Lomefloxacin hydrochloride
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alberto Plate [2]
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Lomefloxacin hydrochloride is a fluoroquinolone antibiotic that is FDA approved for the treatment of lower respiratory tract infections and urinary tract infections (UTI) in adult patients. Common adverse reactions include phototoxicity, diarrhea, nausea, dizziness, headache.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
- Maxaquin may be taken without regard to meals. Sucralfate and antacids containing magnesium or aluminum, or Videx® (didanosine), chewable/buffered tablets or the pediatric powder for oral solution should not be taken within 4 hours before or 2 hours after taking lomefloxacin. Risk of reaction to solar UVA light may be reduced by taking Maxaquin at least 12 hours before exposure to the sun (eg, in the evening).
Treatment
Patients with normal renal function
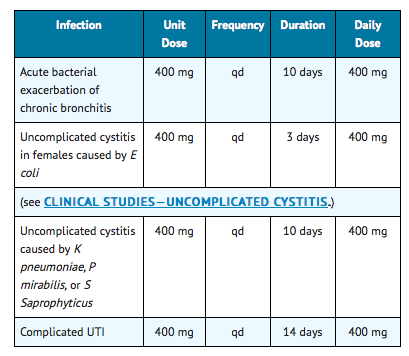
The recommended daily dose of Maxaquin is described in the following chart:
Elderly patients
- No dosage adjustment is needed for elderly patients with normal renal function (ClCr≥ 40 mL/min/1.73 m2).
Patients with impaired renal function
- Lomefloxacin is primarily eliminated by renal excretion. (See CLINICAL PHARMACOLOGY.) Modification of dosage is recommended in patients with renal dysfunction. In patients with a creatinine clearance > 10 mL/min/1.73 m2 but < 40 mL/min/1.73 m2, the recommended dosage is an initial loading dose of 400 mg followed by daily maintenance doses of 200 mg (1/2 tablet) once daily for the duration of treatment. It is suggested that serial determinations of lomefloxacin levels be performed to determine any necessary alteration in the appropriate next dosing interval.
If only the serum creatinine is known, the following formula may be used to estimate creatinine clearance.
- Men:
(weight in kg) × (140 – age)
(72) × serum creatinine (mg/dL)
- Women:
(0.85) × (calculated value for men)
Dialysis patients
- Hemodialysis removes only a negligible amount of lomefloxacin (3% in 4 hours). Hemodialysis patients should receive an initial loading dose of 400 mg followed by daily maintenance doses of 200 mg (1/2 tablet) once daily for the duration of treatment.
Patients with cirrhosis
- Cirrhosis does not reduce the nonrenal clearance of lomefloxacin. The need for a dosage reduction in this population should be based on the degree of renal function of the patient and on the plasma concentrations.
Prevention/prophylaxis
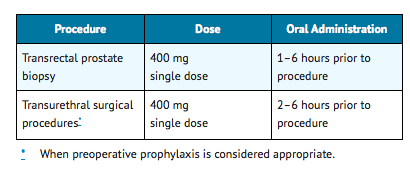
The recommended dose of Maxaquin is described in the following chart:
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lomefloxacin hydrochloride in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lomefloxacin hydrochloride in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Lomefloxacin hydrochloride FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Lomefloxacin hydrochloride in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Lomefloxacin hydrochloride in pediatric patients.
Contraindications
- Maxaquin (lomefloxacin HCl) is contraindicated in persons with a history of hypersensitivity to lomefloxacin or any member of the quinolone group of antimicrobial agents.
Warnings
The safety and efficacy of lomefloxacin in pediatric patients and adolescents (under the age of 18 years), pregnant women, and lactating women have not been established. The oral administration of multiple doses of lomefloxacin to juvenile dogs at 0.3 times and to rats at 5.4 times the recommended adult human dose based on mg/m2 (0.6 and 34 times the recommended adult human dose based on mg/kg, respectively) caused arthropathy and lameness. Histopathologic examination of the weight-bearing joints of these animals revealed permanent lesions of the cartilage. Other quinolones also produce erosions of cartilage of weight-bearing joints and other signs of arthropathy in juvenile animals of various species.
