Abdominal aortic aneurysm
|
Abdominal Aortic Aneurysm Microchapters |
|
Differentiating Abdominal Aortic Aneurysm from other Diseases |
|---|
|
Diagnosis |
|
Treatment |
|
Case Studies |
|
Abdominal aortic aneurysm On the Web |
|
Risk calculators and risk factors for Abdominal aortic aneurysm |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Take Over This Page and Apply to be Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Epidemiology and Demographics
Risk Factors
Diagnostic Findings
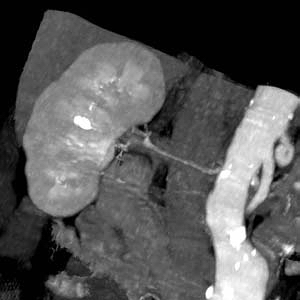
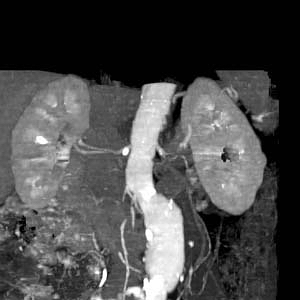
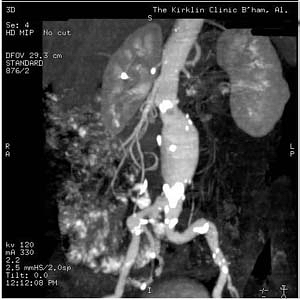
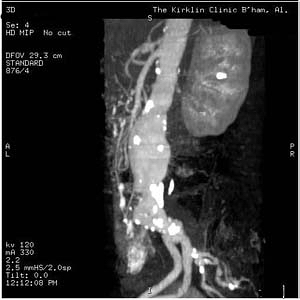
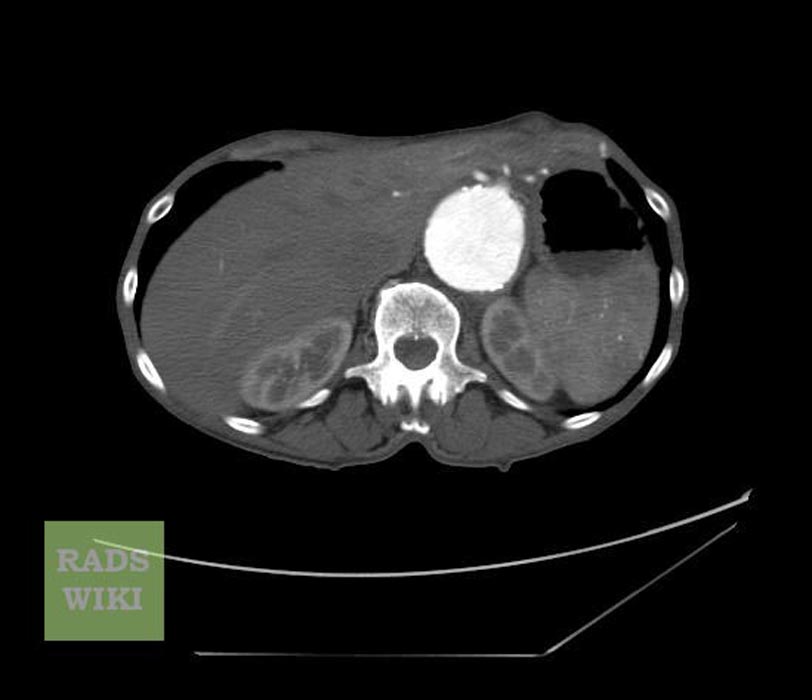
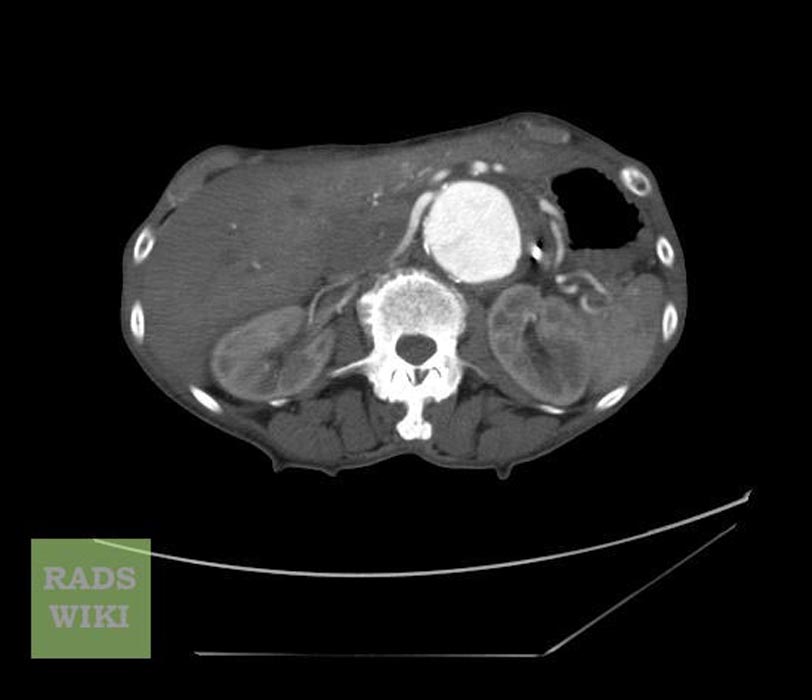
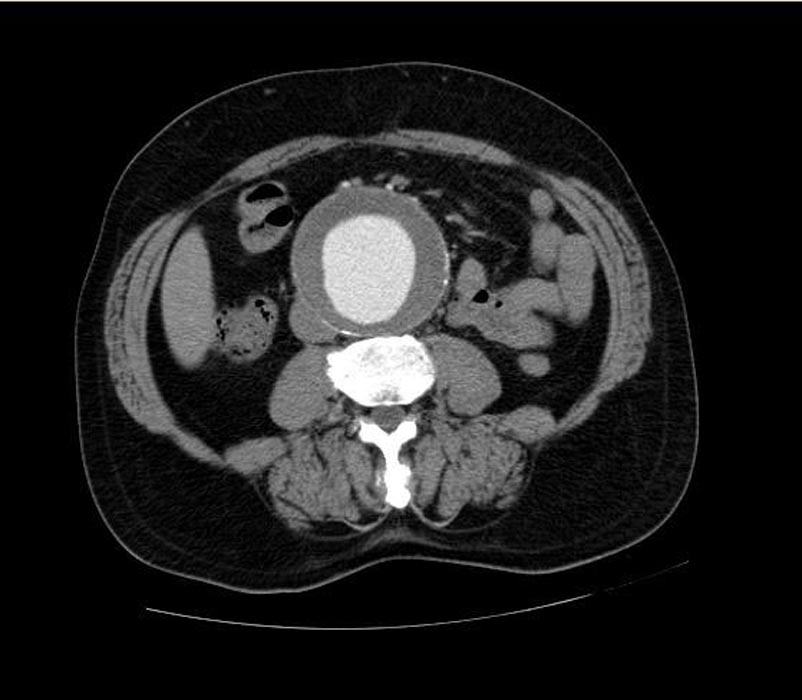
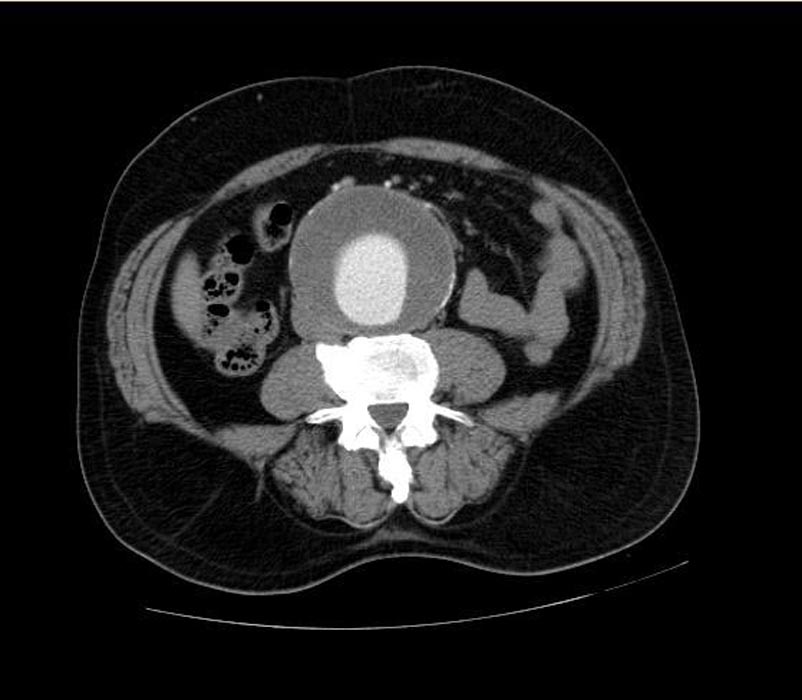
Labeled images shown below are courtesy of Radswiki and copylefted.
