Multiple sclerosis
For patient information click here Editor-In-Chief: C. Michael Gibson, M.S., M.D. [16]; Associate Editor(s)-In-Chief: Cafer Zorkun, M.D., Ph.D. [17]
Synonyms and keywords: Disseminated sclerosis, encephalomyelitis disseminata
| Multiple sclerosis | |
 | |
|---|---|
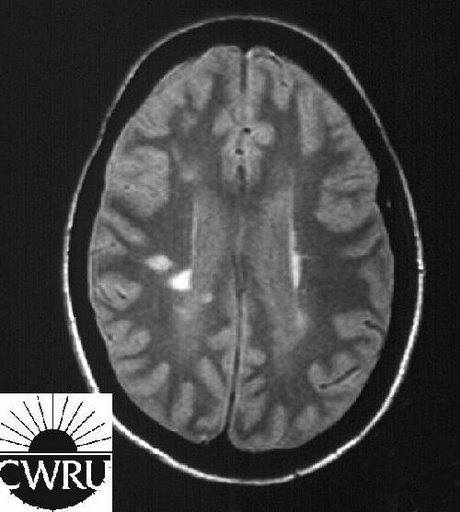
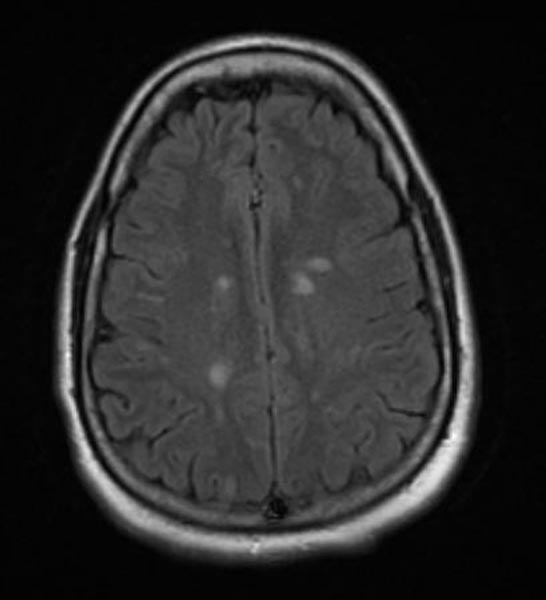
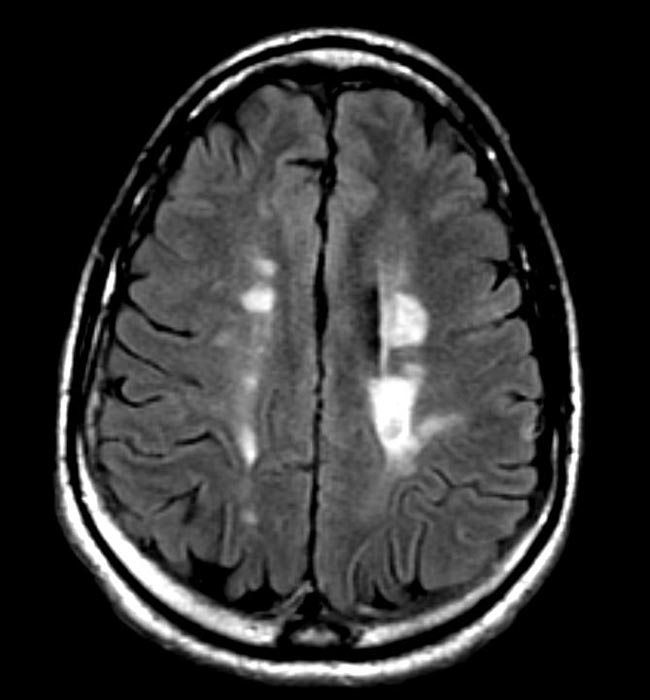
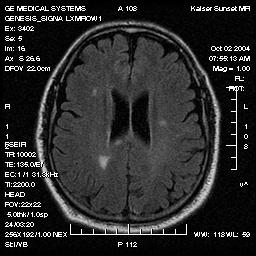
| MRI FLAIR sequence showing four bright spots (plaques) where multiple sclerosis has damaged myelin in the brain | |
| ICD-10 | G35 |
| ICD-9 | 340 |
| OMIM | 126200 |
| DiseasesDB | 8412 |
| MedlinePlus | 000737 |
| MeSH | D009103 |
|
Multiple sclerosis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Multiple sclerosis On the Web |
|
American Roentgen Ray Society Images of Multiple sclerosis |
Overview
Classification
Pathophysiology
Causes
Differential Diagnosis
Risk Factors
Natural History, Complications and Prognosis
Diagnosis
History and Symptoms | Physical Examination |Laboratory Findings | ECG | EEG | Chest X Ray |CT | MRI |Echocardiography or Ultrasound |Other Imaging Findings | Other Diagnostic Studies
Treatment
Medical therapy | Surgery | Prevention |Cost-effectiveness of Therapy| Future or Investigational Therapies
See also
Overview
Multiple sclerosis (abbreviated MS, formerly known as disseminated sclerosis or encephalomyelitis disseminata) is a chronic, inflammatory, demyelinating disease that affects the central nervous system (CNS). Disease onset usually occurs in young adults, is more common in women and the disease has a prevalence that ranges between 2 and 150 per 100,000 depending on the country or specific population.[1] MS was first described in 1868 by Jean-Martin Charcot.
Description
MS affects the neurons in the areas of the brain and spinal cord known as the white matter. These cells carry signals in between the grey matter areas, where the processing is done, and between these and the rest of the body. More specifically, MS destroys oligodendrocytes which are the cells responsible for creating and maintaining a fatty layer, known as the myelin sheath, which helps the neurons carry electrical signals. MS results in a thinning or complete loss of myelin and, less frequently, the cutting (transection) of the neuron's extensions or axons. When the myelin is lost, the neurons can no longer effectively conduct their electrical signals. The name multiple sclerosis refers to the scars (scleroses - better known as plaques or lesions) in the white matter. Loss of myelin in these lesions causes some of the symptoms that may vary widely depending upon which signals are interrupted. However, more advanced forms of imaging are now showing that much of the damage happens outside these regions. A consequence of this course of action is that almost any neurological symptom can accompany the disease.
Multiple sclerosis may take several forms, with new symptoms occurring either in discrete attacks (relapsing forms) or slowly accumulating over time (progressive forms). Most people are first diagnosed with relapsing-remitting MS but develop secondary-progressive MS (SPMS) after a number of years. Between attacks, symptoms may resolve completely, but permanent neurological problems often persist, especially as the disease advances.
Although much is known about the mechanisms involved in the disease process, the cause remains elusive. The theory with the most adherents is that it results from attacks to the nervous system by the body's own immune system. Some believe it is a metabolically dependent disease while others think that it might be caused by a virus such as Epstein-Barr. Still other people believe that its virtual absence from the tropics points to a deficiency of vitamin D during childhood.
The disease currently does not have a cure, but several therapies have proven helpful. The aims of treatment are returning function after an attack, preventing new attacks, and preventing disability. As with any treatment, medications have several adverse effects, and many therapies are still under investigation. At the same time different alternative treatments are pursued by many patients, despite the paucity of supporting scientific study.
The prognosis, or expected course of the disease, for a person depends on the subtype of the disease; the characteristics of the individual, the initial symptoms; and the degree of disability the person experiences as time advances. However life expectancy of patients is nearly the same as that of the unaffected population and in many cases a normal life is possible.
Epidemiology
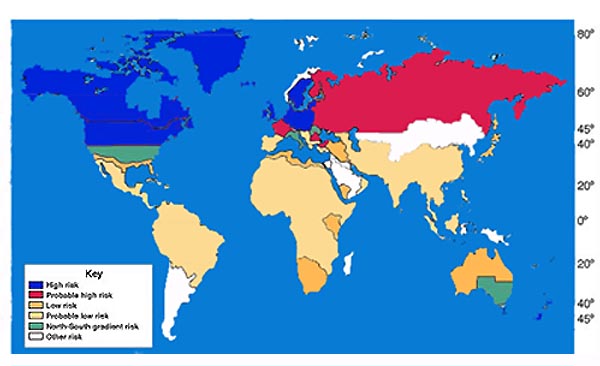
In northern Europe, continental North America, and Australasia, about one of every 1000 citizens suffers from multiple sclerosis, whereas in the [rabian peninsula, Asia, and continental South America, the frequency is much lower. In sub-Saharan Africa, MS is extremely rare. With important exceptions, there is a north-to-south gradient in the northern hemisphere and a south-to-north gradient in the southern hemisphere, with MS being much less common in people living near the equator.[2] Climate, diet, geomagnetism, toxins, sunlight exposure, genetic factors, and infectious diseases have all been discussed as possible reasons for these regional differences. Environmental factors during childhood may play an important role in the development of MS later in life. This idea is based on several studies of migrants showing that if migration occurs before the age of fifteen, the migrant acquires the new region's susceptibility to MS. If migration takes place after age fifteen, the migrant keeps the susceptibility of his home country.[3] However other works suggest that the age/geographical risk for developing multiple sclerosis spans a larger timescale than just the first 15 years of life.[4]
MS occurs mainly in Caucasians. It is twentyfold lower in the Inuit people of Canada than in other Canadians living in the same region. It is also rare in the Native American tribes of North America, Australian Aborigines and the Māori of New Zealand. Scotland appears to have the highest rate of MS in the world.[5] The reasons for this are unknown. These few examples point out that either genetic background or lifestyle and cultural factors play an important role in the development of MS.
As observed in many autoimmune disorders, MS is more common in females than males; the mean sex ratio is about two females for every male. In children (who rarely develop MS) the sex ratio may reach three females for each male. In people over age fifty, MS affects males and females equally. Onset of symptoms usually occurs between fifteen to forty years of age, rarely before age fifteen or after age sixty.
As previously discussed, there is a genetic component to MS. On average one of every 25 siblings of individuals with MS will also develop MS. Almost half of the identical twins of MS-affected individuals will develop MS, but only one of twenty fraternal twins. If one parent is affected by MS, each child has a risk of only about one in forty of developing MS later in life.[6]
Finally, it is important to remark that advances in the study of related diseases have shown that some cases formerly considered MS are not MS at all. In fact, all the studies before 2004 can be affected by the impossibility to distinguish MS and Devic's disease (NMO) reliably before this date. The error can be important in some areas, and is considered to be 30% in Japan.[7]
History
The French neurologist Jean-Martin Charcot (1825–93) was the first person to recognize multiple sclerosis as a distinct, separate disease in 1868. Summarizing previous reports and adding his own important clinical and pathological observations, Charcot called the disease sclerose en plaques. The three signs of MS now known as Charcot's triad are dysarthria (problems with speech), ataxia (problems with coordination), and tremor. Charcot also observed cognition changes in MS since he described his patients as having a "marked enfeeblement of the memory" and "with conceptions that formed slowly".[8]
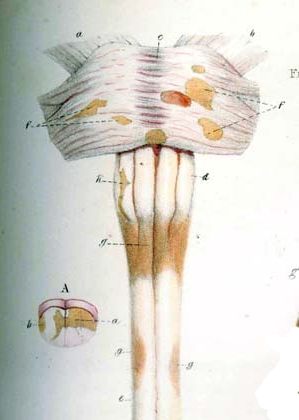
Prior to Charcot, Robert Hooper (1773–1835), a British pathologist and practicing physician, Robert Carswell (1793–1857), a British professor of pathology, and Jean Cruveilhier (1791–1873), a French professor of pathologic anatomy, had described and illustrated many of the disease's clinical details.
After this, several people, such as Eugène Devic (1858–1930), Jozsef Balo (1895–1979), Paul Ferdinand Schilder (1886–1940), and Otto Marburg (1874–1948) found special cases of the disease that some authors consider different diseases and now are called the borderline forms of multiple sclerosis.
There are several historical accounts of people who probably had MS. Saint Lidwina of Schiedam (1380–1433), a Dutch nun, may be one of the first identifiable MS patients. From the age of sixteen until her death at age 53, she suffered intermittent pain, weakness of the legs, and vision loss—symptoms typical of MS. Almost a hundred years before there is a story from Iceland of a young woman called Halla. This girl suddenly lost her vision and capacity to talk; but after praying to the saints recovered them seven days after.[9] Augustus Frederick d'Este (1794–1848), an illegitimate grandson of King George III of Great Britain, almost certainly suffered from MS. D'Este left a detailed diary describing his 22 years living with the disease. He began his diary in 1822 and it had its last entry in 1846 (only to remain unknown until 1948). His symptoms began at age 28 with a sudden transient visual loss after the funeral of a friend. During the course of his disease he developed weakness of the legs, clumsiness of the hands, numbness, dizziness, bladder disturbances, and erectile dysfunction. In 1844, he began to use a wheelchair. Despite his illness, he kept an optimistic view of life.[10] Another early account of MS was kept by the British diarist W. N. P. Barbellion, who maintained a detailed log of his diagnosis and struggle with MS. His diary was published in 1919 as The Journal of a Disappointed Man.
Pathophysiology
Although much is known about how multiple sclerosis causes damage, the reasons why multiple sclerosis occurs are not known.
Multiple sclerosis is a disease in which the myelin (a fatty substance which covers the axons of nerve cells) degenerates. According to the view of most researchers, a special subset of lymphocytes, called T cells, plays a key role in the development of MS.