Photosensitivity
- Moderate to severe phototoxic reactions have occurred in patients exposed to direct or indirect sunlight or to artificial ultraviolet light (eg, sunlamps) during or following treatment with lomefloxacin. These reactions have also occurred in patients exposed to shaded or diffuse light, including exposure through glass. patients should be advised to discontinue lomefloxacin therapy at the first signs or symptoms of a phototoxicity reaction such as a sensation of skin burning, redness, swelling, blisters, rash, itching, or dermatitis.
- These phototoxic reactions have occurred with and without the use of sunscreens or sunblocks. Single doses of lomefloxacin have been associated with these types of reactions. In a few cases, recovery was prolonged for several weeks. As with some other types of phototoxicity, there is the potential for exacerbation of the reaction on re-exposure to sunlight or artificial ultraviolet light prior to complete recovery from the reaction. In rare cases, reactions have recurred up to several weeks after stopping lomefloxacin therapy.
- Exposure to direct or indirect sunlight (even when using sunscreens or sunblocks) should be avoided while taking lomefloxacin and for several days following therapy. Lomefloxacin therapy should be discontinued immediately at the first signs or symptoms of phototoxicity. Risk of phototoxicity may be reduced by taking lomefloxacin in the evening.
Seizures
- Convulsions have been reported in patients receiving lomefloxacin. Whether the convulsions were directly related to lomefloxacin administration has not yet been established. However, convulsions, increased intracranial pressure, and toxic psychoses have been reported in patients receiving other quinolones. Nevertheless, lomefloxacin has been associated with a possible increased risk of seizures compared to other quinolones. Some of these may occur with a relative absence of predisposing factors. Quinolones may also cause central nervous system (CNS) stimulation, which may lead to tremors, restlessness, lightheadedness, confusion, and hallucinations. If any of these reactions occurs in patients receiving lomefloxacin, the drug should be discontinued and appropriate measures instituted. However, until more information becomes available, lomefloxacin, like all other quinolones, should be used with caution in patients with known or suspected CNS disorders, such as severe cerebral arteriosclerosis, epilepsy, or other factors that predispose to seizures. Psychiatric disturbances, agitation, anxiety, and sleep disorders may be more common with lomefloxacin than other products in the quinolone class.
Infections
- The safety and efficacy of lomefloxacin in the treatment of acute bacterial exacerbation of chronic bronchitis due to S pneumoniae have not been demonstrated. This product should not be used empirically in the treatment of acute bacterial exacerbation of chronic bronchitis when it is probable that S pneumoniae is a causative pathogen.
- In clinical trials of complicated UTIs due to P aeruginosa, 12 of 16 patients had the microorganism eradicated from the urine after therapy with lomefloxacin. No patients had concomitant bacteremia. Serum levels of lomefloxacin do not reliably exceed the MIC of Pseudomonas isolates. The safety and efficacy of lomefloxacin in treating patients with pseudomonas bacteremia have not been established.
Hypersensitivity Reactions
- Serious and occasionally fatal hypersensitivity (anaphylactoid or anaphylactic) reactions, some following the first dose, have been reported in patients receiving quinolone therapy. Some reactions were accompanied by cardiovascular collapse, loss of consciousness, tingling, pharyngeal or facial edema, dyspnea, urticaria, or itching. Only a few of these patients had a history of previous hypersensitivity reactions. Serious hypersensitivity reactions have also been reported following treatment with lomefloxacin. If an allergic reaction to lomefloxacin occurs, discontinue the drug. Serious acute hypersensitivity reactions may require immediate emergency treatment with epinephrine. Oxygen, intravenous fluids, antihistamines, corticosteroids, pressor amines, and airway management, including intubation, should be administered as indicated.
Pseudomembranous colitis
- Pseudomembranous colitis has been reported with nearly all antibacterial agents, including lomefloxacin, and may range from mild to life-threatening in severity. Therefore, it is important to consider this diagnosis in patients who present with diarrhea subsequent to the administration of antibacterial agents. Treatment with antimicrobial agents alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of "antibiotic-associated colitis." After the diagnosis of pseudomembranous colitis has been established, therapeutic measures should be initiated. Mild cases of pseudomembranous colitis usually respond to discontinuation of drug alone. In moderate to severe cases, consideration should be given to management with fluids and electrolytes, protein supplementation, and treatment with an antibacterial drug clinically effective against C difficile colitis.
