|
|
| (5 intermediate revisions by 4 users not shown) |
| Line 1: |
Line 1: |
| {{SI}} | | __NOTOC__ |
| | {{Pericarditis}} |
|
| |
|
| {{CMG}} | | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
|
| |
| '''Associate Editor-In-Chief:''' {{CZ}} | |
| | |
| {{Editor Join}}
| |
|
| |
|
| ==Case #1== | | ==Case #1== |
| | ===Clinical Summary=== |
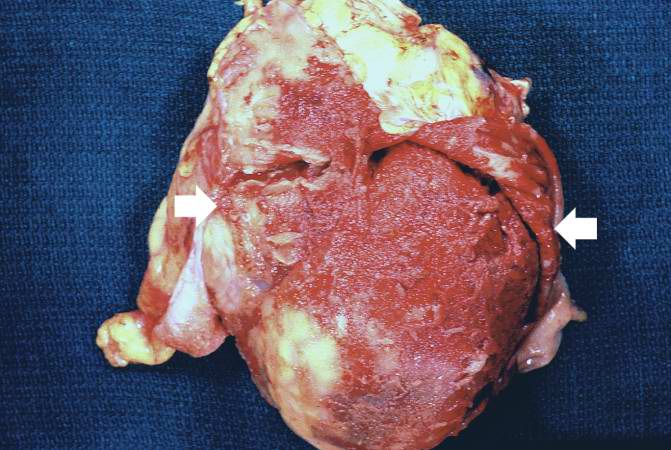
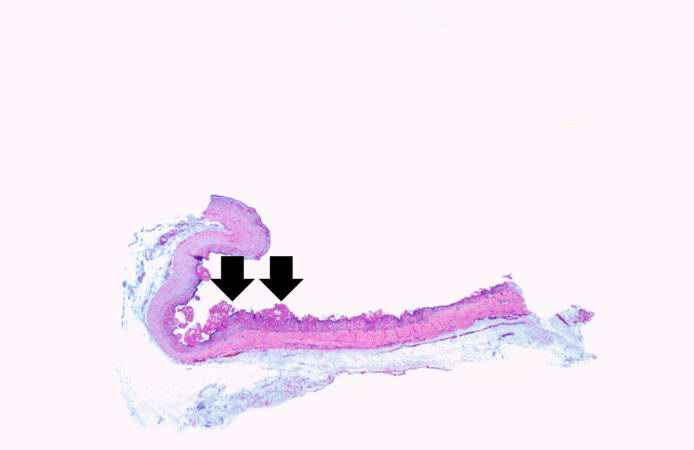
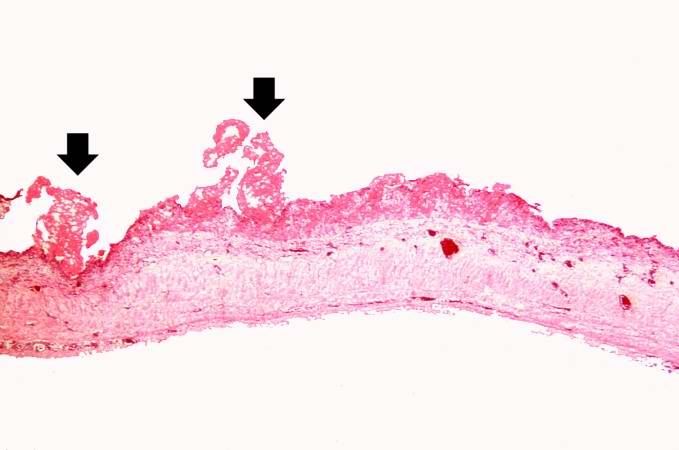
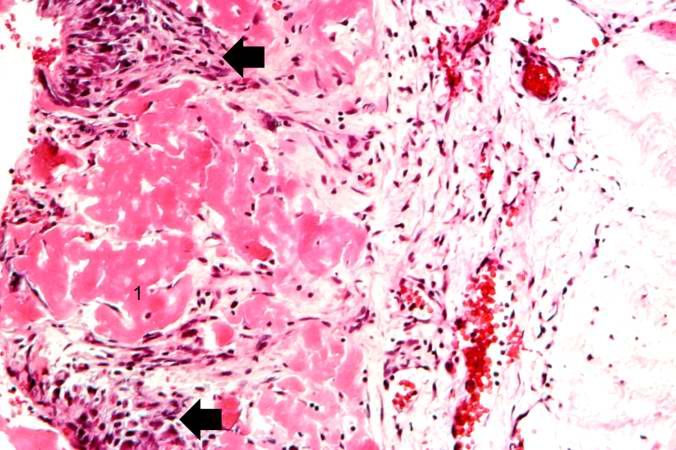
| | This patient is a 36-year-old white male with a history of long-standing renal disease who presents with [[end-stage kidney disease]] and a BUN of 112 mg/dL. During the present hospitalization he developed a [[pericardial friction rub]] and pericardial and pleural effusions. A semi-elective [[pericardiectomy]] was performed. Despite aggressive treatment, the patient expired. |
|
| |
|
| ====Clinical Summary====
| | ===Autopsy Findings=== |
| | |
| This patient is a 36-year-old white male with a history of long-standing renal disease who presents with end-stage kidney disease and a BUN of 112 mg/dL. During the present hospitalization he developed a pericardial friction rub and pericardial and pleural effusions. A semi-elective pericardiectomy was performed.
| |
| | |
| ====Autopsy Findings====
| |
| | |
| Submitted for examination was a rectangular segment of gray-tan tissue measuring 9.5 x 8.5 x 0.3 cm. The outer surface was fatty in appearance. The inner surface was rough and covered by a number of fine red papillary projections. The projections were composed of fine strands having the appearance of [[fibrin]]. | | Submitted for examination was a rectangular segment