According to a strictly immunological explanation of MS, the inflammatory process is triggered by the T cells. T cells gain entry into the brain via the blood-brain barrier (a capillary system that should prevent entrance of T-cells into the nervous system). The blood brain barrier is normally not permeable to these types of cells, unless triggered by either infection or a virus, where the integrity of the tight junctions forming the blood-brain barrier is decreased. When the blood brain barrier regains its integrity (usually after infection or virus has cleared) the T cells are trapped inside the brain. These lymphocytes recognize myelin as foreign and attack it as if it were an invading virus. That triggers inflammatory processes, stimulating other immune cells and soluble factors like cytokines and antibodies. Leaks form in the blood-brain barrier. These leaks, in turn, cause a number of other damaging effects such as swelling, activation of macrophages, and more activation of cytokines and other destructive proteins such as matrix metalloproteinases. A deficiency of uric acid has been implicated in this process.[11]
It is known that a repair process, called remyelination, takes place in early phases of the disease, but the oligodendrocytes that originally formed a myelin sheath cannot completely rebuild a destroyed myelin sheath. The newly-formed myelin sheaths are thinner and often not as effective as the original ones. Repeated attacks lead to successively fewer effective remyelinations, until a scar-like plaque is built up around the damaged axons, according to four different damage patterns.[12] The central nervous system should be able to recruit oligodendrocyte stem cells capable of turning into mature myelinating oligodendrocytes, but it is suspected that something inhibits stem cells in affected areas.
The axons themselves can also be damaged by the attacks.[13] Often, the brain is able to compensate for some of this damage, due to an ability called neuroplasticity. MS symptoms develop as the cumulative result of multiple lesions in the brain and spinal cord. This is why symptoms can vary greatly between different individuals, depending on where their lesions occur.
Causes
Although many risk factors for multiple sclerosis have been identified, no definitive cause has been found. MS likely occurs as a result of some combination of both environmental and genetic factors. Various theories try to combine the known data into plausible explanations. Although most accept an autoimmune explanation, several theories suggest that MS is an appropriate immune response to one or several underlying conditions (the etiology could be heterogeneous[14]). The need for alternative theories is supported by the poor results of present therapies, since autoimmune theory predicted greater success.[15][16][17]
Environmental
The most popular hypothesis is that a viral infection or retroviral reactivation primes a susceptible immune system for an abnormal reaction later in life. On a molecular level, this might occur if there is a structural similarity between the infectious virus and some component of the central nervous system, leading to eventual confusion in the immune system.
Since MS seems to be more common in people who live farther from the equator, another theory proposes that decreased sunlight exposure[18] and possibly decreased vitamin D production may help cause MS. This theory is bolstered by recent research into the biochemistry of vitamin D, which has shown that it is an important immune system regulator. A large, 2006 study by the Harvard School of Public Health, reported evidence of a link between Vitamin D deficiency and the onset of multiple sclerosis.[19] Other data comes from a 2007 study which concluded that sun exposure during childhood reduces the risk of suffering MS, while controlling for genetic factors.[20][21]
Other theories, noting that MS is less common in children with siblings, suggest that less exposure to illness in childhood leads to an immune system which is not primed to fight infection and is thus more likely to attack the body. One explanation for this would be an imbalance between the Th1 type of helper T-cells, which fight infection, and the Th2 type, which are more active in allergy and more likely to attack the body.
Other theories describe MS as an immune response to a chronic infection. The association of MS with the Epstein-Barr virus suggests a potential viral contribution in at least some individuals.[22] Still others believe that MS may sometimes result from a chronic infection with spirochetal bacteria, a hypothesis supported by research in which cystic forms were isolated from the cerebrospinal fluid of all MS patients in a small study.[23] When the cysts were cultured, propagating spirochetes emerged. Another bacterium that has been implicated in MS is Chlamydophila pneumoniae; it or its DNA has been found in the cerebrospinal fluid of MS patients by several research laboratories, with one study finding that the oligoclonal bands of 14 of the 17 MS patients studied consisted largely of antibodies to Chlamydophila antigens.[24]
Severe stress may also be a factor—a large study in Denmark found that parents who had lost a child unexpectedly were 50% more likely to develop MS than parents who had not.[25] Smoking has also been shown to be an independent risk factor for developing MS.[26]
Genetic

MS is not considered a hereditary disease. However, increasing scientific evidence suggests that genetics may play a role in determining a person's susceptibility to MS:
Some populations, such as the Roma, Inuit, and Bantus, rarely if ever get MS. The indigenous peoples of the Americas and Asians have very low incidence rates.
In the population at large, the chance of developing MS is less than a tenth of one percent. However, if one person in a family has MS, that person's first-degree relatives—parents, children, and siblings—have a one to three percent chance of getting the disease.
For identical twins, the likelihood that the second twin may develop MS if the first twin does is about 30%. For fraternal twins (who do not inherit an identical set of genes), the likelihood is closer to that for non-twin siblings, or about 4%. This pattern suggests that, while genetic factors clearly help determine the risk of MS, other factors such as environmental effects or random chance are also involved. The actual correlation may be somewhat higher than reported by these numbers as people with MS lesions remain essentially asymptomatic throughout their lives.
Further indications that more than one gene is involved in MS susceptibility comes from studies of families in which more than one member has MS. Several research teams found that people with MS inherit certain regions on individual genes more frequently than people without MS. Of particular interest is the human leukocyte antigen (HLA) or major histocompatibility complex region on chromosome 6. HLAs are genetically determined proteins that influence the immune system. However, there are other genes in this region which are not related to the immune system.
The HLA patterns of MS patients tend to be different from those of people without the disease. Investigations in northern Europe and America have detected three HLAs that are more prevalent in people with MS than in the general population. Studies of American MS patients have shown that people with MS also tend to exhibit these HLAs in combination—that is, they have more than one of the three HLAs—more frequently than the rest of the population. Furthermore, there is evidence that different combinations of the HLAs may correspond to variations in disease severity and progression.
A large study examining 334,923 single nucleotide polymorphisms (small variations in genes) in 931 families showed that apart from HLA-DRA there were two genes in which polymorphisms strongly predicted MS; these were the IL2RA (a subunit of the receptor for interleukin 2) and the IL7RA (idem for interleukin 7) genes. Mutations in these genes were already known to be associated with diabetes mellitus type 1 and other autoimmune conditions; the findings circumstantially support the notion that MS is an autoimmune disease.[27]
Studies of families with multiple cases of MS and research comparing proteins expressed in humans with MS to those of mice with EAE suggest that another area related to MS susceptibility may be located on chromosome 5. Other regions on chromosomes 2, 3, 7, 11, 17, 19, and X have also been identified as possibly containing genes involved in the development of MS.
These studies strengthen the theory that MS is the result of a number of factors rather than a single gene or other agent. Development of MS is likely to be influenced by the interactions of a number of genes, each of which (individually) has only a modest effect. Additional studies are needed to specifically pinpoint which genes are involved, determine their function, and learn how each gene's interactions with other genes and with the environment make an individual susceptible to MS.
Signs and symptoms
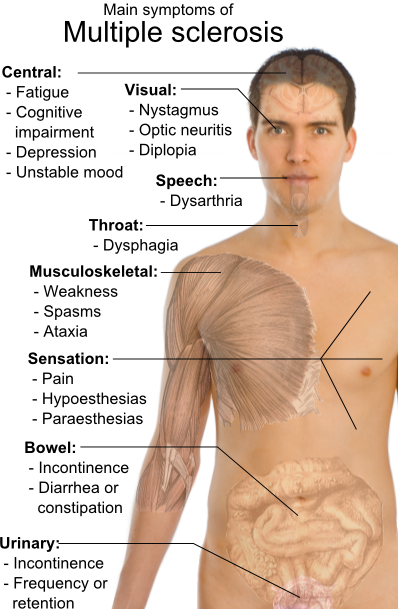
MS can cause a variety of symptoms, including changes in sensation (hypoesthesia), muscle weakness, abnormal muscle spasms, or difficulty in moving; difficulties with coordination and balance (ataxia); problems in speech (dysarthria) or swallowing (dysphagia), visual problems (nystagmus, optic neuritis, or diplopia), fatigue and acute or chronic pain syndromes, bladder and bowel difficulties, cognitive impairment, or emotional symptomatology (mainly depression). Lhermitte's sign is considered a classic MS finding, but it can be seen in several other conditions as well. The main clinical measure of disability progression and severity of the symptoms is the Expanded Disability Status Scale or EDSS.[28]
The initial attacks are often transient, mild (or asymptomatic), and self-limited. They often do not prompt a health care visit and sometimes are only identified in retrospect once the diagnosis has been made based on further attacks. The most common initial symptoms reported are: changes in sensation in the arms, legs or face (33%), complete or partial vision loss (optic neuritis) (16%), weakness (13%), double vision (7%), unsteadiness when walking (5%), and balance problems (3%); but many rare initial symptoms have been reported such as aphasia or psychosis.[29][30] Fifteen percent of individuals have multiple symptoms when they first seek medical attention.[31] For some people the initial MS attack is preceded by infection, trauma, or strenuous physical effort.
Bladder
Bladder problems (See also urinary system and urination) appear in 70-80% of MS patients and they have an important effect both in hygiene habits and social activity.[32][33]
However bladder problems are usually related with high levels of disability and pyramidal signs in lower limbs[34]
The most common problems are an increase of frequency and urgency (incontinence) but difficulties to begin urination, hesitation, leaking, retention and sensation of incomplete urination also appear. When there is retention secondary urinary infections are common.
There are many cortical and subcortical structures implicated in micturition.[35] Accordingly; MS lesions in different central nervous system structures can cause these kind of symptoms.
Treatment objectives are aliviation of symptoms of urinary dysfunction, treatment of urinary infections, reduction of complicating factors and preservation of renal function.Treatments can be classified in two main subtypes: pharmacological and non pharmacological.
Pharmacological treatments vary greatly depending on the origin or type of dysfunction; however some examples of the medications used are:[36] alfuzosin for retention,[37] trospium and flavoxate for urgency and incontinency,[38][39] or desmopressin for nocturia.[40][41]
Non pharmacological treatments involve the use of pelvic floor muscle training, stimulation, biofeedback, pessaries, bladder retraining, and sometimes intermittent catheterization.[42]
Cognitive
Cognitive impairments are common. Neuropsychological studies suggest that 40 to 60 percent of patients have cognitive deficits;[43] with the lowest percentages usually from community-based studies and the highest ones from hospital-based.
Cognitive impairment, sometimes referred to as brain fog, is already present in the beginnings of the disease.[44] Even in probable MS (after the first attack but before a second confirmatory one) up to 50% of patients have mild impairment.[45]
Some of the most common declines are in recent memory, attention, processing speed, visual-spatial abilities and executive functions.[46] Other cognitive-related symptoms are emotional instability, and fatigue, including purely neurological fatigue. The cognitive impairments in MS are usually mild; and only in 5% of patients can we speak of dementia. Nevertheless they are related with unemployment and reduced social interactions.[47] They are also related with driving difficulties.[48]
Neurocognitive testing is important for determining the extent of cognitive deficits. Neuropsychological stimulation may help to reverse or decrease the cognitive defects although its management relies on lifestyle strategies.Interferons have demonstrated that can help to reduce cognitive limitations in multiple sclerosis.[49] Anticholinesterase drugs such as donepezil commonly used in alzheimer disease; although not approved yet for multiple sclerosis; have also shown efficacy in different clinical trials.[50][51][52]
Emotional
Emotional symptoms are also common and are thought to be both the normal response to having a debilitating disease and the result of damage to specific areas of the cental nervous system that generate and control emotions.
Clinical depression is the most common neuropsychiatric condition: lifetime depression prevalence rates of 40-50% and 12 month prevalence rates around 20% have been typically reported for samples of people with MS; these figures are considerably higher than those for the general population or for people with other chronic illnesses.[53][54] Many brain-imaging studies have tried to relate depression to lesions in different brain regions with variable success. On balance the evidence seems to favour an association with neuropathology in the left anterior temporal/parietal regions.[55]
Other feelings such as anger, anxiety, frustration, and hopelessness also appear frequently, and suicide is a very real threat since 15% of deaths in MS sufferers are due to this cause.[56]
Fatigue
Fatigue is very common and disabling in MS. At the same time it has a close relationship with depressive symptomatology.[57] When depression is reduced fatigue also tends to improve, so patients should be evaluated for depression before other therapeutic approaches are used.[58]. In a similar way other factors like disturbed sleep, chronic pain, poor nutrition, or even some medications can contribute to fatigue; and therefore medical professionals are encouraged to identify and modify them.[59] There are also different medications used to treat fatigue; such as amantadine,[60][61] or pemoline;[62][63] as well as psichological interventions of energy conservation;[64][65] but the effects of all of them are small. For this reason fatigue is a very difficult symptom to manage.
Internuclear ophthalmoplegia
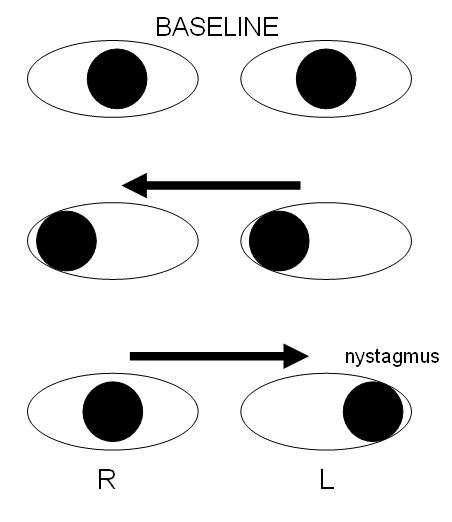
Internuclear ophthalmoplegia is a disorder of conjugate lateral gaze. The affected eye shows impairment of adduction. The partner eye diverges from the affected eye during abduction, producing diplopia; during extreme abduction, compensatory nystagmus can be seen in the partner eye. Diplopia means double vision while nystagmus is involuntary eye movement characterized by alternating smooth pursuit in one direction and a saccadic movement in the other direction.
