Splenic abscess
|
WikiDoc Resources for Splenic abscess |
|
Articles |
|---|
|
Most recent articles on Splenic abscess Most cited articles on Splenic abscess |
|
Media |
|
Powerpoint slides on Splenic abscess |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Splenic abscess at Clinical Trials.gov Trial results on Splenic abscess Clinical Trials on Splenic abscess at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Splenic abscess NICE Guidance on Splenic abscess
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Splenic abscess Discussion groups on Splenic abscess Patient Handouts on Splenic abscess Directions to Hospitals Treating Splenic abscess Risk calculators and risk factors for Splenic abscess
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Splenic abscess |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Venkata Sivakrishna Kumar Pulivarthi M.B.B.S [2]
Synonyms and keywords:Abscess of spleen
To return to abscess main page click here
Overview
Splenic abscess is an uncommon and life-threatening condition. Clinical presentation, etiological factors, natural history, treatment and prognosis depends on whether the abscess was solitary or multiple.[1] It is always fatal if left untreated. Most commonly associated with immunodeficient patients especially and hematological disorders such as leukemia and sickle cell disease. Diagnostic needle aspiration is very important in the management with antibiotics as blood culture may not be the best correlate as abscess culture. Antibiotic of choice depends on the organism but aggressive and early surgical intervention of splenic abscess should be encouraged especially when the risk factors are present. High suspicion of splenic abscess with history of risk factors, broad-spectrum empirical antibiotic therapy should be initiated.[2]
Definition
Splenic abscess is defined as any infectious suppurative process involving identifiable macroscopic filling defects either in the parenchyma of the spleen or in the sub-capsular space.[3]
Historical Perspective
- Since the times of Hippocrates, splenic abscess has been reported several times and he described the natural history and prognosis of splenic abscess.[4]
- In the early days of 20th century, splenic abscess most commonly caused by typhoid and then followed by malaria.[5]
- Ooi et al described significant etiological differences such increase in the percentage of abscess cases due to anaerobics as compared to aerobics (7 vs 18-28%), fungi (1 vs 18-41%) as well as mycobacterium tuberculosis (0.8 vs. 14%) in the second half of 20th century.[6]
Classification
| Classification by Mechanism of pathogenesis | Classification by Etiology | Classification by Pathological Findings |
|---|---|---|
|
Splenic abscess is classified traditionally by Chun and colleagues based on the predisposing causes as follows:[7][1][8]
|
Classification of splenic abscesses based on the etiological factors is as follows:[6] |
Lawhorne and Zuidema classified splenic abscees based on pathological findings as follows:[9]
|
Pathophysiology
Splenic abscess can result from various sources such as:[10]
| Pathogenic Mechanism | Description |
|---|---|
| Hematogenous Dissemination |
|
| Secondary infection of splenic infarction |
|
| Contiguous spread of bacteria |
|
| Trauma or Surgery |
|
| Immunodeficiency |
Gross Findings
Solitary splenic abscess
- Enlarged spleen with due to large solitary abscesses with thick wall around the abscess to prevent dissemination is seen
Multiple splenic abscess
- At the time of autopsy, spleen present as large and soft, and pus extruded organ from the cut surface.
Microscopic Findings
Solitary splenic abscess
- Microscopically the abscess consist of necrotic tissue with a fibrous wall surrounded by inflammatory cell infiltration.
Multiple splenic abscess
- Multiple microscopically visible foci of infection riddled homogeneously throughout the spleen
- Abscesses are filled with polymorphonuclear leukocytes which were scattered throughout the parenchyma, intermixed with other foci of microinfarction and coagulation necrosis
Association
Splenic abscess is commonly associate with:[11]
- Paranchymal liver disease
- Pancreatitis
- Pleural effusion
- Renal cysts
- Ovarian cysts
- Abdominal lymphadenopathy
Causes
Splenic abscess is caused mostly by monomicrobial but some times it can be caused by polymicrobial agents. Bacteria is more common than other microbial agents such as fungi, protozoa which can cause splenic abscess in immunocompromised patients.