of gray-tan tissue measuring 9.5 x 8.5 x 0.3 cm. The outer surface was fatty in appearance. The inner surface was rough and covered by a number of fine red papillary projections. The projections were composed of fine strands having the appearance of [[fibrin]]. |
|
| |
|
| ====Histopathological Findings====
| | ===Histopathological Findings=== |
| | |
| [http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] | | [http://www.peir.net Images courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology] |
|
| |
|
| Line 36: |
Line 29: |
| <br clear="left"/> | | <br clear="left"/> |
|
| |
|
| ==See Also== | | ==Related Chapters== |
| | |
| * [[Hemopericardium]] | | * [[Hemopericardium]] |
| * [[Pneumopericardium]] | | * [[Pneumopericardium]] |
| Line 50: |
Line 42: |
| * [[Pericardium]] | | * [[Pericardium]] |
|
| |
|
| ==Source==
| | {{Circulatory system pathology}} |
| | |
| * [http://www.ngc.gov/summary/summary.aspx?doc_id=4960&nbr=003524&string=Cardiac+AND+Tamponade National Guideline Clearinghouse]
| |
|
| |
|
| ==References== | | ==References== |
| {{Reflist|2}} | | {{Reflist|2}} |
|
| |
|
| == Acknowledgements ==
| |
| The content on this page was first contributed by [[C. Michael Gibson, M.S., M.D.]]
| |
|
| |
| ==Additional Resources==
| |
| {{refbegin|2}}
| |
| * Adler Y, Finkelstein Y, Guindo J, de la Serna R, Shoenfeld Y, Bayes-Genis A, Sagie A, Bayes de Luna A, Spodick DH. Colchicine treatment for recurrent pericarditis: a decade of experience. Circulation. 1998;97:2183–2185.
| |
| * Applegate RJ, Johnston WE, Vinten-Johansen J, Klopfenstein HS, Little WC. Restraining effect of intact pericardium during acute volume leading. Am J Physiol. 1992;262:H1725–H1733.
