Tetrahydrocannabinol
 | |
 | |
| Clinical data | |
|---|---|
| ATC code | |
| Pharmacokinetic data | |
| Elimination half-life | 4.3-12.6 days[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C21H30O2 |
| Molar mass | 314.45 |
| Boiling point | 200 °C (392 °F) 0.02mmHg |
| Solubility in water | 2.8 mg/L (23 °C) mg/mL (20 °C) |
Overview

Template:FixHTML Tetrahydrocannabinol, also known as THC, Δ9-THC, Δ9-tetrahydrocannabinol (delta-9-tetrahydrocannabinol), Δ1-tetrahydrocannabinol (using an older numbering scheme), or dronabinol, is the main psychoactive substance found in the Cannabis plant. It was isolated by Raphael Mechoulam, Yechiel Gaoni, and Habib Edery from the Weizmann Institute in Rehovot, Israel in 1964. In pure form, it is a glassy solid when cold, and becomes viscous and sticky if warmed. An aromatic terpenoid, THC has a very low solubility in water, but good solubility in most organic solvents such as butane or hexane. As is the case with nicotine and caffeine, the role of THC in Cannabis, it seems, is to protect the plant from herbivores or pathogens. [2] THC also possesses high UV-B (280-315 nm) absorption properties, protecting the plant from harmful radiation.
Pharmacology
The pharmacological actions of THC result from its binding to the cannabinoid receptor CB1, located in the brain. The presence of these specialized receptors in the brain implied to researchers that endogenous cannabinoids are manufactured by the body, so the search began for a substance normally manufactured in the brain that binds to these receptors, the so-called natural ligand or agonist, leading to the eventual discovery of anandamide, 2-arachidonyl glyceride (2-AG), and other related compounds. This story resembles the discovery of the endogenous opiates (endorphins, enkephalins, and dynorphin), after the realization that morphine and other opiates bind to specific receptors in the brain. In addition, it has been shown that cannabinoids, through a presently-unknown mechanism, activate endogenous opioid pathways via the μ1 opioid receptor, precipitating a dopamine release in the nucleus accumbens. The effects of the drug can be suppressed by the CB1 cannabinoid receptor antagonist rimonabant (SR141716A) or, interesting to note, the opioid receptor antagonists (opioid blockers) naloxone and naloxonazine.[3]
The mechanism of endocannabinoid synaptic transmission is understood by the following events: An excitatory transmission of the neurotransmitter glutamate causes an influx of calcium ions into the post-synaptic neuron. Through a mechanism not yet fully understood, the presence of calcium post-synaptically induces the production of endocannabinoids in the post-synaptic neuron. These endocannabinoids (such as anandamide) are released into the synaptic cleft. Once in the synaptic cleft, binding occurs at cannabinoid receptors present in pre-synaptic neurons where they can then modulate neurotransmission pre-synaptically. This form of neurotransmission is termed retrograde transmission, as the signal is carried in the opposite direction of orthodox propagation; it provides an interesting insight into neurotransmission, which previously was thought to be exclusively one way.
THC has analgesic effects that, even at low doses, cause a high, thus leading to the fact that medical cannabis can be used to treat pain. The mechanism for analgesic effects caused directly by THC or other cannabinoid agonists is not fully elucidated. Other effects include relaxation; euphoria; altered space-time perception; alteration of visual, auditory, and olfactory senses; disorientation; fatigue; and appetite stimulation related to CB1 receptor activity in the central nervous system. The mechanism for appetite stimulation in subjects is somewhat understood and explained through a gastro-hypothalamic axis. CB1 activity in the hunger centers in the hypothalamus increases the palatability of food when levels of a hunger hormone, ghrelin, increase as food enters the stomach. After chyme is passed into the duodenum, signaling hormones such as cholecystokinin and leptin are released, causing reduction in gastric emptying and transmission of satiety signals to the hypothalamus, respectively. Cannabinoid activity is reduced through the satiety signals induced by leptin release. It also has anti-emetic properties, and also may reduce aggression in certain subjects.
THC has an active metabolite, 11-Hydroxy-THC, which may also play a role in the analgesic and recreational effects of the herb.