Common causes
The most common causative bacteria of the splenic abscess in 50% of the cases is the aerobic bacteria.[3][12]
Other common causes of splenic abscess includes:[3]
| Aerobes | Anaerobes | Fungal | Parasite |
|---|---|---|---|
Less common causes
Differentiating Splenic abscess from Other Diseases
Splenic abscess should be differented from other causes of left upper quadrent pain:[11]
Epidemiology and Demographics
Incidence
Incidence of splenic abscess varies between 0.1% to 0.7% based on population based autopsy studies.[7][13] Incidence of splenic abscess due to hematogenous spread is gradually declining due to increased antibiotic use, but incidence due to fungal infection is increasing due to aggressive chemotherapeutic methods.[14][15]
Prevalence
Prevalence of splenic abscess is increasing gradually due to increased risk factors and increased imaging modalities that can diagnose more accurately.[16]
Case Fatality Rate
Splenic abscesses are associate with increased morbidity and mortality. If left untreated, mortality is definite (100%).[3] Mortality rate also varies with treatment of choice such as splenectomy, percutaneous drainage, anti microbial therapy carries 8%, 29%, 20% of mortality rate respectively.[17]
Age
Splenic abscess shows bimodal distribution in age of the patients, with peak incidence seen in thirties and sixties.[3] First peak of age group is people < 40 years of age who are immunosuppressed or intravenous drug abusers, who commonly present multilocular abscesses. Second peak of age group patients > 70 years with diabetes or nonendocardic septic focus and commonly develop a unilocular abscess.
Gender
Splenic abscess is more predominant in male compared to female (~2 folds).[3][7][18]
Developing Countries
In Africa, splenic abscess is common due to prevalence of hemoglobinopathies such as sickle cell disease, which is a common risk factor for this disease.[19]
Risk Factors
Spleen abscess often co-exists with several risk factors, but the major one is the patient’s immunodeficiency. Common risk factors of splenic abscess include:[11]
| Infectious risk factors | Non infectious risk factors |
|---|---|
|
Screening
No specific screening test for splenic abscess.
Natural History, Complications and Prognosis
Natural History
Splenic abscess is a rare cause of abdominal abscesses, but life-threatening. Because of it's rarity, splenic abscess usually diagnosed at the late stages or after the onset of complications.[1] Solitory abscess present with delayed onset of presentation with history of trauma, sepsis, or adjacent organ disease with fever, abdominal pain, nausea and vomiting where as multiple splenic abscess most commonly present with generalized sepsis because of an ineradicable septic focus remote from the spleen. Early diagnosis, prompt treatment can prevent complications.[1] Mortality rate is very high if left untreated.
Complications
| Life threatening complications | Common complications | Less common complications |
|---|---|---|
|
Prognosis
Prognosis of splenic abscess depends on the time of diagnosis and treatment. Delay in the management can lead to splenic rupture followed by spilling into peritoneal cavity or an adjacent organ which can lead to septicemia and death in severe cases.
Diagnosis
Splenic abscess commonly present with a triad of symptoms include fever, nausea, vomiting and abdominal pain along with palpable spleen on examination. Early diagnosis with imaging studies and prompt drainage is required to reduce morbidity and mortality. Presence of fever, left upper abdominal pain, leukocytosis and radiologic evidence shows pathology in the left chest X-ray especially in immunocompromised patients are the indications for high suspicion of splenic abscess.
History and Symptoms
Common symptoms of splenic abscess include:[3][6]
- Fever
- Abdominal pain localized in the left upper quadrant or mesogastrium
- Nausea and vomiting
- Constitutional symptoms such as fatigue, loss of body weight, sweating and chills
Other symptoms include:[1]
- Referred pain in the left shoulder
- Confusion
- Pain in the left lower hemithorax
- Cough
Physical Examination Findings
Appearance
Patient with splenic abscess appear ill appearing and diaphoretic
Vital signs
If patient present with sepsis:
- Hypotension
- Tachycardia
- Increased capillary refill time
Signs of sepsis indicate that splenic abscess is most likely due to bacterial cause than fungal source.[3]
Heart
- New onset murmur may be present
Lungs
- Left sided pleural effusion may be present with signs of:
- Decreased breath sounds on left side
- Dullness to percussion on left side
- Absent tactile fremitus on left side
- Friction rub over the left chest
Abdomen
Palpation
- Tender splenomegaly
- Palpable spleen or abdominal mass
Auscultation
- Friction rub over the spleen[1]
Laboratory Tests
Blood Tests
Blood tests such leukocytosis are increased but not significant in the diagnosis of splenic abscess because these tests may not be appropriate in immunocompromised patients.