| |
| * Artom G, Koren-Morag N, Spodick DH, Brucato A, Guindo J, Bayesde-Luna A, Brambilla G, Finkelstein Y, Granel B, Bayes-Genis A, Schwammenthal E, Adler Y. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: a multicentre all-case analysis. Eur Heart J. 2005;26:723–727.
| |
| * Arunasalam S, Siegel RJ. Rapid resolution of symptomatic acute pericarditis with ketorolac tromethamine: a parenteral nonsteroidal antiinflammatory agent. Am Heart J. 1993;125(pt 1):1455–1458.
| |
| * Bonnefoy E, Gordon P, Kirkorian G, Fatemi M, Chevalier P, Touboul P. Serum cardiac troponin I and ST-segment elevation in patients with acute pericarditis. Eur Heart J. 2000;21:832–836.
| |
| * Correale E, Maggioni AP, Romano S, Ricciardiello V, Battista R, Salvarola G, Santoro E, Tognoni G, on behalf of the Gruppo Italiano perlo Studio della Sopravvivenza nell’Infarto Miocardico (GISSI). Comparison of frequency, diagnostic and prognostic significance of pericardial involvement in acute myocardial infarction treated with and without thrombolytics. Am J Cardiol. 1993;71:1377–1381.
| |
| * Fowler NO. Tuberculous pericarditis. JAMA. 1991;266:99 –103.
| |
| * Freeman GL, LeWinter MM. Determinants of the intrapericardial pressure in dogs. J Appl Physiol. 1986;60:758 –764.
| |
| * Freeman GL, LeWinter MM. Pericardial adaptations during chronic cardiac dilation in dogs. Circ Res. 1984;54:294 –300.
| |
| * Freeman GL, Little WC. Comparison of in situ and in vitro studies of pericardial pressure-volume relation in the dog. Am J Physiol. 1986;251: H421–H427.
| |
| * Gunukula SR, Spodick DH. Pericardial disease in renal patients. Semin Nephrol. 2001;21:52–56.
| |
| * Hoit BD, Gabel M, Fowler NO. Cardiac tamponade in left ventricular dysfunction. Circulation. 1990;82:1370–1376.
| |
| * Imazio M, Bobbio M, Cecchi E, Demarie D, Demichellis B, Pomari F, Moratti M, Gaschino G, Giammaria M, Ghiso A, Belli R, Trinchero R. Colchicine in addition to conventional therapy for acute pericarditis: results of the COlchicine for acute PEricarditis (COPE) Trial. Circulation. 2005;112:2012–2016.
| |
| * Imazio M, Demichellis B, Cecchi E, Belli R, Ghisio A, Bobbio M, Trinchero R. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol. 2003;42:2144–2148.
| |
| * Imazio M, Demichellis B, Parrini I, Gluggia M, Cecchi E, Gaschino G, Demarie D, Ghislo A, Trinchero R. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol. 2004;43:1042–1046.
| |
| * Jerjes-Sanchez C, Ramirez-Rivera A, Ibarra-Perez C. The Dressler syndrome after pulmonary embolism. Am J Cardiol. 1996;78:343–345.
| |
| * Kansal S, Roitman D, Sheffield LT. Two-dimensional echocardiography of congenital absence of pericardium. Am Heart J. 1985;109:912–915.
| |
| * Klopfenstein HS, Schuchard GH, Wann LS, Palmer TE, Hartz AJ, Gross CM, Singh S, Brooks HL. The relative merits of pulsus paradoxus and right ventricular diastolic collapse in the early detection of cardiac tamponade: an experimental echocardiographic study. Circulation. 1985;71: 829–833.
| |
| * Knopf WD, Talley JD, Murphy DA. An echo-dense mass in the pericardial space as a sign of left ventricular free wall rupture during acute myocardial infarction. Am J Cardiol. 1987;59:1202.
| |
| * Lange RA, Hillis D. Acute pericarditis. N Engl J Med. 2004;351: 2195–2202.