QT interval prolongation/torsades de pointes
- Rare cases of torsades de pointes have been spontaneously reported during post-marketing surveillance in patients receiving quinolones, including lomefloxacin. These rare cases were associated with one or more of the following factors: age over 60, female gender, underlying cardiac disease, and/or use of multiple medications. Lomefloxacin should be avoided in patients with known prolongation of the QT interval, patients with uncorrected hypokalemia, and patients receiving class IA (quinidine, procainamide), or class III (amiodarone, sotalol) antiarrhythmic agents.
Peripheral neuropathy
- Rare cases of sensory or sensorimotor axonal polyneuropathy affecting small and/or large axons resulting in paresthesias, hypoesthesias, dysesthesias and weakness have been reported in patients receiving quinolones, including lomefloxacin. Lomefloxacin should be discontinued if the patient experiences symptoms of neuropathy including pain, burning, tingling, numbness, and/or weakness, or is found to have deficits in light touch, pain, temperature, position sense, vibratory sensation, and/or motor strength in order to prevent the development of an irreversible condition.
Tendon effects
- Ruptures of the shoulder, hand, Achilles tendon or other tendons that required surgical repair or resulted in prolonged disability have been reported in patients receiving quinolones, including lomefloxacin. Postmarketing surveillance reports indicate that this risk may be increased in patients receiving concomitant corticosteroids, especially the elderly. Lomefloxacin should be discontinued if the patient experiences pain, inflammation, or rupture of a tendon. Patients should rest and refrain from exercise until the diagnosis of tendonitis or tendon rupture has been excluded. Tendon rupture can occur during or after therapy with quinolones, including lomefloxacin.
Adverse Reactions
Clinical Trials Experience
In clinical trials, most of the adverse events reported were mild to moderate in severity and transient in nature. During these clinical investigations, 5,623 patients received Maxaquin. In 2.2% of the patients, lomefloxacin was discontinued because of adverse events, primarily involving the gastrointestinal system (0.7%), skin (0.7%), or CNS (0.5%).
Adverse clinical events
The events with the highest incidence (≥ 1%) in patients, regardless of relationship to drug, were headache (3.6%), nausea (3.5%), photosensitivity (2.3%), dizziness (2.1%), diarrhea (1.4%), and abdominal pain (1.2%).
Additional clinical events reported in < 1% of patients treated with Maxaquin, regardless of relationship to drug, are listed below:
- Autonomic: increased sweating, dry mouth, flushing, syncope.
- Body as a whole: fatigue, back pain, malaise, asthenia, chest pain, face edema, hot flashes, influenza-like symptoms, edema, chills, allergic reaction, anaphylactoid reaction, decreased heat tolerance.
- Cardiovascular: tachycardia, hypertension, hypotension, myocardial infarction, angina pectoris, cardiac failure, bradycardia, arrhythmia, phlebitis, pulmonary embolism, extrasystoles, cerebrovascular disorder, cyanosis, cardiomyopathy.
- Central and peripheral nervous system: tremor, vertigo, paresthesias, twitching, hypertonia, convulsions, hyperkinesia, coma.
- Gastrointestinal: dyspepsia, vomiting, flatulence, constipation, gastrointestinal bleeding, dysphagia, stomatitis, tongue discoloration, gastrointestinal inflammation.
- Hearing: earache, tinnitus.
- Hematologic: purpura, lymphadenopathy, thrombocythemia, anemia, thrombocytopenia, increased fibrinolysis.
- Hepatic: abnormal liver function.
- Metabolic: thirst, hyperglycemia, hypoglycemia, gout.
- Musculoskeletal: arthralgia, myalgia, leg cramps.
- Ophthalmologic: abnormal vision, conjunctivitis, photophobia, eye pain, abnormal lacrimation.
- Psychiatric: insomnia, nervousness, somnolence, anorexia, depression, confusion, agitation, increased appetite, depersonalization, paranoid reaction, anxiety, paroniria, abnormal thinking, concentration impairment.