- CBC with differential
- Erythrocyte sedimentation rate (ESR)
- Microbiological tests: In solitary abscesses blood culture is not sensitive in the initial stages when as in multiple abscesses it is helpful in prompt diagnosis and early treatment.[1]
- Gram stain
- Bacterial culture
- Abscess culture
- Mycological tests
- KOH test
- Fungal culture
Diagnostic Evaluation of Splenic abscess
| Suspicion of splenic abscess (Patients with immunodeficiency disorders, fever, changes in chest X-ray, abdominal pain) | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Blood culture | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Patient with immunodeficiency disorders? | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| If immunodeficent patient Initiate wide spectrum antibiotics + antifungal medication | If immunocompetent patient Initiate wide spectrum antibiotics | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Ultrasound of abdominal cavity, CT scan with contrast | If imaging shows negative or equivocal with high clinical suspicion of splenic abscess | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Arteriography | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Presence of indications for minimally invasive procedures | Absence of indications for minimally invasive procedures | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Aspiration or abscess drainage under US or CT guidance | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Abscess cavity content culture, modification of antibiotic therapy according to culture results; Prolonged antibiotic therapy | If ineffective drainage or recurrent abscess | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Spleenectomy or Open abscess drainage | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Abscess cavity content culture, modification of antibiotic therapy according to culture results; Prolonged antibiotic therapy | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Imaging Findings
As the clinical features of splenic abscess are non specific and vague such as abdominal pain, fever and vomiting, that makes diagnosis is challenging and relied on imaging modalities. Imaging studies such as ultrasound, computerized tomography made the diagnosis early and more accurate that reduces morbidity and mortality.[23]
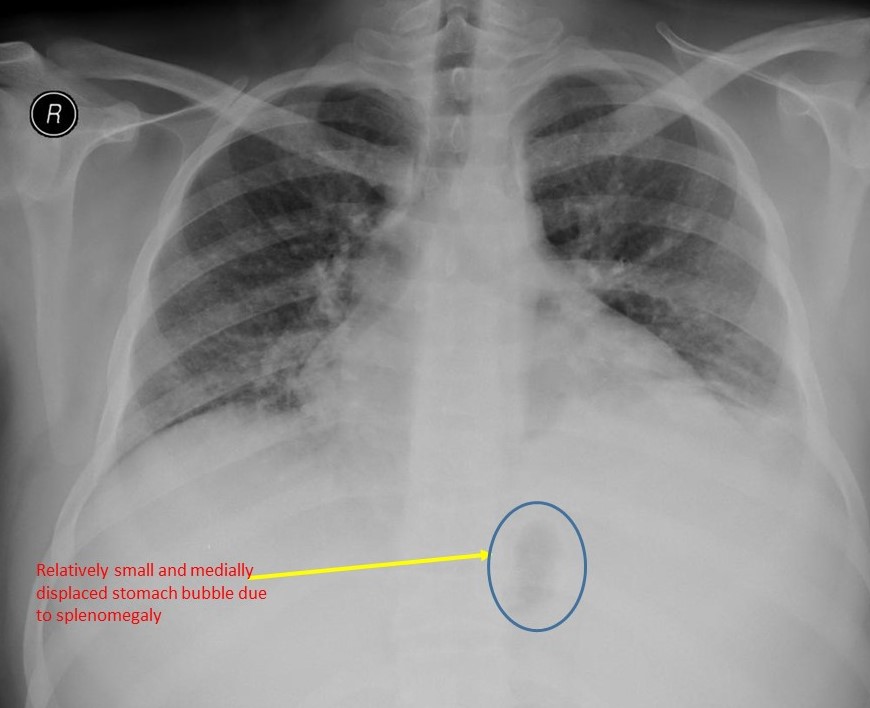
X-ray
Advantages
- High sensitivity
- Directly points to pathological changes
- It is the first line of examination for patients suspected of an ongoing infection
- Can determine phrenic/ diaphragmatic dome positioning and air-fluid level in the left hypochondrium
Common chest x- ray findings includes:
- Elevated and immobile left diaphragm
- Ipsilateral pleural effusion
- Atelectalic and inflammatory changes in interior lung lobe
Common abdominal x- ray findings includes:
- Shift of the stomach and colon by a soft tissue mass (splenic abscess) which is more rectangular than in other causes of splenomegaly
- Increased air-fluid levels with extra alimentary gas collection in the left upper quadrant[2]
Ultrasound
Ultrasound shows lesions of mixed echogenicity i.e anechoic central zone with a surrounding hyperechoic area.[24][25]
Advantages
- Emergency radiography with high sensitivity (75-100%)[8][26]
- Non invasive
- Cost effective
- Determine the size of the spleen, size of the abscess, its location and echogenicity
CT images
Computerised tomography with contrast is both diagnostic and therapeutic test of choice for splenic abscess.[27][28]
Advantages
- High sensitivity (88-100%)
- Can differentiate unolocular and multilocular abscesses
- Can identify the contents of abscess
- Can determine the density index of abscess.