-
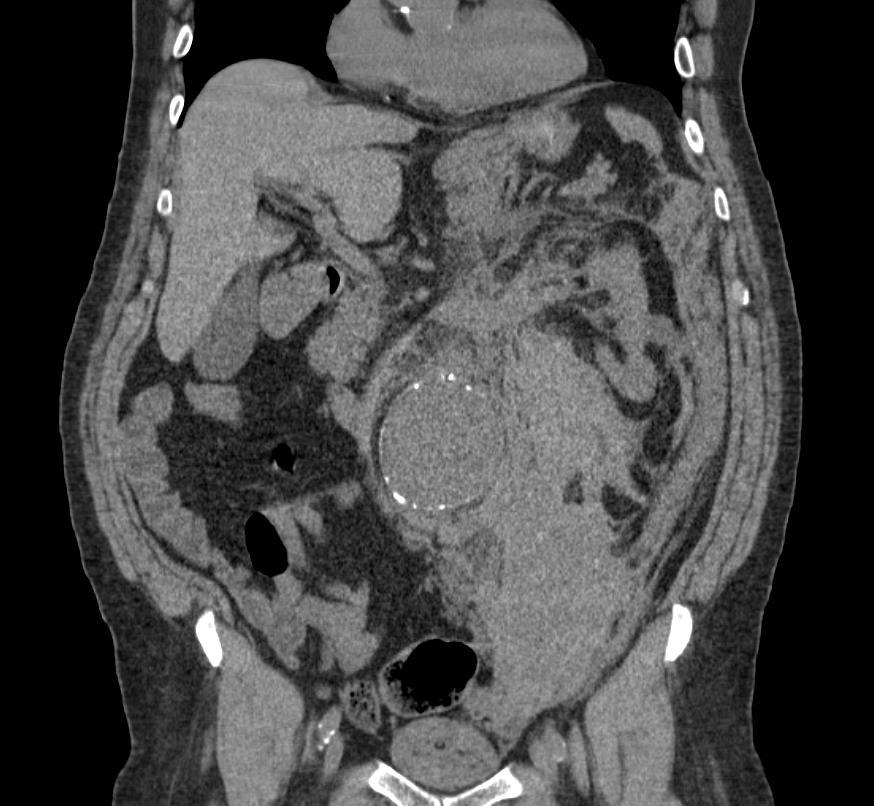
CT: a large abdominal aortic aneurysm
-
CT: a large abdominal aortic aneurysm
-
CT: a large abdominal aortic aneurysm
-
Ruptured abdominal aortic aneurysm
-
This patient presented with acute abdominal pain and hypotension. His non-contrast CT shows a large AAA and extensive periaortic haematoma. A thick (but subtle) hyperdense crescent is present within the aortic wall posteriorly and laterally which represents acute intramural hematoma, a sign of acute or impending rupture. (Image courtesy of Dr Donna D'Souza)
Screening
Pathophysiology & Etiology
Diagnosis
AAAs are commonly divided according to their size and symptomatology. An aneurysm is usually considered to be present if the measured outer aortic diameter is over 3 cm (normal diameter of aorta is around 2 cm). The natural history is of increasing diameter over time, followed eventually by the development of symptoms (usually rupture). If the outer diameter exceeds 5 cm, the aneurysm is considered to be large. For aneurysms under 5 cm, the risk of rupture is low, so that the risks of surgery usually outweigh the risk of rupture. Aneurysms less than 5cm are therefore usually kept under surveillance until such time as they become large enough to warrant repair, or develop symptoms.[1][2] The vast majority of aneurysms are asymptomatic. The risk of rupture is high in a symptomatic aneurysm, which is therefore considered an indication for surgery. Possible symptoms include low back pain, flank pain, abdominal pain, groin pain or pulsating abdominal mass.[3] The complications include rupture, peripheral embolisation, acute aortic occlusion, aortocaval or aortoduodenal fistulae. On physical examination, a palpable abdominal mass can be noted. Bruits can be present in case of renal or visceral arterial stenosis.[4]

As most of the AAAs are asymptomatic, their presence is usually revealed during an abdominal examination for another reason - the most common being abdominal ultrasonography. A physician may also detect the presence of an AAA by abdominal palpation. Ultrasonography provides the initial assessment of the size and extent of the aneurysm, and is the usual modality for surveillance. Preoperative examinations include CT, MRI and special modes thereof, like CT/MR angiography. Angiography may be useful also, as an additional method of measurement for the planning of endoluminal repair. Note that an aneurysmal aorta may appear normal on angiogram, due to thrombus within the sac.
- Many AAAs are detected incidentally during cardiac catheterizations, computed tomography (CT), or magnetic resonance imaging (MRI) performed for unrelated reasons.
- Up to 50% of AAAs can be recognized on plain roentgenograms as a calcified aneurysmal wall.