- Reproductive system:
- Female: vaginal moniliasis, vaginitis, leukorrhea, menstrual disorder, perineal pain, intermenstrual bleeding.
- Male: epididymitis, orchitis.
- Resistance mechanism: viral infection, moniliasis, fungal infection.
- Respiratory: respiratory infection, rhinitis, pharyngitis, dyspnea, cough, epistaxis, bronchospasm, respiratory disorder, increased sputum, stridor, respiratory depression.
- Skin/Allergic: pruritus, rash, urticaria, skin exfoliation, bullous eruption, eczema, skin disorder, acne, skin discoloration, skin ulceration, angioedema.
- Special senses: taste perversion.
- Urinary: hematuria, micturition disorder, dysuria, strangury, anuria.
Adverse laboratory events
Changes in laboratory parameters, listed as adverse events, without regard to drug relationship include:
- Hematologic: monocytosis (0.2%), eosinophilia (0.1%), leukopenia (0.1%), leukocytosis (0.1%).
- Renal: elevated BUN (0.1%), hypokalemia (0.1%), increased creatinine (0.1%).
- Hepatic: elevations of ALT (SGPT) (0.4%), AST (SGOT) (0.3%), bilirubin (0.1%), alkaline phosphatase (0.1%).
- Additional laboratory changes occurring in < 0.1% in the clinical studies included: elevation of serum gamma glutamyl transferase, decrease in total protein or albumin, prolongation of prothrombin time, anemia, decrease in hemoglobin, thrombocythemia, thrombocytopenia, abnormalities of urine specific gravity or serum electrolytes, increased albumin, elevated ESR, albuminuria, macrocytosis.
Postmarketing Experience
Post-marketing adverse events
- Adverse events reported from worldwide marketing experience with lomefloxacin are: anaphylaxis, cardiopulmonary arrest, laryngeal or pulmonary edema, ataxia, cerebral thrombosis, hallucinations, painful oral mucosa, pseudomembranous colitis, hemolytic anemia, hepatitis, tendinitis, diplopia, photophobia, phobia, exfoliative dermatitis, hyperpigmentation, Stevens-Johnson syndrome, toxic epidermal necrolysis, dysgeusia, interstitial nephritis, polyuria, renal failure, urinary retention, and vasculitis.
Quinolone-class adverse events
- Additional quinolone-class adverse events include: peripheral neuropathy, torsades de pointes, erythema nodosum, hepatic necrosis, possible exacerbation of myasthenia gravis, dysphasia, nystagmus, intestinal perforation, manic reaction, renal calculi, acidosis and hiccough.
- Laboratory adverse events include: agranulocytosis, elevation of serum triglycerides, elevation of serum cholesterol, elevation of blood glucose, elevation of serum potassium, albuminuria, candiduria, and crystalluria.
Drug Interactions
Theophylline
- In three pharmacokinetic studies including 46 normal, healthy subjects, theophylline clearance and concentration were not significantly altered by the addition of lomefloxacin. In clinical studies where patients were on chronic theophylline therapy, lomefloxacin had no measurable effect on the mean distribution of theophylline concentrations or the mean estimates of theophylline clearance. Though individual theophylline levels fluctuated, there were no clinically significant symptoms of drug interaction.
Antacids and sucralfate
- Sucralfate and antacids containing magnesium or aluminum, as well as formulations containing divalent and trivalent cations such as Videx® (didanosine), chewable/buffered tablets or the pediatric powder for oral solution can form chelation complexes with lomefloxacin and interfere with its bioavailability. Sucralfate administered 2 hours before lomefloxacin resulted in a slower absorption (mean Cmax decreased by 30% and mean Tmax increased by 1 hour) and a lesser extent of absorption (mean AUC decreased by approximately 25%). Magnesium- and aluminum-containing antacids, administered concomitantly with lomefloxacin, significantly decreased the bioavailability (48%) of lomefloxacin. Separating the doses of antacid and lomefloxacin minimizes this decrease in bioavailability; therefore, administration of these agents should precede lomefloxacin dosing by 4 hours or follow lomefloxacin dosing by at least 2 hours.