Toxicity
According to the Merck Index, 12th edition, THC has a LD50 value of 1270 mg/kg (male rats) and 730 mg/kg (female rats) administered orally dissolved in sesame oil.[4]
If this were scaled up to an adult human, the LD50 would be between approximately 86 g and 50 g for a 68-kg (150-lb) male or female person, respectively. This would be equivalent to 1-1.8 kg of cannabis with a 5% THC content (roughly average) taken orally. The LD50 value for rats by inhalation of THC is 42 mg/kg of body weight. It is important to note, however, that toxicity in animal models does not necessarily correlate to human toxicity. THC receptor distribution in the rat central nervous system is different from that of humans, meaning that there is the significant possibility that toxicity in humans varies from the published animal LD50 studies. There has never been a documented fatality from marijuana or THC overdose. Absorption is limited by serum lipids, which can become saturated with THC, thus the inherent solubility may mitigate toxicity.
Studies of the distribution of the cannabinoid receptors in the brain explain why THC's toxicity is so low (i.e., the LD50 of the compound is so large): Parts of the brain that control vital functions such as respiration do not have many receptors, so they are relatively unaffected even by doses larger than could ever be ingested under any normal conditions.
Research
A number of studies indicate that THC may provide medical benefits for cancer and AIDS patients by increasing appetite and decreasing nausea. It has been shown to assist some glaucoma patients by reducing pressure within the eye, and is used in the form of cannabis by a number of multiple sclerosis patients to relieve the spasms and pain associated with their condition. New scientific evidence is showing that THC can prevent Alzheimer's Disease by counteracting the activation of microglia and thus inducing the inflammation of microglia binding to amyloid protein.
Some studies also claim a variety of negative effects associated with constant, long-term use, including short-term memory loss. Other studies have refuted this by evidence of MRIs of long term users showing little or no difference to MRIs of the non-using control group. Although using positron emission tomography (PET), at least one study claims to have observed altered memory-related brain function in marijuana users. [5] The long-term effects of THC on humans have been disputed because its status as an illegal drug makes research difficult.
Preliminary research on synthetic THC has been conducted on patients with Tourette syndrome, with results suggesting that it may help in reducing nervous tics and urges by a significant degree. Animal studies suggested that Marinol and nicotine could be used as an effective adjunct to neuroleptic drugs in treating TS. Research on twelve patients showed that Marinol reduced tics with no significant adverse effects. A six-week controlled study on 24 patients showed the patients taking Marinol had a significant reduction in tic severity without serious adverse effects. Seven patients dropped out or had to be excluded from the study, one due to adverse side-effects. More significant reduction in tic severity was reported with longer treatment. No detrimental effects on cognitive functioning and a trend towards improvement in cognitive functioning were reported during and after treatment. Marinol's usefulness as a treatment for TS cannot be determined until/unless longer controlled studies on larger samples are undertaken.[6][7][8]
Recent research has shown that many adverse side-effects, generally known as the "stoner" stereotype, fail to hold up to the scientific method. Recent studies with synthetic cannabinoids show that activation of CB1 receptors can facilitate neurogeneration, as well as neuroprotection, and can even help prevent natural neural degradation from neurodegenerative diseases such as MS, Parkinson's, and Alzheimer's; however, neurogeneration has occurred only in rats due to the introduction of an optical isomer of THC, and not THC itself. This, along with research into the CB2 receptor (throughout the immune system), has given the case for medical marijuana more support.