Internuclear ophthalmoplegia occurs when MS affects a part of the brain stem called the medial longitudinal fasciculus, which is responsible for communication between the two eyes by connecting the abducens nucleus of one side to the oculomotor nucleus of the opposite side. This results in the failure of the medial rectus muscle to contract appropriately, so that the eyes do not move equally (called disconjugate gaze).
Different drugs as well as optic compensatory systems and prisms can be used to improve this symptoms.[66][67][68][69] Surgery can also be used in some cases for this problem.[70]
Mobility restrictions
Restrictions in mobility (walking, transfers, bed mobility) are common in individuals suffering from multiple sclerosis. Within 10 years after the onset of MS one-third of patients reach a score of 6 on the Expanded Disability Status Scale (requiring the use of a unilateral walking aid),and by 30 years the proportion increases to 83%. Within 5 years the Expanded Disability Status Score is 6 in 50% of those with the progressive form of MS.[71]
In MS a wide range of impairments may exist which can act either alone or in combination to impact directly on a person's balance, function and mobility. Such impairments include fatigue, weakness, hypertonicity, low exercise tolerance, impaired balance, ataxia and tremor.[72]
Interventions may be aimed at the level of the impairments that reduce mobility; or at the level of disability. At this second level interventions include provision, education and instruction in use of equipment such as walking aids, wheelchairs, motorized scooters and car adaptations; and instruction about compensatory strategies to accomplish an activity, (for example,undertaking safe transfers by pivoting in a flexed posture rather than standing up and stepping around)
Optic neuritis
Up to 50% of patients with MS will develop an episode of optic neuritis, and 20% of the time optic neuritis is the presenting sign of MS. The presence of demyelinating white matter lesions on brain MRI at the time of presentation of optic neuritis is the strongest predictor for developing clinically definite MS. Almost half of the patients with optic neuritis have white matter lesions consistent with multiple sclerosis. At five years follow-up, the overall risk of developing MS is 30%, with or without MRI lesions. Patients with a normal MRI still develop MS (16%), but at a lower rate compared to those patients with three or more MRI lesions (51%). From the other perspective, however, almost half (44%) of patients with any demyelinating lesions on MRI at presentation will not have developed MS ten years later. [73][74]
Individuals experience rapid onset of pain in one eye, followed by blurry vision in part or all of the visual field of that eye. Inflammation of the optic nerve causes loss of vision usually due to the swelling and destruction of the myelin sheath covering the optic nerve.
The blurred vision usually resolves within ten weeks, but individuals are often left with less vivid color vision (especially red) in the affected eye.
Systemic intravenous treatment with corticosteroids, which may quicken the healing of the optic nerve, prevent complete loss of vision, and delay the onset of other symptoms, is often recommended.
Pain
Pain is a common symptom in MS; appearing in 55% of patients at some point of their disease process; specially as time passes.[75] It is strong and debilitating and has a profound effect in the quality of life and mental health of the sufferer.[76] It usually appears after a lesion to the ascending or descending tracts that control the transmission of painful stimulus. such as the anterolateral system, but many other causes are also possible.[77] Most frequent pains reported are headaches (40%), dysesthetic limb pain (19%), back pain (17%), and painful spasms (11%).[78]
Acute pain is mainly due to optic neuritis, being corticosteroids the best treatment available; to trigeminal neuralgia, to Lhermitte's sign or to dysesthesias.[79] Subacute pain is usually secondary to the disease and can be consequence of being too much time in the same position, urinary retention, infected skin ulcers and many others. Treatment will depend on cause. Chronic pain is very common and the harder to treat being its most common cause dysesthesias.
Trigeminal neuralgia
Trigeminal neuralgia or "tic douloureux", is a disorder of the trigeminal nerve that causes episodes of intense pain in the eyes, lips, nose, scalp, forehead, and jaw. It affects 1 to 2% of MS patients during their disease.[80][81] The episodes of pain occur paroxysmally, or suddenly; and the patients describe it as trigger area on the face, so sensitive that touching or even air currents can bring an episode of pain. Usually it's successfully treated with anticonvulsants such as carbamazepine[82] or phenytoin[83] but others such as gabapentin[84] can be used. [85] When drugs are not effective enough surgery may be recommended. Further damage to the nerve to prevent the transmission of pain (Rhyzotomy) has proven its efficacy;[86] however the beneficial effects and risks in multiple sclerosis patients of those procedures that consist in relieving the pressure on the nerve are still under discussion.[87][88]
Lhermitte's sign
Lhermitte's sign is an electrical sensation that runs down the back and into the limbs, and is produced by bending the neck forward. The sign suggests a lesion of the dorsal columns of the cervical cord or of the caudal medulla; correlating significantly with cervical MRI abnormalities.[89] Between 25 and 40% of MS patients report having Lhermitte's sign during the course of their illness. [90][91][92]
Dysesthesias
Dysesthesias are disagreeable sensations produced by ordinary stimuli. The abnormal sensations are often described as painful feelings such as burning, wetness, itching, electric shock or pins and needles; and are caused by lesions of the peripheral or central sensory pathways. Both Lhermitte's sign and painful dysesthesias usually respond well to treatment with carbamazepine, clonazepam or amitriptyline. [93][94][95]
Sexual
Sexual dysfunction (SD) is one of many symptoms affecting persons with a diagnosis of multiple sclerosis (MS) and other neurological disease. SD in men encompasses both erectile and ejaculatory disorder. The prevalence of SD in men with MS ranges from 75 to 91% (O'Leary et al., 2007). Erectile dysfunction appears to be the most common form of SD documented in MS. SD may be due to alteration of the ejaculatory reflexe which may be affected by neurological conditions such as MS [96]
Spasticity
Spasticity is characterised by increased stiffness and slowness in limb movement, the development of certain postures, an association with weakness of voluntary muscle power, and with involuntary and sometimes painful spasms of limbs.[59] A physiotherapist can help to reduce spasticity and avoid the development of contractures with techniques such as passive stretching.[97] There is evidence, albeit limited, of the clinical effectiveness of baclofen,[98] dantrolene,[99] diazepam,[100] and tizanidine.[101][102][103] In the most complicated cases intrathecal injections of baclofen can be used.[104] There are also palliative measures like castings, splints or customised seatings.[59]
Transverse myelitis
Some MS patients develop rapid onset of numbness, weakness, bowel or bladder dysfunction, and/or loss of muscle function, typically in the lower half of the body. This is the result of MS attacking the spinal cord. The symptoms and signs depend upon the level of the spinal cord involved and the extent of the involvement.
Prognosis for complete recovery is generally poor. Recovery from transverse myelitis usually begins between weeks 2 and 12 following onset and may continue for up to 2 years in some patients and as many as 80% of individuals with transverse myelitis are left with lasting disabilities.
Treatment is usually symptomatic only, corticosteroids being used with limited success.
Tremor and ataxia
Tremor is an unintentional, somewhat rhythmic, muscle movement involving to-and-fro movements (oscillations) of one or more parts of the body. It is the most common of all involuntary movements and can affect the hands, arms, head, face, vocal cords, trunk, and legs.
Ataxia is an unsteady and clumsy motion of the limbs or torso due to a failure of the gross coordination of muscle movements. People with ataxia experience a failure of muscle control in their arms and legs, resulting in a lack of balance and coordination or a disturbance of gait.
Tremor and ataxia are frequent in MS. They present in 25 to 60% of patients. They can be very disabling and embarrassing, and are difficult to manage.[105] The origin of tremor in MS is difficult to precise but it can be due to a mixture of different factors such as damage to the cerebellar connections, weakness, spasticity, etc.
In the treatment of tremor many medications have been proposed; however their efficacy is very limited. Medications that have been reported to provide some relief are isoniazid,[106][107][108][109] carbamazepine,[110] propranolol;[111][112][113] and gluthetimide,[114] but published evidence of effectiveness is very limited.[115]
Physical therapy is not indicated as a treatment for tremor or ataxia; however, the use of different orthese devices can help. An example is the use of wrist bandages with weights, which can be useful to increase the inertia of movement and therefore reduce tremor.[116] Daily use objects have also to be adapted so they are easier to grab and use.
If all these measures fail some patients are candidates for thalamus surgery. This kind of surgery can be both a thalamotomy or the implantation of a thalamic stimulator. Complications are frequent (30% in thalamotomy and 10% in deep brain stimulation) and include a worsening of ataxia, dysarthria and hemiparesis.
Thalamotomy is a more efficacious surgical treatment for intractable MS tremor, however the higher incidence of persistent neurological deficits in patients receiving lesional surgery supports the use of deep brain stimulation as the preferred surgical strategy.[117]
Diagnosis

Multiple sclerosis is difficult to diagnose in its early stages. In fact, a definite diagnosis cannot be made until other disease processes (differential diagnoses) have been ruled out and, in the case of relapsing-remitting MS, there is evidence of at least two anatomically separate demyelinating events separated by at least thirty days. In the case of primary progressive, a slow progression of signs and symptoms over at least 6 months is required.
Historically, different criteria were used and the Schumacher and Poser criteria were both popular. Currently, the McDonald criteria represent international efforts to standardize the diagnosis of MS using clinical, laboratory and radiologic data.[118]
- Clinical data alone may be sufficient for a diagnosis of MS. If an individual has suffered two separate episodes of neurologic symptoms characteristic of MS, and the individual also has consistent abnormalities on physical examination, a diagnosis of MS can be made with no further testing. Since some people with MS seek medical attention after only one attack, other testing may hasten the diagnosis and allow earlier initiation of therapy.
- Magnetic resonance imaging (MRI) of the brain and spine is often used during the diagnostic process. MRI shows areas of demyelination (lesions) as bright spots on the image. A substance, called Gadolinium, can be injected into the spinal column to highlight active plaques and, by elimination, demonstrate the existence of historical lesions not associated with clinical symptoms. This can provide the evidence of chronic disease needed for a definitive diagnosis of MS.
- Testing of cerebrospinal fluid (CSF) can provide evidence of chronic inflammation of the central nervous system. The CSF is tested for oligoclonal bands, which are immunoglobulins found in 85% to 95% of people with definite MS (but also found in people with other diseases).[119] Combined with MRI and clinical data, the presence of oligoclonal bands can help make a definite diagnosis of MS. Lumbar puncture is the procedure used to collect a sample of CSF.
- The brain of a person with MS often responds less actively to stimulation of the optic nerve and sensory nerves. These brain responses can be examined using visual evoked potentials (VEPs) and somatosensory evoked potentials (SEPs). Decreased activity on either test can reveal demyelination which may be otherwise asymptomatic. Along with other data, these exams can help find the widespread nerve involvement required for a definite diagnosis of MS.[120]
Another test, which may become important in the future, is measurement of antibodies against myelin proteins such as myelin oligodendrocyte glycoprotein (MOG) and myelin basic protein (MBP). As of 2007, however, there is no established role for these tests in diagnosing MS. Optical coherence tomography of the eye's retina is also under study[121], mainly as a tool to measure response to medication and axonal degeneration[122].
The signs and symptoms of MS can be similar to other medical problems, such as neuromyelitis optica, stroke, brain inflammation, infections such as Lyme disease (which can produce identical MRI lesions and CSF abnormalities[123][124][125][126]), tumors, and other autoimmune problems, such as lupus. Additional testing may be needed to help distinguish MS from these other problems.
