10 HPF |
| |||
| Irritable Bowel Syndrome[26][27][28][29] | +
Perioidic |
|
- | - | - | - | - | - | - | - | - | - | - | - | - | - |
|
- | - | Rome IV criteria
•Related to defecation •Associated with a change in stool frequency •Associated with a change in stool form (appearance) |
|||||
| Malignant neoplasms of small intestine[30][31][32] | +/- | +/- | - | - | +/- |
|
- | - | +/- | - | * Abdominal mass | - | + | Abdominal CT scan may be diagnostic of small intestine cancer. Findings on CT scan suggestive of small intestine cancer include intrinsic mass with a short segment of bowel wall thickening | MRI and MRI enteroscopy are other advance modalities to diagnose and stage small intestinal cancers | - | - | Enteroscopy, capsule endoscopy and double balloon enteroscopy |
|
Biopsy and histopathology | |||||
| Crohn disease[33][34][35][36] | +/- | - | - | - |
|
- | - | - | - | - |
|
- | - |
|
- | - |
|
- |
|
|
|||||
| Benign cutaneous flushing[37] | - | - | + | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | |||
| Systemic mastocytosis[38][39][40][41][42] | + | + | + | + | - | +/- | +/- | + | - | - | - | - | - | - | |||||||||||
| Asthma exacerbation[43][44][45][46] | - | - | - | + | + | + | - | - | + | - |
|
- | - | - | -- | - | - | - | Chest X ray | - |
|
||||
| Anaphylaxis[47][48][49][50][51] | + | -/+ | + | + | + | +/- | - | + | + | - | - | - | - | - | - | - | - |
|
- | - | History of exposure to insect stings,food alllergy,rubber latex,food additives,,allergy to medications,physical factors such s excercise and cold | ||||
| Histaminergic Angioedema[52][53][54][55][56] | +/- | +/- | + | + | + |
|
+ | - | + | + | - | - | - | - |
|
- | - | - |
|
- | - | - |
| ||
| Medullary Thyroid Carcinoma[57][58][59][60] | - | +/- | +/- | +/- | - | - | - | - | - | - | - | - |
|
- | - | - | - |
|
- |
|
|
||||
References
- ↑ 1.0 1.1 1.2 1.3 Kornbluth, Asher. "Ulcerative Colitis Practice Guidelines in Adults" (PDF). American Journal of Gastroenterology. doi:10.1111/j.1572-0241.2004.40036.x. PMID 15233681. Retrieved 2006-11-08.
- ↑ 2.0 2.1 2.2 2.3 Hanauer, Stephen B. "Management of Crohn's Disease in Adults" (PDF). American Journal of Gastroenterology. 96 (3): 635–643. doi:10.1111/j.1572-0241.2001.03671.x. PMID 11280528. Retrieved 2006-11-08.
- ↑ Broomé, Ulrika. "Primary sclerosing cholangitis, inflammatory bowel disease, and colon cancer". Seminars in Liver Disease. 26 (1): 31–41. doi:10.1055/s-2006-933561. PMID 16496231.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar. "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312.
- ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur. J. Intern. Med. 17 (8): 529–35. doi:10.1016/j.ejim.2006.07.012. PMID 17142169.
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.
- ↑ Rubin de Celis Ferrari AC, Glasberg J, Riechelmann RP (August 2018). "Carcinoid syndrome: update on the pathophysiology and treatment". Clinics (Sao Paulo). 73 (suppl 1): e490s. doi:10.6061/clinics/2018/e490s. PMC 6096975. PMID 30133565.
- ↑ Hegyi J, Schwartz RA, Hegyi V (January 2004). "Pellagra: dermatitis, dementia, and diarrhea". Int. J. Dermatol. 43 (1): 1–5. PMID 14693013.
- ↑ Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E (May 2004). "Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours". Nucl Med Commun. 25 (5): 445–9. PMID 15100502.