History and Symptoms
- Most AAAs are asymptomatic and expand silently.
- Spontaneous abdominal pain in a patient with a pulsatile epigastric mass or a known AAA may signal rupture into the retroperitoneum or leakage within the aneurysm wall
- This could lead to rapid expansion or imminent rupture.
- Peripheral embolization to the lower extremities (common in popliteal artery aneurysms) is rare with AAAs.
- Rarely in larger or unstable aneurysms, disseminated intravascular coagulopathy may develop.
Physical Examination
- The physical examination may miss a substantial number of asymptomatic AAAs
- The abdominal aorta should be checked during regular physical examinations because it is easy to do and may detect a life-threatening aneurysm.
- The sensitivity of physical examination increases with the size of the aneurysm:
- 29-61% for AAAs 3.0-3.9 cm in diameter
- 76-82% for those AAAs 5.0 cm or larger
- Generally, it is easier to detect a pulsatile mass in thin patients and those who do not have tense abdomens.
- Contrary to popular belief, gentle palpation of AAAs is safe, and does not precipitate rupture.
Differential Diagnosis
- Acute Abdominal Pain
- Acute Cholecystitis
- Perpforated peptic ulcer
- Diverticulitis
- Nephrolithiasis
Conditions Associated with AAAs
- Atherosclerosis
- Cystic medial necrosis
- Vasculitis
- Infectious diseases
- Congenital
- Trauma
Contrast CT
- Provides detailed anatomic information and is valuable in planning AAA repair
- The disadvantages include:
- Nephrotoxicity
- Cost
- Exposure to radiation
- Suboptimal visualization of the origins of the aortic branch vessels
- Occasionally, inaccurate localizing of the aneurysmal neck
Magnetic Resonance Angiography (MRA)
- Does not require nephrotoxic contrast
- Less accurate than thin-slice CT
- Costly, and is not as readily available as contrast CT and ultrasonography
Echocardiography or Ultrasound
- Ultrasonography has a sensitivity close to 100%
- Well accepted by patients
- The preferred method for detecting and following the progression of AAAs
- Able to show the dimensions of the abdominal aorta and other relevant findings:
- Mural thrombus
- Iliac artery aneurysms
- Patients should fast before examination to optimize image quality.
Contrast Aortography
- Performed before surgery in patients suspected of having the following:
- Suprapenal or juxtarenal aneurysms
- Renovascular hypertension
- Ischemic nephropathy
- Mesenteric ischemia
- Associated iliofemoral arterial occlusive disease
- Should not be used to assess the size of an AAA because the common presence of mural thrombus often leads to diameter underestimation
Treatment
Acute Pharmacotherapies
- Antimetalloproteases such as doxycycline and roxithromycin may halt aneurysm expansion