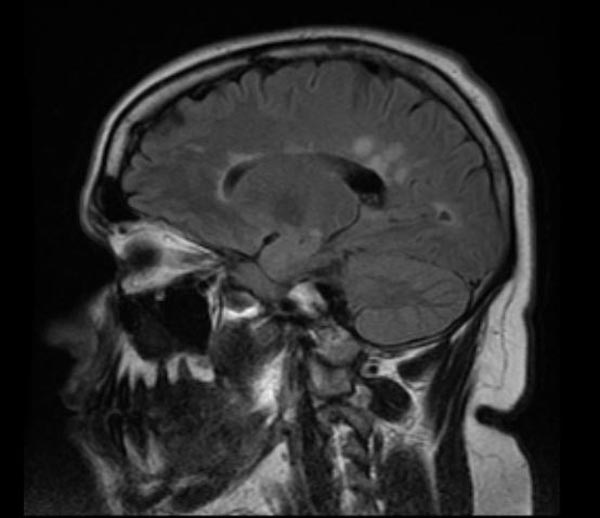
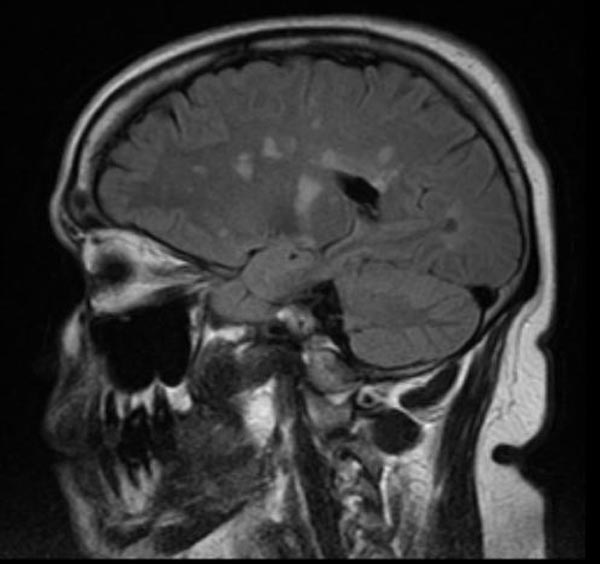
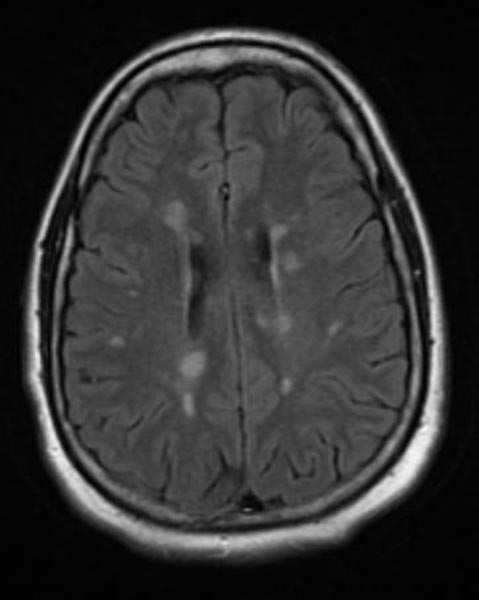
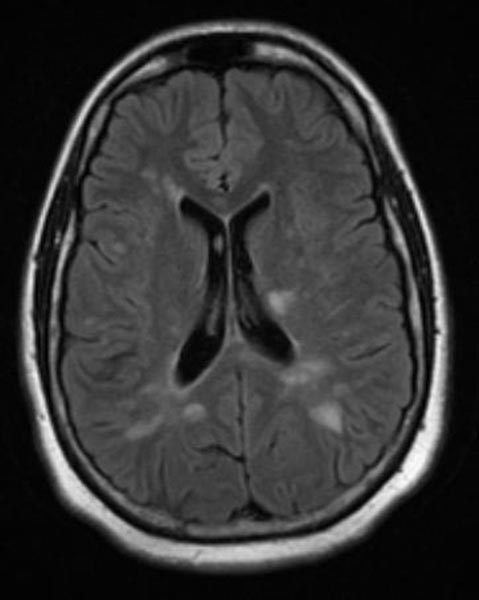
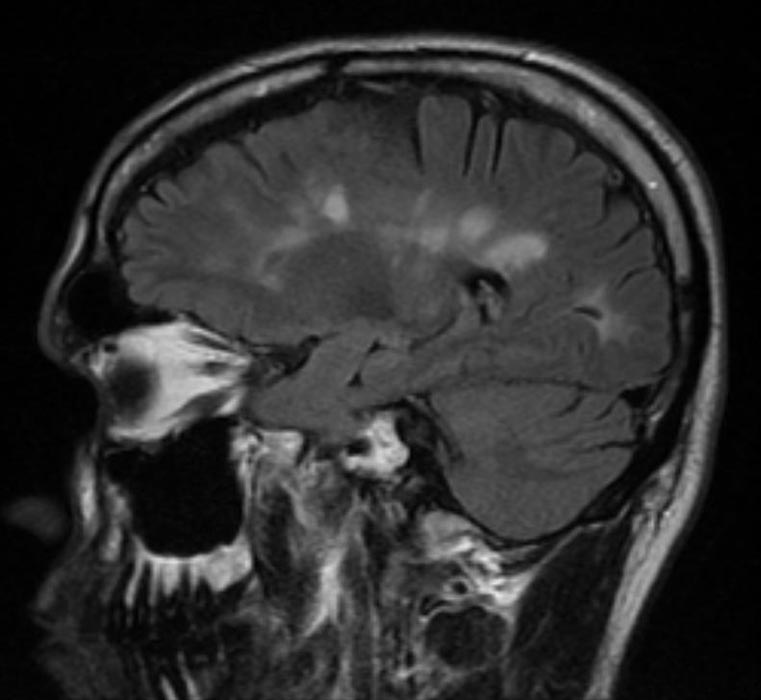
MRI
-
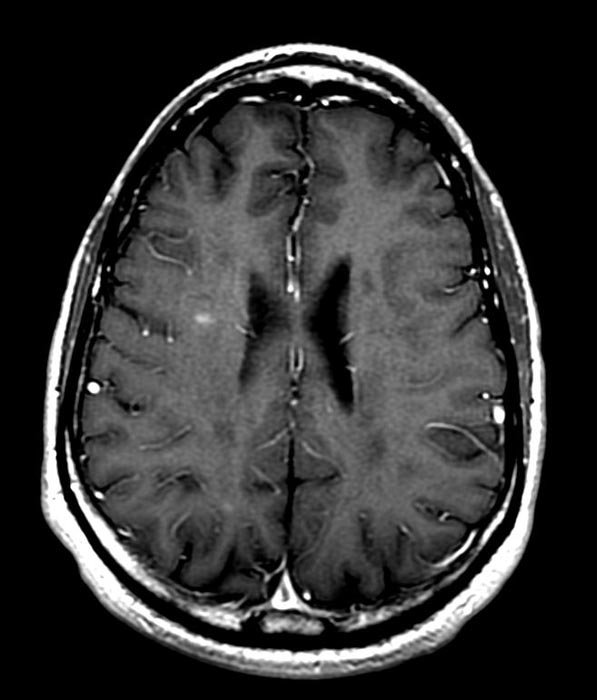
T1-weighted MRI scans (post-contrast) of same brain slice at monthly intervals. Bright spots indicate active lesions.
-
Multiple Sclerosis
Patient #1
-
Multiple sclerosis
-
Multiple sclerosis
-
Multiple sclerosis
-
Multiple sclerosis
-
Multiple sclerosis
-
Multiple sclerosis
Patient #2: Contrast enchancement of several lesions indicates active disease
-
-
-
-
GAD enhanced T1
Disease course and clinical subtypes
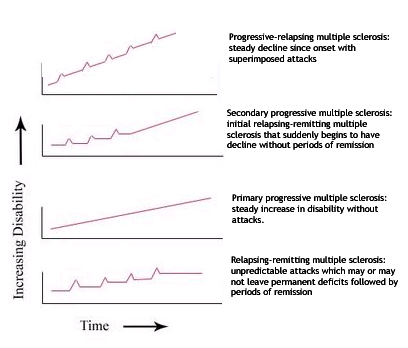
The course of MS is difficult to predict, and the disease may at times either lie dormant or progress steadily. Several subtypes, or patterns of progression, have been described. Subtypes use the past course of the disease in an attempt to predict the future course. Subtypes are important not only for prognosis but also for therapeutic decisions. In 1996 the United States National Multiple Sclerosis Society standardized the following four subtype definitions:[127]
- Relapsing-remitting
- Relapsing-remitting describes the initial course of 85% to 90% of individuals with MS. This subtype is characterized by unpredictable attacks (relapses) followed by periods of months to years of relative quiet (remission) with no new signs of disease activity. Deficits suffered during the attacks may either resolve or may be permanent. When deficits always resolve between attacks, this is referred to as "benign" MS.
- Secondary progressive
- Secondary progressive describes around 80% of those with initial relapsing-remitting MS, who then begin to have neurologic decline between their acute attacks without any definite periods of remission. This decline may include new neurologic symptoms, worsening cognitive function, or other deficits. Secondary progressive is the most common type of MS and causes the greatest amount of disability.
- Primary progressive
- Primary progressive describes the approximately 10% of individuals who never have remission after their initial MS symptoms. Decline occurs continuously without clear attacks. The primary progressive subtype tends to affect people who are older at disease onset.
- Progressive relapsing
- Progressive relapsing describes those individuals who, from the onset of their MS, have a steady neurologic decline but also suffer superimposed attacks; and is the least common of all subtypes
Nevertheless the earliest clinical presentation of relapsing-remitting MS (RRMS) is the clinically isolated syndrome (CIS). In CIS, there is a subacute attack suggestive of demyelination but the person does not fullfill the criteria for multiple sclerosis.[128] Several studies have shown that starting treatment with interferons during the initial attack can decrease the chance that a patient will develop MS.[129][130][131]
Special cases of the disease with non-standard behavior have also been described although many researchers believe they are different diseases. These cases are sometimes referred to as borderline forms of multiple sclerosis and are Neuromyelitis optica (NMO), Balo concentric sclerosis, Schilder's diffuse sclerosis and Marburg multiple sclerosis.[132]
Factors triggering a relapse
Multiple sclerosis relapses are often unpredictable and can occur without warning with no obvious inciting factors. Some attacks, however, are preceded by common triggers. In general, relapses occur more frequently during spring and summer than during autumn and winter. Infections, such as the common cold, influenza, and gastroenteritis, increase the risk for a relapse.[133] Emotional and physical stress may also trigger an attack,[134][135][136] as can severe illness of any kind. Statistically, there is no good evidence that either trauma or surgery trigger relapses.[137] People with MS can participate in sports, but they should probably avoid extremely strenuous exertion, such as marathon running. Heat can transiently increase symptoms, which is known as Uhthoff's phenomenon. This is why some people with MS avoid saunas or even hot showers. However, heat is not an established trigger of relapses.[138]
Pregnancy can directly affect the susceptibility for relapse. The last three months of pregnancy offer a natural protection against relapses. However, during the first few months after delivery, the risk for a relapse is increased 20%–40%. Pregnancy does not seem to influence long-term disability. Children born to mothers with MS are not at increased risk for birth defects or other problems.[139]
Many potential triggers have been examined and found not to influence relapse rates in MS. Influenza vaccination is safe, does not trigger relapses, and can therefore be recommended for people with MS. There is also no evidence that vaccines for hepatitis B, varicella, tetanus, or Bacille Calmette-Guerin (BCG—immunization for tuberculosis) increases the risk for relapse.[140]
Treatment
Although there is no known cure for multiple sclerosis, several therapies have proven helpful. The primary aims of therapy are returning function after an attack, preventing new attacks, and preventing disability. As with any medical treatment, medications used in the management of MS have several adverse effects, and many possible therapies are still under investigation. At the same time different alternative treatments are pursued by many patients, despite the paucity of supporting, comparable, replicated scientific study.
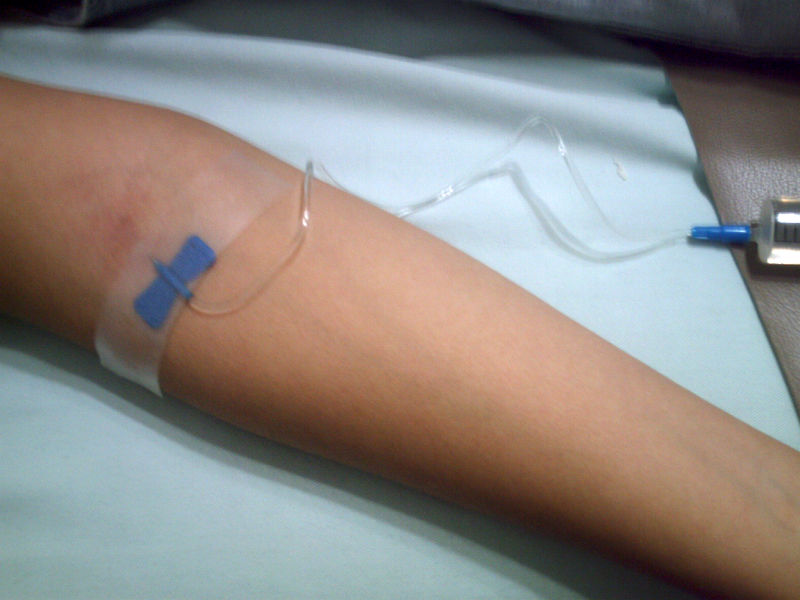
Management of acute attacks
During symptomatic attacks administration of high doses of intravenous corticosteroids, such as methylprednisolone,[141][142] is the routine therapy for acute relapses.The aim of this kind of treatment is to end the attack sooner and leave fewer lasting deficits in the patient. Although generally effective in the short term for relieving symptoms, corticosteroid treatments do not appear to have a significant impact on long-term recovery.[143] Potential side effects include osteoporosis[144] and impaired memory, being the latter reversible[145]
Disease modifying treatments
The earliest clinical presentation of relapsing-remitting MS (RRMS) is the clinically isolated syndrome (CIS). Several studies have shown that treatment with interferons during an initial attack can decrease the chance that a patient will develop MS.[146][147][131]
As of 2007, six disease-modifying treatments have been approved by regulatory agencies of different countries for relapsing-remitting MS. Three are interferons: two formulations of interferon beta-1a (trade names Avonex and Rebif) and one of interferon beta-1b (U.S. trade name Betaseron, in Europe and Japan Betaferon). A fourth medication is glatiramer acetate (Copaxone). The fifth medication, mitoxantrone, is an immunosuppressant also used in cancer chemotherapy. Finally, the sixth is natalizumab (marketed as Tysabri). All six medications are modestly effective at decreasing the number of attacks and slowing progression to disability, although they differ in their efficacy rate and studies of their long-term effects are still lacking.[148][149][150][151] Comparisons between immunomodulators (all but mitoxantrone) show that the most effective is natalizumab.[152] Mitoxantrone is probably the most effective of them all;[153] however, its use is limited by severe cardiotoxicity.[154]
Treatment of progressive MS is more difficult than relapsing-remitting MS. Mitoxantrone has shown positive effects in patients with a secondary progressive and progressive relapsing courses. It is moderately effective in reducing the progression of the disease and the frequency of relapses in patients in short-term follow-up.[151] On the other hand no treatment has been proven to modify the course of primary progresive MS.[155]
As with any medical treatment, these treatments have several adverse effects. One of the most common is irritation at the injection site. Interferons also produce symtoms similar to influenza; [156] while some patients taking glatiramer experience a post-injection reaction manifested by flushing, chest tightness, heart palpitations, breathlessness, and anxiety, which usually lasts less than thirty minutes.[149]. More dangerous are liver damage of interferons and mitoxantrone,[157][158][159] [160] the immunosuppressive effects and cardiac toxicity of the latter; [160] or the relation between natalizumab and some cases of progressive multifocal leukoencephalopathy in patients who had taken it in combination with interferons.[161][162]
Management of the effects of MS
Disease-modifying treatments only reduce the progression rate of the disease but do not stop it. As multiple sclerosis progresses, the symptomatology tends to increase. The disease is associated with a variety of symptoms and functional deficits that result in a range of progressive impairments and handicap. Management of these deficits is therefore very important. Both drug therapy and neurorehabilitation have shown to ease the burden of some symptoms, even though neither influence disease progression.[163] As for any patient with neurologic deficits, a multidisciplinary approach is key to limiting and overcoming disability; however there are particular difficulties in specifying a ‘core team’ because people with MS may need help from almost any health profession or service at some point.[59] Similarly for each symptom there are different treatment options. Treatments should therefore be individualized depending both on the patient and the physician
Therapies under investigation
Scientists continue their extensive efforts to create new and better therapies for MS. There are a number of treatments under investigation that may curtail attacks or improve function. Some of these treatments involve the combination of drugs that are already in use for multiple sclerosis, such as the combination of mitoxantrone and glatiramer acetate (Copaxone).[164] However most treatments already in clinical trials involve drugs that are used in other diseases or medications that have been designed specifically for MS. Finally, there are also many basic investigations that try to understand better the disease and in the future may help to find new treatments.