- ↑ Savelli G, Lucignani G, Seregni E, Marchianò A, Serafini G, Aliberti G, Villano C, Maccauro M, Bombardieri E (May 2004). "Feasibility of somatostatin receptor scintigraphy in the detection of occult primary gastro-entero-pancreatic (GEP) neuroendocrine tumours". Nucl Med Commun. 25 (5): 445–9. PMID 15100502.
- ↑ Bora, ManashKumar; Vithiavathi, S (2012). "Primary bronchial carcinoid: A rare differential diagnosis of pulmonary koch in young adult patient". Lung India. 29 (1): 59. doi:10.4103/0970-2113.92366. ISSN 0970-2113.
- ↑ Yazıcıoğlu A, Yekeler E, Bıcakcıoğlu P, Ozaydın E, Karaoğlanoğlu N (December 2012). "Synchronous bilateral multiple typical pulmonary carcinoid tumors: a unique case with 10 typical carcinoids". Balkan Med J. 29 (4): 450–2. doi:10.5152/balkanmedj.2012.081. PMC 4115868. PMID 25207053.
- ↑ Krausz Y, Keidar Z, Kogan I, Even-Sapir E, Bar-Shalom R, Engel A, Rubinstein R, Sachs J, Bocher M, Agranovicz S, Chisin R, Israel O (November 2003). "SPECT/CT hybrid imaging with 111In-pentetreotide in assessment of neuroendocrine tumours". Clin. Endocrinol. (Oxf). 59 (5): 565–73. PMID 14616879.
- ↑ van der Lely, Aart J.; Herder, Wouter W. de (2005). "Carcinoid syndrome: diagnosis and medical management". Arquivos Brasileiros de Endocrinologia & Metabologia. 49 (5): 850–860. doi:10.1590/S0004-27302005000500028. ISSN 0004-2730.
- ↑ Halperin DM, Shen C, Dasari A, Xu Y, Chu Y, Zhou S, Shih YT, Yao JC (April 2017). "Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study". Lancet Oncol. 18 (4): 525–534. doi:10.1016/S1470-2045(17)30110-9. PMC 6066284. PMID 28238592.
- ↑ Sjöblom SM (September 1988). "Clinical presentation and prognosis of gastrointestinal carcinoid tumours". Scand. J. Gastroenterol. 23 (7): 779–87. PMID 3227292.
- ↑ Ganeshan D, Bhosale P, Yang T, Kundra V (October 2013). "Imaging features of carcinoid tumors of the gastrointestinal tract". AJR Am J Roentgenol. 201 (4): 773–86. doi:10.2214/AJR.12.9758. PMID 24059366.
- ↑ Signs and symptoms of carcinoid syndrome. National Cancer Institute. http://www.cancer.gov/types/gi-carcinoid-tumors/patient/gi-carcinoid-treatment-pdq
- ↑ Modlin IM, Kidd M, Latich I, Zikusoka MN, Shapiro MD (May 2005). "Current status of gastrointestinal carcinoids". Gastroenterology. 128 (6): 1717–51. PMID 15887161.
- ↑ Gustafsson BI, Kidd M, Chan A, Malfertheiner MV, Modlin IM (July 2008). "Bronchopulmonary neuroendocrine tumors". Cancer. 113 (1): 5–21. doi:10.1002/cncr.23542. PMID 18473355.
- ↑ Jeung, Mi-Young; Gasser, Bernard; Gangi, Afshin; Charneau, Dominique; Ducroq, Xavier; Kessler, Romain; Quoix, Elisabeth; Roy, Catherine (2002). "Bronchial Carcinoid Tumors of the Thorax: Spectrum of Radiologic Findings". RadioGraphics. 22 (2): 351–365. doi:10.1148/radiographics.22.2.g02mr01351. ISSN 0271-5333.
- ↑ Nessi R, Basso Ricci P, Basso Ricci S, Bosco M, Blanc M, Uslenghi C (April 1991). "Bronchial carcinoid tumors: radiologic observations in 49 cases". J Thorac Imaging. 6 (2): 47–53. PMID 1649924.
- ↑ Melmon KL, Sjoerdsma A, Mason DT (October 1965). "Distinctive clinical and therapeutic aspects of the syndrome associated with bronchial carcinoid tumors". Am. J. Med. 39 (4): 568–81. PMID 5831899.