- Can differentiate splenic abscess from splenic cysts and splenic hematomas
- More precise and accurate than ultrasonography, in identifying the location of abscess in relation to other internal organs during percutaneous drainage.
- It is superior to all other diagnostic tests for splenic abscess.
|valign=top| Scintigraphic studies include technetium-99m liver and spleen scans, gallium scans, and indium scans. Splenic scan is diagnostic modality to identify abscesses which relies upon splenic uptake of the radionuclide 99m technetium which shows abscess as a negative or filling defect.
Advantages
- High specificity: If patient showing high suspicion of splenic abscess and scan supports the diagnosis, then splenectomy can be performed.
Disadvantages:
- Scan can not identifie or visualize incurable small abscesses.[1]
- Less sensitive: If the scan shows negative or equivocal results for splenci abscess but clinical suspicion remains, an arteriogram should be ordered.
Other Imaging Studies
Scintigraphic studies
Scintigraphic studies include technetium-99m liver and spleen scans, gallium scans, and indium scans. Splenic scan is diagnostic modality to identify abscesses which relies upon splenic uptake of the radionuclide 99m technetium which shows abscess as a negative or filling defect.
Advantages
- High specificity: If patient showing high suspicion of splenic abscess and scan supports the diagnosis, then splenectomy can be performed.
Disadvantages:
- Scan can not identifie or visualize incurable small abscesses.[1]
- Less sensitive: If the scan shows negative or equivocal results for splenic abscess but clinical suspicion remains, an arteriogram should be ordered.
Arteriography
Arteriography is the technique that involves injection of contrast material through a catheter passed retrograde into the splenic artery followed by rapid exposure of sequential x-ray films which shows abscesses as filling defects in the spleen.
Advantages:
More reliable and precise than splenic scan in diagnosing small abscesses.
Disadvantages:
- Invasive technique
Treatment
Medical Therapy
Antibiotic regimen should start before the procedure and continue until 7 days after the procedure. Diagnostic needle aspiration is very important in the management with antibiotics as blood culture may not be the best correlate as abscess culture. Antibiotic of choice depends on the organism, but aggressive and early surgical intervention of splenic abscess should be encouraged especially when the risk factors are present. High suspicion of splenic abscess with history of risk factors, broad-spectrum empirical antibiotic therapy should be initiated. [2] Empiric antibiotic should cover streptococci, staphylococci, and aerobic gram-negative rods such as vancomycin or oxacillin plus an aminoglycoside, a third- or fourth-generation cephalosporin, fluoroquinolone or carbapenem. If culture shows fungi as causative organism, start Amphotericin B immediately and continue for 6-24 weeks and during the procedure amphotericin B should be administered directly into the abscess.[29]
Surgery
Treatment of splenic abscess depends on etiology. In bacterial abscesses, splenectomy combined with post-operative antibiotic therapy is the most appropriate treatment of choice with least mortality rate when compared to percutaneous drainage or antimicrobial therapy.[17]
Percutaneous Drainage
Percutaneous drainage is the initial tretament of choice for splenic abscess even though splenectomy is the definitive treatment because of increased risk of infections in splenectomised patient.[10][30] It is genereally done under the guidance of imaging studies such as ultrasound or computerised tomography and under the guidence of imaging efficy of percuteneous drainage is equivalent to splenectomy.[31][32]
- First line of treatment for splenic abscess
- Safe and effective than surgery in both unilocular and bilocular abscesses, especially in peripherally located abscesses.
- Preferred in critically ill patient and patients unfit for general anesthesia
Advantages
- Preserves spleen so, it became the treatment of choice in children to prevent post-splenectomy septicemia[33]
- No abdominal spillage of abscess contents
- Less expensive, high acceptance rate and less operative risk
Complications
- Splenic haemorrhage
- Injury to other abdominal organs
- Septicemia
- Empyema
- Pneumothorax
- Fistula formation
- Deep vein thrombosis
Contraindications or limitations
- Multiple or septated abscesses[34][8][12]
- Anatomically inaccessible for drainage such as upper pole or hilar of the spleen,
- Uncontrolled coagulopathies
- Ascites
- Simultaneous surgical procedure required of other indications such as subphrenic abscess
- Abscess perforation or bleeding
- Refractoriness to abscess-content drainage
- Secondary infected spleen hematoma
Splenectomy
Splenectomy is the most effective and definitive treatment of choice for splenic abscess. Splenectomy can be performed either from left subcostal incision or from midline epigastric entry.