Alternative treatments
Different alternative treatments are pursued by many patients, despite the paucity of supporting, comparable, replicated scientific study. Examples are dietary regimens,[165], herbal medicine, including the use of marijuana to help alleviate symptoms,[166][167] or hyperbaric oxygenation.[168] On the other hand the therapeutic practice of martial arts such as tai chi, relaxation disciplines such as yoga, or general exercise, seem to mitigate fatigue and improve quality of life.[169]
Prognosis
The prognosis (the expected future course of the disease) for a person with multiple sclerosis depends on the subtype of the disease; the individual's sex, race, age, and initial symptoms; and the degree of disability the person experiences. The life expectancy of people with MS is now nearly the same as that of unaffected people. This is due mainly to improved methods of limiting disability, such as physical therapy, occupational therapy and speech therapy, along with more successful treatment of common complications of disability, such as pneumonia and urinary tract infections.[170] Nevertheless half of the deaths in people with MS are directly related to the consequences of the disease, while 15% more are due to suicide.[171]
- Individuals with progressive subtypes of MS, particularly the primary progressive subtype, have a more rapid decline in function. In the primary progressive subtype, supportive equipment (such as a wheelchair or standing frame) is often needed after six to seven years. However, when the initial disease course is the relapsing-remitting subtype, the average time until such equipment is needed is twenty years. This means that many individuals with MS will never need a wheelchair. There is also more cognitive impairment in the progressive forms than in the relapsing-remitting course.
- The earlier in life MS occurs, the slower disability progresses. Individuals who are older than fifty when diagnosed are more likely to experience a chronic progressive course, with more rapid progression of disability. Those diagnosed before age 35 have the best prognosis. Females generally have a better prognosis than males. Although individuals of African descent tend to develop MS less frequently, they are often older at the time of onset and may have a worse prognosis.
- Initial MS symptoms of visual loss or sensory problems, such as numbness or tingling, are markers for a relatively good prognosis, whereas difficulty walking and weakness are markers for a relatively poor prognosis. Better outcomes are also associated with the presence of only a single symptom at onset, the rapid development of initial symptoms, and the rapid regression of initial symptoms.
- The degree of disability varies among individuals with MS. In general, one of three individuals will still be able to work after 15–20 years. Fifteen percent of people diagnosed with MS never have a second relapse, and these people have minimal or no disability after ten years.[172] The degree of disability after five years correlates well with the degree of disability after fifteen years. This means that two-thirds of people with MS with low disability after five years will not get much worse during the next ten years. It should be noted that most of these outcomes were observed before the use of medications such as interferon, which can delay disease progression for several years.
Currently there are no clinically established laboratory investigations available that can predict prognosis or response to treatment. However, several promising approaches have been proposed. These include measurement of the two antibodies anti-myelin oligodendrocyte glycoprotein and anti-myelin basic protein, and measurement of TRAIL (TNF-related apoptosis-inducing ligand).[173]
Research directions
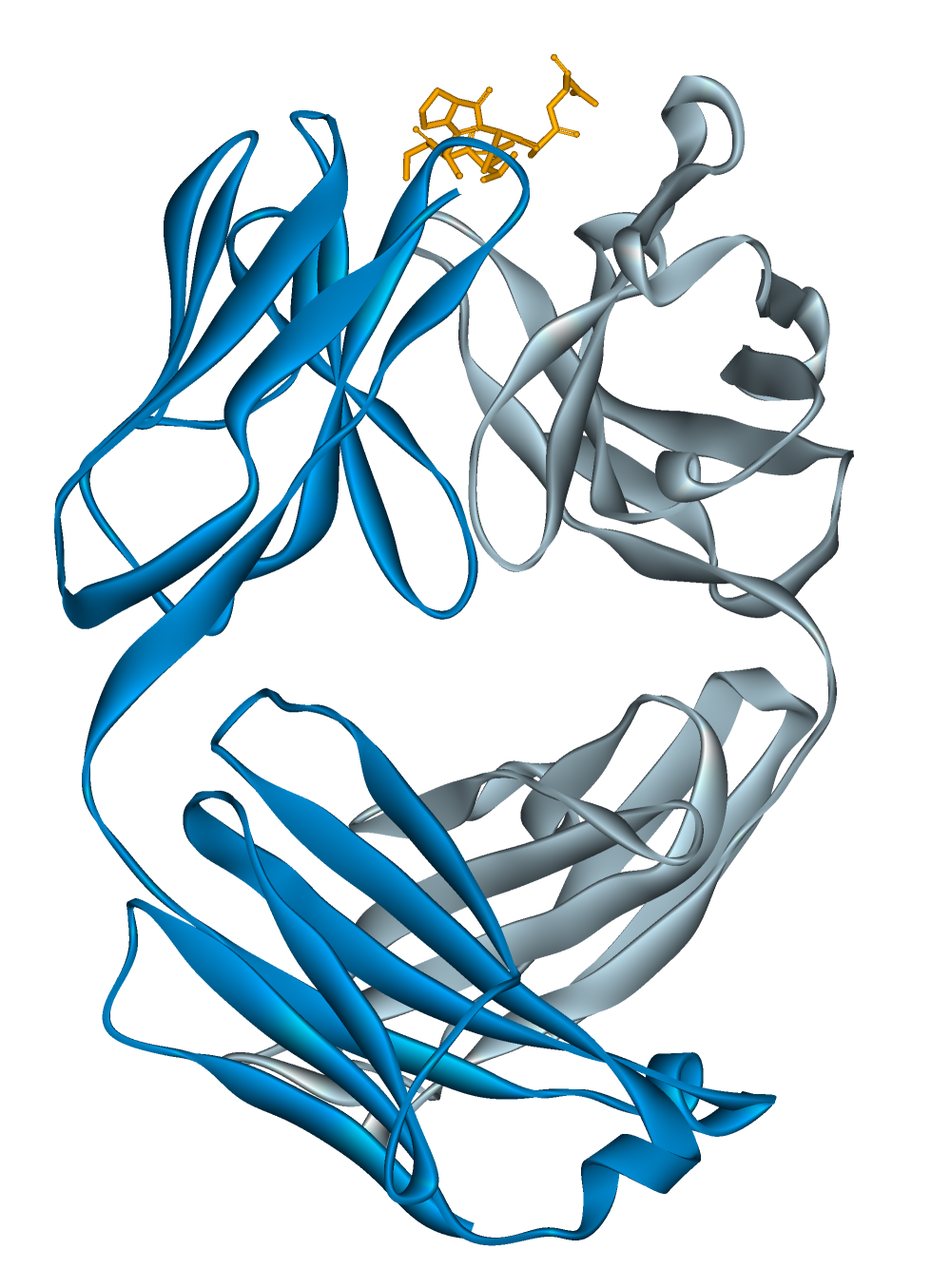
A number of treatments that may curtail attacks or improve function are under investigation. Some of these treatments involve the combination of drugs that are already in use for multiple sclerosis, such as the joint administration of mitoxantrone and glatiramer acetate (Copaxone).[174] However, most treatments already in clinical trials involve drugs that are used in other diseases. These are alemtuzumab (trade name Campath),[175] daclizumab (trade name Zenapax),[176] inosine,[177] BG00012,[178] fingolimod,[179] and teriflunomide, the active metabolite of the DMARD leflunomide. Alemtuzumab performed better than interferon beta-1a in relapsing-remitting MS reducing disability, imaging abnormalities and frequence of relapses, at the cost of increased autoimmunity problems. These included three cases of thrombocytopenic purpura which led to the suspension of the therapy.[180]
Other drugs in clinical trials have been designed specifically for MS, such as laquinimod,[181] and Neurovax.[182]
Low dose naltrexone has been prescribed off-label for certain autoimmune disorders, including MS, and there is anecdotal evidence of benefit,[183][184] but only two small clinical trials have been conducted (as on December 2008), one in San Francisco, USA,[185] the other for the primary progressive variety in Milan, Italy.[186]
New diagnostic and evolution evaluation methods are also being investigated. The measurement of antibodies against myelin proteins such as myelin oligodendrocyte glycoprotein and myelin basic protein could be useful for diagnosis. Optical coherence tomography of the eye's retina could be used as a measure of response to medication, axonal degeneration and brain atrophy.[187][188] Currently there are no clinically established laboratory investigations available that can predict prognosis. However, several promising approaches have been proposed, such as the measurement of a lipid-specific immunoglobulin M as predictor of long-term outcomes.[189]
Additional Images
-
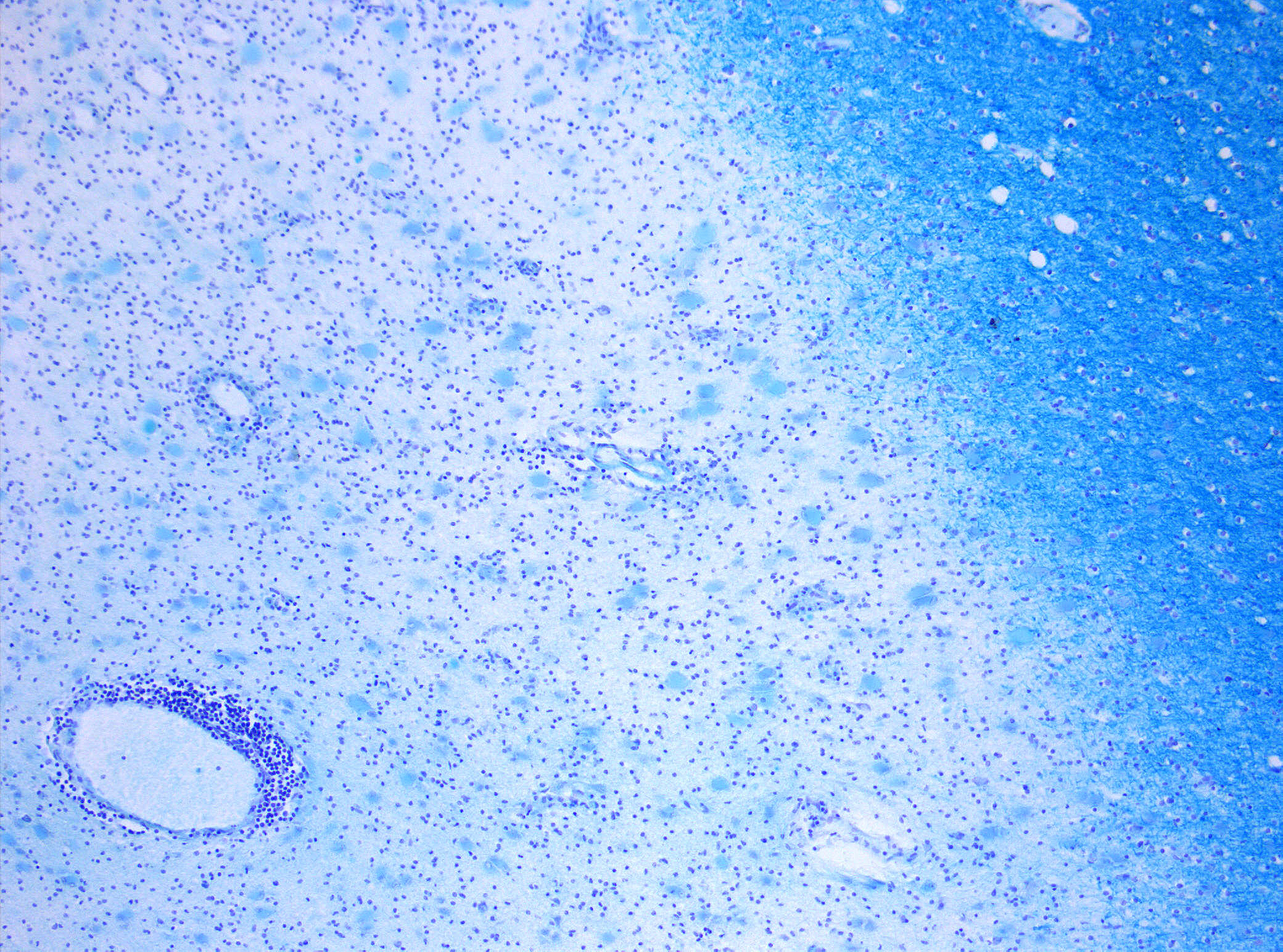
Demyelinization in MS. On Klüver-Barrera myelin staining, decoloration in the area of the lesion can be appreciated (Original scale 1:100).
-
Main symptoms of multiple sclerosis.
-
World map showing that risk for MS increases with greater distance from the equator
-
Detail of drawing from Carswell book depicting multiple sclerosis lesions in the brain stem and spinal cord (1838)
-
Chemical structure of alemtuzumab.
References
- ↑ Rosati G (2001). "The prevalence of multiple sclerosis in the world: an update". Neurol. Sci. 22 (2): 117–39. PMID 11603614.