- ↑ Ford AC, Forman D, Bailey AG, Axon AT, Moayyedi P (May 2008). "Irritable bowel syndrome: a 10-yr natural history of symptoms and factors that influence consultation behavior". Am. J. Gastroenterol. 103 (5): 1229–39, quiz 1240. doi:10.1111/j.1572-0241.2007.01740.x. PMID 18371141.
- ↑ Simren M, Palsson OS, Whitehead WE (April 2017). "Update on Rome IV Criteria for Colorectal Disorders: Implications for Clinical Practice". Curr Gastroenterol Rep. 19 (4): 15. doi:10.1007/s11894-017-0554-0. PMC 5378729. PMID 28374308.
- ↑ "American Gastroenterological Association medical position statement: irritable bowel syndrome". Gastroenterology. 123 (6): 2105–7. December 2002. doi:10.1053/gast.2002.37095b. PMID 12454865.
- ↑ Mearin F, Lacy BE, Chang L, Chey WD, Lembo AJ, Simren M, Spiller R (February 2016). "Bowel Disorders". Gastroenterology. doi:10.1053/j.gastro.2016.02.031. PMID 27144627.
- ↑ McLaughlin PD, Maher MM (July 2013). "Primary malignant diseases of the small intestine". AJR Am J Roentgenol. 201 (1): W9–14. doi:10.2214/AJR.12.8492. PMID 23789703.
- ↑ Hatzaras I, Palesty JA, Abir F, Sullivan P, Kozol RA, Dudrick SJ, Longo WE (March 2007). "Small-bowel tumors: epidemiologic and clinical characteristics of 1260 cases from the connecticut tumor registry". Arch Surg. 142 (3): 229–35. doi:10.1001/archsurg.142.3.229. PMID 17372046.
- ↑ Lepage C, Bouvier AM, Manfredi S, Dancourt V, Faivre J (December 2006). "Incidence and management of primary malignant small bowel cancers: a well-defined French population study". Am. J. Gastroenterol. 101 (12): 2826–32. doi:10.1111/j.1572-0241.2006.00854.x. PMID 17026561.
- ↑ Hara AK, Swartz PG (2009). "CT enterography of Crohn's disease". Abdom Imaging. 34 (3): 289–95. doi:10.1007/s00261-008-9443-1. PMID 18649092.
- ↑ Baumgart, Daniel C; Sandborn, William J (2012). "Crohn's disease". The Lancet. 380 (9853): 1590–1605. doi:10.1016/S0140-6736(12)60026-9. ISSN 0140-6736.
- ↑ Feuerstein, Joseph D.; Cheifetz, Adam S. (2017). "Crohn Disease: Epidemiology, Diagnosis, and Management". Mayo Clinic Proceedings. 92 (7): 1088–1103. doi:10.1016/j.mayocp.2017.04.010. ISSN 0025-6196.
- ↑ García-Bosch, O.; Ordás, I.; Aceituno, M.; Rodríguez, S.; Ramírez, A. M.; Gallego, M.; Ricart, E.; Rimola, J.; Panes, J. (2016). "Comparison of Diagnostic Accuracy and Impact of Magnetic Resonance Imaging and Colonoscopy for the Management of Crohn's Disease". Journal of Crohn's and Colitis. 10 (6): 663–669. doi:10.1093/ecco-jcc/jjw015. ISSN 1873-9946.
- ↑ Izikson, Leonid; English, Joseph C.; Zirwas, Matthew J. (2006). "The flushing patient: Differential diagnosis, workup, and treatment". Journal of the American Academy of Dermatology. 55 (2): 193–208. doi:10.1016/j.jaad.2005.07.057. ISSN 0190-9622.