In in-vitro experiments, THC at extremely high concentrations, which could not be reached with commonly-consumed doses, caused inhibition of plaque formation, the cause of Alzheimer's disease, better than currently-approved drugs.[9]
THC may also be an effective anti-cancer treatment, with studies showing tumor reduction in mice, conducted in 1975.[10]
On July 28, 2007, British medical journal The Lancet published a study that indicates that cannabis users have, on average, a 41% greater risk of developing psychosis than non-users. The risk was most pronounced in cases with an existing risk of psychotic disorder, and was said to grow up to 200% for the most-frequent users.[11][12][13]
Recent research has also shown a correlation between cannabis use and increased cognitive function in schizophrenic patients.[14]
A two-year study in which rats and mice were force-fed tetrahydrocannabinol dissolved in corn oil showed reduced body mass, enhanced survival rates, and decreased tumor incidences in several sites, mainly organs under hormonal control. It also caused testicular atrophy and uterine and ovarian hypoplasia, as well as hyperactivity and convulsions immediately after administration.[15]
In mice low doses of Δ9-THC reduce the progression of atherosclerosis. [16]
Biosynthesis
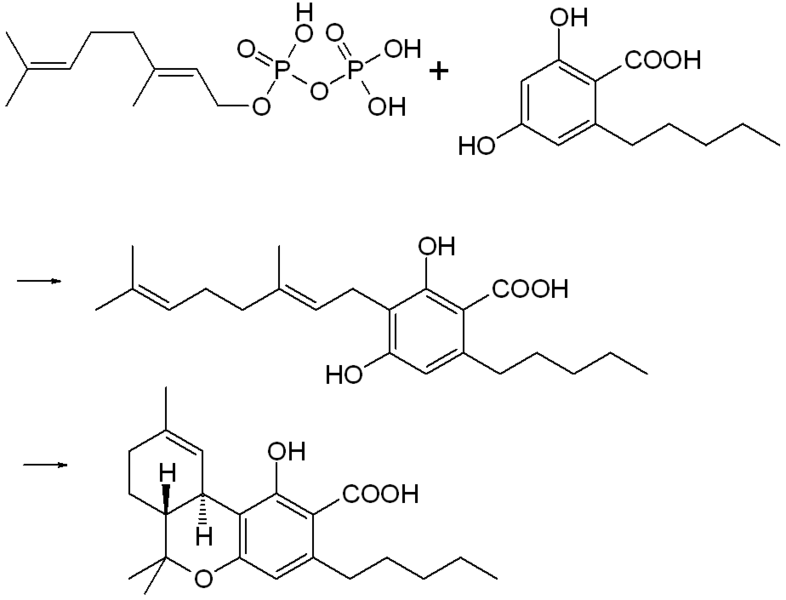
In the cannabis plant THC occurs mainly as tetrahydrocannabinol carboxylic acid (THC-COOH). The enzymatic condensation of geranyl pyrophosphate and olivetolic acid gives cannabigerolic acid which is cyclized by the enzyme THC acid synthase to give THC-COOH. Heating decarboxylates the acid to THC.
Metabolism
THC is mainly metabolized to 11-OH-THC (11-hydroxy-THC) by the human body. This metabolite is still psychoactive and is further oxidized to 11-nor-9-carboxy-THC (THC-COOH). In humans and animals more than 100 metabolites could be identified but 11-OH-THC and THC-COOH are the dominating metabolites. Metabolism mainly occurs in the liver by cytochrome P450 enzymes CYP2C9, CYP2C19, and CYP3A4. More than 55% of THC are excreted in the feces and ~20% in the urine. The main metabolite in urine is the ester of glucuronic acid and THC-COOH and free THC-COOH. In the feces mainly 11-OH-THC was detected.[17]
Synthetic THC
Synthetic THC, also known under the substance name dronabinol, is available as a prescription drug (under the trade name Marinol) in several countries including the U.S. and Germany. In the United States, Marinol is a Schedule III drug, available by prescription, considered to be non-narcotic and to have a low risk of physical or mental dependence. Efforts to get cannabis rescheduled as analogous to Marinol have not succeeded thus far, though a 2002 petition has been accepted by the DEA. As a result of the rescheduling of Marinol from Schedule II to Schedule III, refills are now permitted for this substance. Marinol has been approved by the FDA in the treatment of anorexia in AIDS patients, as well as for refractory nausea and vomiting of patients undergoing chemotherapy.
An analog of dronabinol, nabilone, is available commercially in Canada under the trade name Cesamet, manufactured by Valeant. Cesamet has also received FDA approval for future availability in the United States and is a Schedule II drug.
In April 2005, Canadian authorities approved the marketing of Sativex, a mouth spray for multiple sclerosis to alleviate pain. Sativex contains tetrahydrocannabinol together with cannabidiol. It is marketed in Canada by GW Pharmaceuticals, being the first cannabis-based prescription drug in the world.
See also
- Cannabis (drug)
- Psychoactive drug
- Cannabinoids
- Medical cannabis
- Dronabinol
- War on Drugs
- THC Ministry
- Cannabis rescheduling in the United States
- Cannabidiol, an isomer of THC
- Health issues and the effects of cannabis
References
- ↑ Johansson E, Halldin MM, Agurell S, Hollister LE, Gillespie HK. (1989). "Terminal elimination plasma half-life of delta 1-tetrahydrocannabinol (delta 1-THC) in heavy users of marijuana". European Journal of Clinical Pharmacology. 37 (3): 273–7. PMID 2558889.
|access-date=requires|url=(help) - ↑ http://www.madsci.org/posts/archives/jun2000/961475085.Bt.r.html
- ↑ Carl R Lupica; et al. "Marijuana and cannabinoid regulation of brain reward circuits". Retrieved 2007-07-01.
