Right heart failure
| Right heart failure | |
 | |
|---|---|
| ICD-10 | I26, I27 |
| ICD-9 | 415.0 |
| MeSH | D011660 |
For the WikiPatient page for this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and Keywords: right ventricular failure, right heart failure, RV failure
Overview
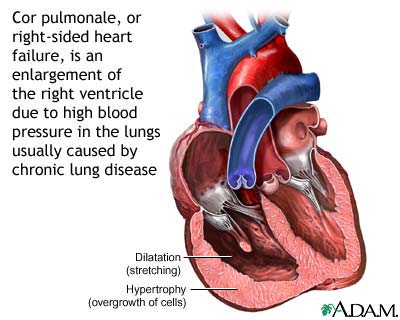
Cor pulmonale, also known as right heart failure, is a medical term used to describe a decline in right ventricular function, usually as result of either volume overload of the right ventricle or pressure overload of the right ventricle. When the term Cor pulmonale is applied, the right ventricular failure is due to an underlying respiratory disorder.
Pathophysiology
Right ventricular hypertrophy or RVH is the predominant change in chronic cor pulmonale although in acute cases dilation dominates. Both hypertrophy and dilation are the result of increased right ventricular pressure.
Dilation is essentially a stretching of the ventricle, the immediate result of increasing the pressure in an elastic container. Ventricular hypertrophy is an adaptive response to a long-term increase in pressure. Additional muscle grows to allow for the increased contractile force required to move the blood against greater resistance.
To be classified as cor pulmonale, the cause must originate in the pulmonary circulation system. Two major causes are vascular changes as a result of tissue damage (e.g. disease, hypoxic injury, chemical agents etc.), and chronic hypoxic pulmonary vasoconstriction. RVH due to a systemic defect is not classified as cor pulmonale.
There are several pathophysiologic mechanisms leading to pulmonary arterial hypertension and cor pulmonale:
- Pulmonary vasoconstriction
- Anatomic changes in vascularization
- Increased blood viscosity
- Idiopathic or primary pulmonary hypertension
- Increased volume overload of the right ventricle (e.g. Atrial septal defect
Causes
Acute
- Massive pulmonary embolization
- Exacerbation of chronic cor pulmonale
Chronic
- COPD
- Loss of lung tissue following trauma or surgery
- Pierre Robin Sequence
- End stage Pneumoconiosis
Differential Diagnosis
In alphabetical order. [1] [2]
- Adenopathy
- Adult Respiratory Distress Syndrome (ARDS)
- After pulmonary resection
- Alpha-1 Antitrypsin Deficiency
- Alveolar hypoxia in chronic high altitude exposure
- Amyotrophic Lateral Sclerosis (ALS)
- Bilateral diaphragmatic paralysis
- Bronchiectasis
- Bronchopulmonary dysplasia following neonatal respiratory distress syndrome (RDS)
- Chest wall dysfunction
- Chronic bronchitis
- Chronic fungal obstruction
- Chronic Obstructive Pulmonary Disease (COPD)
- Collagen vascular disease
- Congenital heart disease
- Cystic Fibrosis
- Drug-induced lung disease
- Drugs
- Emphysema
- Fibrosing mediastinitis
- Guillain-Barre Syndrome
- Histiocytosis X
- HIV infection
- Hypersensitivity pneumonitis
- Idiopathic pulmonary fibrosis
- Impairment of the respiratory system
- Interstitial lung disease
- Kyphoscoliosis
- Left atrial myxoma
- Left ventricular failure
- Mitral valve disease
- Myasthenia Gravis
- Necrotizing and granulomatous arteritis
- Neuromuscular disease
- Obesity
- Persistent pulmonary hypertension of the newborn
- Pneumoconiose
- Poliomyelitis
- Portal hypertension
- Polyradiculitis
- Primary pulmonary hypertension
- Pulmonary capillary hemangiomatosis
- Pulmonary embolism
- Pulmonary emphysema
- Pulmonary fibrosis
- Sarcoidosis
- Schistosomiasis
- Sickle Cell Anemia
- Sleep Apnea
- Tuberculosis
- Tumor embolism
- Tumor masses
- Veno-occlusive lung disease
- Scleroderma
Complications
Blood backups up into the system venous system, including the hepatic vein. Chronic congestion in the centrilobular region of the liver leads to hypoxia and fatty changes of more peripheral hepatocytes, leading to what's known as nutmeg liver. Left untreated, cor pulmonale can lead to right heart failure and death.
Treatment
Elimination of the cause is the most important intervention. In pulmonary embolism, thrombolysis (enzymatic dissolution of the blood clot) is advocated if there is dysfunction of the right ventricle. In COPD, long-term oxygen therapy may improve cor pulmonale.
Cor pulmonale may lead to congestive heart failure (CHF), with worsening of respiration due to pulmonary edema, swelling of the legs due to peripheral edema and painful congestive hepatomegaly. This situation requires diuretics (to decrease strain on the heart), sometimes nitrates (to improve blood flow), phosphodiesterase inhibitors like Sildenafil, tadalafil and occasionally inotropes (to improve heart contractility). CHF is a negative prognostic indicator in cor pulmonale.