Caffeine
- Two hundred mg of caffeine (equivalent to 1 to 3 cups of American coffee) was administered to 16 normal, healthy volunteers who had achieved steady-state blood concentrations of lomefloxacin after being dosed at 400 mg qd. This did not result in any statistically or clinically relevant changes in the pharmacokinetic parameters of either caffeine or its major metabolite, paraxanthine. No data are available on potential interactions in individuals who consume greater than 200 mg of caffeine per day or in those, such as the geriatric population, who are generally believed to be more susceptible to the development of drug-induced CNS-related adverse effects. Other quinolones have demonstrated moderate to marked interference with the metabolism of caffeine, resulting in a reduced clearance, a prolongation of plasma half-life, and an increase in symptoms that accompany high levels of caffeine.
Cimetidine
- Cimetidine has been demonstrated to interfere with the elimination of other quinolones. This interference has resulted in significant increases in half-life and AUC. The interaction between lomefloxacin and cimetidine has not been studied.
Cyclosporine
- Elevated serum levels of cyclosporine have been reported with concomitant use of cyclosporine with other members of the quinolone class. Interaction between lomefloxacin and cyclosporine has not been studied.
Omeprazole
- No clinically significant changes in lomefloxacin pharmacokinetics (AUC, Cmax, or Tmax) were observed when a single dose of lomefloxacin 400 mg was given after multiple doses of omeprazole (20 mg qd) in 13 healthy volunteers. Changes in omeprazole pharmacokinetics were not studied.
Phenytoin
- No significant differences were observed in mean phenytoin AUC, Cmax, Cmin or Tmax (although Cmax increased by 11%) when extended phenytoin sodium capsules (100 mg tid) were coadministered with lomefloxacin (400 mg qd) for five days in 15 healthy males. Lomefloxacin is unlikely to have a significant effect on phenytoin metabolism.
Probenecid
- Probenecid slows the renal elimination of lomefloxacin. An increase of 63% in the mean AUC and increases of 50% and 4%, respectively, in the mean Tmax and mean Cmax were noted in 1 study of 6 individuals.
Terfenadine
- No clinically significant changes occurred in heart rate or corrected QT intervals, or in terfenadine metabolite or lomefloxacin pharmacokinetics, during concurrent administration of lomefloxacin and terfenadine at steady-state in 28 healthy males.
Warfarin
- Quinolones may enhance the effects of the oral anticoagulant, warfarin, or its derivatives. When these products are administered concomitantly, prothrombin or other suitable coagulation tests should be monitored closely. However, no clinically or statistically significant differences in prothrombin time ratio or warfarin enantiomer pharmacokinetics were observed in a small study of 7 healthy males who received both warfarin and lomefloxacin under steady-state conditions.
Use in Specific Populations
Pregnancy
- Reproductive function studies have been performed in rats at doses up to 8 times the recommended human dose based on mg/m2 (34 times the recommended human dose based on mg/kg), and no impaired fertility or harm to the fetus was reported due to lomefloxacin. Increased incidence of fetal loss in monkeys has been observed at approximately 3 to 6 times the recommended human dose based on mg/m2 (6 to 12 times the recommended human dose based on mg/kg). No teratogenicity has been observed in rats and monkeys at up to 16 times the recommended human dose exposure. In the rabbit, maternal toxicity and associated fetotoxicity, decreased placental weight, and variations of the coccygeal vertebrae occurred at doses 2 times the recommended human exposure based on mg/m2. There are, however, no adequate and well-controlled studies in pregnant women. Lomefloxacin should be used during pregnancy only if the potential benefit justifies the potential risk to the fetus.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Lomefloxacin hydrochloride in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Lomefloxacin hydrochloride during labor and delivery.
Nursing Mothers
- It is not known whether lomefloxacin is excreted in human milk. However, it is known that other drugs of this class are excreted in human milk and that lomefloxacin is excreted in the milk of lactating rats. Because of the potential for serious adverse reactions from lomefloxacin in nursing infants, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
- The safety and effectiveness of lomefloxacin in pediatric patients and adolescents less than 18 years of age have not been established. Lomefloxacin causes arthropathy in juvenile animals of several species.