- ↑ Epidemiology and multiple sclerosis. a personal review
- ↑ Marrie, RA. Environmental risk factors in multiple sclerosis aetiology. Lancet Neurol. 2004 Dec;3(12):709-18. Review. PMID 15556803
- ↑ Hammond SR, English DR, McLeod JG (2000). "The age-range of risk of developing multiple sclerosis: evidence from a migrant population in Australia". Brain. 123 ( Pt 5): 968–74. PMID 10775541.
- ↑ Rothwell PM, Charlton D (1998). "High incidence and prevalence of multiple sclerosis in south east Scotland: evidence of a genetic predisposition". J. Neurol. Neurosurg. Psychiatr. 64 (6): 730–5. PMID 9647300.
- ↑ Sadovnick, AD, Ebers, GC, Dyment, DA, Risch, NJ. Evidence for genetic basis of multiple sclerosis. The Canadian Collaborative Study Group. Lancet 1996; 347:1728. PMID 8656905
- ↑ Weinshenker B (2005). "Western vs optic-spinal MS: two diseases, one treatment?". Neurology. 64 (4): 594–5. PMID 15728277.
- ↑ Charcot, J. Histologie de la sclerose en plaques. Gazette des hopitaux, Paris, 1868; 41: 554–555.
- ↑ Poser C (1994). "The dissemination of multiple sclerosis: a Viking saga? A historical essay". Ann. Neurol. 36 Suppl 2: S231–43. PMID 7998792.
- ↑ Firth, D (1948). The Case of August D`Esté. Cambridge: Cambridge University Press.
- ↑ Rentzos M, Nikolaou C, Anagnostouli M, Rombos A, Tsakanikas K, Economou M, Dimitrakopoulos A, Karouli M, Vassilopoulos D (2006). "Serum uric acid and multiple sclerosis". Clinical neurology and neurosurgery. 108 (6): 527–31. PMID 16202511.
- ↑ Lucchinetti, C. Bruck, W. Parisi, J. Scherhauer, B. Rodriguez, M. Lassmann, H.Heterogeneity of multiple sclerosis lesions: implications for the pathogenesis of demyelination Ann Neurol, 2000; 47(6):707-17. PMID 10852536
- ↑ Pascual AM, Martínez-Bisbal MC, Boscá I; et al. (2007). "Axonal loss is progressive and partly dissociated from lesion load in early multiple sclerosis". Neurology. 69 (1): 63–7. doi:10.1212/01.wnl.0000265054.08610.12. PMID 17606882.
- ↑ Lassmann H (2007). "Experimental models of multiple sclerosis". Rev. Neurol. (Paris). 163 (6–7): 651–5. PMID 17607184.
- ↑ Peter Behan and Abhijit Chaudhuri (2002). "The pathogenesis of multiple sclerosis revisited" (PDF). J R Coll Physicians Edinb. 32: 244–265.
- ↑ Chaudhuri A, Behan P (2004). "Multiple sclerosis is not an autoimmune disease". Arch. Neurol. 61 (10): 1610–2. PMID 15477520.
- ↑ Altmann D (2005). "Evaluating the evidence for multiple sclerosis as an autoimmune disease". Arch. Neurol. 62 (4): 688, author reply 688-9. PMID 15824275.
- ↑ van der Mei IA, Ponsonby AL, Dwyer T; et al. (2003). "Past exposure to sun, skin phenotype, and risk of multiple sclerosis: case-control study". BMJ. 327 (7410): 316. doi:10.1136/bmj.327.7410.316. PMID 12907484.
- ↑ Munger KL, Levin LI, Hollis BW, Howard NS, Ascherio A (2006). "Serum 25-hydroxyvitamin D levels and risk of multiple sclerosis". JAMA. 296 (23): 2832–8. doi:10.1001/jama.296.23.2832. PMID 17179460.
- ↑ Childhood sun exposure influences risk of multiple sclerosis in monozygotic twins. Talat Islam, MBBS, PhD, W. James Gauderman, PhD, Wendy Cozen, DO, MPH and Thomas M. Mack, MD, MPH. Neurology 2007;69:381-388
- ↑ Sunshine 'protective' against MS. BBC News, 28 July 2007, 23:40
- ↑ Levin LI, Munger KL, Rubertone MV; et al. (2005). "Temporal relationship between elevation of epstein-barr virus antibody titers and initial onset of neurological symptoms in multiple sclerosis". JAMA. 293 (20): 2496–500. doi:10.1001/jama.293.20.2496. PMID 15914750.
- ↑ Brorson O, Brorson SH, Henriksen TH, Skogen PR, Schøyen R (2001). "Association between multiple sclerosis and cystic structures in cerebrospinal fluid". Infection. 29 (6): 315–9. PMID 11787831.
- ↑ Yao SY, Stratton CW, Mitchell WM, Sriram S (2001). "CSF oligoclonal bands in MS include antibodies against Chlamydophila antigens". Neurology. 56 (9): 1168–76. PMID 11342681.
- ↑ Li J, Johansen C, Bronnum-Hansen H, Stenager E, Koch-Henriksen N, Olsen J (2004). "The risk of multiple sclerosis in bereaved parents: A nationwide cohort study in Denmark". Neurology. 62 (5): 726–9. PMID 15007121.
- ↑ Franklin GM, Nelson L (2003). "Environmental risk factors in multiple sclerosis: causes, triggers, and patient autonomy". Neurology. 61 (8): 1032–4. PMID 14581658.
- ↑ "Risk Alleles for Multiple Sclerosis Identified by a Genomewide Study". N Engl J Med. 2007. doi:10.1056/NEJMoa073493. PMID 17660530.
- ↑ Kurtzke JF (1983). "Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS)". Neurology. 33 (11): 1444–52. PMID 6685237.
- ↑ Navarro S, Mondéjar-Marín B, Pedrosa-Guerrero A, Pérez-Molina I, Garrido-Robres J, Alvarez-Tejerina A. "[Aphasia and parietal syndrome as the presenting symptoms of a demyelinating disease with pseudotumoral lesions]". Rev Neurol. 41 (10): 601–3. PMID 16288423.
- ↑ Jongen P (2006). "Psychiatric onset of multiple sclerosis". J Neurol Sci. 245 (1–2): 59–62. PMID 16631798.
- ↑ Paty D, Studney D, Redekop K, Lublin F. MS COSTAR: a computerized patient record adapted for clinical research purposes. Ann Neurol 1994;36 Suppl:S134-5. PMID 8017875
- ↑ Hennessey A, Robertson NP, Swingler R, Compston DA (1999). "Urinary, faecal and sexual dysfunction in patients with multiple sclerosis". J. Neurol. 246 (11): 1027–32. PMID 10631634.
- ↑ Burguera-Hernández JA (2000). "[Urinary alterations in multiple sclerosis]". Revista de neurologia (in Spanish; Castilian). 30 (10): 989–92. PMID 10919202.
- ↑ Betts CD, D'Mellow MT, Fowler CJ (1993). "Urinary symptoms and the neurological features of bladder dysfunction in multiple sclerosis". J. Neurol. Neurosurg. Psychiatr. 56 (3): 245–50. PMID 8459239.
- ↑ Nour S, Svarer C, Kristensen JK, Paulson OB, Law I (2000). "Cerebral activation during micturition in normal men". Brain. 123 ( Pt 4): 781–9. PMID 10734009.
- ↑ Ayuso-Peralta L, de Andrés C (2002). "[Symptomatic treatment of multiple sclerosis]". Revista de neurologia (in Spanish; Castilian). 35 (12): 1141–53. PMID 12497297.
- ↑ Information from the USA National library of medicine on alfuzosin [1]
- ↑ Information from the USA National library of medicine on trospium [2]
- ↑ Information from the USA National library of medicine on flavoxate [3]
- ↑ Bosma R, Wynia K, Havlíková E, De Keyser J, Middel B (2005). "Efficacy of desmopressin in patients with multiple sclerosis suffering from bladder dysfunction: a meta-analysis". Acta Neurol. Scand. 112 (1): 1–5. doi:10.1111/j.1600-0404.2005.00431.x. PMID 15932348.
- ↑ Information from the USA National library of medicine on desmopressin [4]
- ↑ Frances M Diro (2006) "Urological Management in Neurological Disease". [5]
- ↑ Rao S, Leo G, Bernardin L, Unverzagt F (1991). "Cognitive dysfunction in multiple sclerosis. I. Frequency, patterns, and prediction". Neurology. 41 (5): 685–91. PMID 2027484.
- ↑ "Attention impairment in recently diagnosed multiple sclerosis". Eur J Neurol. 5 (1): 61–66. 1998. PMID 10210813.
- ↑ Achiron A, Barak Y (2003). "Cognitive impairment in probable multiple sclerosis". J Neurol Neurosurg Psychiatry. 74 (4): 443–6. PMID 12640060.
- ↑ Bobholz J, Rao S (2003). "Cognitive dysfunction in multiple sclerosis: a review of recent developments". Curr Opin Neurol. 16 (3): 283–8. PMID 12858063.
- ↑ Amato M, Ponziani G, Siracusa G, Sorbi S (2001). "Cognitive dysfunction in early-onset multiple sclerosis: a reappraisal after 10 years". Arch Neurol. 58 (10): 1602–6. PMID 11594918.
- ↑ Shawaryn M, Schultheis M, Garay E, Deluca J (2002). "Assessing functional status: exploring the relationship between the multiple sclerosis functional composite and driving". Arch Phys Med Rehabil. 83 (8): 1123–9. PMID 12161835.
- ↑ Montalban X, Rio J (2006). "Interferons and cognition". J Neurol Sci. 245 (1–2): 137–40. PMID 16626757.
- ↑ Christodoulou C, Melville P, Scherl W, Macallister W, Elkins L, Krupp L (2006). "Effects of donepezil on memory and cognition in multiple sclerosis". J Neurol Sci. 245 (1–2): 127–36. PMID 16626752.
- ↑ Porcel J, Montalban X (2006). "Anticholinesterasics in the treatment of cognitive impairment in multiple sclerosis". J Neurol Sci. 245 (1–2): 177–81. PMID 16674980.
- ↑ Information from the USA National library of medicine on donepezil [6]
- ↑ Sadovnick A, Remick R, Allen J, Swartz E, Yee I, Eisen K, Farquhar R, Hashimoto S, Hooge J, Kastrukoff L, Morrison W, Nelson J, Oger J, Paty D (1996). "Depression and multiple sclerosis". Neurology. 46 (3): 628–32. PMID 8618657.
- ↑ Patten S, Beck C, Williams J, Barbui C, Metz L (2003). "Major depression in multiple sclerosis: a population-based perspective". Neurology. 61 (11): 1524–7. PMID 14663036.
- ↑ Siegert R, Abernethy D (2005). "Depression in multiple sclerosis: a review". J. Neurol. Neurosurg. Psychiatr. 76 (4): 469–75. PMID 15774430.
- ↑ Sadovnick A, Eisen K, Ebers G, Paty D (1991). "Cause of death in patients attending multiple sclerosis clinics". Neurology. 41 (8): 1193–6. PMID 1866003.
- ↑ Bakshi R (2003). "Fatigue associated with multiple sclerosis: diagnosis, impact and management". Mult. Scler. 9 (3): 219–27. PMID 12814166.
- ↑ Mohr DC, Hart SL, Goldberg A (2003). "Effects of treatment for depression on fatigue in multiple sclerosis". Psychosomatic medicine. 65 (4): 542–7. PMID 12883103.
- ↑ 59.0 59.1 59.2 59.3 The Royal College of Physicians (2004). Multiple Sclerosis. National clinical guideline for diagnosis and management in primary and secondary care. Salisbury, Wiltshire: Sarum ColourView Group. ISBN 1 86016 182 0.Free full text(2004-08-13). Retrieved on 2007-10-01.
- ↑ Pucci E, Branãs P, D'Amico R, Giuliani G, Solari A, Taus C (2007). "Amantadine for fatigue in multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD002818. doi:10.1002/14651858.CD002818.pub2. PMID 17253480.
- ↑ Amantadine. US National Library of Medicine (Medline) (2003-04-01). Retrieved on 2007-10-07.
- ↑ Weinshenker BG, Penman M, Bass B, Ebers GC, Rice GP (1992). "A double-blind, randomized, crossover trial of pemoline in fatigue associated with multiple sclerosis". Neurology. 42 (8): 1468–71. PMID 1641137.
- ↑ Pemoline. US National Library of Medicine (Medline) (2006-01-01). Retrieved on 2007-10-07.
- ↑ Mathiowetz VG, Finlayson ML, Matuska KM, Chen HY, Luo P (2005). "Randomized controlled trial of an energy conservation course for persons with multiple sclerosis". Mult. Scler. 11 (5): 592–601. PMID 16193899.
- ↑ Matuska K, Mathiowetz V, Finlayson M (2007). "Use and perceived effectiveness of energy conservation strategies for managing multiple sclerosis fatigue". The American journal of occupational therapy. : official publication of the American Occupational Therapy Association. 61 (1): 62–9. PMID 17302106.
- ↑ Leigh RJ, Averbuch-Heller L, Tomsak RL, Remler BF, Yaniglos SS, Dell'Osso LF (1994). "Treatment of abnormal eye movements that impair vision: strategies based on current concepts of physiology and pharmacology". Ann. Neurol. 36 (2): 129–41. PMID 8053648.
- ↑ Starck M, Albrecht H, Pöllmann W, Straube A, Dieterich M (1997). "Drug therapy for acquired pendular nystagmus in multiple sclerosis". J. Neurol. 244 (1): 9–16. PMID 9007739.
- ↑ Clanet MG, Brassat D (2000). "The management of multiple sclerosis patients". Curr. Opin. Neurol. 13 (3): 263–70. PMID 10871249.
- ↑ Menon GJ, Thaller VT (2002). "Therapeutic external ophthalmoplegia with bilateral retrobulbar botulinum toxin- an effective treatment for acquired nystagmus with oscillopsia". Eye (London, England). 16 (6): 804–6. PMID 12439689.