- Similarly, non-steriod anti inflammatory drugs have shown to be beneficial in small studies
- Beta blockers have numerous benefits in patients with cardiovascular disease
- Reduce aortic complications in patients with Marfan syndrome
- Slow progression of AAAs in hypertensive patients
- In the absence of other indications for beta blockers, the evidence is insufficient to recommend using them routinely for the sole purpose of slowing atherosclerotic aneurysm growth
Surgery and Device Based Therapy
Indications for Surgery
The treatment options for asymptomatic AAA are immediate repair, surveillance with a view to eventual repair, and conservative. There are currently two modes of repair available for an AAA: open aneurysm repair (OR), and endovascular aneurysm repair (EVAR).
- Conservative treatment is indicated in patients where repair carries a high risk of mortality and also in patients where repair is unlikely to improve life expectancy. The two mainstays of the conservative treatment are smoking cessation and blood pressure control.
- Surveillance is indicated in small aneurysms, where the risk of repair exceeds the risk of rupture. As an AAA grows in diameter the risk of rupture increases. Although some controversy exists around the world, most vascular surgeons would not consider repair until the aneurysm reached a diameter of 5cm. The threshold for repair varies slightly from individual to individual, depending on the balance of risks and benefits when considering repair versus ongoing surveillance. The size of an individual's native aorta may influence this, along with the presence of comorbitities that increase operative risk or decrease life expectancy.
- Open repair (operation) is indicated in young patients as an elective procedure, or in growing or large, symptomatic or ruptured aneurysms. Open repair has been the mainstay of intervention from the 1950's until recently.
- Endovascular repair first became practical in the 1990's and although it is now an established alternative to open repair, its role is yet to be clearly defined. It is generally indicated in older, high-risk patients or patients unfit for open repair. However, endovascular repair is feasible for only a proportion of AAA's, depending on the morphology of the aneurysm. The main advantage over open repair is that the peri-operative period has less impact on the patient (less time in intensive care, less time in hospital overall, earlier return to normal activity). Disadvantages of endovascular repair include a requirement for more frequent ongoing hospital reviews, and a higher chance of further procedures being required. According to the latest studies, the EVAR procedure doesn't offer any overall survival benefit.[5] Regarding unruptured aneurysms, EVAR is associated with lower operative mortality than open repair but unknown long-term mortality[6]
