Health issues and effects of cannabis
This article is about health issues and the effects of cannabis.
Today, there is still a substantial amount of propaganda and misinformation from both cannabis advocates and opponents due to the legal issues of cannabis, including legal and political constraints on cannabis research. While cannabis is associated with certain health risks, the Drug Awareness Warning Network Annual Report, published by the US federal government contains a statistical compilation of all drug deaths which occur in the United States. According to this report, there has never been a death recorded from the use of marijuana by natural causes.[1]
Biochemical effects
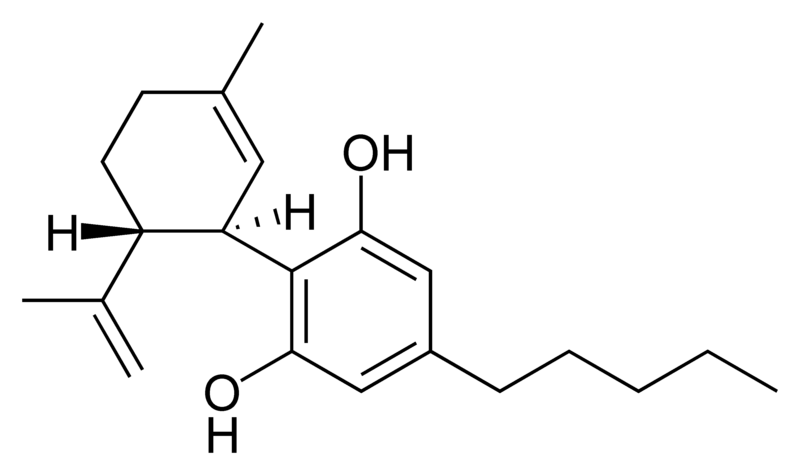
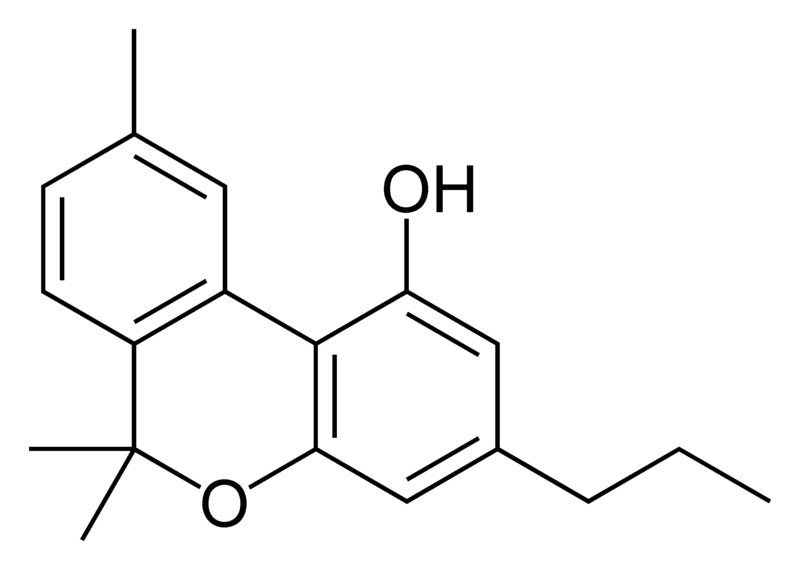
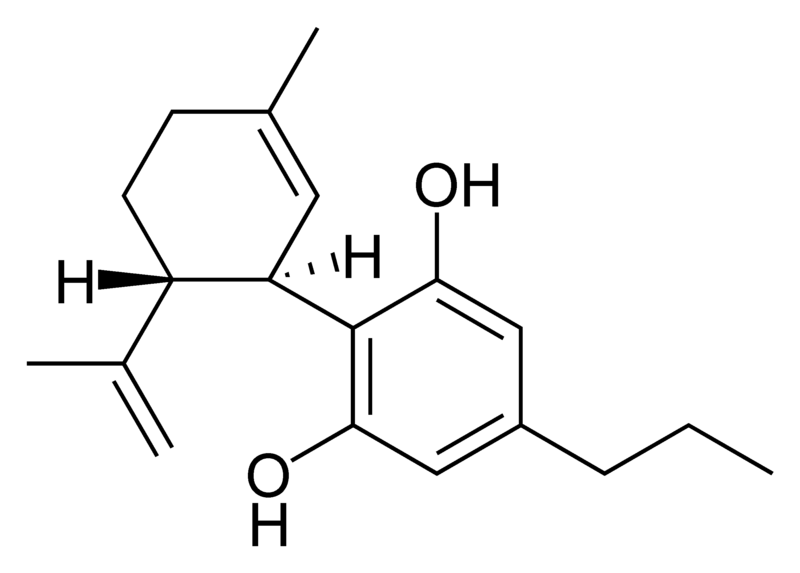
The most prevalent group of psychoactive substances in cannabis is delta-9-tetrahydrocannabinol (commonly called Δ9-THC, or simply THC). In the past two decades, the average content of THC in marijuana sold in North America has increased from about 1% to 3-4% or more. Carefully selected and cloned plants can yield as much as 15% THC (however in the Netherlands the maximum is 29% THC).[2] Another psychoactive cannabinoid present in Cannabis sativa is Tetrahydrocannabivarin (THCV), but it is only found in small amounts.[3] In addition, there are also similar compounds contained in cannabis that do not exhibit any psychoactive response but are obligatory for functionality: cannabidiol (CBD), an isomer of THC; cannabinol (CBN), an oxidation product of THC; cannabivarin (CBV), an analog of CBN with a different sidechain, Cannabidivarin (CBDV), an analog of CBD with a different sidechain, and cannabinolic acid. How these other compounds interact with THC is not fully understood. Some clinical studies have proposed that CBD acts as a balancing force to regulate the strength of the psychoactive agent THC. Anecdotal and inconclusive reports claim that marijuana with relatively high ratios of THC:CBD is less likely to induce anxiety than marijuana with low THC:CBD ratios.[4] CBD is also believed to regulate the body’s metabolism of THC by inactivating cytochrome P450, an important class of enzymes that metabolize drugs. Experiments in which mice were treated with CBD followed by THC showed that CBD treatment was associated with a substantial increase in brain concentrations of THC and its major metabolites, most likely because it decreased the rate of clearance of THC from the body.[4] Cannabis cofactor compounds have also been linked to lowering body temperature, modulating immune functioning, and cell protection. The essential oil of cannabis contains many fragrant terpenoids which may synergize with the cannabinoids to produce their unique effects. THC is converted rapidly to 11-hydroxy-THC, which is also pharmacologically active, so the drug effect outlasts measurable THC levels in blood.[2]
In 1990, the discovery of cannabinoid receptors located throughout the brain and body, along with endogenous cannabinoid neurotransmitters like anandamide (a lipid material derived ligand from arachidonic acid), suggested that the use of cannabis affects the brain in the same manner as a naturally occurring brain chemical. Cannabinoids usually contain a 1,1'-di-methyl-pyrane ring, a variedly derivatized aromatic ring and a variedly unsaturated cyclohexyl ring and their immediate chemical precursors, constituting a family of about 60 bi-cyclic and tri-cyclic compounds. Like most other neurological processes, the effects of cannabis on the brain follow the standard protocol of signal transduction, the electrochemical system of sending signals through neurons for a biological response. It is now understood that cannabinoid receptors appear in similar forms in most vertebrates and invertebrates and have a long evolutionary history of 500 million years. Cannabinoid receptors decrease adenylyl cyclase activity, inhibit calcium N channels, and disinhibit K+A channels. There are two types of cannabinoid receptors (CB1 and CB2).
The CB1 receptor is found primarily in the brain and mediates the psychological effects of THC. The CB2 receptor is most abundantly found on cells of the immune system. Cannabinoids act as immunomodulators at CB2 receptors, meaning they increase some immune responses and decrease others. For example, nonpsychotropic cannabinoids can be used as a very effective anti-inflammatory.[4] The affinity of cannabinoids to bind to either receptor is about the same, with only a slight increase observed with the plant-derived compound CBD binding to CB2 receptors more frequently. Cannabinoids likely have a role in the brain’s control of movement and memory, as well as natural pain modulation. It is clear that cannabinoids can affect pain transmission and, specifically, that cannabinoids interact with the brain's endogenous opioid system and may affect dopamine transmission.[5] This is an important physiological pathway for the medical treatment of pain.
The cannabinoid receptor is a typical member of the largest known family of receptors called a G protein-coupled receptor. A signature of this type of receptor is the distinct pattern of how the receptor molecule spans the cell membrane seven times. The location of cannabinoid receptors exists on the cell membrane, and both outside (extracellularly) and inside (intracellularly) the cell membrane. CB1 receptors, the bigger of the two, are extraordinarily abundant in the brain: 10 times more plentiful than μ-opioid receptors, the receptors responsible for the effects of morphine. CB2 receptors are structurally different (the homology between the two subtypes of receptors is 44%), found only on cells of the immune system, and seems to function similarly to its CB1 counterpart. CB2 receptors are most commonly prevalent on B-cells, natural killer cells, and monocytes, but can also be found on polymorphonuclear neurtrophil cells, T8 cells, and T4 cells. In the tonsils the CB2 receptors appear to be restricted to B-lymphocyte-enriched areas.