Geriatic Use
- Of the total number of subjects in clinical studies of lomefloxacin, 25% were ≥ 65 years and 9% were ≥ 75 years. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
- This drug is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
Gender
There is no FDA guidance on the use of Lomefloxacin hydrochloride with respect to specific gender populations.
Race
There is no FDA guidance on the use of Lomefloxacin hydrochloride with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Lomefloxacin hydrochloride in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Lomefloxacin hydrochloride in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Lomefloxacin hydrochloride in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Lomefloxacin hydrochloride in patients who are immunocompromised.
Administration and Monitoring
Administration
There is limited information regarding Lomefloxacin hydrochloride Administration in the drug label.
Monitoring
There is limited information regarding Lomefloxacin hydrochloride Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Lomefloxacin hydrochloride and IV administrations.
Overdosage
- Information on overdosage in humans is limited. In the event of acute overdosage, the stomach should be emptied by inducing vomiting or by gastric lavage, and the patient should be carefully observed and given supportive treatment. Adequate hydration must be maintained. Hemodialysis or peritoneal dialysis is unlikely to aid in the removal of lomefloxacin as < 3% is removed by these modalities.
- Clinical signs of acute toxicity in rodents progressed from salivation to tremors, decreased activity, dyspnea, and clonic convulsions prior to death. These signs were noted in rats and mice as lomefloxacin doses were increased.
Pharmacology
| |
Lomefloxacin hydrochloride
| |
| Systematic (IUPAC) name | |
| (RS)-1-Ethyl-6,8-difluoro-7-(3-methylpiperazin-1-yl)-4-oxo-quinoline-3-carboxylic acid | |
| Identifiers | |
| CAS number | |
| ATC code | J01 S01AE04 (WHO) |
| PubChem | |
| DrugBank | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 351.348 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Protein binding | 10% |
| Metabolism | ? |
| Half life | 8 hours |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |
Mechanism of Action
- The bactericidal action of lomefloxacin results from interference with the activity of the bacterial enzyme DNA gyrase, which is needed for the transcription and replication of bacterial DNA. The minimum bactericidal concentration (MBC) generally does not exceed the minimum inhibitory concentration (MIC) by more than a factor of 2, except for staphylococci, which usually have MBCs 2 to 4 times the MIC.
Structure
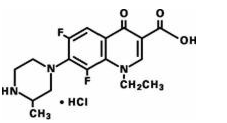
- Lomefloxacin HCl, a difluoroquinolone, is the monohydrochloride salt of (±)-1-ethyl-6,8-difluoro-1,4-dihydro-7-(3-methyl-1-piperazinyl)-4-oxo-3-quinolinecarboxylic acid. Its empirical formula is C17H19F2N3O3•HCl, and its structural formula is:
Pharmacodynamics
There is limited information regarding Lomefloxacin hydrochloride Pharmacodynamics in the drug label.
Pharmacokinetics
Pharmacokinetics in healthy volunteers
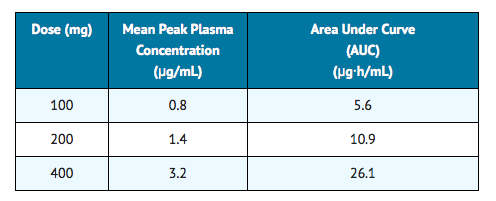
- In 6 fasting healthy male volunteers, approximately 95% to 98% of a single oral dose of lomefloxacin was absorbed. Absorption was rapid following single doses of 200 and 400 mg (Tmax 0.8 to 1.4 hours). Mean plasma concentration increased proportionally between 100 and 400 mg as shown below:
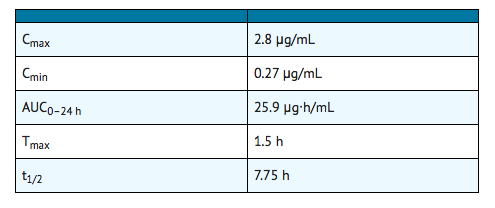
- In 6 healthy male volunteers administered 400 mg of lomefloxacin on an empty stomach qd for 7 days, the following mean pharmacokinetic parameter values were obtained:
- The elimination half-life in 8 subjects with normal renal function was approximately 8 hours. At 24 hours postdose, subjects with normal renal function receiving single doses of 200 or 400 mg had mean plasma lomefloxacin concentrations of 0.10 and 0.24 µg/mL, respectively. Steady-state concentrations were achieved within 48 hours of initiating therapy with one-a-day dosing. There was no drug accumulation with single-daily dosing in patients with normal renal function.