Pre-Operative Assessment
- The ADAM trial suggested that the "biological age," as reflected by the condition of the vital organs such as the lungs, kidneys, heart was more important than the chronological age as a determinant of operative outcome. ADAMref4
- Patients with poor renal and pulmonary function have worse operative outcomes
- Chronic obstructive pulmonary disease
- Elevated creatinine concentrations
- Electrocardiographic evidence of ischemia
- Aortic factors implicated in postoperative morbidity and mortality include:
- Extensive atheromatous disease
- Mural calcification
- Thrombosis
- Juxtarenal extension of aneurysm
- Inflammatory aortic aneurysms
- The increased risk resulted from:
- Longer suprapenal clamping time
- Need for complex dissection
- Increased hemodynamic stresses
Pathological Findings
-
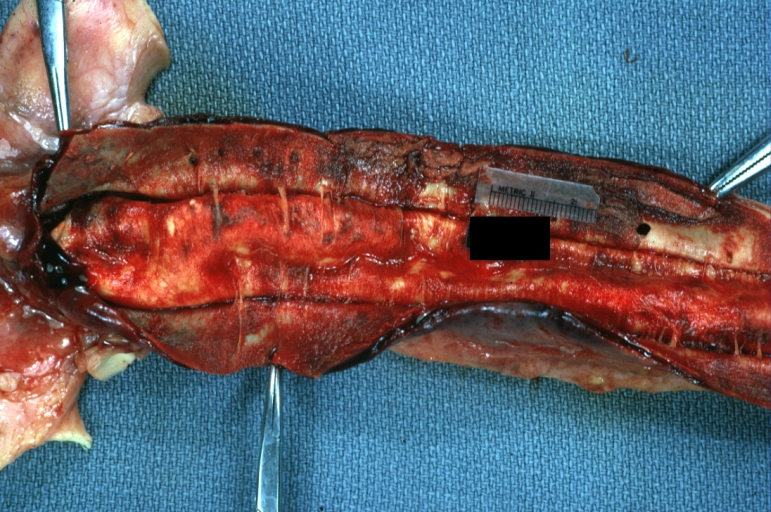
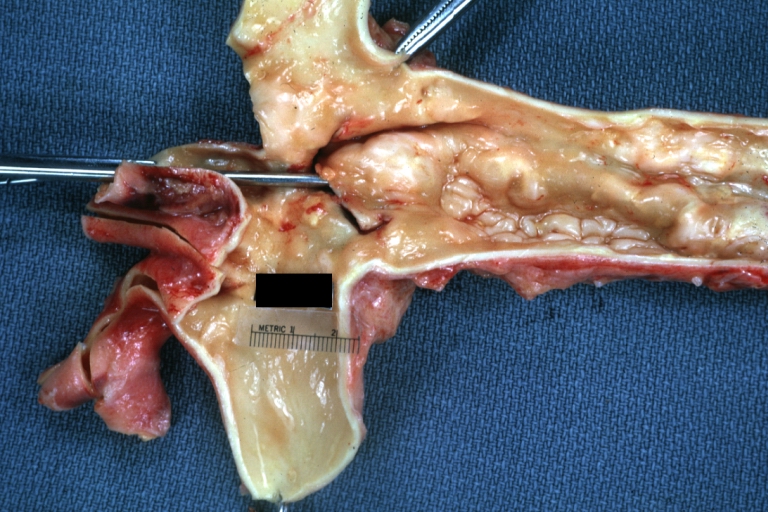
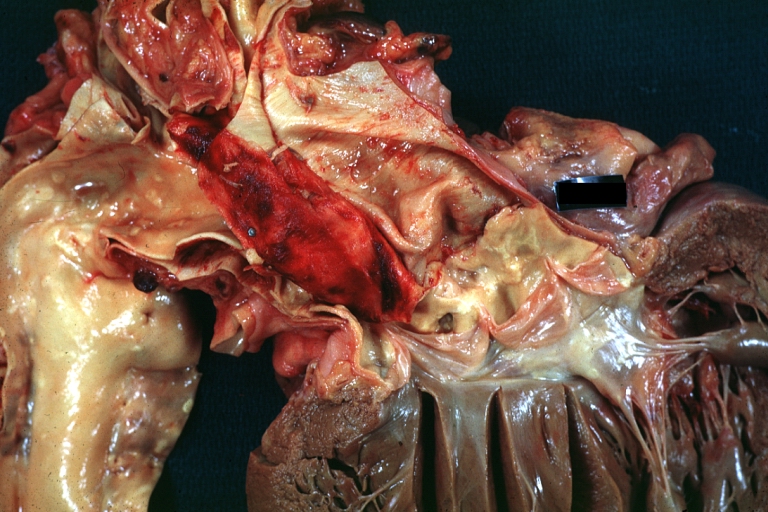
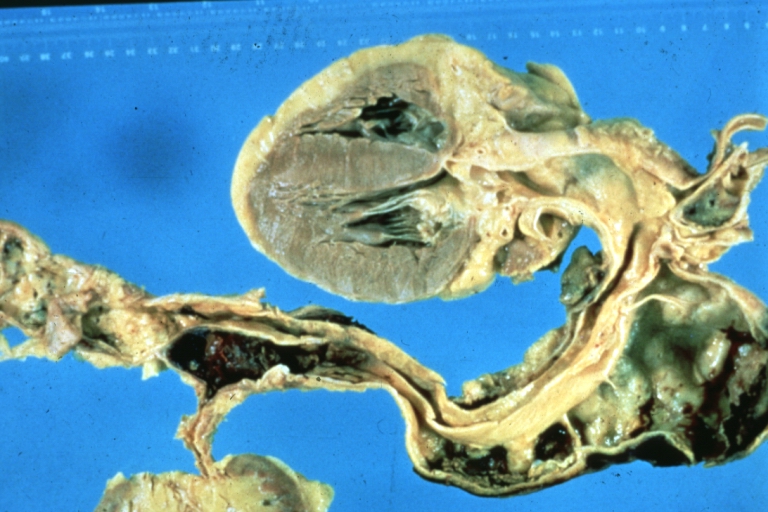
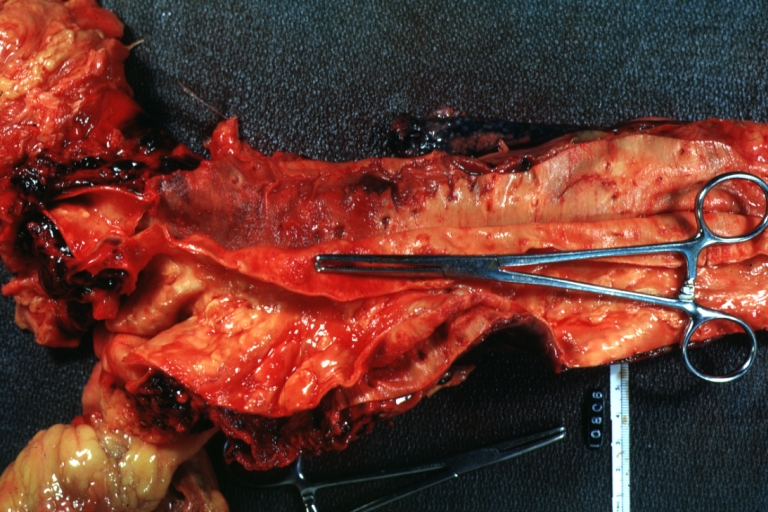
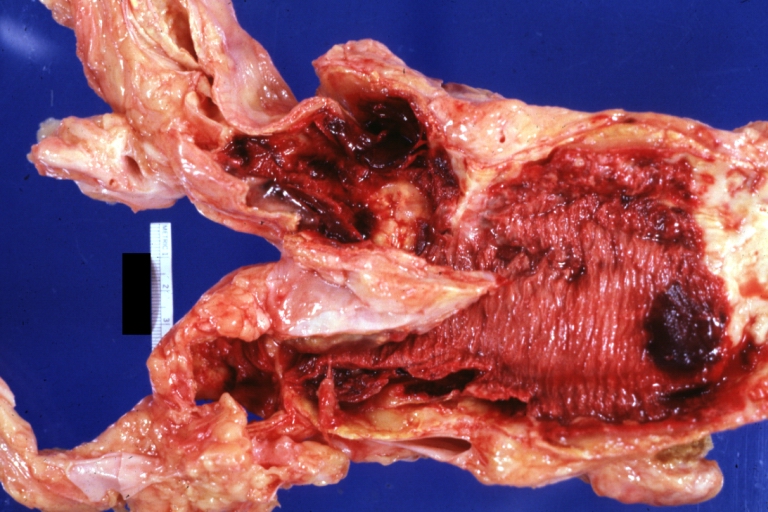
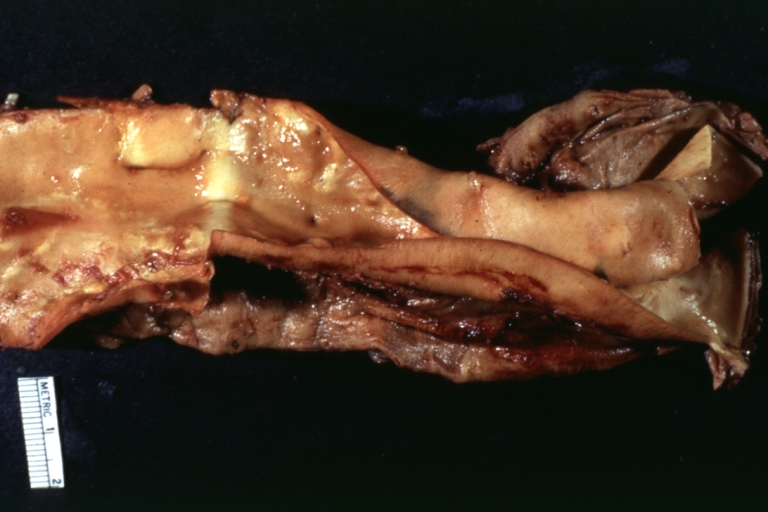
Dissecting Aneurysm: Gross very good example dissected channel has been opened
-
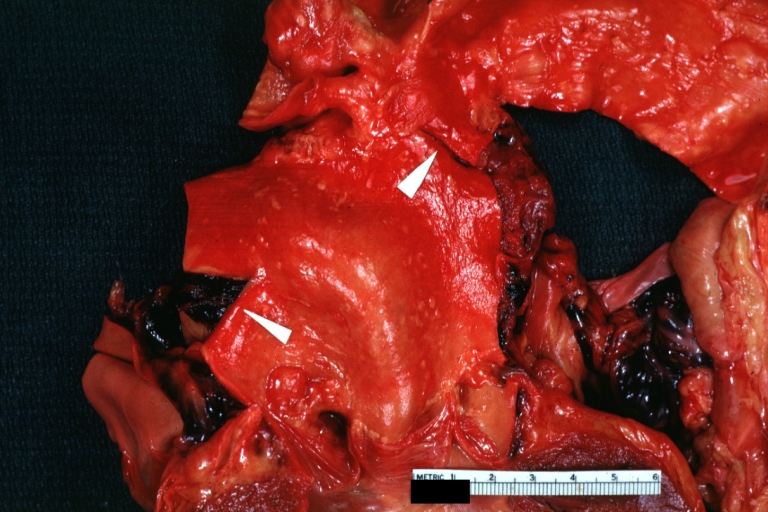
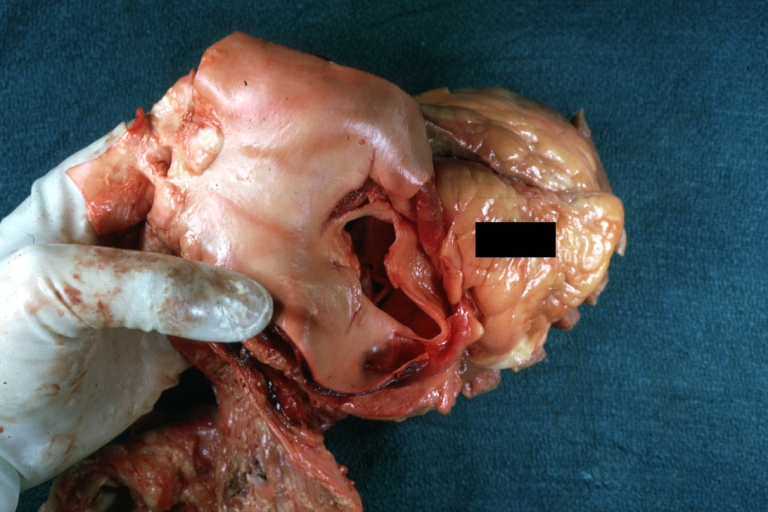
Dissecting Aneurysm: Gross external view good appearance from adventitia
-
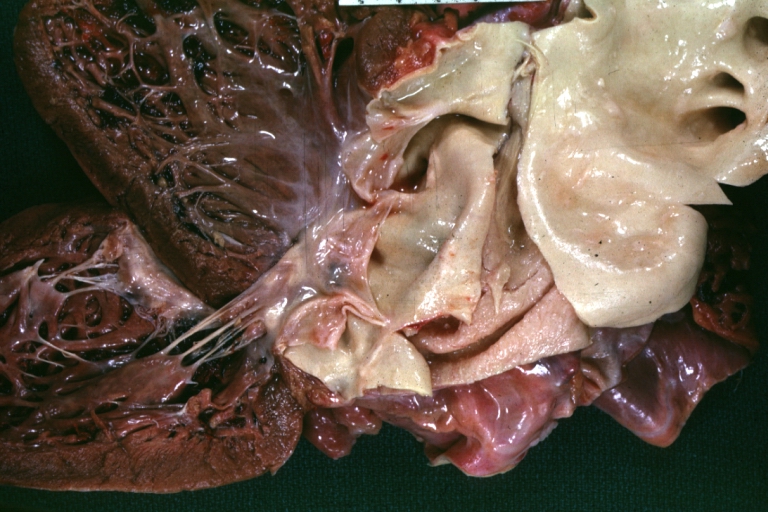
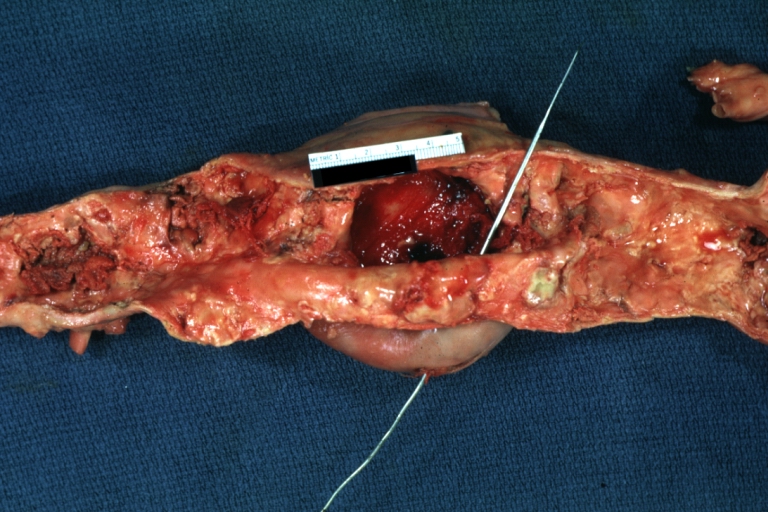
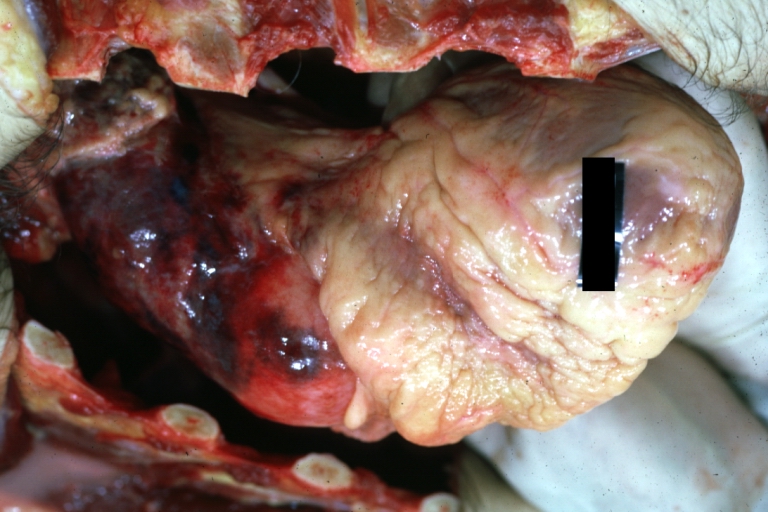
Dissecting Aneurysm: Gross opened false channel
-
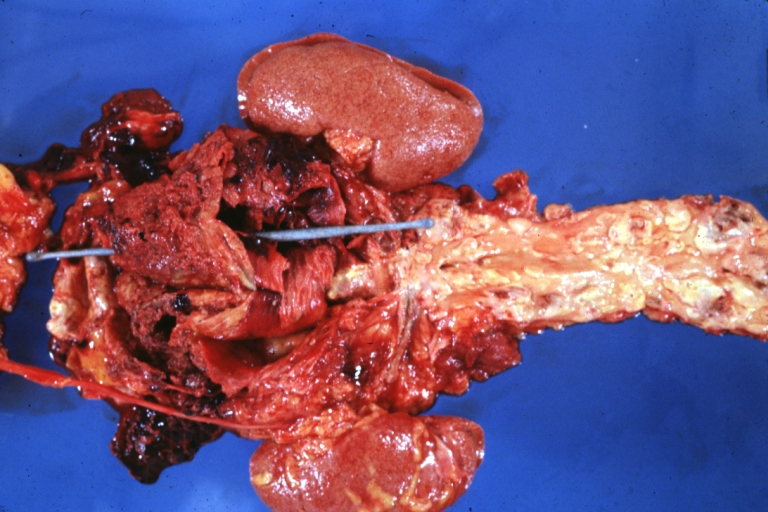
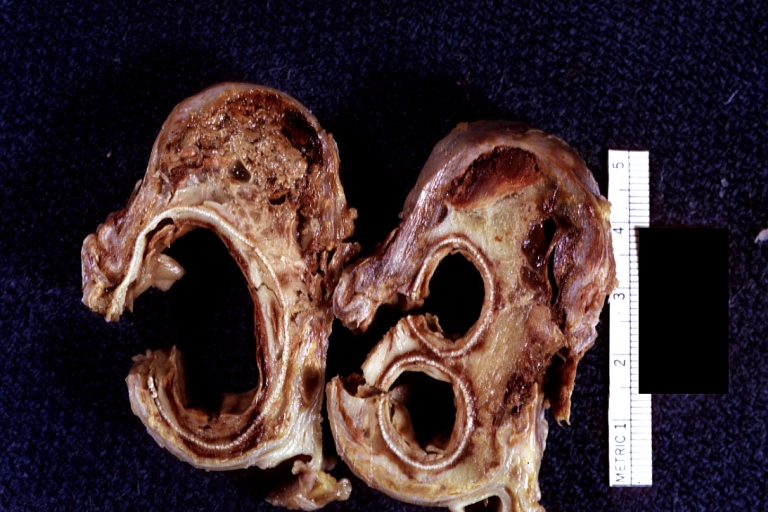
Dissecting Aneurysm: Gross good example dissection beginning at third portion aortic arch
-
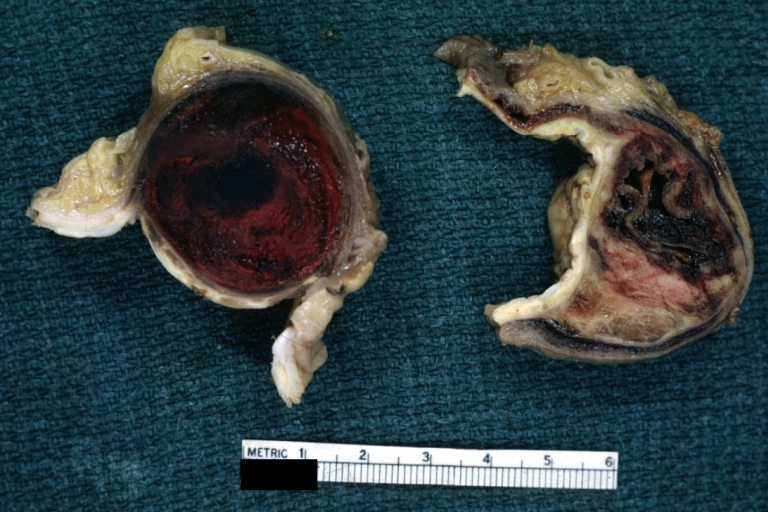
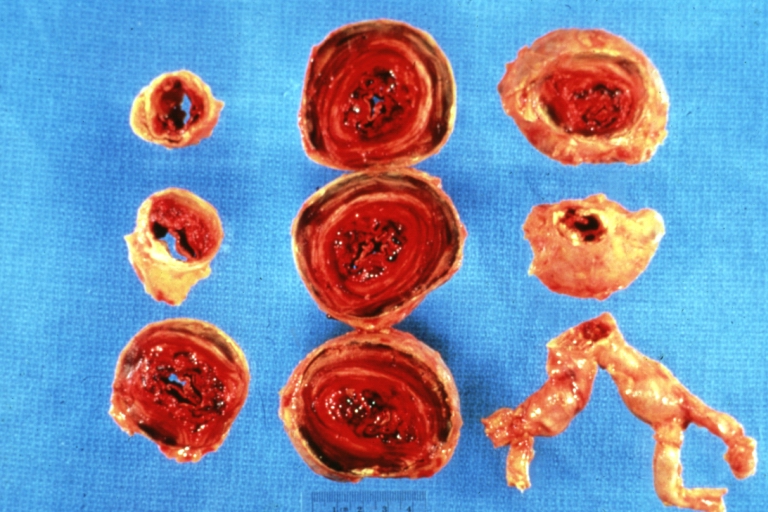
Dissecting Aneurysm: Gross cross sections showing thrombus in false lumen true lumen has been opened longitudinally
-
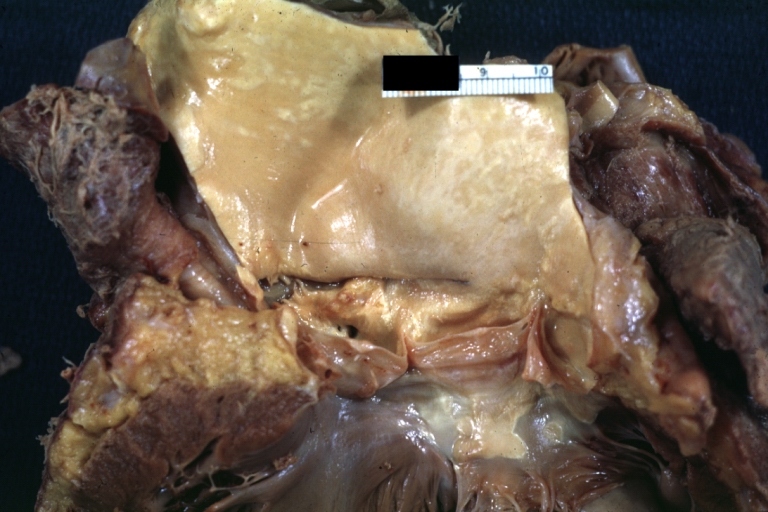
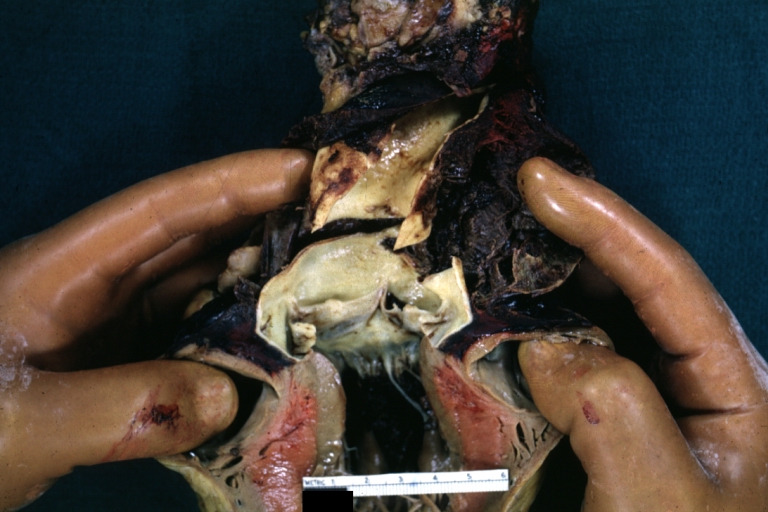
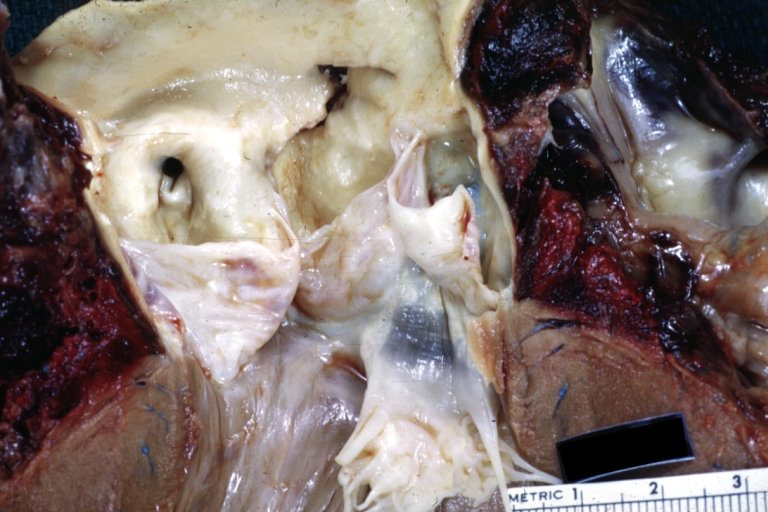
Dissecting Aneurysm: Gross shows origin just above aortic valve false channel shown in descending thoracic aorta (very good example)
-
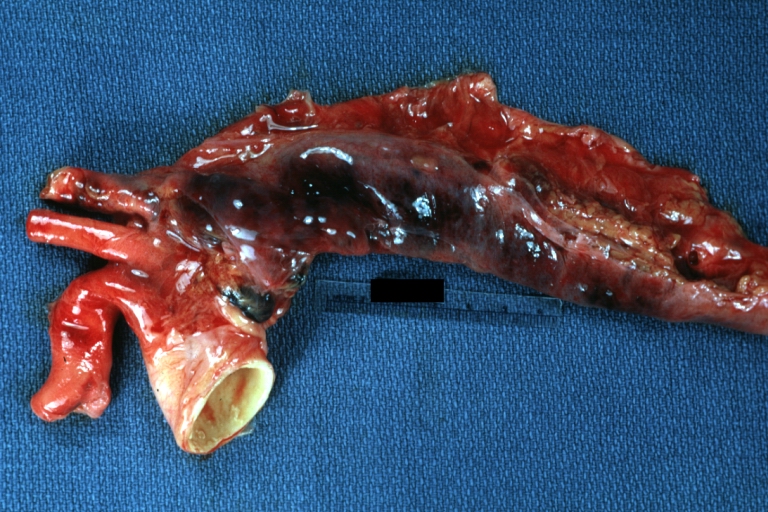
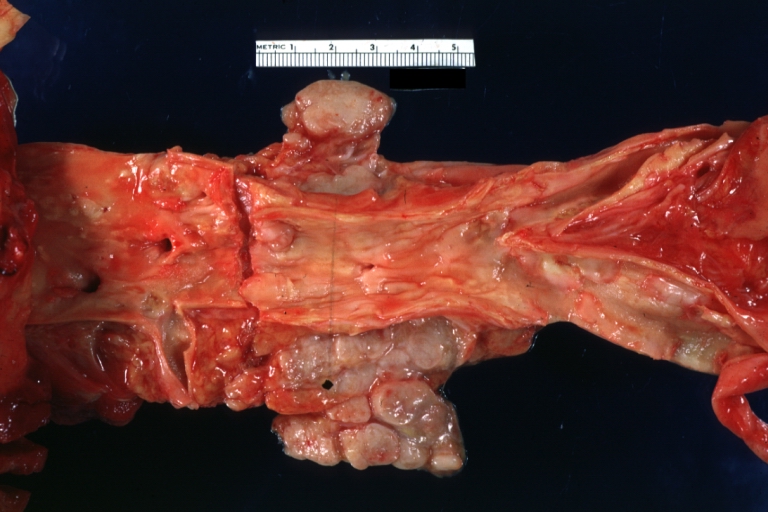
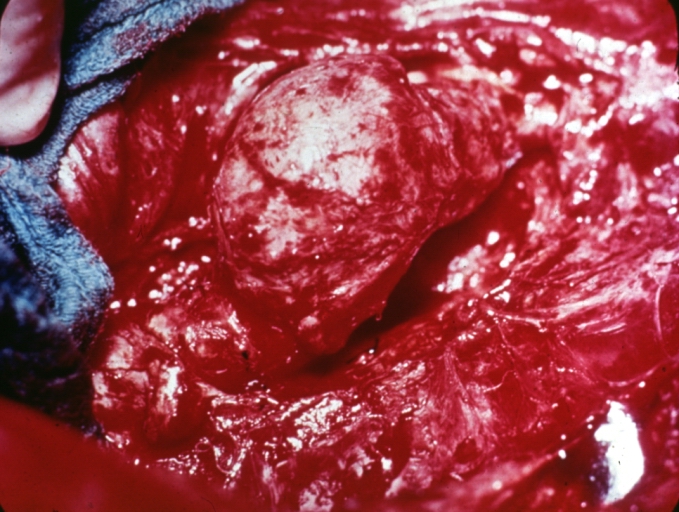
Atherosclerotic Aneurysm: Gross, a good example of typical abdominal aorta aneurysm with mural thrombus
-
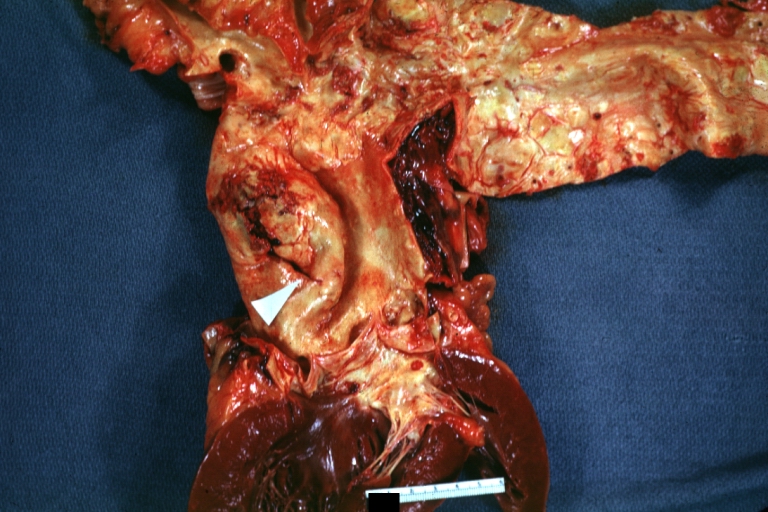
Dissecting Aneurysm: Gross, a very good example of dissection beginning just above aortic ring
-
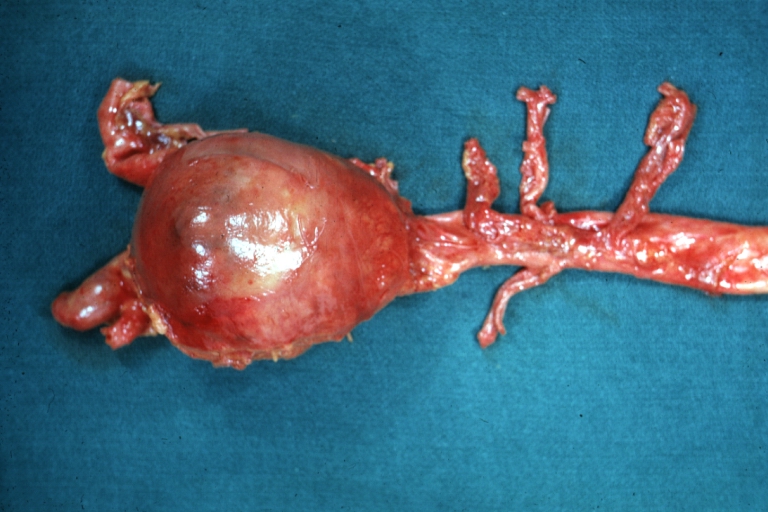
Atherosclerotic Aneurysm: Gross, (rather) good example of abdominal aortic aneurysm