THC and endogenous anandamide additionally interact with glycine receptors.
Cannabis also contains a related class of compound: the Cannaflavins. These compounds have been suggested to contribute certain effects of cannabis, such as analgesia and anti-inflammatory properties, and are considerably more effective than aspirin. Cannaflavins usually contain a 1,4-pyrone ring fused to a variedly derivatized aromatic ring and linked to a 2nd variedly derivatized aromatic ring and include for example the non-psychoactive Cannflavin A and B.
The nature of cannabis, its lipophilic (fat soluble) properties, yields a long elimination half-life relative to other recreational drugs. The THC molecule, and related compounds, are usually detectable in drug tests for up to approximately one month after using cannabis (see drug test). This detection is possible because non-psychoactive THC metabolites are stored for long periods of time in fat cells, and THC has an extremely low water solubility. It is this slow and steady removal from the body that is linked with usually mild or nonexistent withdrawal symptoms after single or occasional use of the drug. The rate of elimination of metabolites is slightly greater for more frequent users due to tolerance.[citation needed]
The LD50 of THC is 1270 mg/kg (male rats), 730 mg/kg (female rats) oral in sesame oil, and 42 mg/kg (rats) from inhalation.[6]
Physiological effects
The psychoactive effects of cannabis, known as a "high", are subjective and can vary based on the individual. Some effects may include general change in consciousness (altered perception); mild euphoria; feelings of well-being, relaxation or stress reduction; lethargy; increased appreciation of humor, music or art; joviality; metacognition and introspection; enhanced recollection of episodic memory; increased sensuality; increased awareness of sensation; increased libido; creative or philosophical thinking; disruption of linear memory; paranoia, agitation or anxiety; experiential augmentation of other psychedelics and increased awareness of patterns and color.
Some of the effects of cannabis use include increased heart rate, dryness of the mouth, reddening of the eyes (congestion of the conjunctival blood vessels), a reduction in intra-ocular pressure, mild impairment of motor skills and concentration, and increased hunger. Electroencephalography or EEG shows somewhat more persistent alpha waves of slightly lower frequency than usual.[2] Cannabis also produces many subjective effects, such as greater enjoyment of food's taste and aroma and an enhanced enjoyment of music and comedy. At higher doses, cannabis can cause marked distortions in time and space perception, altered body image, auditory and/or visual illusions, ataxia from selective impairment of polysynaptic reflexes, and depersonalization.
The total short-term duration of cannabis intoxication when smoked is about 1 to more than 8 hours depending on percent of THC in the cannabis. A study of ten healthy male volunteers who resided in a residential research facility sought to examine both acute and residual subjective, physiologic, and performance effects of smoking marijuana cigarettes. On three separate days, subjects smoked one NIDA marijuana cigarette containing either 0%, 1.8%, or 3.6% THC, documenting subjective, physiologic, and performance measures prior to smoking, five times following smoking on that day, and three times on the following morning. Subjects reported robust subjective effects following both active doses of marijuana, which returned to baseline levels within 3.5 hours. Heart rate increased and the puplilary light reflex decreased following active dose administration with return to baseline on that day. Additionally, marijuana smoking acutely produced decrements in smooth pursuit eye tracking. Although robust acute effects of marijuana were found on subjective and physiological measures, no effects were evident the day following administration, indicating that the residual effects of smoking a single marijuana cigarette are minimal.[7]
A Dutch double-blind, randomized, placebo-controlled, cross-over study examining male volunteers aged 18–45 years with a self-reported history of regular cannabis use concluded that smoking of cannabis with high THC levels (marijuana with 9–23% THC), as currently sold in coffee shops in the Netherlands, may lead to higher THC blood-serum concentrations. This is reflected by an increase of the occurrence of impaired psychomotor skills, particularly among younger or inexperienced cannabis smokers, who do not adapt their smoking-style to the higher THC content.[8] High THC concentrations in cannabis was associated with a dose-related increase of physical effects (such as increase of heart rate, and decrease of blood pressure) and psychomotor effects (such as reacting more slowly, being less concentrated, making more mistakes during performance testing, having less motor control, and experiencing drowsiness). It was also observed during the study that the effects from a single joint lasted for more than eight hours. Reaction times were remained impaired five hours after smoking, when the THC serum concentrations were significantly reduced, but still present. When subjects smoke on several occasions per day, accumulation of THC in blood-serum may occur.
Another study showed that consumption of 15 mg of Delta(9)-THC resulted in no learning whatsoever occurring over a three-trial selective reminding task after two hours. In several tasks, delta(9)-THC increased both speed and error rates, reflecting “riskier” speed–accuracy trade-offs.[9]
A 2008 study by the National Institutes of Health suggested a link between heavy long-term marijuana smoking (138 joints per week over 6 years) and increased risk of heart attack or stroke.[10]
Neurological effects
The areas of the brain where cannabinoid receptors are most prevalently located are consistent with the behavioral effects produced by cannabinoids. Brain regions in which cannabinoid receptors are very abundant are the basal ganglia, associated with movement control; the cerebellum, associated with body movement coordination; the hippocampus, associated with learning, memory, and stress control; the cerebral cortex, associated with higher cognitive functions; and the nucleus accumbens, regarded as the reward center of the brain. Other regions where cannabinoid receptors are moderately concentrated are the hypothalamus, which regulates homeostatic functions; the amygdala, associated with emotional responses and fears; the spinal cord, associated with peripheral sensations like pain; the brain stem, associated with sleep, arousal, and motor control; and the nucleus of the solitary tract, associated with visceral sensations like nausea and vomiting.[11]
Most notably, the two areas of motor control and memory are where the effects of cannabis are directly and irrefutably evident. Cannabinoids, depending on the dose, inhibit the transmission of neural signals through the basal ganglia and cerebellum. At lower doses, cannabinoids seem to stimulate locomotion while greater doses inhibit it, most commonly manifested by lack of steadiness (body sway and hand steadiness) in motor tasks that require a lot of attention. Other brain regions, like the cortex, the cerebellum, and the neural pathway from cortex to striatum, are also involved in the control of movement and contain abundant cannabinoid receptors, indicating their possible involvement as well.
Experiments on animal and human tissue have shown the potential for the disruption of short-term memory,[4] which is consistent with the abundance of CB1 receptors on the hippocampus. The effects of THC at these receptor sites produce what resembles a "temporary hippocampal lesion."[4] As a result of this, several neurotransmitters like acetylcholine, norepinephrine, and glutamate, are released that trigger a major decrease in neuronal activity in the hippocampus and its inputs. In the end, this procedure could lead to the blocking of cellular processes that are associated with memory formation. There is no scientific evidence to suggest that these effects are permanent, and normal neurological functionality is eventually regained, usually as the drug is metabolized.
In in-vitro experiments THC at extremely high concentrations, which could not be reached with commonly consumed doses, caused competitive inhibition of the AChE enzyme and inhibition of β-amyloid peptide aggregation, the cause of Alzheimer's disease[12]
Long-term, heavy cannabis use (five joints daily for ten years) may be associated with structural abnormalities in the hippocampus and amygdala areas of the brain, according to a report in the June, 2008 issue of Archives of General Psychiatry. The hippocampus, thought to regulate emotion and memory, and the amygdala, involved with fear and aggression, tended to be smaller in cannabis users than in controls (volume was reduced by an average of 12 percent in the hippocampus and 7.1 percent in the amygdala).[13]
Reproductive effects
This article or section appears to contradict itself. |
Marijuana enhances both male and female orgasms, while at the same time delaying ejaculation.[14] But, it has been shown that administration of high doses of THC to animals lowers serum testosterone levels, impairs sperm production, motility, and viability, disrupts the ovulation cycle, and decreases output of gonadotropic hormones. However, there are also contradictory reports, and it is also possible that tolerance develops to these effects.[2][15] According to the 1997 Merck Manual of Diagnosis and Therapy, fertility effects related to cannabis use are uncertain.
Research has demonstrated that human sperm contains receptors which are stimulated by substances like THC and other cannabis-related chemicals. Tests have implied that smoking of marijuana could impact the sperm's functions, though this impact is unknown.[16] While many men who use cannabis have fathered children, certain menTemplate:Specify at risk for infertility may be more susceptible to reproductive complications.
Pregnancy
One study by Zuckerman and colleagues included a large sample of women with a substantial prevalence of marijuana use that was verified by urine analysis and no increased probability of birth defects was found in the sample group. Opposed to fetal alcohol syndrome, similar type facial features and related symptoms are not associated with prenatal marijuana exposure.[17] THC passes into the breast milk and may affect a breastfed infant.[18] Many studies about drug use during pregnancy are self-administered by the applicants and not always anonymous. The stigma of using illicit drugs while pregnant discourages honest reporting and can invalidate the results. Studies show that women who consume cannabis while they are pregnant may also be likely to consume alcohol, tobacco, caffeine, or other illicit drugs, which makes it difficult to deduce scientific facts about just marijuana use from statistical results. Very few large, well-controlled epidemiological studies have taken place to understand the connection of marijuana use and pregnancy.