- Approximately 65% of an orally administered dose was excreted in the urine as unchanged drug in patients with normal renal function. Following a 400-mg dose of lomefloxacin administered qd for 7 days, the mean urine concentration 4 hours postdose was in excess of 300 µg/mL. The mean urine concentration exceeded 35 µg/mL for at least 24 hours after dosing.
- Following a single 400-mg dose, the solubility of lomefloxacin in urine usually exceeded its peak urinary concentration 2- to 6-fold. In this study, urine pH affected the solubility of lomefloxacin with solubilities ranging from 7.8 mg/mL at pH 5.2, to 2.4 mg/mL at pH 6.5, and 3.03 mg/mL at pH 8.12.
- The urinary excretion of lomefloxacin was virtually complete within 72 hours after cessation of dosing, with approximately 65% of the dose being recovered as parent drug and 9% as its glucuronide metabolite. The mean renal clearance was 145 mL/min in subjects with normal renal function (GFR = 120 mL/min). This may indicate tubular secretion.
Food effect
- When lomefloxacin and food were administered concomitantly, the rate of drug absorption was delayed (Tmax increased to 2 hours [delayed by 41%], Cmax decreased by 18%), and the extent of absorption (AUC) was decreased by 12%.
Pharmacokinetics in the geriatric population
- In 16 healthy elderly volunteers (61 to 76 years of age) with normal renal function for their age, the half-life of lomefloxacin (mean of 8 hours) and its peak plasma concentration (mean of 4.2 µg/mL) following a single 400-mg dose were similar to those in 8 younger subjects dosed with a single 400-mg dose. Thus, drug absorption appears unaffected in the elderly. Plasma clearance was, however, reduced in this elderly population by approximately 25%, and the AUC was increased by approximately 33%. This slower elimination most likely reflects the decreased renal function normally observed in the geriatric population.
Pharmacokinetics in renally impaired patients
In 8 patients with creatinine clearance (ClCr) between 10 and 40 mL/min/1.73 m2, the mean AUC after a single 400-mg dose of lomefloxacin increased 335% over the AUC demonstrated in patients with a ClCr> 80 mL/min/1.73 m2. Also, in these patients, the mean t1/2 increased to 21 hours. In 8 patients with ClCr< 10 mL/min/1.73 m2, the mean AUC after a single 400-mg dose of lomefloxacin increased 700% over the AUC demonstrated in patients with a ClCr> 80 mL/min/1.73 m2. In these patients with ClCr< 10 mL/min/1.73 m2, the mean t1/2 increased to 45 hours. The plasma clearance of lomefloxacin was closely correlated with creatinine clearance, ranging from 31 mL/min/1.73 m2 when creatinine clearance was zero to 271 mL/min/1.73 m2 at a normal creatinine clearance of 110 mL/min/1.73 m2. Peak lomefloxacin concentrations were not affected by the degree of renal function when single doses of lomefloxacin were administered. Adjustment of dosage schedules for patients with such decreases in renal function is warranted.
Pharmacokinetics in patients with cirrhosis
- In 12 patients with histologically confirmed cirrhosis, no significant changes in rate or extent of lomefloxacin exposure (Cmax, Tmax, t1/2, or AUC) were observed when they were administered 400 mg of lomefloxacin as a single dose. No data are available in cirrhotic patients treated with multiple doses of lomefloxacin. Cirrhosis does not appear to reduce the nonrenal clearance of lomefloxacin. There does not appear to be a need for a dosage reduction in cirrhotic patients, provided adequate renal function is present.
Metabolism and pharmacodynamics of lomefloxacin
- Lomefloxacin is minimally metabolized although 5 metabolites have been identified in human urine. The glucuronide metabolite is found in the highest concentration and accounts for approximately 9% of the administered dose. The other 4 metabolites together account for < 0.5% of the dose.
