Clopidogrel: Difference between revisions
No edit summary |
No edit summary |
||
| Line 197: | Line 197: | ||
Avoid using omeprazole or esomeprazole with clopidogrel tablets USP. [[Omeprazole]] and [[esomeprazole]] significantly reduce the antiplatelet activity of clopidogrel tablets USP. When concomitant administration of a PPI is required, consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Clinical Pharmacology (12.3)]. | Avoid using omeprazole or esomeprazole with clopidogrel tablets USP. [[Omeprazole]] and [[esomeprazole]] significantly reduce the antiplatelet activity of clopidogrel tablets USP. When concomitant administration of a PPI is required, consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Clinical Pharmacology (12.3)]. | ||
|overdose=Platelet inhibition by clopidogrel is irreversible and will last for the life of the platelet. Overdose following clopidogrel administration may result in bleeding complications. A single oral dose of clopidogrel at 1500 or 2000 mg/kg was lethal to mice and to rats and at 3000 mg/kg to baboons. Symptoms of acute toxicity were [[vomiting]], [[prostration]], difficult breathing, and [[gastrointestinal hemorrhage]] in animals. | |||
Based on biological plausibility, platelet transfusion may restore clotting ability. | |||
|mechAction=Clopidogrel is an inhibitor of platelet activation and aggregation through the irreversible binding of its active metabolite to the P2Y12 class of ADP receptors on platelets. | |||
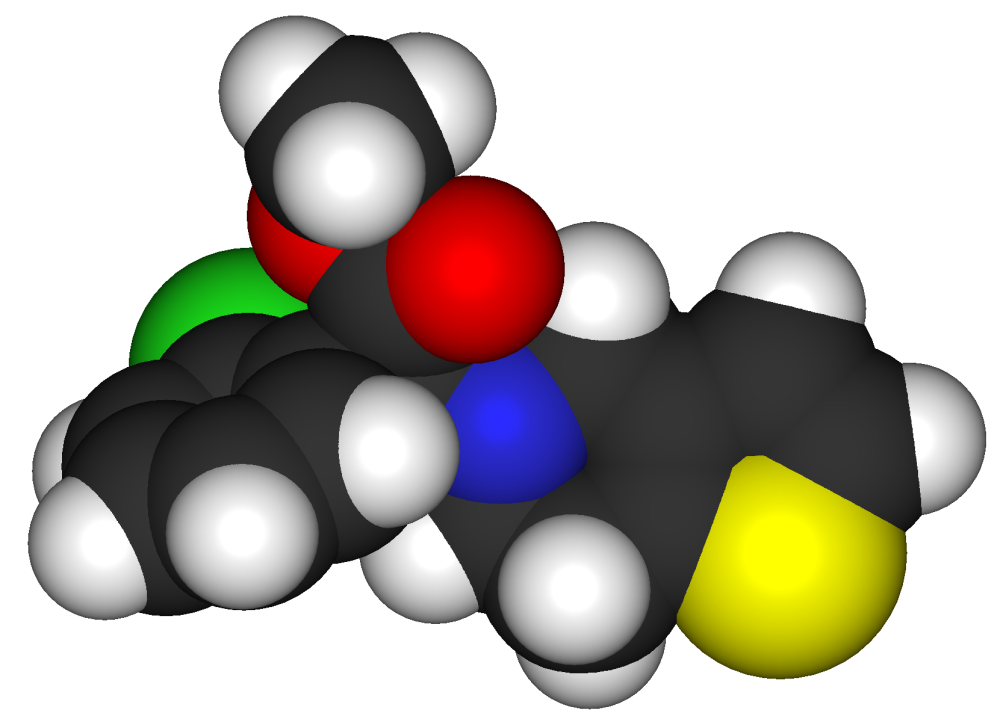
|structure=Clopidogrel bisulfate, USP is a thienopyridine class inhibitor of P2Y12 ADP platelet receptors. Chemically it is methyl (+)-(S)-α-(2-chlorophenyl)-6,7-dihydrothieno[3,2-c]pyridine-5(4H)-acetate sulfate (1:1). | |||
The structural formula is as follows: | |||
[[File:Clopidogrel_pharmacology_01.jpg|thumb|none|400px]] | |||
C16H16ClNO2S•H2SO4 M.W. 419.9 | |||
Clopidogrel bisulfate, USP is a white to off-white powder. It is practically insoluble in water at neutral pH but freely soluble at pH 1. It also dissolves freely in methanol, dissolves sparingly in methylene chloride, and is practically insoluble in ethyl ether. It has a specific optical rotation of about +56°. | |||
Clopidogrel bisulfate, USP for oral administration is provided as light-pink to pink, debossed, film-coated, capsule shaped tablets containing 97.875 mg of clopidogrel bisulfate, USP which is the molar equivalent of 75 mg of clopidogrel base. | |||
Each tablet contains the following inactive ingredients: crospovidone, hydrogenated vegetable oil, hydroxypropyl cellulose, hypromellose, indigo carmine aluminum lake FD&C blue #2, iron oxide red, iron oxide yellow, lactose, lactose monohydrate, microcrystalline cellulose, polyethylene glycol, sodium lauryl sulfate, and titanium dioxide. | |||
|PD=Clopidogrel must be metabolized by CYP450 enzymes to produce the active metabolite that inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible. Consequently, platelets exposed to clopidogrel’s active metabolite are affected for the remainder of their lifespan (about 7 to 10 days). Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP. | |||
Dose-dependent inhibition of platelet aggregation can be seen 2 hours after single oral doses of clopidogrel. Repeated doses of 75 mg clopidogrel per day inhibit ADP-induced platelet aggregation on the first day, and inhibition reaches steady state between Day 3 and Day 7. At steady state, the average inhibition level observed with a dose of 75 mg clopidogrel per day was between 40% and 60%. Platelet aggregation and bleeding time gradually return to baseline values after treatment is discontinued, generally in about 5 days. | |||
''Geriatric Patients'' | |||
Elderly (≥ 75 years) and young healthy subjects had similar effects on platelet aggregation. | |||
''Renally-Impaired Patients'' | |||
After repeated doses of 75 mg clopidogrel per day, patients with severe renal impairment (creatinine clearance from 5 to 15 mL/min) and moderate renal impairment (creatinine clearance from 30 to 60 mL/min) showed low (25%) inhibition of ADP-induced platelet aggregation. | |||
''Hepatically-Impaired Patients'' | |||
After repeated doses of 75 mg clopidogrel per day for 10 days in patients with severe hepatic impairment, inhibition of ADP-induced platelet aggregation was similar to that observed in healthy subjects. | |||
''Gender'' | |||
In a small study comparing men and women, less inhibition of ADP-induced platelet aggregation was observed in women. | |||
|PK=Clopidogrel is a prodrug and is metabolized to a pharmacologically active metabolite and inactive metabolites. | |||
Absorption | |||
After single and repeated oral doses of 75 mg per day, clopidogrel is rapidly absorbed. Absorption is at least 50%, based on urinary excretion of clopidogrel metabolites. | |||
Effect of Food | |||