-
Dissecting Aneurysm: Gross, an excellent example, starting just above the aortic valve with reflection of aorta to show the dissection tract and some thrombus
-
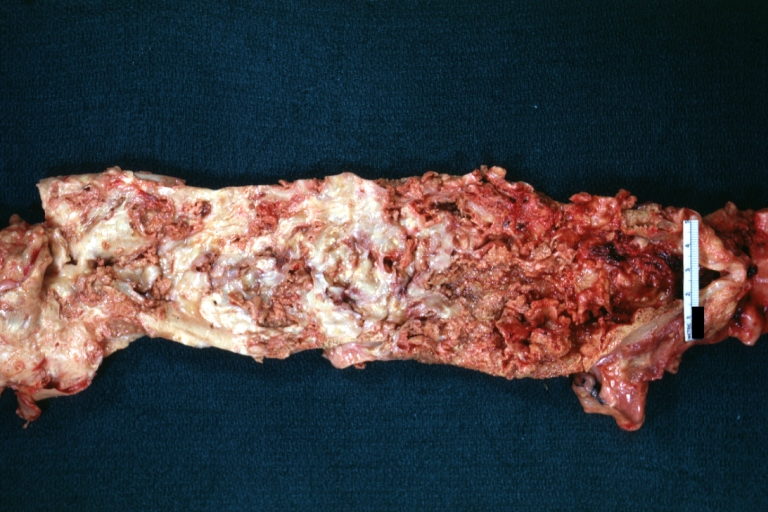
Dissecting Aneurysm: Gross shows dilated aorta with extensive atherosclerosis dissection is seen, a small abdominal aorta atherosclerotic aneurysm is present good for association of dilation with dissection
-
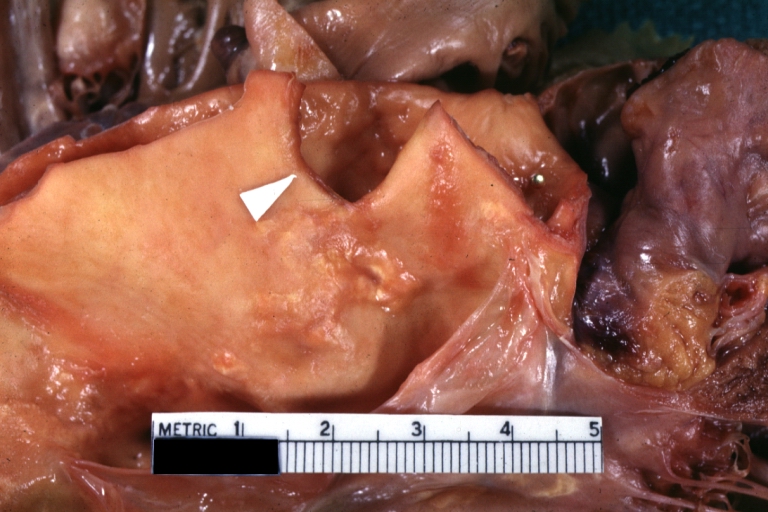
Dissecting Aneurysm: Gross arrow points to start of dissection in first portion aortic arch good but not the best example shows dilation
-
Dissecting Aneurysm: Gross, very good to show start of dissection above aortic valve and blood in false channel
-
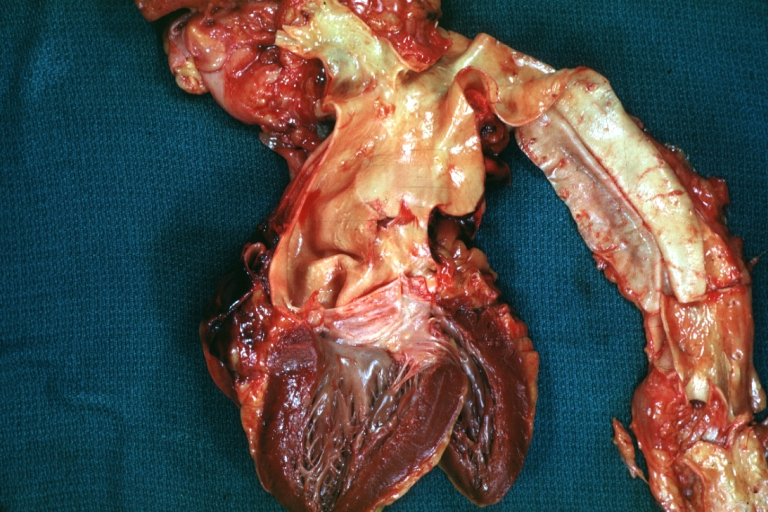
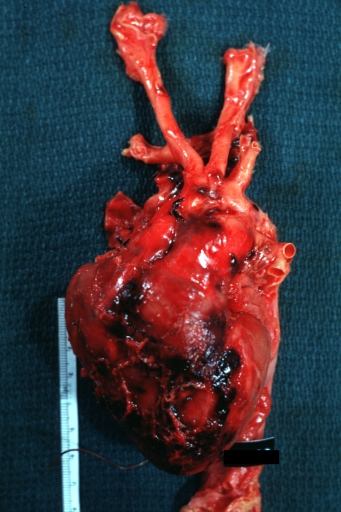
Dissecting Aneurysm: Gross, heart with root of aorta to show hemorrhage into pericardium (a very good example)
-
Dissecting Aneurysm: Gross, of heart and aorta with dissection and large false channel (a good example)
-
Dissecting Aneurysm: Gross cross section of aorta with two channels (a good example)
-
Atherosclerotic Aneurysm: Gross, a nice view of cross section of abdominal aorta aneurysm
-
Dissecting Aneurysm: Gross good example of typical angular tear above aortic valve
-
Dissecting Aneurysm: Gross good example angular tear above aortic valve
-
Atherosclerotic Aneurysm: Gross, external natural color very good example of an atherosclerotic thoracic aorta aneurysm with focal rupture
-
Atherosclerotic Aneurysm: Gross, excellent color, opened thoracic segment of aorta with two saccular atherosclerotic ruptured aneurysms
-
Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms
-
Atherosclerotic Aneurysm: Gross unopened lesion natural color
-
Dissecting Aneurysm: Gross dissection first portion of arch fixed specimen (a good example)
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
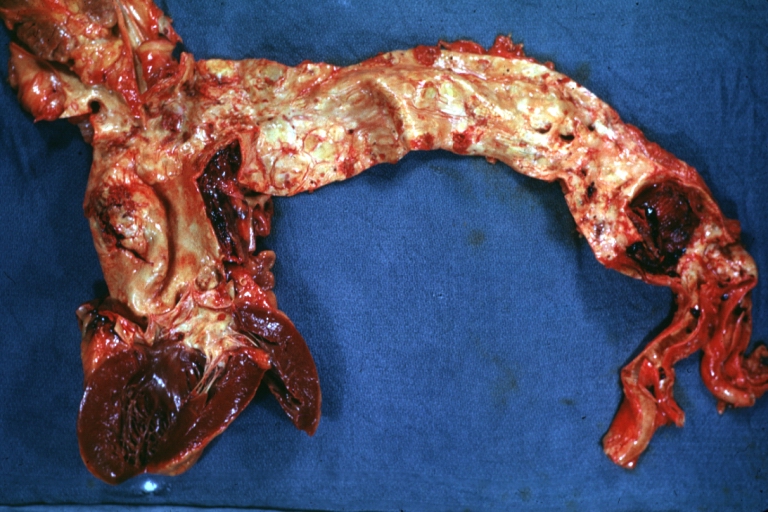
Dissecting Aneurysm: Gross, an excellent example of type I lesion
-
Dissecting Aneurysm: Gross, external view, an excellent example
-
Dissecting Aneurysm: Gross, Type I shows false channel
-
Dissecting Aneurysm: Gross, opened to show false channel (good example)
-
Atherosclerotic Aneurysm: Gross, very good example of ruptured thoracic segment
-
Dissecting Aneurysm: Gross, coagulum of blood in false channel
-
Dissecting Aneurysm: Gross, aortic valve area dissection (well shown, typical lesion)
-
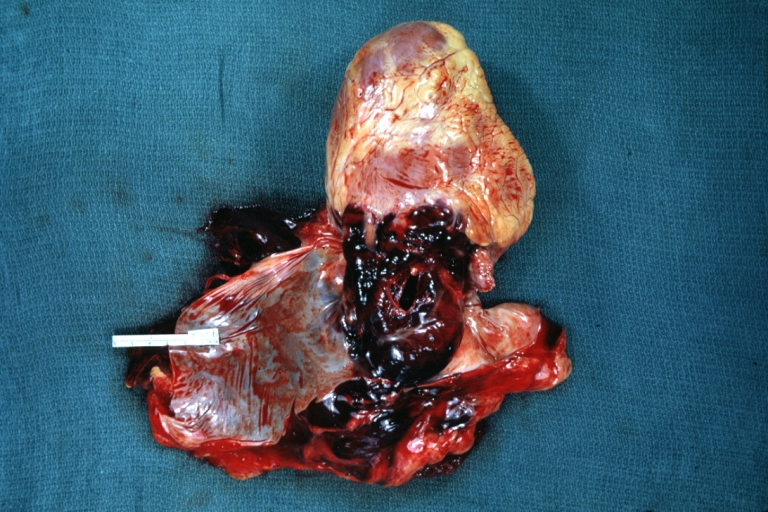
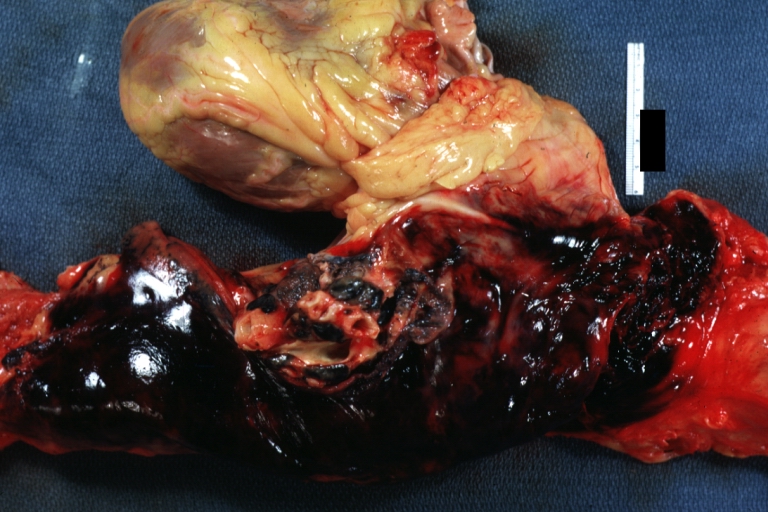
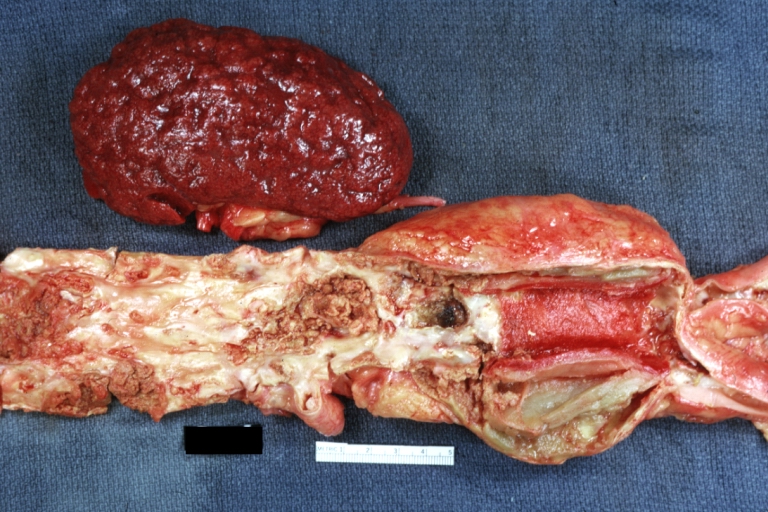
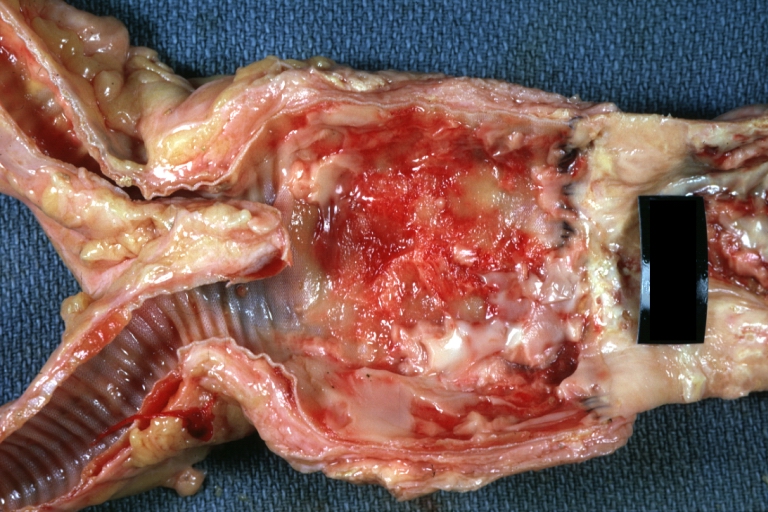
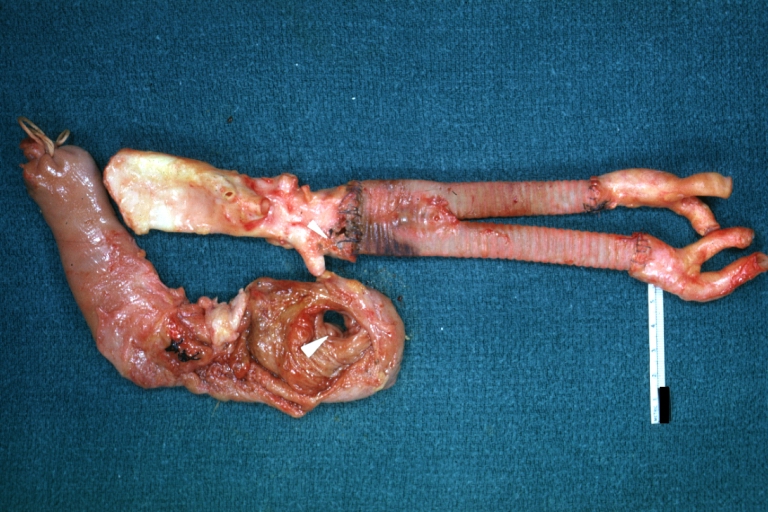
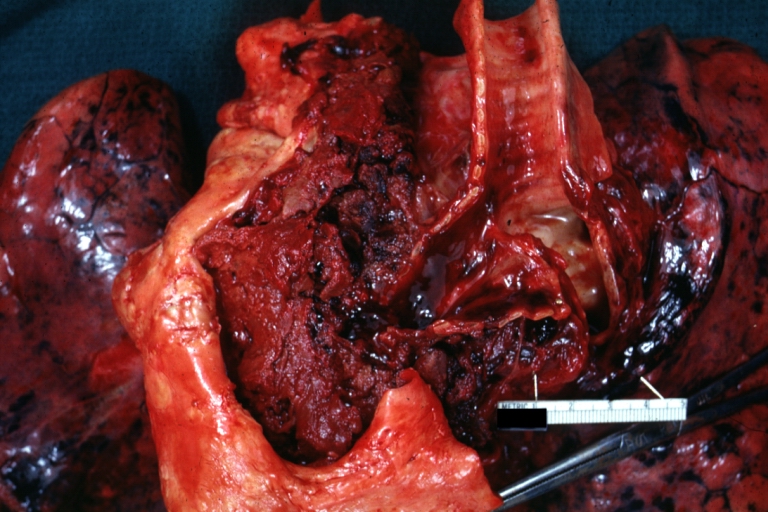