- ↑ Jain S, Proudlock F, Constantinescu CS, Gottlob I (2002). "Combined pharmacologic and surgical approach to acquired nystagmus due to multiple sclerosis". Am. J. Ophthalmol. 134 (5): 780–2. PMID 12429265.
- ↑ Weinshenker BG, Bass B, Rice GP; et al. (1989). "The natural history of multiple sclerosis: a geographically based study. I. Clinical course and disability". Brain. 112 ( Pt 1): 133–46. PMID 2917275.
- ↑ Freeman JA (2001). "Improving mobility and functional independence in persons with multiple sclerosis". J. Neurol. 248 (4): 255–9. PMID 11374088.
- ↑ Beck RW, Trobe JD (1995). "What we have learned from the Optic Neuritis Treatment Trial". Ophthalmology. 102 (10): 1504–8. PMID 9097798.
- ↑ "The 5-year risk of MS after optic neuritis: experience of the optic neuritis treatment trial. 1997". Neurology. 57 (12 Suppl 5): S36–45. 2001. PMID 11902594.
- ↑ Stenager E, Knudsen L, Jensen K (1995). "Acute and chronic pain syndromes in multiple sclerosis. A 5-year follow-up study". Italian journal of neurological sciences. 16 (9): 629–32. PMID 8838789.
- ↑ Archibald CJ, McGrath PJ, Ritvo PG; et al. (1994). "Pain prevalence, severity and impact in a clinic sample of multiple sclerosis patients". Pain. 58 (1): 89–93. PMID 7970843.
- ↑ Clanet MG, Brassat D (2000). "The management of multiple sclerosis patients". Curr. Opin. Neurol. 13 (3): 263–70. PMID 10871249.
- ↑ Pöllmann W, Feneberg W, Erasmus LP (2004). "[Pain in multiple sclerosis--a still underestimated problem. The 1 year prevalence of pain syndromes, significance and quality of care of multiple sclerosis inpatients]". Der Nervenarzt (in German). 75 (2): 135–40. doi:10.1007/s00115-003-1656-5. PMID 14770283.
- ↑ Kerns RD, Kassirer M, Otis J (2002). "Pain in multiple sclerosis: a biopsychosocial perspective". Journal of rehabilitation research and development. 39 (2): 225–32. PMID 12051466.
- ↑ Brisman R (1987). "Trigeminal neuralgia and multiple sclerosis". Arch. Neurol. 44 (4): 379–81. PMID 3493757.
- ↑ Bayer DB, Stenger TG (1979). "Trigeminal neuralgia: an overview". Oral Surg. Oral Med. Oral Pathol. 48 (5): 393–9. PMID 226915.
- ↑ Information from the USA National library of medicine on carbamazepine [7]
- ↑ Information from the USA National library of medicine on phenytoin [8]
- ↑ Information from the USA National library of medicine on gabapentin [9]
- ↑ Solaro C, Messmer Uccelli M, Uccelli A, Leandri M, Mancardi GL (2000). "Low-dose gabapentin combined with either lamotrigine or carbamazepine can be useful therapies for trigeminal neuralgia in multiple sclerosis". Eur. Neurol. 44 (1): 45–8. PMID 10894995.
- ↑ Kondziolka D, Lunsford LD, Bissonette DJ (1994). "Long-term results after glycerol rhizotomy for multiple sclerosis-related trigeminal neuralgia". The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques. 21 (2): 137–40. PMID 8087740.
- ↑ Athanasiou TC, Patel NK, Renowden SA, Coakham HB (2005). "Some patients with multiple sclerosis have neurovascular compression causing their trigeminal neuralgia and can be treated effectively with MVD: report of five cases". British journal of neurosurgery. 19 (6): 463–8. doi:10.1080/02688690500495067. PMID 16574557.
- ↑ Eldridge PR, Sinha AK, Javadpour M, Littlechild P, Varma TR (2003). "Microvascular decompression for trigeminal neuralgia in patients with multiple sclerosis". Stereotactic and functional neurosurgery. 81 (1–4): 57–64. doi:10.1159/000075105. PMID 14742965.
- ↑ Gutrecht JA, Zamani AA, Slagado ED (1993). "Anatomic-radiologic basis of Lhermitte's sign in multiple sclerosis". Arch. Neurol. 50 (8): 849–51. PMID 8352672.
- ↑ Al-Araji AH, Oger J (2005). "Reappraisal of Lhermitte's sign in multiple sclerosis". Mult. Scler. 11 (4): 398–402. PMID 16042221.
- ↑ Sandyk R, Dann LC (1995). "Resolution of Lhermitte's sign in multiple sclerosis by treatment with weak electromagnetic fields". Int. J. Neurosci. 81 (3–4): 215–24. PMID 7628912.
- ↑ Kanchandani R, Howe JG (1982). "Lhermitte's sign in multiple sclerosis: a clinical survey and review of the literature". J. Neurol. Neurosurg. Psychiatr. 45 (4): 308–12. PMID 7077340.
- ↑ Information from the USA National library of medicine on clonazepam[10]
- ↑ Information from the USA National library of medicine on amitriptyline[11]
- ↑ Moulin DE, Foley KM, Ebers GC (1988). "Pain syndromes in multiple sclerosis". Neurology. 38 (12): 1830–4. PMID 2973568.
- ↑ O'Leary, M., Heyman, R., Erickson, J., Chancellor, M.B.: Premature ejaculation and MS: A Review, Consortium of MS Centers, http://www.mscare.org, June 2007
- ↑ Cardini RG, Crippa AC, Cattaneo D (2000). "Update on multiple sclerosis rehabilitation". J. Neurovirol. 6 Suppl 2: S179–85. PMID 10871810.
- ↑ ; Baclofen oral. US National Library of Medicine (Medline) (2003-04-01). Retrieved on 2007-10-17.
- ↑ Dantrolene oral. US National Library of Medicine (Medline) (2003-04-01). Retrieved on 2007-10-17.
- ↑ Diazepam. US National Library of Medicine (Medline) (2005-07-01). Retrieved on 2007-10-17.
- ↑ Tizanidine. US National Library of Medicine (Medline) (2005-07-01). Retrieved on 2007-10-17.
- ↑ Beard S, Hunn A, Wight J (2003). "Treatments for spasticity and pain in multiple sclerosis: a systematic review". Health technology assessment (Winchester, England). 7 (40): iii, ix–x, 1–111. PMID 14636486.
- ↑ Paisley S, Beard S, Hunn A, Wight J (2002). "Clinical effectiveness of oral treatments for spasticity in multiple sclerosis: a systematic review". Mult. Scler. 8 (4): 319–29. PMID 12166503.
- ↑ Becker WJ, Harris CJ, Long ML, Ablett DP, Klein GM, DeForge DA (1995). "Long-term intrathecal baclofen therapy in patients with intractable spasticity". The Canadian journal of neurological sciences. Le journal canadien des sciences neurologiques. 22 (3): 208–17. PMID 8529173.
- ↑ Koch M, Mostert J, Heersema D, De Keyser J (2007). "Tremor in multiple sclerosis". J. Neurol. 254 (2): 133–45. doi:10.1007/s00415-006-0296-7. PMID 17318714.
- ↑ Bozek CB, Kastrukoff LF, Wright JM, Perry TL, Larsen TA (1987). "A controlled trial of isoniazid therapy for action tremor in multiple sclerosis". J. Neurol. 234 (1): 36–9. PMID 3546605.
- ↑ Duquette P, Pleines J, du Souich P (1985). "Isoniazid for tremor in multiple sclerosis: a controlled trial". Neurology. 35 (12): 1772–5. PMID 3906430.
- ↑ Hallett M, Lindsey JW, Adelstein BD, Riley PO (1985). "Controlled trial of isoniazid therapy for severe postural cerebellar tremor in multiple sclerosis". Neurology. 35 (9): 1374–7. PMID 3895037.
- ↑ Information from the USA National library of medicine on Isoniazid [12]
- ↑ Information from the USA National library of medicine on carbamazepine [13]
- ↑ Koller WC (1984). "Pharmacologic trials in the treatment of cerebellar tremor". Arch. Neurol. 41 (3): 280–1. PMID 6365047.
- ↑ Sechi GP, Zuddas M, Piredda M, Agnetti V, Sau G, Piras ML, Tanca S, Rosati G (1989). "Treatment of cerebellar tremors with carbamazepine: a controlled trial with long-term follow-up". Neurology. 39 (8): 1113–5. PMID 2668787.
- ↑ Information from the USA National library of medicine on propanolol [14]
- ↑ Aisen ML, Holzer M, Rosen M, Dietz M, McDowell F (1991). "Glutethimide treatment of disabling action tremor in patients with multiple sclerosis and traumatic brain injury". Arch. Neurol. 48 (5): 513–5. PMID 2021365.
- ↑ Mills RJ, Yap L, Young CA (2007). "Treatment for ataxia in multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD005029. doi:10.1002/14651858.CD005029.pub2. PMID 17253537.
- ↑ Aisen ML, Arnold A, Baiges I, Maxwell S, Rosen M (1993). "The effect of mechanical damping loads on disabling action tremor". Neurology. 43 (7): 1346–50. PMID 8327136.
- ↑ Bittar RG, Hyam J, Nandi D, Wang S, Liu X, Joint C, Bain PG, Gregory R, Stein J, Aziz TZ (2005). "Thalamotomy versus thalamic stimulation for multiple sclerosis tremor". Journal of clinical neuroscience : official journal of the Neurosurgical Society of Australasia. 12 (6): 638–42. doi:10.1016/j.jocn.2004.09.008. PMID 16098758.
- ↑ McDonald WI; Compston A; Edan G; Goodkin D; Hartung HP; Lublin FD; McFarland HF; Paty DW; Polman CH; Reingold SC; Sandberg-Wollheim M; Sibley W; Thompson A; van den Noort S; Weinshenker BY; Wolinsky JS. Recommended diagnostic criteria for multiple sclerosis: guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann Neurol 2001 Jul;50(1):121-7 PMID 11456302
- ↑ Rudick, RA, Whitaker, JN. Cerebrospinal fluid tests for multiple sclerosis. In Scheinberg, P (Ed). Neurology/neurosurgery update series, Vol. 7, CPEC. Princeton, NJ 1987
- ↑ Gronseth GS; Ashman EJ. Practice parameter: the usefulness of evoked potentials in identifying clinically silent lesions in patients with suspected multiple sclerosis (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000 May 9;54(9):1720–5. PMID 10802774
- ↑ Gordon-Lipkin E, Chodkowski B, Reich DS; et al. (2007). "Retinal nerve fiber layer is associated with brain atrophy in multiple sclerosis". Neurology. 69 (16): 1603–09. PMID 17938370. Unknown parameter
|month=ignored (help) - ↑ Albrecht P, Fröhlich R, Hartung HP, Kieseier BC, Methner A (2007). "Optical coherence tomography measures axonal loss in multiple sclerosis independently of optic neuritis". J Neurol. Online. doi:10.1007/s00415-007-0538-3. PMID 17987252.
- ↑ Garcia-Monco JC; Miro Jornet J; Fernandez Villar B; Benach JL; Guerrero Espejo A; Berciano JA. [Multiple sclerosis or Lyme disease? a diagnosis problem of exclusion] Med Clin (Barc) 1990 May 12;94(18):685-8. PMID 2388492
- ↑ Hansen K; Cruz M; Link H. Oligoclonal Borrelia burgdorferi-specific IgG antibodies in cerebrospinal fluid in Lyme neuroborreliosis. J Infect Dis 1990 Jun;161(6):1194-202. PMID 2345300
- ↑ Schluesener HJ; Martin R; Sticht-Groh V. Autoimmunity in Lyme disease: molecular cloning of antigens recognized by antibodies in the cerebrospinal fluid. Autoimmunity 1989 2(4):323-30. PMID 2491615
- ↑ Kohler J; Kern U; Kasper J; Rhese-Kupper B; Thoden U. Chronic central nervous system involvement in Lyme borreliosis Neurology 1988 Jun;38(6):863-7. PMID 3368066
- ↑ Lublin FD; Reingold SC. Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology 1996 Apr;46(4):907-11. PMID 8780061
- ↑ Miller D, Barkhof F, Montalban X, Thompson A, Filippi M (2005). "Clinically isolated syndromes suggestive of multiple sclerosis, part I: natural history, pathogenesis, diagnosis, and prognosis". Lancet neurology. 4 (5): 281–8. doi:10.1016/S1474-4422(05)70071-5. PMID 15847841.
- ↑ Jacobs LD; Beck RW; Simon JH; Kinkel RP; Brownscheidle CM; Murray TJ; Simonian NA; Slasor PJ; Sandrock AW. Intramuscular interferon beta-1a therapy initiated during a first demyelinating event in multiple sclerosis. CHAMPS Study Group. N Engl J Med 2000 September 28;343(13):898–904. PMID 11006365
- ↑ Comi G; Filippi M; Barkhof F; Durelli L; Edan G; Fernandez O; Hartung H; Seeldrayers P; Sorensen PS; Rovaris M; Martinelli V; Hommes OR.Effect of early interferon treatment on conversion to definite multiple sclerosis: a randomised study. Lancet 2001 May 19;357(9268):1576–82. PMID 11377645
- ↑ 131.0 131.1 Kappos L, Freedman MS, Polman CH; et al. (2007). "Effect of early versus delayed interferon beta-1b treatment on disability after a first clinical event suggestive of multiple sclerosis: a 3-year follow-up analysis of the BENEFIT study". Lancet. 370 (9585): 389–97. doi:10.1016/S0140-6736(07)61194-5. PMID 17679016.