Advantages
- Definitive treatment for splenic abscess
- Treatment of choice if more than 2 abscesses are present
- Patients with failed percutaneous drainage
- Patient with recurrent abscesses
Disadvantages
- Splenecetomisesd patients are more prone to infections especially catalase positive bacteria such as Streptococcus pneumoniae.
- Mortality rate varies between 0-20% [28]
- Extended duration operation time, larger volume of intra-operative blood loss
- Longer duration of hospital stay than percutaneous drainage procedure
Complications
Prevention
Primary Prevention
Primary prevention for splenic abscess can prevent in specific cases especially patients who are at high risk such as immunocompromised patients (e.g. recipients of renal transplants or patients on immunosuppressive drugs for other reasons).
- In transplant patients best way to prevent splenic abscess is by splenectomy, where as in patients with other immunocompromised states it can be achieved by proper care, early detection and aggressive treatment of minor infections.[1]
- Avoid intravenous drug abuse
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 Gadacz T, Way LW, Dunphy JE (1974). "Changing clinical spectrum of splenic abscess". Am J Surg. 128 (2): 182–7. PMID 4550054.
- ↑ 2.0 2.1 2.2 ZATZKIN HR, DRAZAN AD, IRWIN GA (1964). "ROENTGENOGRAPHIC DIAGNOSIS OF SPLENIC ABSCESS". Am J Roentgenol Radium Ther Nucl Med. 91: 896–9. PMID 14139921.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Nelken N, Ignatius J, Skinner M, Christensen N (1987). "Changing clinical spectrum of splenic abscess. A multicenter study and review of the literature". Am J Surg. 154 (1): 27–34. PMID 3300398.
- ↑ Billings AE (1928). "ABSCESS OF THE SPLEEN". Ann Surg. 88 (3): 416–28. PMC 1398901. PMID 17865957.
- ↑ Elting AW (1915). "ABSCESS OF THE SPLEEN". Ann Surg. 62 (2): 182–92. PMC 1406707. PMID 17863403.
- ↑ 6.0 6.1 6.2 6.3 6.4 Ooi LL, Leong SS (1997). "Splenic abscesses from 1987 to 1995". Am J Surg. 174 (1): 87–93. PMID 9240961.
- ↑ 7.0 7.1 7.2 Chun CH, Raff MJ, Contreras L, Varghese R, Waterman N, Daffner R; et al. (1980). "Splenic abscess". Medicine (Baltimore). 59 (1): 50–65. PMID 6986009.
- ↑ 8.0 8.1 8.2 Phillips GS, Radosevich MD, Lipsett PA (1997). "Splenic abscess: another look at an old disease". Arch Surg. 132 (12): 1331–5, discussion 1335-6. PMID 9403539.
- ↑ Lawhorne TW, Zuidema GD (1976). "Splenic abscess". Surgery. 79 (6): 686–9. PMID 1273753.
- ↑ 10.0 10.1 Zerem E, Bergsland J (2006). "Ultrasound guided percutaneous treatment for splenic abscesses: the significance in treatment of critically ill patients". World J Gastroenterol. 12 (45): 7341–5. PMC 4087495. PMID 17143953.
- ↑ 11.0 11.1 11.2 11.3 Sreekar H, Saraf V, Pangi AC, Sreeharsha H, Reddy R, Kamat G (2011). "A retrospective study of 75 cases of splenic abscess". Indian J Surg. 73 (6): 398–402. doi:10.1007/s12262-011-0370-y. PMC 3236272. PMID 23204694.
- ↑ 12.0 12.1 Ho HS, Wisner DH (1993). "Splenic abscess in the intensive care unit". Arch Surg. 128 (8): 842–6, discussion 846-8. PMID 8343056.
- ↑ Gadacz TR (1985). "Splenic abscess". World J Surg. 9 (3): 410–5. PMID 3892934.
- ↑ Helton WS, Carrico CJ, Zaveruha PA, Schaller R (1986). "Diagnosis and treatment of splenic fungal abscesses in the immune-suppressed patient". Arch Surg. 121 (5): 580–6. PMID 3518659.
- ↑ Linker CA, DeGregorio MW, Ries CA (1984). "Computerized tomography in the diagnosis of systemic candidiasis in patients with acute leukemia". Med Pediatr Oncol. 12 (6): 380–5. PMID 6503858.