- ↑ Hartmann, Karin; Escribano, Luis; Grattan, Clive; Brockow, Knut; Carter, Melody C.; Alvarez-Twose, Ivan; Matito, Almudena; Broesby-Olsen, Sigurd; Siebenhaar, Frank; Lange, Magdalena; Niedoszytko, Marek; Castells, Mariana; Oude Elberink, Joanna N.G.; Bonadonna, Patrizia; Zanotti, Roberta; Hornick, Jason L.; Torrelo, Antonio; Grabbe, Jürgen; Rabenhorst, Anja; Nedoszytko, Boguslaw; Butterfield, Joseph H.; Gotlib, Jason; Reiter, Andreas; Radia, Deepti; Hermine, Olivier; Sotlar, Karl; George, Tracy I.; Kristensen, Thomas K.; Kluin-Nelemans, Hanneke C.; Yavuz, Selim; Hägglund, Hans; Sperr, Wolfgang R.; Schwartz, Lawrence B.; Triggiani, Massimo; Maurer, Marcus; Nilsson, Gunnar; Horny, Hans-Peter; Arock, Michel; Orfao, Alberto; Metcalfe, Dean D.; Akin, Cem; Valent, Peter (2016). "Cutaneous manifestations in patients with mastocytosis: Consensus report of the European Competence Network on Mastocytosis; the American Academy of Allergy, Asthma & Immunology; and the European Academy of Allergology and Clinical Immunology". Journal of Allergy and Clinical Immunology. 137 (1): 35–45. doi:10.1016/j.jaci.2015.08.034. ISSN 0091-6749.
- ↑ Lee, Jason K; Whittaker, Scott J; Enns, Robert A; Zetler, Peter (2008). "Gastrointestinal manifestations of systemic mastocytosis". World Journal of Gastroenterology. 14 (45): 7005. doi:10.3748/wjg.14.7005. ISSN 1007-9327.
- ↑ Horan RF, Austen KF (March 1991). "Systemic mastocytosis: retrospective review of a decade's clinical experience at the Brigham and Women's Hospital". J. Invest. Dermatol. 96 (3): 5S–13S, discussion 13S–14S. PMID 2002264.
- ↑ Sokol, Harry; Georgin-Lavialle, Sophie; Grandpeix-Guyodo, Catherine; Canioni, Danielle; Barete, Stéphane; Dubreuil, Patrice; Lortholary, Olivier; Beaugerie, Laurent; Hermine, Olivier (2010). "Gastrointestinal involvement and manifestations in systemic mastocytosis". Inflammatory Bowel Diseases. 16 (7): 1247–1253. doi:10.1002/ibd.21218. ISSN 1078-0998.
- ↑ Bedeir A, Jukic DM, Wang L, Mullady DK, Regueiro M, Krasinskas AM (November 2006). "Systemic mastocytosis mimicking inflammatory bowel disease: A case report and discussion of gastrointestinal pathology in systemic mastocytosis". Am. J. Surg. Pathol. 30 (11): 1478–82. doi:10.1097/01.pas.0000213310.51553.d7. PMID 17063092.
- ↑ Fuhlbrigge A, Peden D, Apter AJ, Boushey HA, Camargo CA, Gern J, Heymann PW, Martinez FD, Mauger D, Teague WG, Blaisdell C (March 2012). "Asthma outcomes: exacerbations". J. Allergy Clin. Immunol. 129 (3 Suppl): S34–48. doi:10.1016/j.jaci.2011.12.983. PMC 3595577. PMID 22386508.
- ↑ Limb SL, Brown KC, Wood RA, Wise RA, Eggleston PA, Tonascia J, Adkinson NF (December 2005). "Irreversible lung function deficits in young adults with a history of childhood asthma". J. Allergy Clin. Immunol. 116 (6): 1213–9. doi:10.1016/j.jaci.2005.09.024. PMID 16337448.
- ↑ Aldington S, Beasley R (May 2007). "Asthma exacerbations. 5: assessment and management of severe asthma in adults in hospital". Thorax. 62 (5): 447–58. doi:10.1136/thx.2005.045203. PMC 2117186. PMID 17468458.