Abdominal Aneurysm Ruptured: Gross (good example) opened kidneys in marked place, atherosclerosis in lower thoracic aorta
-
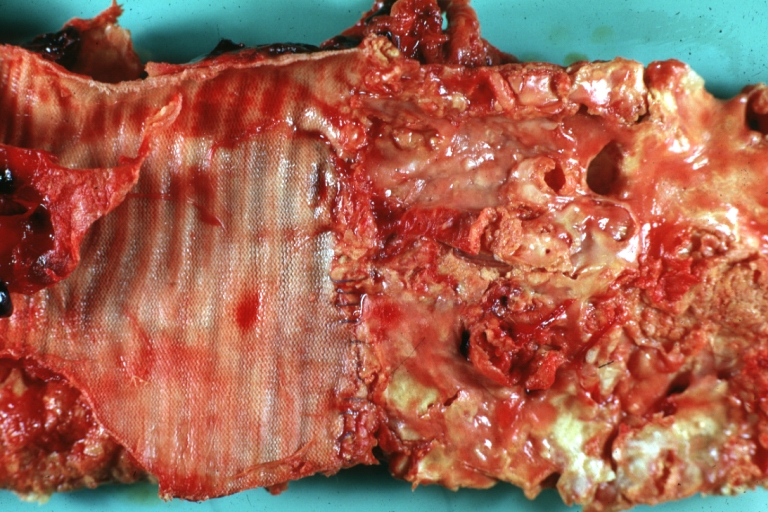
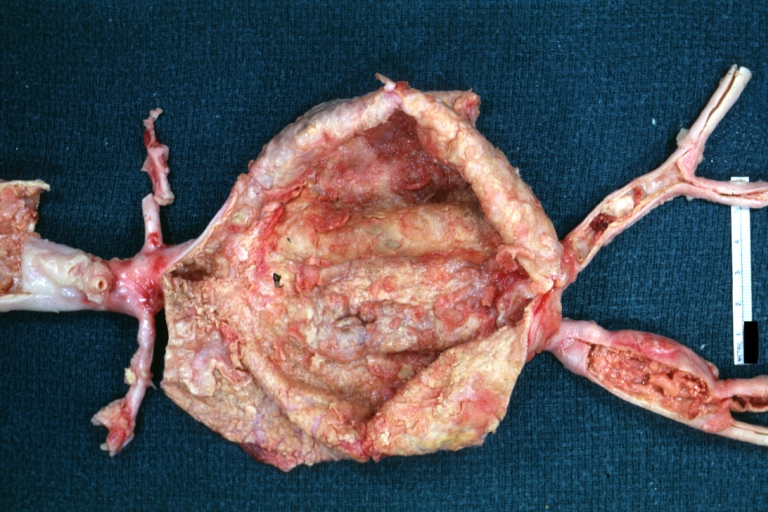
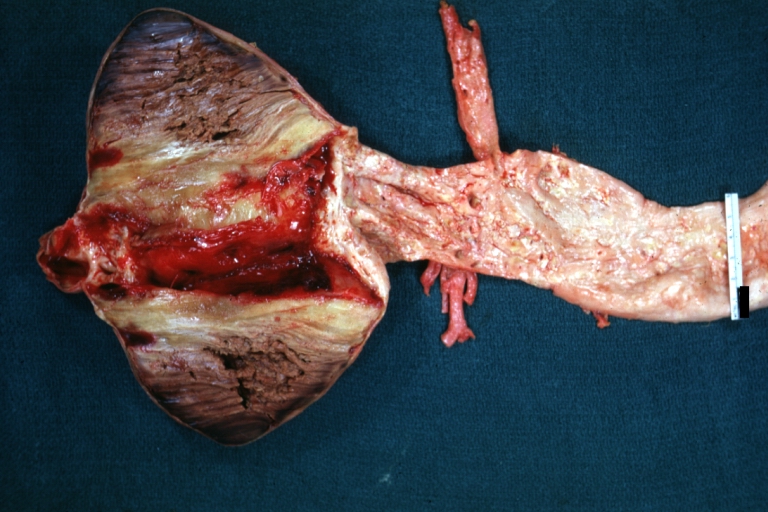
Abdominal Aneurysm: Gross, (very good example) opened lesion with mural thrombus
-
Dissecting Aneurysm: Gross, large tear in first portion of aortic arch, annuloaortic ectasis
-
Dissecting Aneurysm: Gross, external view of heart and first portion of aortic arch, annuloaortic ectasia, hemorrhage beneath adventitia is evidence of dissection
-
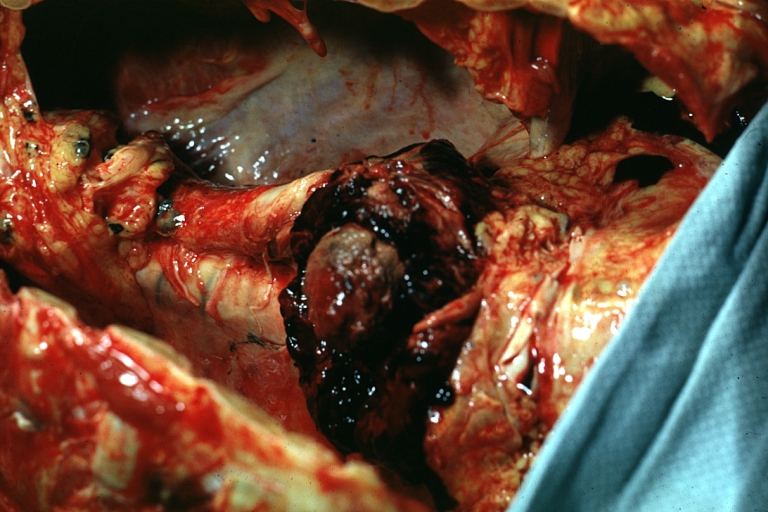
Atherosclerotic Aneurysm Infected: Gross, infected abdominal aneurysm at superior suture line with rupture into duodenum
-
Atherosclerotic Aneurysm: Gross, cross sections of repaired aneurysm showing Dacron graft and old mural thrombus. A nice example of fibrin layer in graft
-
Ruptured Syphilitic Aneurysm
-
Dissecting Aneurysm in a patient with Marfan's syndrome
-
Traumatic Aneurysm
-
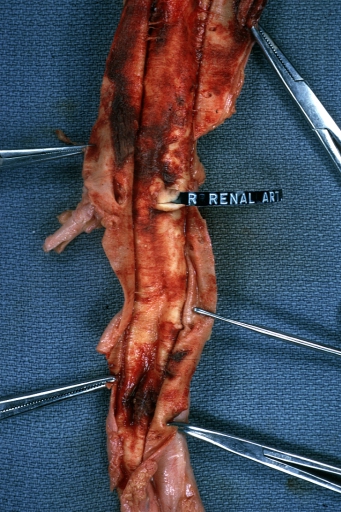
Kidney: Arteriosclerosis: Gross aorta with well shown renal artery containing large plaque and kidney with multiple cortical scars and atrophy also abdominal aorta aneurysm with mural thrombus (excellent example for renovascular hypertension)
-
Dissecting Aneurysm: Gross, fixed tissue, descending thoracic segment dissection opened to show the false channel. The true surface is also visible
-
Aneurysm: Gross, ruptured thoracic aorta aneurysm, in situ lower thoracic portion (probably due to atherosclerosis)
-
Abdominal Aneurysm Graft Repair: Gross, natural color, close-up view, an excellent example of Dacron graft that has been in place for years with pseudointima and atherosclerosis
-
Dacron Graft: Gross, close-up Dacron graft to repair aneurysm. Aorta completely covered with a calcified and ulcerated plaque with small mural thrombi (an excellent depiction of proximal suture line)
-
Dissecting Aneurysm: Gross natural color descending aorta opened into false channel
-
Abdominal Aneurysm: Gross, natural color, unopened specimen with about a six centimeter aneurysm between renals and bifurcation (a very good example of opened aneurysm)
-
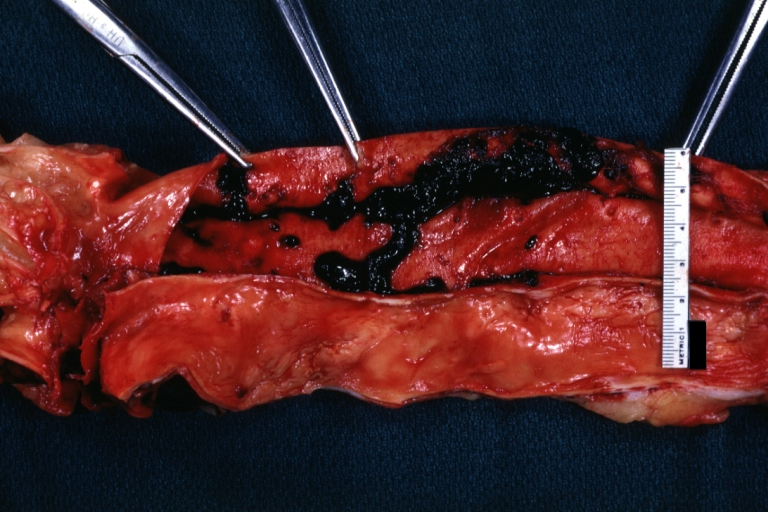
Abdominal Aneurysm: Gross, natural color, an opened aneurysm showing quite well laminated thrombus
-
Atherosclerosis with Mural Thrombi: Gross, natural color, a nice photo of descending thoracic aorta with extensive ulcerated plaques and mural thrombi in distal portion. The case also has an abdominal aneurysm
-
Pseudoaneurysm Ruptured Into Duodenum: Gross natural color aorta and duodenum with arrow pointing to rupture point of aortobifemoral bypass pseudoaneurysm rupture and another in duodenum a very good demonstration of this very well known complication of aortic prostheses