- ↑ Borderline forms of MS, Fontaine, B., Federation de Neurologie, INSERM U546, Groupe Hospitalier, Faculte de Medecine Pitie-Salpetriere, Paris [15]
- ↑ Confavreux C (2002). "Infections and the risk of relapse in multiple sclerosis". Brain. 125 (Pt 5): 933–4. PMID 11960883.
- ↑ Buljevac D, Hop WC, Reedeker W; et al. (2003). "Self reported stressful life events and exacerbations in multiple sclerosis: prospective study". BMJ. 327 (7416): 646. doi:10.1136/bmj.327.7416.646. PMID 14500435.
- ↑ Brown RF, Tennant CC, Sharrock M, Hodgkinson S, Dunn SM, Pollard JD (2006). "Relationship between stress and relapse in multiple sclerosis: Part I. Important features". Mult. Scler. 12 (4): 453–64. PMID 16900759.
- ↑ Brown RF, Tennant CC, Sharrock M, Hodgkinson S, Dunn SM, Pollard JD (2006). "Relationship between stress and relapse in multiple sclerosis: Part II. Direct and indirect relationships". Mult. Scler. 12 (4): 465–75. PMID 16900760.
- ↑ Martinelli V (2000). "Trauma, stress and multiple sclerosis". Neurol. Sci. 21 (4 suppl 2): S849–52. PMID 11205361.
- ↑ Tataru N, Vidal C, Decavel P, Berger E, Rumbach L (2006). "Limited impact of the summer heat wave in France (2003) on hospital admissions and relapses for multiple sclerosis". Neuroepidemiology. 27 (1): 28–32. doi:10.1159/000094233. PMID 16804331.
- ↑ Worthington J, Jones R, Crawford M, Forti A (1994). "Pregnancy and multiple sclerosis--a 3-year prospective study". J. Neurol. 241 (4): 228–33. PMID 8195822.
- ↑ Confavreux C, Suissa S, Saddier P, Bourdès V, Vukusic S (2001). "Vaccinations and the risk of relapse in multiple sclerosis. Vaccines in Multiple Sclerosis Study Group". N. Engl. J. Med. 344 (5): 319–26. PMID 11172162.
- ↑ Methylprednisolone Oral. US National Library of Medicine (Medline) (2003-04-01). Retrieved on 2007-09-01.
- ↑ Methylprednisolone Sodium Succinate Injection. US National Library of Medicine (Medline) (2003-04-01). Retrieved on 2007-09-01.
- ↑ Brusaferri F, Candelise L (2000). "Steroids for multiple sclerosis and optic neuritis: a meta-analysis of randomized controlled clinical trials". J. Neurol. 247 (6): 435–42. PMID 10929272.
- ↑ Dovio A, Perazzolo L, Osella G; et al. (2004). "Immediate fall of bone formation and transient increase of bone resorption in the course of high-dose, short-term glucocorticoid therapy in young patients with multiple sclerosis". J. Clin. Endocrinol. Metab. 89 (10): 4923–8. doi:10.1210/jc.2004-0164. PMID 15472186.
- ↑ Uttner I, Müller S, Zinser C; et al. (2005). "Reversible impaired memory induced by pulsed methylprednisolone in patients with MS". Neurology. 64 (11): 1971–3. doi:10.1212/01.WNL.0000163804.94163.91. PMID 15955958.
- ↑ Jacobs LD, Beck RW, Simon JH; et al. (2000). "Intramuscular interferon beta-1a therapy initiated during a first demyelinating event in multiple sclerosis. CHAMPS Study Group". N Engl J Med. 343 (13): 898–904. PMID 11006365.
- ↑ Comi G, Filippi M, Barkhof F; et al. (2001). "Effect of early interferon treatment on conversion to definite multiple sclerosis: a randomised study". Lancet. 357 (9268): 1576–82. PMID 11377645.
- ↑ Ruggieri M, Avolio C, Livrea P, Trojano M (2007). "Glatiramer acetate in multiple sclerosis: a review". CNS Drug Rev. 13 (2): 178–91. doi:10.1111/j.1527-3458.2007.00010.x. PMID 17627671.
- ↑ 149.0 149.1 Munari L, Lovati R, Boiko A (2004). "Therapy with glatiramer acetate for multiple sclerosis". Cochrane Database Syst Rev (1): CD004678. doi:10.1002/14651858.CD004678. PMID 14974077.
- ↑ Rice GP, Incorvaia B, Munari L; et al. (2001). "Interferon in relapsing-remitting multiple sclerosis". Cochrane Database Syst Rev (4): CD002002. PMID 11687131.
- ↑ 151.0 151.1 Martinelli Boneschi F, Rovaris M, Capra R, Comi G (2005). "Mitoxantrone for multiple sclerosis". Cochrane Database Syst Rev (4): CD002127. doi:10.1002/14651858.CD002127.pub2. PMID 16235298.
- ↑ Johnson KP (2007). "Control of multiple sclerosis relapses with immunomodulating agents". J. Neurol. Sci. 256 Suppl 1: S23–8. doi:10.1016/j.jns.2007.01.060. PMID 17350652.
- ↑ Gonsette RE (2007). "Compared benefit of approved and experimental immunosuppressive therapeutic approaches in multiple sclerosis". Expert opinion on pharmacotherapy. 8 (8): 1103–16. doi:10.1517/14656566.8.8.1103. PMID 17516874.
- ↑ Murray TJ (2006). "The cardiac effects of mitoxantrone: do the benefits in multiple sclerosis outweigh the risks?". Expert opinion on drug safety. 5 (2): 265–74. doi:10.1517/14740338.5.2.265. PMID 16503747.
- ↑ Leary SM, Thompson AJ (2005). "Primary progressive multiple sclerosis: current and future treatment options". CNS drugs. 19 (5): 369–76. PMID 15907149.
- ↑ Sládková T, Kostolanský F (2006). "The role of cytokines in the immune response to influenza A virus infection". Acta Virol. 50 (3): 151–62. PMID 17131933.
- ↑ Betaseron [package insert]. Montville, NJ: Berlex Inc; 2003
- ↑ Rebif [package insert]. Rockland, MA: Serono Inc; 2005.
- ↑ Avonex [package insert]. Cambridge, MA: Biogen Inc; 2003
- ↑ 160.0 160.1 Fox EJ (2006). "Management of worsening multiple sclerosis with mitoxantrone: a review". Clinical therapeutics. 28 (4): 461–74. doi:10.1016/j.clinthera.2006.04.013. PMID 16750460.
- ↑ Kleinschmidt-DeMasters BK, Tyler KL (2005). "Progressive multifocal leukoencephalopathy complicating treatment with natalizumab and interferon beta-1a for multiple sclerosis". N Engl J Med. 353 (4): 369–74. doi:10.1056/NEJMoa051782. PMID 15947079. Free full text with registration
- ↑ Langer-Gould A, Atlas SW, Green AJ, Bollen AW, Pelletier D (2005). "Progressive multifocal leukoencephalopathy in a patient treated with natalizumab". N Engl J Med. 353 (4): 375–81. doi:10.1056/NEJMoa051847. PMID 15947078. Free full text with registration
- ↑ Kesselring J, Beer S (2005). "Symptomatic therapy and neurorehabilitation in multiple sclerosis". Lancet neurology. 4 (10): 643–52. doi:10.1016/S1474-4422(05)70193-9. PMID 16168933.
- ↑ United Kingdom early Mitoxantrone Copaxone trial. Onyx Healthcare (2006-01-01). Retrieved on 2007-09-02.
- ↑ Farinotti M, Simi S, Di Pietrantonj C; et al. (2007). "Dietary interventions for multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD004192. doi:10.1002/14651858.CD004192.pub2. PMID 17253500.
- ↑ Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E (2006). "Cannabis use in patients with multiple sclerosis". Mult. Scler. 12 (5): 646–51. PMID 17086912.
- ↑ Zajicek JP, Sanders HP, Wright DE, Vickery PJ, Ingram WM, Reilly SM, Nunn AJ, Teare LJ, Fox PJ, Thompson AJ (2005). "Cannabinoids in multiple sclerosis (CAMS) study: safety and efficacy data for 12 months follow up". J. Neurol. Neurosurg. Psychiatr. 76 (12): 1664–9. doi:10.1136/jnnp.2005.070136. PMID 16291891.
- ↑ Bennett M, Heard R (2004). "Hyperbaric oxygen therapy for multiple sclerosis". Cochrane database of systematic reviews (Online) (1): CD003057. doi:10.1002/14651858.CD003057.pub2. PMID 14974004.
- ↑ Oken BS, Kishiyama S, Zajdel D; et al. (2004). "Randomized controlled trial of yoga and exercise in multiple sclerosis". Neurology. 62 (11): 2058–64. PMID 15184614.
- ↑ Weinshenker BG. Natural history of multiple sclerosis. Ann Neurol 1994;36 Suppl:S6–11. PMID 8017890
- ↑ Stern M (2005). "Aging with multiple sclerosis". Physical medicine and rehabilitation clinics of North America. 16 (1): 219–34. PMID 15561552.
- ↑ Pittock SJ; McClelland RL; Mayr WT; Jorgensen NW; Weinshenker BG; Noseworthy J; Rodriguez M. Clinical implications of benign multiple sclerosis: a 20-year population-based follow-up study Ann Neurol 2004 Aug;56(2):303-6. PMID 15293286
- ↑ Berger T, Rubner P, Schautzer F, Egg R, Ulmer H, Mayringer I, Dilitz E, Deisenhammer F, Reindl M. Antimyelin antibodies as a predictor of clinically definite multiple sclerosis after a first demyelinating event. N Engl J Med. 2003 Jul 10;349(2):139-45. PMID 12853586
- ↑ United Kingdom early Mitoxantrone Copaxone trial. Onyx Healthcare (2006-01-01). Retrieved on 2007-09-02.
- ↑ Genzyme and Bayer HealthCare Announce Detailed Interim Two-Year Alemtuzumab in Multiple Sclerosis Data Presented at AAN. Genzyme (2007-02-01). Retrieved on 2007-09-02.
- ↑ Daclizumab. PDL Biopharma (2006-01-01). Retrieved on 2007-09-02.
- ↑ Treatment of Multiple Sclerosis Using Over the Counter Inosine. ClinicalTrials.gov (2006-03-16). Retrieved on 2007-09-02.
- ↑ Efficacy and Safety of BG00012 in Relapsing-Remitting Multiple Sclerosis. ClinicalTrials.gov (2007-09-01). Retrieved on 2007-11-12.
- ↑ Efficacy and Safety of Fingolimod in Patients With Relapsing-Remitting Multiple Sclerosis. ClinicalTrials.gov (2006-02-09). Retrieved on 2007-09-02.
- ↑ The CAMMS223 Trial Investigators (2008). "Alemtuzumab vs. Interferon Beta-1a in Early Multiple Sclerosis". N Engl J Med. 359 (17): 1786–1801. PMID 18946064.
- ↑ Polman C, Barkhof F, Sandberg-Wollheim M, Linde A, Nordle O, Nederman T (2005). "Treatment with laquinimod reduces development of active MRI lesions in relapsing MS". Neurology. 64 (6): 987–91. doi:10.1212/01.WNL.0000154520.48391.69. PMID 15781813.
- ↑ Darlington CL (2005). "Technology evaluation: NeuroVax, Immune Response Corp". Curr. Opin. Mol. Ther. 7 (6): 598–603. PMID 16370383.
- ↑ Agrawal YP (2005). "Low dose naltrexone therapy in multiple sclerosis". Med. Hypotheses. 64 (4): 721–4. doi:10.1016/j.mehy.2004.09.024. PMID 15694688.
- ↑ search of clinicaltrials.gov data-base for Low dose naltrexone Multiple Sclerosis
- ↑ 2007 clinical trial using LDN
- ↑ Gironi M, Martinelli-Boneschi F, Sacerdote P, Solaro C, Zaffaroni M, Cavarretta R, Moiola L, Bucello S, Radaelli M, Pilato V, Rodegher M, Cursi M, Franchi S, Martinelli V, Nemni R, Comi G, Martino G (2008). "A pilot trial of low-dose naltrexone in primary progressive multiple sclerosis". Multiple Sclerosis. 14 (8): 1076–83. PMID 18728058.
- ↑ Albrecht P, Fröhlich R, Hartung HP, Kieseier BC, Methner A (2007). "Optical coherence tomography measures axonal loss in multiple sclerosis independently of optic neuritis". J Neurol. Online: 1595. doi:10.1007/s00415-007-0538-3. PMID 17987252.
- ↑ Gordon-Lipkin E, Chodkowski B, Reich DS; et al. (2007). "Retinal nerve fiber layer is associated with brain atrophy in multiple sclerosis". Neurology. 69 (16): 1603–09. doi:10.1212/01.wnl.0000295995.46586.ae. PMID 17938370. Unknown parameter
|month=ignored (help) - ↑ Thangarajh M, Gomez-Rial J, Hedström AK; et al. (2008). "Lipid-specific immunoglobulin M in CSF predicts adverse long-term outcome in multiple sclerosis". Mult. Scler. doi:10.1177/1352458508095729. PMID 18755821. Unknown parameter
|month=ignored (help)
See also
- MS fundraisers include the MS Challenge Walk, MS Walk and MS Bike Tour.
- List of multiple sclerosis organizations
Template:Diseases of the nervous system
ar:تصلب الأنسجة المتعدد bg:Множествена склероза ca:Esclerosi múltiple cs:Roztroušená skleróza de:Multiple Sklerose el:Πολλαπλή σκλήρυνση eo:Sklerozo multiloka fa:اسکلروز چندگانه id:Sklerosis ganda it:Sclerosi multipla he:טרשת נפוצה hu:Sclerosis multiplex nl:Multiple sclerose no:Multippel sklerose sq:Multiple skleroza sr:Multipla skleroza fi:MS-tauti sv:Multipel skleros