- ↑ Farres H, Felsher J, Banbury M, Brody F (2004). "Management of splenic abscess in a critically ill patient". Surg Laparosc Endosc Percutan Tech. 14 (2): 49–52. PMID 15287600.
- ↑ 17.0 17.1 Chang KC, Chuah SK, Changchien CS, Tsai TL, Lu SN, Chiu YC; et al. (2006). "Clinical characteristics and prognostic factors of splenic abscess: a review of 67 cases in a single medical center of Taiwan". World J Gastroenterol. 12 (3): 460–4. PMC 4066069. PMID 16489650.
- ↑ Linos DA, Nagorney DM, McIlrath DC (1983). "Splenic abscess--the importance of early diagnosis". Mayo Clin Proc. 58 (4): 261–4. PMID 6834894.
- ↑ Kolawole TM, Bohrer SP (1973). "Splenic abscess and the gene for hemoglobin S." Am J Roentgenol Radium Ther Nucl Med. 119 (1): 175–89. PMID 4744723.
- ↑ Simson JN (1980). "Solitary abscess of the spleen". Br J Surg. 67 (2): 106–10. PMID 7362937.
- ↑ Balasubramanian SP, Mojjada PR, Bose SM (2002). "Ruptured staphylococcal splenic abscess resulting in peritonitis: report of a case". Surg Today. 32 (6): 566–7. doi:10.1007/s005950200100. PMID 12107789.
- ↑ Nikolaidis N, Giouleme O, Gkisakis D, Grammatikos N (2005). "Posttraumatic splenic abscess with gastrosplenic fistula". Gastrointest Endosc. 61 (6): 771–2. PMID 15855993.
- ↑ Thanos L, Dailiana T, Papaioannou G, Nikita A, Koutrouvelis H, Kelekis DA (2002). "Percutaneous CT-guided drainage of splenic abscess". AJR Am J Roentgenol. 179 (3): 629–32. doi:10.2214/ajr.179.3.1790629. PMID 12185032.
- ↑ Ralls PW, Quinn MF, Colletti P, Lapin SA, Halls J (1982). "Sonography of pyogenic splenic abscess". AJR Am J Roentgenol. 138 (3): 523–5. doi:10.2214/ajr.138.3.523. PMID 7039270.
- ↑ Pawar S, Kay CJ, Gonzalez R, Taylor KJ, Rosenfield AT (1982). "Sonography of splenic abscess". AJR Am J Roentgenol. 138 (2): 259–62. doi:10.2214/ajr.138.2.259. PMID 6976726.
- ↑ Paris S, Weiss SM, Ayers WH, Clarke LE (1994). "Splenic abscess". Am Surg. 60 (5): 358–61. PMID 8161087.
- ↑ Faught WE, Gilbertson JJ, Nelson EW (1989). "Splenic abscess: presentation, treatment options, and results". Am J Surg. 158 (6): 612–4. PMID 2589597.
- ↑ 28.0 28.1 Green BT (2001). "Splenic abscess: report of six cases and review of the literature". Am Surg. 67 (1): 80–5. PMID 11206904.
- ↑ Johnson JD, Raff MJ (1984). "Fungal splenic abscess". Arch Intern Med. 144 (10): 1987–93. PMID 6385895.
- ↑ Choudhury S R, Rajiv C, Pitamber S, Akshay S, Dharmendra S (2006). "Management of splenic abscess in children by percutaneous drainage". J Pediatr Surg. 41 (1): e53–6. doi:10.1016/j.jpedsurg.2005.10.085. PMID 16410091.
- ↑ Teich S, Oliver GC, Canter JW (1986). "The early diagnosis of splenic abscess". Am Surg. 52 (6): 303–7. PMID 3521422.
- ↑ Hadas-Halpren I, Hiller N, Dolberg M (1992). "Percutaneous drainage of splenic abscesses: an effective and safe procedure". Br J Radiol. 65 (779): 968–70. doi:10.1259/0007-1285-65-779-968. PMID 1450832.
- ↑ Kang M, Saxena AK, Gulati M, Suri S (2004). "Ultrasound-guided percutaneous catheter drainage of splenic abscess". Pediatr Radiol. 34 (3): 271–3. doi:10.1007/s00247-003-1068-5. PMID 14530888.
- ↑ Gerzof SG, Johnson WC, Robbins AH, Nabseth DC (1985). "Expanded criteria for percutaneous abscess drainage". Arch Surg. 120 (2): 227–32. PMID 3977590.