A study of the development of 59 Jamaican children, one-half of the sample's mothers used marijuana during pregnancy, was research from birth to age 5 years. Pregnant non-using mothers were paired with cannabis users who matched age, parity, and socioeconomic status. Testing was done at 1, 3, and 30 days of age with the Brazelton Neonatal Behavioral Assessment Scales, and at ages 4 and 5 years with the McCarthy Scales of Children's Abilities test. Data was also collected from the child's home environment and temperament, as well as standardized tests. The results over the entire research period showed no significant differences in development testing outcomes between using and non-using mothers. At 30 days of age, however, the children of marijuana-using mothers had higher scores on autonomic stability and reflexes.[19] The absence of any differences between the exposed and nonexposed groups in the early neonatal period suggest that the better scores of exposed neonates at 1 month are traceable to the cultural positioning and social and economic characteristics of mothers using marijuana that select for the use of marijuana but also promote neonatal development.[20]
Some studies have found that children of tobacco and marijuana-smoking mothers more frequently suffer from permanent cognitive deficits, concentration disorders, hyperactivity, and impaired social interactions than non-exposed children of the same age and social background.[21][22] A recent study with participation of scientists from Europe and the United States, have now identified that endogenous cannabinoids, molecules naturally produced by our brains and functionally similar to THC from cannabis, play unexpectedly significant roles in establishing how certain nerve cells connect to each other. The formation of connections among nerve cells occurs during a relatively short period in the fetal brain. The study tries to give a closer understanding of if and when cannabis damages the fetal brain.[23][24][25]
Harkany and his colleagues cultured mouse embryonic brain cells that expressed cannabinoid receptor proteins (CBRs) and exposed them to gradients of synthetic cannabinoids. The cells withdrew their rootlike feelers, or axons, from the high concentration of cannabinoids; the axons, which seek out and communicate with neighboring cells, veered instead in other directions, In effect, "if you activate the cannabinoid system" of these cells, Harkany says, "it will send a message to the cell that 'I don't want to grow there, I want to grow somewhere else'" and connect to another cell. [26]
Other studies on Jamaica have suggested that cannabis use by expectant mothers does not appear to cause birth defects or developmental delays in their newborn children.[27][28] In a study in 1994 of Twenty-four Jamaican neonates exposed to marijuana prenatally and 20 non exposed neonates comparisons were made at 3 days and 1 month old, using the Brazelton Neonatal Assessment Scale, including supplementary items to capture possible subtle effects. Results showed there were no significant differences between exposed and nonexposed neonates on day 3. At 1 month, the exposed neonates showed better physiological stability and required less examiner facilitation to reach organized states. The neonates of heavy-marijuana-using mothers had better scores on autonomic stability, quality of alertness, irritability, and self-regulation and were judged to be more rewarding for caregivers. This work was supported by the March of Dimes Foundation.[29]
Toxicity
This article may be confusing or unclear to readers. (February 2008) (Learn how and when to remove this template message) |
THC has an extremely low toxicity and the amount that can enter the body through the consumption of cannabis plants poses no threat of death. In lab animal tests, scientists have had much difficulty administering a dosage of THC that is high enough to be lethal. It also appears that humans cannot die from ingesting too much THC, unless it were introduced into the body intravenously.[citation needed] Indeed, a 1988 ruling from the United States Department of Justice concluded that "In practical terms, marijuana cannot induce a lethal response as a result of drug-related toxicity."[30]
According to the Merck Index,[31] the LD50 (dosage lethal to 50% of rats tested) of Δ9-THC by inhalation is 42 mg/kg of body weight. That is the equivalent of a man weighing 75 kg (164.0625 lb) inhaling the THC found in 21 grams of extremely high-potency (15% THC) marijuana all in one sitting, assuming no THC is lost through smoke loss or absorption by the lungs. For oral consumption, the LD50 for male rats is 1270 mg/kg, and 730 mg/kg for females—equivalent to the THC in about a pound of 15% THC marijuana.[32]
The ratio of cannabis material required to saturate cannabinoid receptors to the amount required for a fatal overdose is 40,000:1 [12][13]; consumption of such a large dose is virtually impossible. There have been no reported deaths or permanent injuries sustained as a result of a marijuana overdose [14][15][16][17][18]. It is, for all practical purposes, impossible to overdose on marijuana, as the user would certainly either fall asleep or otherwise become incapacitated from the effects of the drug before being able to consume enough THC to be mortally toxic. According to a 2006 United Kingdom government report, using cannabis is much less dangerous than tobacco, prescription drugs, and alcohol in social harms, physical harm, and addiction.[33] It was found in 2007 that while tobacco and cannabis smoke are quite similar, cannabis smoke contained higher amounts of ammonia, hydrogen cyanide, and nitrogen oxides, but somewhat lower levels of carcinogenic polycyclic aromatic hydrocarbons (PAHs).[34]
Adulterated cannabis
Contaminants may be found in hashish when consumed from soap bar-type sources.[35] The dried flowers of the plant may be contaminated by the plant taking up heavy metals and other toxins from its growing environment,[36] or by the addition of glass beads, used to increase the weight and to make the cannabis appear as if it has more 'crystals' indicating a higher THC content. [37]
Confounding combination
The most obvious confounding factor in cannabis research is the prevalent usage of other recreational drugs, including alcohol and tobacco.[38] Such complications demonstrate the need for studies on cannabis that have stronger controls, and investigations into the symptoms of cannabis use that may also be caused by tobacco. Some people question whether the agencies that do the research try to make an honest effort to present an accurate, unbiased summary of the evidence, or whether they "cherry-pick" their data, and others caution that the raw data, and not the final conclusions, are what should be examined.[39]
Cannabis also has been shown to have a synergistic cytotoxic effect on lung cancer cell cultures in vitro with the food additive butylated hydroxyanisole (BHA) and possibly the related compound butylated hydroxytoluene (BHT). The study concluded, "Exposure to marijuana smoke in conjunction with BHA, a common food additive, may promote deleterious health effects in the lung." BHA & BHT are human-made fat preservatives, and are found in many packaged foods including: plastics in boxed Cereal, Jello, Slim Jims, and more.[40]
Psychological effects
Addiction
Animal research has shown that the potential for cannabinoid addiction does exist. Research suggests cannabis withdrawal is similar to tobacco withdrawal.[41] Heavy users experience withdrawal symptoms such as insomnia, restlessness, loss of appetite, depression, irritability, and anger after ceasing use.[42]. Prolonged marijuana use produces both pharmacokinetic changes (how the drug is absorbed, distributed, metabolized, and excreted) and pharmacodynamic changes (how the drug interacts with target cells) to the body. These changes require the user to consume higher doses of the drug to achieve a common desirable effect, and reinforce the body’s metabolic systems for synthesizing and eliminating the drug more efficiently.[4]
Preliminary research, published in the April 2006 issue of the Journal of Consulting and Clinical Psychology, indicates that cannabis addiction can be offset by a combination of cognitive-behavioral therapy and motivational incentives. Participants in the study (previously diagnosed with marijuana dependence) received either vouchers as incentives to stay drug free, cognitive-behavioral therapy, or both over a 14-week period. At the end of 3 months, 43 percent of those who received both treatments were no longer using marijuana, compared with 40 percent of the voucher group, and 30 percent of the therapy group. At the end of a 12-month follow-up, 37 percent of those who got both treatments remained abstinent, compared with 17 percent of the voucher group, and 23 percent of the therapy group.[43]
A 1998 French governmental report commissioned by Health Secretary of State Bernard Kouchner, and directed by Dr. Pierre-Bernard Roques, classed drugs according to addictiveness and neurotoxicity. It placed heroin, cocaine and alcohol in the most addictive and lethal categories; benzodiazepine, hallucinogens and tobacco in the medium category, and cannabis in the last category. The report stated that "Addiction to cannabis does not involve neurotoxicity such as it was defined in chapter 3 by neuroanatomical, neurochemical and behavioral criteria. Thus, former results suggesting anatomic changes in the brain of chronic cannabis users, measured by tomography, were not confirmed by the accurate modern neuro-imaging techniques. Moreover, morphological impairment of the hippocampus [which plays a part in memory and navigation] of rat after administration of very high doses of THC (Langfield et al., 1988) was not shown (Slikker et al., 1992)." Health Secretary Bernard Kouchner concluded that : "Scientific facts show that, for cannabis, no neurotoxicity is demonstrated, to the contrary of alcohol and cocaine."[44]
Mental health
Cannabis use has been assessed by several studies to be correlated with the development of anxiety, psychosis and depression,[45][46] however, the causality of the correlation and its direction is a subject of debate that hasn't been resolved in the scientific community. Some studies assess that the causality is more likely to involve a path from cannabis use to psychotic symptoms rather than a path from psychotic symptoms to cannabis use,[47] while others assess the opposite direction of the causality, or hold cannabis to only form parts of "causal constellation", while not inflicting mental health problems that would not have occurred in the absence of the cannabis use.[48][49]
A common interpretation of the correlation and theorized direction of the causality is the self-medication hypothesis, which is based on partially or fully attributing the correlation between psychiatric diseases and cannabis to the extensive substance abuse among sufferers of certain mental disorders, before diagnosis in many cases, which increases the likeliness of cannabis use among the mentally ill and the undiagnosed, thus accounting for correlation and debunking some claims of causality with the opposite direction.[50] As much as 60% of the mentally ill are suspected to be substance abusers, and many seem to prefer cannabis and alcohol.[51] Dr Stanley Zammit of Bristol and Cardiff universities (in the Daily express newspaper of the 27th of July 2007) reported "Even if cannabis did increase the risk of psychosis, most people using the drug would not get ill" But he added: "Nevertheless, we would still advise people to avoid or limit their use of this drug, especially if they start to develop any mental health symptoms or if they have relatives with psychotic illnesses." A 2007 study of studies published in the Lancet concluded that cannabis users are 40% more likely to be sufferers of a psychotic illness than non-users.[52] In comparison, alcohol, as the only intoxicating drug with similar levels of popularity, has been linked to more than 65% of all suicides in a UK study,[53] and linked to general psychiatric mental health problems including depression, anxiety, schizophrenia, psychosis, psychoneurosis, Post Traumatic Stress Disorder, physical brain damage and more.[53][54] That is not to suggest that alcohol can cause schizophrenia, and if it were to cause temporary psychosis, it would be ameliorated after cessation of its consumption.