- Approximately 10% of an oral dose was recovered as unchanged drug in the feces.
- Serum protein binding of lomefloxacin is approximately 10%.
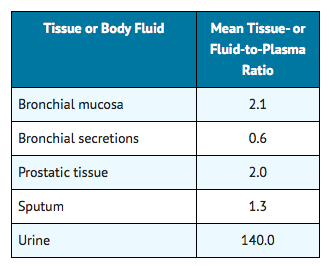
- The following are mean tissue- or fluid-to-plasma ratios of lomefloxacin following oral administration. Studies have not been conducted to assess the penetration of lomefloxacin into human cerebrospinal fluid.
Nonclinical Toxicology
There is limited information regarding Lomefloxacin hydrochloride Nonclinical Toxicology in the drug label.
Clinical Studies
Uncomplicated Cystitis
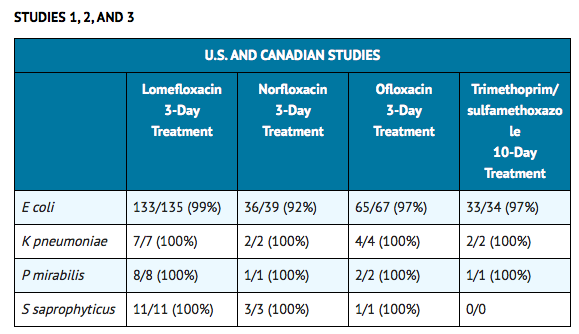
- In three controlled clinical studies of uncomplicated cystitis in females, two performed in the United States and one in Canada, lomefloxacin was compared to other oral antimicrobial agents. In these studies, using very strict evaluability criteria and microbiological criteria at 5–9 days posttherapy follow-up, the following bacterial eradication outcomes were obtained:
- In a controlled clinical study of uncomplicated cystitis performed in Sweden, lomefloxacin 3-day treatment was compared with lomefloxacin 7-day treatment and norfloxacin 7-day treatment. In this study, using very strict evaluability criteria and microbiological criteria at 5–9 days post-therapy follow-up, the following bacterial eradication outcomes were obtained:

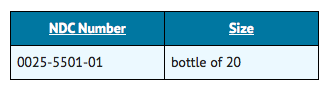
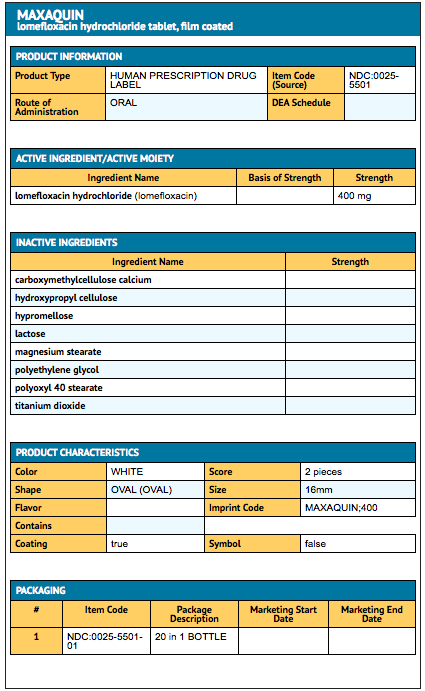
How Supplied
- Maxaquin is supplied as a scored, film-coated tablet containing the equivalent of 400 mg of lomefloxacin base present as the hydrochloride. The tablet is oval, white, and film-coated with "MAXAQUIN 400" debossed on one side and scored on the other side and is supplied in:
Storage
Store at 59° to 77°F (15° to 25°C).
Images
Drug Images
{{#ask: Page Name::Lomefloxacin hydrochloride |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Lomefloxacin hydrochloride |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Lomefloxacin hydrochloride Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Lomefloxacin hydrochloride interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
Look-Alike Drug Names
There is limited information regarding Lomefloxacin hydrochloride Look-Alike Drug Names in the drug label.
Price
References
The contents of this FDA label are provided by the National Library of Medicine.