- ↑ Dougherty RH, Fahy JV (February 2009). "Acute exacerbations of asthma: epidemiology, biology and the exacerbation-prone phenotype". Clin. Exp. Allergy. 39 (2): 193–202. doi:10.1111/j.1365-2222.2008.03157.x. PMC 2730743. PMID 19187331.
- ↑ Peavy RD, Metcalfe DD (August 2008). "Understanding the mechanisms of anaphylaxis". Curr Opin Allergy Clin Immunol. 8 (4): 310–5. doi:10.1097/ACI.0b013e3283036a90. PMC 2683407. PMID 18596587.
- ↑ Tupper J, Visser S (October 2010). "Anaphylaxis: A review and update". Can Fam Physician. 56 (10): 1009–11. PMC 2954079. PMID 20944042.
- ↑ Kemp SF, Lockey RF (September 2002). "Anaphylaxis: a review of causes and mechanisms". J. Allergy Clin. Immunol. 110 (3): 341–8. PMID 12209078.
- ↑ Bjornsson HM, Graffeo CS (December 2010). "Improving diagnostic accuracy of anaphylaxis in the acute care setting". West J Emerg Med. 11 (5): 456–61. PMC 3027438. PMID 21293765.
- ↑ "Usefulness and Limitations of Sequential Serum Tryptase for the Diagnosis of Anaphylaxis in 102 Patients - FullText - International Archives of Allergy and Immunology 2013, Vol. 160, No. 2 - Karger Publishers".
- ↑ Busse PJ, Smith T (August 2017). "Histaminergic Angioedema". Immunol Allergy Clin North Am. 37 (3): 467–481. doi:10.1016/j.iac.2017.03.001. PMID 28687103.
- ↑ Hahn J, Hoffmann TK, Bock B, Nordmann-Kleiner M, Trainotti S, Greve J (July 2017). "Angioedema". Dtsch Arztebl Int. 114 (29–30): 489–496. doi:10.3238/arztebl.2017.0489. PMC 5569554. PMID 28818177.
- ↑ Bernstein JA, Cremonesi P, Hoffmann TK, Hollingsworth J (December 2017). "Angioedema in the emergency department: a practical guide to differential diagnosis and management". Int J Emerg Med. 10 (1): 15. doi:10.1186/s12245-017-0141-z. PMC 5389952. PMID 28405953.
- ↑ Bernstein JA, Moellman J (November 2012). "Emerging concepts in the diagnosis and treatment of patients with undifferentiated angioedema". Int J Emerg Med. 5 (1): 39. doi:10.1186/1865-1380-5-39. PMC 3518251. PMID 23131076.
- ↑ Kaplan AP (June 2008). "Angioedema". World Allergy Organ J. 1 (6): 103–13. doi:10.1097/WOX.0b013e31817aecbe. PMC 3651192. PMID 23282406.
- ↑ Pacini F, Castagna MG, Cipri C, Schlumberger M (August 2010). "Medullary thyroid carcinoma". Clin Oncol (R Coll Radiol). 22 (6): 475–85. doi:10.1016/j.clon.2010.05.002. PMID 20627492.
- ↑ Roy M, Chen H, Sippel RS (2013). "Current understanding and management of medullary thyroid cancer". Oncologist. 18 (10): 1093–100. doi:10.1634/theoncologist.2013-0053. PMC 3805151. PMID 24037980.
- ↑ Mian C, Perrino M, Colombo C, Cavedon E, Pennelli G, Ferrero S, De Leo S, Sarais C, Cacciatore C, Manfredi GI, Verga U, Iacobone M, De Pasquale L, Pelizzo MR, Vicentini L, Persani L, Fugazzola L (May 2014). "Refining calcium test for the diagnosis of medullary thyroid cancer: cutoffs, procedures, and safety". J. Clin. Endocrinol. Metab. 99 (5): 1656–64. doi:10.1210/jc.2013-4088. PMID 24552221.
- ↑ Bae YJ, Schaab M, Kratzsch J (2015). "Calcitonin as Biomarker for the Medullary Thyroid Carcinoma". Recent Results Cancer Res. 204: 117–37. doi:10.1007/978-3-319-22542-5_5. PMID 26494386.