Behavioral effects
Government studies often point to statistical data accumulated by methods like the National Household Survey on Drug Abuse (NHSDA), the Monitoring the Future study (MTF), and the Arrestee Drug Abuse Monitoring (ADAM) program, which claim lower school averages and higher dropout rates among users than nonusers, even though these differences are very small and may be exaggerated by the stigma attached to students who use the drug. However, the major contributor to a lack of credibility in these studies, is that in many cases, like with NHSDA and MTF, these surveys are usually self-administered and may be anonymous. The likeliness of over or under representing data definitely undermines the effectiveness of these instruments.[5] The MTF study is conducted anonymously, but only seeks information from a sample of people who have been arrested for drug-related offenses. Socially deviant behavior may be found more frequently in individuals of the criminal justice system compared to those in the general population, including non users. In response, independent studies of college students have shown that there was no difference in grade point average, and achievement, between marijuana users and nonusers, but the users had a little more difficulty deciding on career goals, and a smaller number were seeking advanced professional degrees.[55] Laboratory studies of the relationship between motivation and marijuana outside of the classroom, where volunteers worked on operant tasks for a wage representing a working world model, also fail to distinguish a noticeable difference between users and non users.[56]
At least one study has shown a decrease in depression in cannabis users.[57]
Gateway drug hypothesis
The gateway drug hypothesis asserts that the use of cannabis may ultimately lead to the use of harder drugs. For the most part, it was commonly thought that cannabis gateways to other drugs because of social factors. For example, the criminalization of cannabis in many countries associates its users with organized crime promoting the illegal drug trade.
A July 2006 study by Ellgren et al.[58] strictly tested lab rats for the biological mechanism of the gateway drug effect. The study administered 6 "teenage" (28 and 49 days old) rats delta-9-tetrahydrocannabinol, and 6 were the control. One week after the first part was completed, catheters were inserted in the jugular vein of all of the adult rats and they were able to self-administer themselves heroin by pushing a lever. The study found that initially both groups behaved the same and began to self-administer heroin frequently, but then stabilized at different levels. The rats that had previously been administered THC consumed about 1.5 times more heroin than those that had not. Because many THC receptors interact with the opioid system, the study found that adolescent cannabis use overstimulates and alters the pleasure and reward structures of the brain, thus increasing the already high risk of addiction for people who start to use heroin. However, Other studies have shown that the dopamine system is independent of the THC receptor glands thus negating these negative effects.[citation needed] Psychopharmacologist Ian Stolerman, from King's College London, finds the biological cannabis gateway drug effect "somewhat preliminary", and states "it's too early to say there's a consensus, but a small number of studies like this suggest that there is a physiological basis for this effect." Other drugs, he notes, such as cocaine and amphetamines are involved in another brain pathway called the dopaminergic system. Cells in that system also interact with THC receptors and could be modified by cannabis exposure.[59] Cannabinoid receptors are 10 times more prevalent in the brain than opioid receptors. According to Dr. Hurd, one of the study leaders, two other drugs that also stimulate opioid cells, and could therefore also feasibly cause a gateway effect, are nicotine and alcohol.
However, a December 2006 study by the American Psychiatric Association[60][61] challenges these findings. A 12 year study on 214 boys from ages 10-12 showed that adolescents who used marijuana prior to using other drugs, including alcohol and tobacco, were no more likely to develop a substance abuse disorder than other subjects in the study. "This evidence supports what's known as the common liability model ... [which] states [that] the likelihood that someone will transition to the use of illegal drugs is determined not by the preceding use of a particular drug, but instead by the user's individual tendencies and environmental circumstances," investigators stated in a press release. They added, "The emphasis on the drugs themselves, rather than other, more important factors that shape a person's behavior, has been detrimental to drug policy and prevention programs."
Models used in a 2002 study[62] by RAND cast doubt on the gateway effect and show "that the marijuana gateway effect is not the best explanation for the link between marijuana use and the use of harder drugs," as noted by Andrew Morral, associate director of RAND's Public Safety and Justice unit and lead author of the study.
Co-occurrence of mental illness
Studies have shown that a risk does exist in some individuals with a predisposition to mental illness to develop symptoms of psychosis.[63] The risk was found to be directly related to high dosage and frequency of use, early age of introduction to the drug, and was especially pronounced for those with a predisposition for mental illness. These results have been questioned as being biased by failing to account for medicinal versus recreational usage[64] — critics contend it could be a causal relationship, or it could be that people who are susceptible to mental problems tend to smoke cannabis, or it could be connected to the criminalization of cannabis. Another important question is whether the observed symptoms of mental illness are actually connected to development of a permanent mental disorder; cannabis may trigger latent conditions, or be part of a complex coordination of causes of mental illness, referred to in psychology as the diathesis-stress model. People with developed psychological disorders are known to self-medicate their symptoms with cannabis as well, although one study has claimed that those with a predisposition for psychosis did not show an increase in likelihood of cannabis use four years later.[citation needed]
Correlation versus causality
Some studies conclude that there is a correlation of cannabis use and some symptoms of psychosis, but don't necessarily support the notion that cannabis use is a sufficient or necessary cause for psychosis. It might be a component cause, part of a complex constellation of factors leading to psychosis, or it might be a correlation without forward causality at all.
For example, a review of the evidence by Louise Arsenault, et al., in 2004 reports that on an individual level, cannabis use confers an overall twofold increase in the relative risk of later schizophrenia, assuming a causal relationship. This same research also states that "There is little dispute that cannabis intoxication can lead to acute transient psychotic episodes in some individuals". The study synthesizes the results of several studies into a statistical model. The study does not correct for the use of other illicit drugs, and relies on self-reporting of cannabis dosage. The study also does not determine if the cannabis use preceded or followed the mental health problem.[65]
Similarly, a landmark study, in 1987, of 50,000 Swedish Army conscripts, found that those who admitted at age 18 to having taken cannabis on more than 50 occasions, were six times more likely to develop schizophrenia in the following 15 years. In fact, psychosis cases were restricted to patients requiring a hospital admission. These findings have not been replicated in another population based sample. As the study did not control for symptoms preexisting onset of cannabis use, the use of other illicit drugs, the study does not resolve the correlation versus causality question but has fueled a major debate within the scientific community. This study also used self reporting for cannabis dosage.[66]
A 2005 study found that "the onset of schizotypal symptoms generally precedes the onset of cannabis use. The findings do not support a causal link between cannabis use and schizotypal traits".[67] It should be noted that a schizotypal personality disorder is a personality disorder different from schizophrenia. A 2007 British study concluded, "We found few appreciable differences in symptomatology between schizophrenic patients who were or were not cannabis users. There were no differences in the proportion of people with a positive family history of schizophrenia between cannabis users and non-users. This argues against a distinct schizophrenia-like psychosis caused by cannabis."[68]
Research based on the Dunedin Multidisciplinary Health and Development Study has found that those who begin regular use of cannabis in early adolescence (from age 15, median 25 days per year by age 18) and also fit a certain genetic profile (specifically, the Val/Val variant of the COMT gene) are five times more likely to develop psychotic illnesses than individuals with differing genotypes, or those who do not use cannabis.[69][70] The study was noted for having controlled for preexisting symptoms, but is open to the criticism that it cannot control for late adolescent onset of psychotic illness. Also, the study was on a cohort population, so there is no way to correlate a change in the rate of adolescent use with a change in the rate of incidence of schizophrenia in the study population. These points undermine its value in resolving the correlation versus causality question.