| |
| * LeWinter MM, Kabbani S. Pericardial diseases. In: Zipes DP, Libby P, Bonow RO, Braunwald E, eds. Braunwald’s Heart Disease. 7th ed. Philadelphia, Pa: Elsevier Saunders; 2005:1757–1780.
| |
| * Maisch B, Ristic D, Pankuweit S. Intrapericardial treatment of autoreactive pericardial effusion with triamcinolone. Eur Heart J. 2002;23: 1503–1508.
| |
| * Maisch B, Seferovic PM, Ristic AD, Erbel R, Rienmuller R, Adler Y, Tomkowski WZ, Thiene G, Yacoub MH, for the Task Force on the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology. Guidelines on the diagnosis and management of pericardial diseases: executive summary. Eur Heart J. 2004;25:587– 610.
| |
| * Maisch B. Recurrent pericarditis: mysterious or not so mysterious? Eur Heart J. 2005;26:631– 633.
| |
| * Mandell BF. Cardiovascular involvement in systemic lupus erythematosus. Semin Arthritis Rheum. 1987;17:126 –141.
| |
| * Miyazaki T, Pride HP, Zipes DP. Prostaglandins in the pericardial fluid modulate neural regulation of cardiac electrophysiological properties. Circ Res. 1990;66:163–175.
| |
| * Park JH, Choo SJ, Park SW. Acute pericarditis caused by acrylic bone cement after percutaneous vertebroplasty. Circulation. 2005; 111:e98.
| |
| * Permanyer-Miralda G, Sagrista-Sauleda J, Soler-Soler J. Primary acute pericardial disease: a prospective series of 231 consecutive patients. Am J Cardiol. 1985;56:623– 630.
| |
| * Permanyer-Miralda G. Acute pericardial disease: approach to the aetiologic diagnosis. Heart. 2004;90:252–254.
| |
| * Reddy PS, Curtiss EI, O’Toole JD, Shaver JA. Cardiac tamponade: hemodynamic observations in man. Circulation. 1978;58:265–272.
| |
| * Reddy PS, Curtiss EI, Uretsky BF. Spectrum of hemodynamic changes in cardiac tamponade. Am J Cardiol. 1990;66:1487–1491.
| |
| * Shabetai R, Fowler NO, Guntheroth WG. The hemodynamics of cardiac tamponade and constrictive pericarditis. Am J Cardiol. 1970;26: 480–489.
| |
| * Shabetai R. Pericardial effusion: haemodynamic spectrum. Heart. 2004; 90:255–256.
| |
| * Shabetai R. Recurrent pericarditis: recent advances and remaining questions. Circulation. 2005;112:1921–1923.
| |
| * Singh S, Wann S, Schuchard GH, Klopfenstein HS, Leimgruber PP, Keelan MH, Brooks HL. Right ventricular and right atrial collapse in patients with cardiac tamponade: a combined echocardiographic and hemodynamic study. Circulation. 1984;70:966–971.
| |
| * Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349: 684–690.
| |
| * Spodick DH. Acute pericarditis: current concepts and practice. JAMA. 2003;289:1150 –1153.
| |
| * Spodick DH. Intrapericardial treatment of persistent autoreactive pericarditis / myopericarditis and pericardial effusion. Eur Heart J. 2002;23: 1481–1482.
| |
| * Spodick DH. Macrophysiology, microphysiology, and anatomy of the pericardium: a synopsis. Am Heart J. 1992;124:1046 –1051.
| |
| * Troughton RW, Asher CR, Klein AL. Pericarditis. Lancet. 2004;363: 717–727.
| |
| * Tsang TS, Barnes ME, Hayes SN, Freeman WK, Dearani JA, Butler SL, Seward JB. Clinical and echocardiographic characteristics of significant pericardial effusions following cardiothoracic surgery and outcomes of echo-guided pericardiocentesis for management: Mayo Clinic experience, 1979–1998. Chest. 1999;116:322–331.