- ↑ Erowid. "Cannabis Chemistry". Retrieved 2006-03-20.
- ↑ Pharmacology, Biochemistry and Behavior 72 (2002) 237–250. www.elsevier.com/locate/pharmbiochembeh
- ↑ Müller-Vahl,K.R. Schneider,U. Koblenz,A. Jöbges,M. Kolbe,H. Daldrup,T. Emrich,H.M. "Treatment of Tourette's Syndrome with ?9-Tetrahydrocannabinol (THC): A Randomized Crossover Trial". Pharmacopsychiatry. 35 (2): 57–61. PMID 11951146.
- ↑ Müller-Vahl KR, Schneider U, Prevedel H, Theloe K, Kolbe H, Daldrup T, Emrich HM. (April 2003). "Delta 9-tetrahydrocannabinol (THC) is effective in the treatment of tics in Tourette syndrome: a 6-week randomized trial". J Clin Psychiatry. 64 (4): 459–65. PMID 12716250.
- ↑ Muller-Vahl KR, Prevedel H, Theloe K, Kolbe H, Emrich HM, Schneider U. (February 2003). "Treatment of Tourette syndrome with delta-9-tetrahydrocannabinol (delta 9-THC): no influence on neuropsychological performance". Neuropsychopharmacology. 28 (2): 384–388. PMID 12589392.
- ↑ Eubanks LM, Rogers CJ, Beuscher AE; et al. (2006). "A molecular link between the active component of marijuana and Alzheimer's disease pathology". Mol. Pharm. 3 (6): 773–7. doi:10.1021/mp060066m. PMID 17140265.
- ↑ "Anticancer activity of cannabinoids (Journal of the National Cancer Institute, Vol. 55, No. 3, September 1975, pp.597-602)". Retrieved 2007-10-27.
- ↑ "Cannabis could increase risk of psychotic illness later in life by 40 %". The Lancet.
- ↑ "Prospective cohort study of cannabis use, predisposition for psychosis, and psychotic symptoms in young people". BMJ. line feed character in
|title=at position 61 (help) - ↑ "Marijuana may increase psychosis risk". CTV.
- ↑ Coulston CM, Perdices M, Tennant CC. The neuropsychological correlates of cannabis use in schizophrenia: Lifetime abuse/dependence, frequency of use, and recency of use. Schizophrenia Research (2007); 96(1-3):169-184.
- ↑ Chan PC, Sills RC, Braun AG, Haseman JK, Bucher JR (1996). "Toxicity and carcinogenicity of delta 9-tetrahydrocannabinol in Fischer rats and B6C3F1 mice". Fundamental and applied toxicology : official journal of the Society of Toxicology. 30 (1): 109–17. PMID 8812248.
- ↑ Steffens S, Veillard NR, Arnaud C; et al. (2005). "Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice". Nature. 434 (7034): 782–6. doi:10.1038/nature03389. PMID 15815632.
- ↑ Huestis MA (2005). "Pharmacokinetics and metabolism of the plant cannabinoids, Δ9-tetrahydrocannabinol, cannabidiol and cannabinol". Handb Exp Pharmacol (168): 657–90. PMID 16596792.
External links
- Scientific American Marijuana research
- Erowid Compounds found in Cannabis sativa.
- Machinery of the "marijuana munchies"
- Erowid interview An interesting look into a group advocating the intentional, spiritual, and transformative use of cannabis.
Template:Ancient anaesthesia-footer
bs:Tetrahidrokanabinol ca:Tetrahidrocannabinol cs:Tetrahydrocannabinol cy:Tetrahydrocannabinol de:Tetrahydrocannabinol gl:Tetrahidrocannabinol hr:Tetrahidrokanabinol it:Delta-9-Tetraidrocannabinolo he:THC lt:Tetrahidrokanabinolis hu:Tetrahidrokannabinol nl:Tetrahydrocannabinol no:Tetrahydrocannabinol sk:Tetrahydrokanabinol sl:Tetrahidrokanabinol sr:Tetrahidrokanabinol fi:Tetrahydrokannabinoli sv:Tetrahydrocannabinol th:เตตร้าไฮโดรแคนนาบินอล uk:Тетрагідроканнабінол Template:Jb1
- Pages with script errors
- Pages using citations with accessdate and no URL
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- CS1 errors: invisible characters
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Infobox drug articles with non-default infobox title
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Chemical pages without DrugBank identifier
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Drugs with no legal status
- Articles containing unverified chemical infoboxes
- Cannabinoids