A study that inversely correlated cerebrospinal anandamide (an endogenous cannabinoid) levels with severity of schizophrenia (i.e., that anandamide was released in order to suppress psychosis) suggests that cannabis use may be an effect of schizophrenia or its predisposition, as opposed to a cause.[71]
The fact that the prevalence of cannabis use has increased substantially during the last decades whereas the prevalence of psychotic illness has not suggests no causal relationship.[72]
Appetite
Clinical studies and survey data have found that cannabis increases food enjoyment and interest in food.[73][74] Scientists have claimed to be able to explain what causes the increase in appetite, concluding that "endocannabinoids in the hypothalamus activate cannabinoid receptors that are responsible for maintaining food intake".[74]
Memory
THC (the main psychoactive substance in Cannabis) is known to act on the hippocampus, an area of the brain associated with memory and learning, and impairs short term memory and attention for the duration of its effects; THC impairs episodic memory and learning in a dose-dependent manner whilst not affecting perceptual priming and working memory.[75]
Cannabis was found to be neuroprotective against excitotoxicity and is therefore beneficial for the prevention of progressive degenerative diseases like Alzheimer's disease.[76]
A 1998 report by INSERM and CNRS, which was directed by Dr. Pierre-Bernard Roques, determined that, "former results suggesting anatomic changes in the brain of chronic cannabis users, measured by tomography, were not confirmed by the accurate modern neuro-imaging techniques (such as MRI) ... Moreover, morphological impairment of the hippocampus [which plays a part in memory and navigation] of rat after administration of very high doses of THC was not shown". He concluded that cannabis does not have any neurotoxicity as defined in the report, unlike alcohol and cocaine.[77][78][79]
In contradiction to the INSERM/CNRS report, a 1998 Journal of Neuroscience article states THC is toxic for hippocampal neurons.[80]
Legal and political constraints on open research
In many countries, experimental science regarding cannabis is legally restricted because cannabis is illegal. Thus, cannabis as a drug is often hard to fit into the structural confines of medical research because appropriate, research-grade samples are difficult to obtain legally for research purposes, unless granted under authority of national governments.
United States
This issue was recently highlighted in the United States by the clash between Multidisciplinary Association for Psychedelic Studies (MAPS), an independent research group, and the National Institute on Drug Abuse (NIDA), a federal agency charged with the application of science to the study of drug abuse. The NIDA largely operates under the general control of the Office of National Drug Control Policy (ONDCP), a White House office responsible for the direct coordination of all legal, legislative, scientific, social and political aspects of federal drug control policy.
The cannabis that is available for research studies in the United States is grown at the University of Mississippi and solely controlled by the NIDA, which has veto power over the Food and Drug Administration (FDA) to define accepted protocols. Since 1942, when cannabis was removed from the U.S. Pharmacopoeia and its medical use was prohibited, there have been no legal (under federal law) privately funded cannabis production projects. This has resulted in a limited amount of research being done and possibly NIDA's producing cannabis which has been alleged to be of very low potency and inferior quality.[81]
MAPS, in conjunction with Professor Lyle Craker, PhD, the director of the Medicinal Plant Program of the University of Massachusetts at Amherst, sought to provide independently grown cannabis of more appropriate research quality for FDA-approved research studies, and encountered opposition by NIDA, the ONDCP, and the U.S. Drug Enforcement Administration (DEA).
United Kingdom
In countries such as the United Kingdom a license for growing cannabis is required if it is to be used for botanical or scientific reasons. It is referred to as a "controlled drug". In such countries a greater depth and variety of scientific research has been performed. Recently several habitual smokers were invited to partake in various tests by British medical companies in order for the UK government to ascertain the influence of cannabis on operating a motor vehicle.
Smoking
The process most popularly used to ingest cannabis is smoking, and for this reason most research has evaluated health effects from this method of ingestion. Other methods of ingestion may have lower or higher health risks. See section on harm reduction below for more information on other methods of ingestion.
Risks compared to tobacco
Tobacco smoking has well-established risks such as bronchitis, coughing, overproduction of mucus,wheezing and addiction. Similar risks for smoking cannabis related to airway inflammation have been suggested in a study of healthy cannabis users who exhibited similar early characteristics to tobacco smoking.[82]
The effects of tobacco and cannabis smoking differ, however, as they affect different parts of the respiratory tract: whereas tobacco tends to penetrate to the smaller, peripheral passageways of the lungs, cannabis tends to concentrate on the larger, central passageways. One consequence of this is that cannabis, unlike tobacco, does not appear to cause emphysema, though this claim is disputed. A 2002 report by the British Lung Foundation estimated that three to four cannabis cigarettes a day were associated with the same amount of damage to the lungs as 20 or more tobacco cigarettes a day.[83] Unlike tobacco, regular cannabis use does not appear to cause chronic obstructive pulmonary disease.[84]
It is important to note that in some cases, a cannabis user may mix commercial tobacco in joints, called "Spliff" (popular in Europe), tobacco mixed with hash in a chillum (India), or cannabis rolled in tobacco leaves (Blunt), which would expose the user to the additional risks of tobacco.
Cancer risk
Cannabis smoke contains numerous carcinogens.[85][86][87] In 2008 a study was released by the Medical Research Institute of New Zealand which showed that smoking cannabis increased the risk of lung cancer by 5.7 times over non-smokers.[88] The 79 person study noted that "In the near future we may see an 'epidemic' of lung cancers connected with this new carcinogen. And the future risk probably applies to many other countries, where increasing use of cannabis among young adults and adolescents is becoming a major public health problem."
A previous study published in 2006 by Donald Tashkin of the University of California, Los Angeles had concluded there is no link between smoking cannabis and lung cancer.[89]
A study published in 2006 on a large population sample (1,200 people with lung, neck, or head cancer, and a matching group of 1,040 without cancer) failed to positively correlate a lung cancer risk. The results indicated a slight negative correlation between long and short-term cannabis use and cancer, suggesting a possible therapeutic effect. Cellular studies and even some studies in animal models suggest that THC has antitumor properties, either by encouraging programmed cell death of genetically damaged cells that can become cancerous, or by restricting the development of the blood supply that feeds tumors.[90]
Prior, a 1997 study examining the records of 64,855 Kaiser patients (14,033 of whom identified themselves as current smokers), also found no positive correlation between cannabis use and cancer.[91]
A Research Triangle Institute study concluded that THC, a dilative agent, may help cleanse the lungs by dilating the bronchi, and could actively reduce the instance of tumors.[92] Additionally, a study by Rosenblatt et al. found no association between marijuana use and the development of head and neck squamous cell carcinoma.[93] However, a contrasting 2000 study linked the smoking of cannabis to the growth of cancerous tumors through the impairment of anti-tumor defenses.[94]
UCLA study
On 23 May 2006, Donald Tashkin, M.D., Professor of Medicine at the David Geffen School of Medicine at UCLA in Los Angeles announced that the use of cannabis does not appear to increase the risk of developing lung cancer, or increase the risk of head and neck cancers, such as cancer of the tongue, mouth, throat, or esophagus.[95]The study involved 2252 participants, with some of the most chronic marijuana smokers having smoked over 22,000 marijuana cigarettes.[95][96][97][98] The finding of Donald Tashkin, M.D., and his team of researchers in 2006 refines their earlier studies published in a Dec. 17th 2000 edition of the peer-reviewed journal Cancer Epidemiology Biomarker and Prevention. [19] Many opponents of marijuana incorrectly cite the original finding of UCLA Medical Center from 2000 as "proof" that marijuana leaves the users at higher risk for cancer of the lung, and cancerous tumors,[94] even though the researchers at the UCLA Medical Center have revised their finding with a more in-depth study on the effects of the use of marijuana. This seemed to contradict assumptions made after some studies, like those from Dale Geirringer et al., which found that 118 carcinogens were produced when marijuana underwent combustion, and two carcinogens {2-Methyl-2, 4(2H-1-benzopyran-5-ol) & 5-[Acetyl benz[e]azulene-3,8-dione} formed when marijuana underwent vaporization with the Volcano Vaporizer.[99] To help explain this seemingly chemical proof of carcinogenity inherent in the process of combustion, Tashkin noted that "one possible explanation for the new findings, he said, is that THC, a chemical in marijuana smoke, may encourage aging cells to die earlier and therefore be less likely to undergo cancerous transformation."[95]
Attempts at reducing harm
The health consequences of cannabis use may vary depending on method of use. Proposed alternatives include:
- filtered cigarettes +(see below)
- vaporizers (devices for inhaling THC without burning the cannabis; top temperature 210°C (410°F) compared to 815°C (1500°F) in a burning cigarette)
- one-hitters or mini-toke utensils (narrow-diameter screened crater; suck slow for minimum burning temperature; minimizes THC loss; minimizes carbon monoxide dosage; eliminates side-stream smoke). Researchers have not published data about burning temperature compared to cigarettes.
- eating Cannabis brownies or other foods containing cannabutter or budder
- bongs (specialized pipes filtering, and often cooling, smoke through water) +(see below)
- high potency cannabis
- THC extracts, hashish or honey oil
Like tobacco smoke, cannabis smoke contains tars which are rich in carcinogenic polycyclic aromatic hydrocarbons, which are a prime culprit in smoking-related cancers. However, cannabinoids themselves are not carcinogenic. An obvious way to protect smokers' health is therefore to minimize the content of smoke tars relative to cannabinoids.