| |
| * Tsang TS, Oh JK, Seward JB, Tajik AJ. Diagnostic value of echocardiography in cardiac tamponade. Herz. 2000;25:734–740.
| |
| * Zayas R, Anguita M, Torres F, Gimenez D, Bergillos F, Ruiz M, Ciudad M, Gallardo A, Valles F. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol. 1995;75:378 –382.
| |
| {{refend}}
| |
|
| |
| == Suggested Links and Web Resources ==
| |
| * [http://www.mayoclinic.com/invoke.cfm?objectid=CE3BC2CF-B4C1-4401-8F0F9E0B7C284538&dsection=1 Pericarditis] - Mayo Clinic series
| |
| * [http://cardiologychannel.com/pericarditis/diagnosis.shtml Pericarditis] - cardiologychannel.com
| |
| * [http://heartcenter.seattlechildrens.org/conditions_treated/pericarditis.asp Pericarditis information] from Seattle Children's Hospital Heart Center
| |
| * [http://www.jpgmonline.com/article.asp?issn=0022-3859;year=2002;volume=48;issue=1;spage=46;epage=9;aulast=Khasnis Pulsus paradoxus] - Journal of Postgraduate Medicine
| |
| * http://en.wikipedia.org/wiki/Pericarditis
| |
| * [http://www.SeeMyHeart.org SeeMyHeart] - Patient Information on Echocardiograms (Heart Ultrasounds)
| |
| * [http://www.asecho.org American Society] of Echocardiography
| |
| * [http://www.ptca.org/imaging/stress_test.html Stress Test with Echocardiography] from Angioplasty.Org
| |
| * [http://heartcenter.seattlechildrens.org/what_to_expect/echocardiogram.asp Echocardiography information] from Children's Hospital Heart Center, Seattle.
| |
| * [http://know-heart-diseases.com Coronary heart disease] And echocardiography
| |
| * [http://www.echocardiology.org Echocardiography Resources] Simple echocardiography tutorials
| |
| * [http://www.manbit.com/ERS/ERSindex.asp Atlas of Echocardiography] Echocardiography Database
| |
| * [http://www2.umdnj.edu/~shindler/index.html E-chocardiography] Internet Journal of Cardiac Ultrasound
| |
| * [http://www.echobasics.de Echobasics] Basic introduction to echocardiography - German/Spanish English planned for 2007
| |
| * [http://www.mitral.com/echocardiography.shtml Echocardiography] Basic information about echocardiography - HealthwoRx
| |
|
| |
| == For Patients ==
| |
|
| |
| * [http://www.mssm.edu/cvi/pericarditis.shtml#q1 Pericarditis]
| |
|
| |
| {{Electrocardiography}}
| |
| {{Circulatory system pathology}}
| |
| {{SIB}}
| |
| [[Category:Cardiology]] | | [[Category:Cardiology]] |
| [[Category:Diseases involving the fasciae]] | | [[Category:Diseases involving the fasciae]] |
| Line 136: |
Line 52: |
| [[Category:Emergency medicine]] | | [[Category:Emergency medicine]] |
|
| |
|
| | [[Category:Disease]] |
| | [[Category:Intensive care medicine]] |
| | [[Category:Up-To-Date]] |
| | [[Category:Up-To-Date cardiology]] |
| | [[Category:Needs overview]] |
|
| |
|
| [[de:Perikarditis]] | | [[de:Perikarditis]] |
| Line 145: |
Line 66: |
| [[sv:Hjärtsäcksinflammation]] | | [[sv:Hjärtsäcksinflammation]] |
| [[tr:Perikard hastalıkları]] | | [[tr:Perikard hastalıkları]] |
|
| |
|
| |
|
| {{WikiDoc Help Menu}} | | {{WikiDoc Help Menu}} |
| {{WikiDoc Sources}} | | {{WikiDoc Sources}} |