-
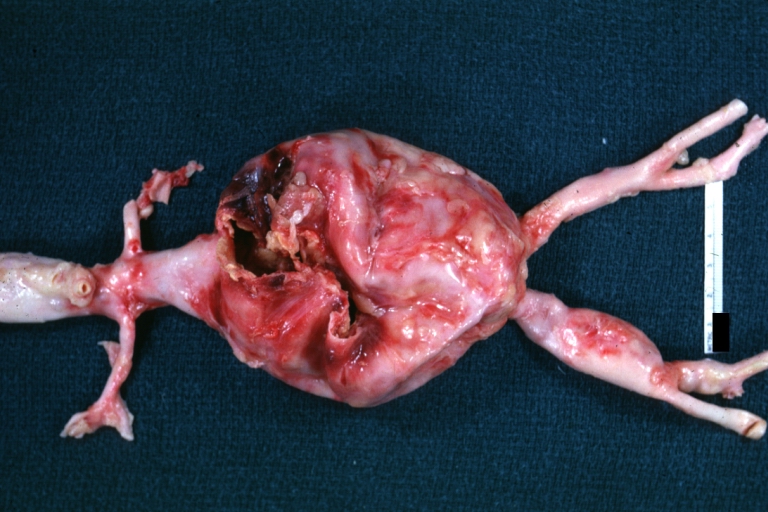
Abdominal Aneurysm: Gross, natural color, large aneurysm opened showing sessile calcified plaques with no mural thrombus. Lesion extends from renal arteries to the bifurcation (the same lesion seen externally with focus of rupture)
-
Abdominal Aneurysm Ruptured: Gross, natural color, external view with large area of apparent rupture. Aorta is opened to show this aneurysm)
-
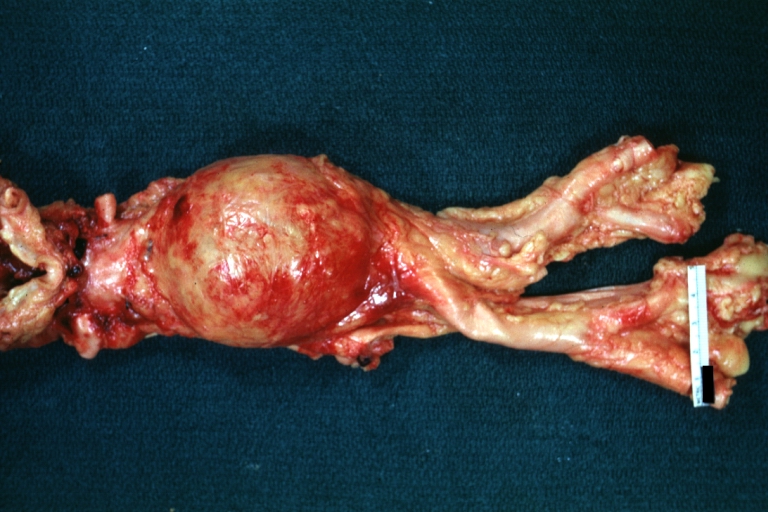
Abdominal Aneurysm: Gross, natural color, unopened large and quite typical aneurysm extending from below renal arteries to bifurcation
-
Abdominal Aneurysm: Gross, natural color, opened aneurysm with well shown and typical laminated thrombus (external view)
-
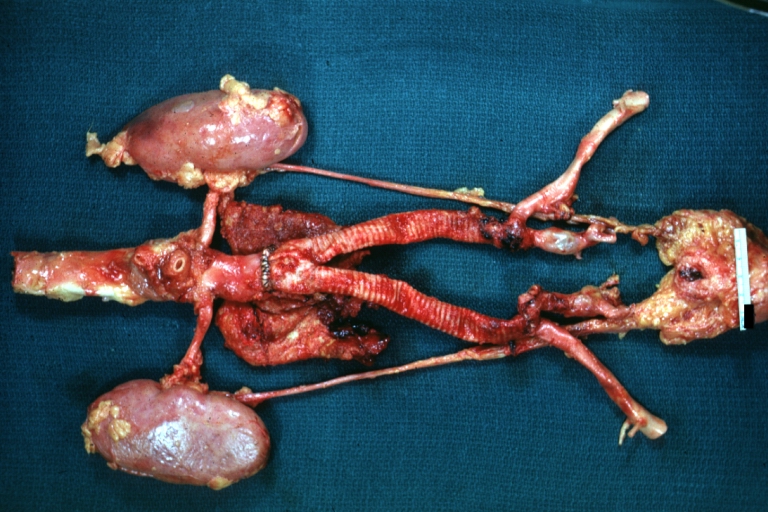
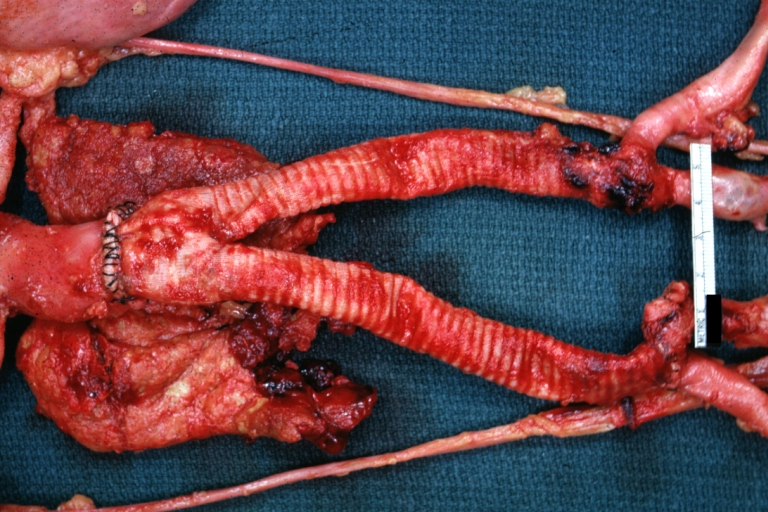
Aortobifemoral Prosthesis: Gross, natural color, nice dissection showing Dacron prosthesis replacing abdominal segment of aorta with portion of atherosclerotic aneurysm with renal arteries and kidneys
-
Aortobifemoral Prosthesis: Gross natural color close-up view of nicely dissected prosthesis extending from below renals to common iliac arteries portion of atherosclerotic aneurysm behind prosthesis
-
Dissecting Aneurysm: Gross natural color close-up view of aortic valve and proximal aortic arch with ruptured intima rather good illustration of this lesion
-
Syphilitic Aneurysm: Gross natural color rather a close-up view and outstanding photo of aneurysm ruptured into the left main stem bronchus
-
Syphilitic Aneurysm: Gross natural color typical tree barking in aorta aneurysm opening is seen in which is a thrombus aneurysm ruptured into left main stem bronchus (shown very well)
-
Dissecting Aneurysm Chronic: Gross natural color first portion of aortic arch with intimal rent well shown with healed margins and view into false channel that shows a surface looking like atherosclerosis which is known to develop in a chronic dissection
-
Dissecting Aneurysm Chronic: Gross, natural color, closer view of the previous one (a very good example)
Videos on Abdominal Aortic Aneurysm
<youtube v=Sb1bM8MnpRk/>
<youtube v=9XPPbWsrtRA/>
<youtube v=ovGI2fYc_U8/>
References
- ↑
- ↑
- ↑ O'Connor RE: Aneurysm, Abdominal, on emedicine, accessed June 23, 2006.
- ↑
- ↑ Rutherford RB. Randomized EVAR Trials and Advent of Level I Evidence: A Paradigm Shift in Management of Large Abdominal Aortic Aneurysms? Semin Vasc Surg 2006; 19:69-74. PMID 16782510
- ↑ Lederle FA, Kane RL, MacDonald R, Wilt TJ (2007). "Systematic review: repair of unruptured abdominal aortic aneurysm". Ann. Intern. Med. 146 (10): 735–41. PMID 17502634.
Acknowledgements
The content on this page was first contributed by: C. Michael Gibson M.S., M.D.