The most obvious way to do this is to bypass smoking completely by simply eating the cannabis by extracting the THC and other cannabinoids to a fat (like butter) or alcoholic drink, such as Green Dragon, or by vaporization.
Another way is to increase the THC potency of the cannabis (see also section on potency above). This can be done with hashish, honey oil, or high-quality cannabis. Assuming smokers adjust their smoke intake to the cannabinoid dosage; the higher the concentration of cannabinoids, the lower the amount of tars—- and carbon monoxide—- they are likely to consume to achieve their desired effect.
Vaporisers, by heating the cannabis active constituents and aromatic substances to be inhaled without combustion of the preparation, almost exclude the risk altogether.[100] A 2000 study conducted by NORML and MAPS found that the two tested vaporizers delivered significantly fewer carcinogens than a cigarette.
Cannabis and driving
There are several main obstacles to determining the effect of cannabis use on driving: Cannabis use is most common in a demographic that is already vulnerable for traffic accidents; dangerous drivers who tested positive for THC often test positive for alcohol as well[citation needed]; there are no figures or estimates available as a "base-line," for instance, how many cannabis users drive safely without incidents; and there are many ethical and legal obstacles impeding research on this topic.
A 2001 study by the United Kingdom Transit Research Laboratory (TRL) specifically focuses on the effects of cannabis use on driving,[101] and is one of the most recent and commonly quoted studies on the subject. The report summarizes current knowledge about the effects of cannabis on driving and accident risk based on a review of available literature published since 1994 and the effects of cannabis on laboratory based tasks.
The study identified young males, amongst whom cannabis consumption is frequent and increasing, and in whom alcohol consumption is also common, as an a priori risk group for traffic accidents. This is due to driving inexperience and factors associated with youth relating to risk taking, delinquency and motivation. These demographic and psychosocial variables may relate to both drug use and accident risk, thereby presenting an artificial relationship between use of drugs and accident involvement.
The effects of cannabis on laboratory-based tasks show clear impairment with respect to tracking ability, attention, and other tasks depending on the dose administered. These effects however, are not as pronounced on real world tasks, like driving or simulator tasks. Both simulation and road trials generally find that driving behavior shortly after consumption of larger doses of cannabis results in:
- increased variability in lane position (such as taking a curve too tightly or too loosely).
- longer decision times, leading to slower responses to driving situations; and
- a more cautious driving style, including slower average speed and greater following distance.
Whereas these results indicate a 'change' from normal conditions, they do not necessarily reflect 'impairment' in terms of performance effectiveness, since few studies report increased accident risk. However, the results do suggest 'impairment' in terms of performance efficiency given that some of these behaviors may limit the available resources to cope with any additional, unexpected or high demand, events. Indeed, compensatory effort may be invoked to offset impairment in the driving task. Subjects under cannabis treatment may perceive that they are impaired and may strategically compensate, for example, by not overtaking, by slowing down and by focusing their attention when they know a response will be required. This compensatory effort may be one reason for the failure to implicate cannabis consumption as an accident risk factor, particularly at lower doses or with more than about one hour after consumption. According to the TRL study, the same compensatory behavior could also be an unconscious adaptation, similar to reduced driving speeds used by a sleepy driver.
Specifically, 4-12% of accident fatalities have detected levels of cannabis.[citation needed] However, most studies report that the majority of fatal cases with detected levels of cannabis are compounded by alcohol.
The study estimates 11 ng/ml THC as the equivalent dose to the legal limit of alcohol (0.08% BAC in the UK). Complicating this assessment is the fact that cannabis effects on driving fade after a short period of time, while some THC may be present in the body for weeks.
Similar conclusions have been reached by studies maintained by the federal governments of Australia, United Kingdom, New Zealand and the United States (see here for a list of studies). Those studies that have concluded that cannabis has a significant negative effect on driving ability generally involve the use of roadside sobriety tests as an indicator of reduced ability (for example, see this NIDA report). However, studies that employ this methodology show that a majority of subjects who tested positive for THC also tested positive for alcohol, already described as a limiting factor of validity.
Pathogens and microtoxins
Most microorganisms found in cannabis only affect plants and not humans, but some, especially those that proliferate after the plant is harvested, especially when not correctly dried and stored, can be harmful to humans.[102]
Fungi
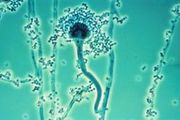
The fungi Aspergillus flavus,[103] Aspergillus fumigatus,[103] Aspergillus niger,[103] Aspergillus parasiticus, Aspergillus tamarii, Aspergillus sulphureus, Aspergillus repens, Mucor hiemalis (not a human pathogen), Penicillin chrysogenum, Penicillin italicum and Rhizopus nigrans have been found in moldy cannabis.[102] Aspergillus mold species can infect the lungs via smoking or handling of infected cannabis and cause opportunistic and sometimes deadly Aspergillosis. Some of the microorganisms found create aflatoxins, which are toxic and carcinogenic. Researchers suggest that moldy cannabis thus be discarded.
Mold may also not be readily apparent. It is also found in smoke from mold infected cannabis,[103][102] and the lungs and nasal passages are a major means of contracting fungal infections. "Levitz and Diamond (1991) suggested baking marijuana in home ovens at 150 °C [302 °F], for five minutes before smoking. Oven treatment killed conidia of A. fumigatus, A. flavus and A. niger, and did not degrade the active component of marijuana, tetrahydrocannabinol (THC)."[102]
Bacteria
Cannabis contaminated with Salmonella muenchen was positively correlated with dozens of cases of salmonellosis in 1981.[104] "Thermophilic actinomycetes" were also found in cannabis.[103]
See also
- Drug abuse
- Drug addiction
- Drug rehabilitation
- Harm reduction
- Medical cannabis
- Psychoactive drug
- Responsible drug use
- Tradable smoking pollution permits
External links
- How marijuana works from HowStuffWorks
- Microbiological contaminants of marijuana
- Cannabis Use and Psychosis from National Drug and Alcohol Research Centre, Australia
- The key research on cannabis use and mental illness at BBC News
- Provision of Marijuana and Other Compounds For Scientific Research recommendations of The National Institute on Drug Abuse National Advisory Council
- Scientific American Magazine (December 2004 Issue) The Brain's Own Marijuana
- Ramström, J. (2003), Adverse Health Consequences of Cannabis Use, A Survey of Scientific Studies Published up to and including the Autumn of 2003, National institute of public health, Sweden, Stockholm.
- Hall, W., Solowij, N., Lemon, J., The Health and Psychological Consequences of Cannabis Use. Canberra: Australian Government Publishing Service; 1994.
- Deaths from Marijuana v. 17 FDA-Approved Drugs
- Benefits and risks of marijuana use in treating various diseases & conditions Analysis includes AIDS, Alzheimer's, Crohn's, glaucoma, depression, arthritis, etc.
- World Health Organisation, PROGRAMME ON SUBSTANCE ABUSE, Cannabis: a health perspective and research agenda;1997.
- ProCon's Marijuana Health Facts
- Bibliography of scholarly histories on cannabis and hashish. (Updated to include article abstracts.)
- Marijuana and Immunity
- The National Cannabis Prevention and Information Centre (Australia)
References
- ↑ Drug Overdose - there has never been a death recorded from the use of marijuana by natural causes.
- ↑ 2.0 2.1 2.2 2.3 H.K. Kalant & W.H.E. Roschlau (1998). Principles of Medical Pharmacology (6th edition ed.). pp. 373–375.
- ↑ Turner C, Bouwsma O, Billets S, Elsohly M (1980). "Constituents of Cannabis sativa L. XVIII--Electron voltage selected ion monitoring study of cannabinoids". Biomed. Mass Spectrom. 7 (6): 247–56. doi:10.1002/bms.1200070605. PMID 7426688.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 J.E. Joy, S. J. Watson, Jr., and J.A. Benson, Jr, (1999). Marijuana and Medicine: Assessing The Science Base. Washington D.C: National Academy of Sciences Press.
- ↑ 5.0 5.1 H. Abadinsky (2004). Drugs: An Introduction (5th edition ed.). pp. 62–77, 160–166.
- ↑ "Erowid Cannabis (Marijuana) Vault". Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - ↑ Fant R, Heishman S, Bunker E, Pickworth W (1998). "Acute and residual effects of marijuana in humans". Pharmacol. Biochem. Behav. 60 (4): 777–84. doi:10.1016/S0091-3057(97)00386-9. PMID 9700958.
- ↑ Tj. T. Mensinga; et al., A double-blind, randomized, placebo-controlled, cross-over study on the pharmacokinetics and effects of cannabis (PDF), RIVM, retrieved 2007-09-21
- ↑ Curran H.V.; et al. (2002). "Cognitive and subjective dose-response effects". National Center for Biotechnology Information. Retrieved 2007-09-21.
- ↑ "Heavy pot smoking could raise risk of heart attack, stroke". CBC.
- ↑ Pertwee R (1997). "Pharmacology of cannabinoid CB1 and CB2 receptors". Pharmacol. Ther. 74 (2): 129–80. doi:10.1016/S0163-7258(97)82001-3. PMID 9336020.
- ↑ Eubanks L, Rogers C, Beuscher A, Koob G, Olson A, Dickerson T, Janda K (2006). "A molecular link between the active component of marijuana and Alzheimer's disease pathology". Mol. Pharm. 3 (6): 773–7. doi:10.1021/mp060066m. PMID 17140265.
- ↑ Newswise: Long-Term Cannabis Users May Have Structural Brain Abnormalities
- ↑ Marijuana and Sex: A Classic Combination
- ↑ W. Hall, N. Solowij (November 1998). "Adverse Effects of Cannabis". The Lancet. 352: 1611–6.
- ↑ H. Schuel; et al. (September 2002). "Evidence that anandamide-signaling regulates human sperm functions required for fertilization". Molecular Reproduction and Development. 63 (3): 376–387. doi:10.1002/mrd.90021.
- ↑ S.J. Astley, S.K. Clarren, R.E. Little, P.D. Sampson, J.R. Daling (January 1992). "Analysis of facial shape in children gestationally exposed to marijuana, alcohol, and/or cocaine". Pediatrics. 89 (1): 67–77.
- ↑ R. Berkow MD; et al. (1997). The Merck Manual of Medical Information (Home Edition). p. 449.
- ↑ J.S. Hayes, R. Lampart, M.C. Dreher, L. Morgan (September 1991). "Five-year follow-up of rural Jamaican children whose mothers used marijuana during pregnancy". West Indian Medical Journal. 40 (3): 120–3.
- ↑ M.C. Dreher, K. Nugent, R. Hudgins (February 1994). "Prenatal Marijuana Exposure and Neonatal Outcomes in Jamaica: An Ethnographic Study". Pediatrics. 93 (3): 254–260.
- ↑ Huizink, A.C. and Mulder, E.J. (2006) Maternal smoking, drinking or cannabis use during pregnancy and neurobehavioral and cognitive functioning in human offspring. Neurosci. Biobehav. Rev. 30, 24–41
- ↑ Fried, P.A. et al. (2003) Differential effects on cognitive functioning in 13- to 16-year-olds prenatally exposed to cigarettes and marihuana.Neurotoxicol. Teratol. 25, 427–436
- ↑ Hardwiring the Brain: Endocannabinoids Shape Neuronal Connectivity Science, May 25, 2007
- ↑ Paul Berghuis,...:Endocannabinoids regulate interneuron migration and morphogenesis... 2007
- ↑ Harkany et al: The emerging functions of endocannabinoid signaling during CNS development
- ↑ JR Minkel: Marijuana-Like Chemicals Guide Fetal Brain Cells, Scientific American, May24, 2007
- ↑ J.S. Hayes, R. Lampart, M.C. Dreher, L. Morgan (1991). "Five-year follow-up of rural Jamaican children whose mothers used marijuana during pregnancy". West Indian Medical Journal. 40 (3): 120–3.
- ↑ Dreher, M. C., Nugent, K., Hudgins, R. 1994. Prenatal marijuana exposure and neonatal outcomes in Jamaica: an ethnographic study. Pediatrics 93(2): 254-260. Retrieved on 5 Mar 2007
- ↑ [http://www.druglibrary.org/Schaffer/hemp/medical/can-babies.htm Prenatal Marijuana Exposure and Neonatal Outcomes in Jamaica: An Ethnographic Study, February, 1994]
- ↑ Judge Young - Part 4
- ↑ 1996. The Merck Index, 12th ed., Merck & Co., Rahway, New Jersey
- ↑ Erowid. "Cannabis Chemistry". Retrieved 2006-03-20.
- ↑ "UK government report" (PDF). House of Commons Science and Technology Committee. 2006-07-18. Retrieved 2006-08-29. Check date values in:
|date=(help)] - ↑ Moir D, Rickert WS, Levasseur G, Larose Y, Maertens R, White P, Desjardins S. (2007). "A comparison of mainstream and sidestream marijuana and tobacco cigarette smoke produced under two machine smoking conditions". Chem. Res. Toxicol.: 494. doi:10.1021/tx700275p. PMID 18062674.
- ↑ Soapbar - Just Say No to polluted hash
- ↑ Flin Flon Mine Area Marijuana Contamination
- ↑ [1]
- ↑ Zhang, Z.-F., Morgenstern, H., Spitz, M. R., Tashkin, D. P., Yu, G.-P., Marshall, J. R., Hsu, T. C., and Schantz, S. P. 1999. [2]
- ↑ Public opinion on drugs and drug policy. Transform Drug Policy Foundation: Fact Research Guide. "Data is notoriously easy to cherry pick or spin to support a particular agenda or position. Often the raw data will conceal all sorts of interesting facts that the headlines have missed." Transform Drug Policy Foundation, Easton Business Centre, Felix Rd., Bristol, UK. Retrieved on 24 March 2007.
- ↑ Synergistic cytotoxicity of Delta(9)-tetrahydrocannabinol and butylated hydroxyanisole {{http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=12119125&dopt=Abstract
- ↑ "MARIJUANA WITHDRAWAL AS BAD AS WITHDRAWAL FROM CIGARETTES" (Press release). Johns Hopkins Medicine. January 24, 2008.
- ↑ Withdrawal Symptoms From Smoking Pot? [3]
- ↑ "Combination of Cognitive-Behavioral Therapy and Motivational Incentives Enhance Treatment for Marijuana Addiction" (Press release). National Institutes of Health. April 1, 2006.
- ↑ 1998 INSERM-CNRS report, directed by Pr. Bernard Roques and commissioned by Health Secretary of State Bernard Kouchner [4] [5] [6] [7]
- ↑ Henquet, C., Krabbendam, L., Spauwen, J., Kaplan, C., Lieb, R., Wittchen, H.-U., and van Os, J. 2005. Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people. BMJ 330(7481): 11. Retrieved on 4 Mar 2007
- ↑ Patton, G. C., Coffey, C., Carlin, J. B., Degenhardt, L., Lynskey, M., and Hall, W. 2002. Cannabis use and mental health in young people: cohort study. BMJ 325(7374): 1195-1198. Retrieved 45 Mar 2007
- ↑ Fergusson, David M.; Horwood, John L.; Ridder, Elizabeth M. "Research Report: Tests of causal linkages between cannabis use and psychotic symptoms. University of Otago Christchurch School of Medicine published in the Society for the Study of Addiction (2004-11-05). Retrieved on 2007-11-03.
- ↑ Hall, Wayne; Degenhardt, Lousia; Teesson, Maree. "Cannabis use and psychotic disorders: an update". Office of Public Policy and Ethics, Institute for Molecular Bioscience University of Queensland Australia, and National Drug and Alcohol Research Centre University of New South Wales Australia published in Drug and Alcohol Review (December 2004). Vol 23 Issue 4. Pg 433-443
- ↑ Arseneault, Louise; Cannon, Mary; Wiitton, John; Murray, Robin M. "Causal association between cannabis and psychosis:Causal association between cannabis and psychosis: examination of the evidence". Institute of Psychiatry published in British Journal of Psychiatry (2004). #184, Pg. 110-117
- ↑ Earth Erowid (2005). "Cannabis & Psychosis - A guide to current research about cannabis and mental health".
- ↑ Robert E. Drake M.D.,Ph.D. and Michael A. Wallach Ph.D. Substance Abuse Among the Chronic Mentally Ill
- ↑ "Cannabis 'raises psychosis risk'". BBC News (2007-07-27). Retrieved on 2007-11-03.
- ↑ 53.0 53.1 'Cheers', U.K study of alcohol and its role in mental health[8]
- ↑ eMedicine - Alcohol-Related Psychosis : Article by Michael Larson
- ↑ N.Q. Brill, R.L. Christie (1974). "Marihuana and Psychosocial Adjustment". Archives of General Psychiatry. 31: 713–719.
- ↑ H.H. Mendelson, J.C. Kuehnle, I. Greenberg; N.K. Mello (1976). "The Effects of Marihuana Use on Human Operant Behavior: Individual Data…". Pharmacology of Marihuana. 2. New York: Academic Press. pp. 643–653.
- ↑ T.F. Denson, M. Earleywine (June 20, 2005). "Decreased depression in marijuana users". Addictive Behaviors.
- ↑ Maria Ellgren, Sabrina M Spano & Yasmin L Hurd (July 5, 2006). "Adolescent Cannabis Exposure Alters Opiate Intake and Opioid Limbic Neuronal Populations in Adult Rats". Neuropsychopharmacology. advance online.
- ↑ Michael Hopkin (July 5, 2006). "Rats taking cannabis get taste for heroin". Nature.
- ↑ Marijuana Use Per Se Not a 'Gateway' To Illicit Drug Use, Study Says - NORML
- ↑ Predictors of Marijuana Use in Adolescents Before and After Licit Drug Use: Examination of the Gateway Hypothesis - Tarter et al. 163 (12): 2134 - Am J Psychiatry
- ↑ RAND | News Release | RAND Study Casts Doubt on Claims That Marijuana Acts as "Gateway" to the Use of Cocaine and Heroin
- ↑ Cécile Henquet, Lydia Krabbendam, Janneke Spauwen, Charles Kaplan, Roselind Lieb, Hans-Ulrich Wittchen and Jim van Os (December 2004). "Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people". British Medical Journal. 330 (11).
- ↑ T.F. Denson, M. Earleywine (June 20, 2005). "Decreased depression in marijuana users". Addictive Behaviors.
- ↑ L. Arseneault; et al. (2004). "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry. 184: 110–117.
- ↑ S. Andreasson; et al. (1987). "Cannabis and Schizophrenia: A Longitudinal Study of Swedish Conscripts". The Lancet. 2: 1483–1486.
- ↑ J. Schiffman; et al. (30 March 2005). "Symptoms of schizotypy precede cannabis use". Psychiatry Research. 134 (1): 37–42. doi:10.1016/j.psychres.2005.01.004.
- ↑ Boydell J, et al. Schizophrenia Research 2007 Apr 24 [9]
- ↑ Louise Arseneault, Mary Cannon, Richie Poulton, Robin Murray, Avshalom Caspi, Terrie E Moffitt (23 November 2002). "Cannabis use in adolescence and risk for adult psychosis: longitudinal prospective study" (PDF). British Medical Journal.
- ↑ Avshalom Caspi, Terrie E. Moffitt, Mary Cannon, Joseph McClay, Robin Murray, HonaLee Harrington, Alan Taylor, Louise Arseneault, Ben Williams, Antony Braithwaite, Richie Poulton, and Ian W. Craig (18 January 2005). "Moderation of the Effect of Adolescent-Onset Cannabis Use on Adult Psychosis by a Functional Polymorphism in the catechol-O-Methyltransferase Gene: Longitudinal Evidence of a Gene X Environment Interaction" (PDF). Society of Biological Psychiatry.
- ↑ Cerebrospinal anandamide levels are elevated in acute schizophrenia and are inversely correlated with psychotic symptoms, Giuffrida A, Leweke FM, Gerth CW, Schreiber D, Koethe D, Faulhaber J, Klosterkotter J, Piomelli D, Department of Pharmacology, University of California, Irvine, CA, USA PubMed, New Scientist
- ↑ Degenhardt L, Hall W, Lynskey M ,Comorbidity between cannabis use and psychosis: Modelling some possible relationships. Technical Report No. 121. Sydney: National Drug and Alcohol Research Centre. 2001, [10] Retrieved on 19.18.2006
- ↑ Ad Hoc Group of Experts. "Report to the Director, National Institutes of Health" (Workshop on the Medical Utility of Marijauana). Institute of Medicine.
- ↑ 74.0 74.1 Bonsor, Kevin. "How Marijauan Works: Other Physiological Effects". HowStuffWorks. Retrieved on 2007-11-03
- ↑ HV, Brignell C, Fletcher S, Middleton P, Henry J. Cognitive and subjective dose-response effects...
- ↑ [11] Neuroprotection by 9-Tetrahydrocannabinol, the Main Active Compound in Marijuana, against Ouabain-Induced In Vivo Excitotoxicity, M. van der Stelt, W. B. Veldhuis, P. R. Bär, G. A. Veldink1, J. F. G. Vliegenthart, and K. Nicolay, The Journal of Neuroscience, September 1, 2001
- ↑ INSERM-CNRS. Released June 1998. Excerpts from the Roques report. Hemp Info. Retrieved 5 Mar 2007
- ↑ Rapport Roques sur la dangerosité des drogues. (in French). Retrieved on 5 Mar 2007
- ↑ L'alcool aussi dangereux que l'héroïne. (in French) Retrieved on 5 Mar 2007
- ↑ Hippocampal Neurotoxicity of Delta 9-Tetrahydrocannabinol - Chan et al. 18 (14): 5322 - Journal of Neuroscience
- ↑ Lyle E. Craker, Ph. D. v. U.S. Drug Enforcement Administration, Docket No. 05-16, May 8 2006, 8-27 PDF
- ↑ M.D. Roth; et al. (March 1998). "Airway Inflammation in Young Marijuana and Tobacco Smokers". American Journal of Respiratory and Critical Care Medicine. 157 (3): 928–937.
- ↑ http://www.lunguk.org/downloads/A_Smoking_Gun.pdf
- ↑ D.P. Tashkin; et al. (January 1997). "Heavy habitual marijuana smoking does not cause an accelerated decline in FEV1 with age". Am. J. Respir. Crit. Care Med. 155 (1): 141–148.
- ↑ Hashibe M, Straif K, Tashkin D, Morgenstern H, Greenland S, Zhang Z (2005). "Epidemiologic review of marijuana use and cancer risk". Alcohol. 35 (3): 265–75. doi:10.1016/j.alcohol.2005.04.008. PMID 16054989.
- ↑ Novotny M, Lee M, Bartle K (1976). "A possible chemical basis for the higher mutagenicity of marijuana smoke as compared to tobacco smoke". Experientia. 32 (3): 280–2. doi:10.1007/BF01940790. PMID 1253890.
- ↑ http://www.norml.org/pdf_files/NORML_Cannabis_Smoke_Cancer.pdf
- ↑ Cannabis bigger cancer risk than cigarettes: study | Health | Reuters
- ↑ "Study Finds No Cancer-Marijuana Connection". Washington Post. 05-26-2006. Retrieved 2007-02-23. Check date values in:
|date=(help); External link in|publisher=(help) - ↑ WebMD (23 May 2006). "Pot Smoking Not Linked to Lung Cancer". ScienceNOW, Abstract
- ↑ S. Sidney (September 1997). "Marijuana use and cancer incidence (California, United States)". Cancer Causes and Control. 8 (5): 722–728. doi:10.1023/A:1018427320658.
- ↑ J. Huff & P. Chan (October 2000). "Antitumor Effects of THC". Environmental Health Perspectives. 108 (10): A442–3. doi:10.2307/3435034.
- ↑ K.A. Rosenblatt; et al. (1 June 2004). "Marijuana Use and Risk of Oral Squamous Cell Carcinoma". Cancer Research. 64: 4049–4054. doi:10.1158/0008-5472.CAN-03-3425.
- ↑ 94.0 94.1 Dr. Steven M. Dubinett (2006-07). "Study Finds Marijuana Ingredient Promotes Tumor Growth, Impairs Anti-Tumor Defenses". Unknown parameter
|org=ignored (help); Check date values in:|date=(help) - ↑ 95.0 95.1 95.2 "Study Finds No Link Between Marijuana Use And Lung Cancer". 26 May 2006. Unknown parameter
|org=ignored (help); Check date values in:|date=(help) - ↑ Fred Gardner (2006-07-06). "Marijuana Smoking Does Not Cause Lung Cancer". Unknown parameter
|org=ignored (help); Check date values in:|date=(help) - ↑ Tashkin, D. P., Simmons, M. S., Sherrill, D. L., and Coulson, A. H. 1997. Heavy habitual marijuana smoking does not cause an accelerated decline in FEV1 with age. American Journal of Respiratory and Critical Care Medicine 155(1): 141-148. Retrieved on 5 Mar 2007
- ↑ "Study finds no marijuana-lung cancer link". Washington Post. 2006-05-26. Retrieved 2006-07-13. Check date values in:
|date=(help) - ↑ Cannabis Vaporizer Combines Efficient Deliver of THC with Effective Suppression of Pyrolytic Compounds {{http://www.ncbi.nlm.nih.gov/sites/entrez?cmd=Retrieve&db=PubMed&list_uids=12119125&dopt=Abstract
- ↑ B. Mirken (17 Sep 1999). "Vaporizers for Medical Marijuana". AIDS Treatment News. 327.
- ↑ United Kingdom Department for Transport (4 Nov 2004). "Cannabis and driving: a review of the literature and commentary (No.12)". Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Unknown parameter|accessmonthday=ignored (help) - ↑ 102.0 102.1 102.2 102.3 Microbiological contaminants of marijuana
- ↑ 103.0 103.1 103.2 103.3 103.4 "Marijuana smoking and fungal sensitization. [J Allergy Clin Immunol. 1983] - PubMed Result". www.ncbi.nlm.nih.gov. Retrieved 2008-03-20.
- ↑ lib.bioinfo.pl
Template:WH Template:WS it:Effetti della cannabis sulla salute he:השפעות פיזיולוגיות של קנאביס sr:Деловање конопље
- Pages with reference errors
- Pages using duplicate arguments in template calls
- CS1 maint: Extra text
- CS1 maint: Multiple names: authors list
- Pages with citations using unsupported parameters
- CS1 maint: Explicit use of et al.
- CS1 errors: dates
- CS1 errors: external links
- Pages with broken file links
- All articles with unsourced statements
- Articles with unsourced statements from May 2008
- Articles with invalid date parameter in template
- Self-contradictory articles
- All self-contradictory articles
- Wikipedia articles needing clarification from February 2008
- All Wikipedia articles needing clarification
- Articles with unsourced statements from December 2007
- Articles with unsourced statements from February 2008
- Articles with unsourced statements from November 2007
- Articles with unsourced statements from January 2008
- Cannabis
- Medicinal use of cannabis