Clopidogrel can be administered with or without food. In a study in healthy male subjects when clopidogrel 75 mg per day was given with a standard breakfast, mean inhibition of ADP-induced platelet aggregation was reduced by less than 9%. The active metabolite AUC0-24 was unchanged in the presence of food, while there was a 57% decrease in active metabolite Cmax. Similar results were observed when a clopidogrel 300 mg loading dose was administered with a high-fat breakfast. | |||
Metabolism | |||
Clopidogrel is extensively metabolized by two main metabolic pathways: one mediated by esterases and leading to hydrolysis into an inactive carboxylic acid derivative (85% of circulating metabolites) and one mediated by multiple cytochrome P450 enzymes. Cytochromes first oxidize clopidogrel to a 2-oxo-clopidogrel intermediate metabolite. Subsequent metabolism of the 2-oxo-clopidogrel intermediate metabolite results in formation of the active metabolite, a thiol derivative of clopidogrel. This metabolic pathway is mediated by CYP2C19, CYP3A, CYP2B6 and CYP1A2. The active thiol metabolite binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation for the lifespan of the platelet. | |||
The Cmax of the active metabolite is twice as high following a single 300 mg clopidogrel loading dose as it is after four days of 75 mg maintenance dose. Cmax occurs approximately 30 to 60 minutes after dosing. In the 75 to 300 mg dose range, the pharmacokinetics of the active metabolite deviates from dose proportionality: increasing the dose by a factor of four results in 2.0 and 2.7 fold increases in Cmax and AUC, respectively. | |||
Elimination | |||
Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% of total radioactivity was excreted in urine and approximately 46% in feces over the 5 days post-dosing. After a single, oral dose of 75 mg, clopidogrel has a half-life of approximately 6 hours. The half-life of the active metabolite is about 30 minutes. | |||
Drug Interactions | |||
Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of certain inhibitors of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition. | |||
Proton Pump Inhibitors (PPI) | |||
The effect of proton pump inhibitors (PPI) on the systemic exposure to the clopidogrel active metabolite following multiple doses of clopidogrel 75 mg evaluated in dedicated drug interaction studies is presented in Figure 1. | |||
|nonClinToxic=There was no evidence of tumorigenicity when clopidogrel was administered for 78 weeks to mice and 104 weeks to rats at dosages up to 77 mg/kg per day, which afforded plasma exposures > 25 times that in humans at the recommended daily dose of 75 mg. | |||
Clopidogrel was not genotoxic in four in vitro tests (Ames test, DNA-repair test in rat hepatocytes, gene mutation assay in Chinese hamster fibroblasts, and metaphase chromosome analysis of human lymphocytes) and in one in vivo test (micronucleus test by oral route in mice). | |||
Clopidogrel was found to have no effect on fertility of male and female rats at oral doses up to 400 mg/kg per day (52 times the recommended human dose on a mg/m2 basis). | |||
|alcohol=Alcohol-Clopidogrel interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | |alcohol=Alcohol-Clopidogrel interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. | ||
}} | }} | ||
Revision as of 03:33, 7 May 2014
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [2],Sheng Shi, M.D. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERS
See full prescribing information for complete Boxed Warning.
* Effectiveness of clopidogrel depends on activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19. (5.1)
|
Overview
Clopidogrel is a {{{drugClass}}} that is FDA approved for the {{{indicationType}}} of acute coronary syndrome (ACS), recent MI, recent stroke, or established peripheral arterial disease. There is a Black Box Warning for this drug as shown here. Common adverse reactions include non-major bleeding.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Acute Coronary Syndrome
- For patients with non-ST-elevation ACS
- Initial loading dosage: 300 mg PO
- Maitaining dosage: 75 mg PO qd
- In combination with: Aspirin 75-300 mg PO qd
- For patients with STEMI
- Recommended dosage: 75 mg PO qd (With or without the loading dosage)
- In combination with: Aspirin 75-300 mg PO qd
Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
- Dosing information
- 75 mg PO qd
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
Prophylaxis of Thrombosis in PCI treated patients
- Class of Recommendation: Class I
- Level of Evidence: Level B
- Dosing Information
Non–Guideline-Supported Use
Prophylaxis of ThrombosisAtrial in patient with Atrial Fibrillation
- Dosing Information
Prophylaxis of Thrombosis in patient with Chronical Heart failure
- Dosing information
- 75 mg/day[2]
Stasis ulcer
- Dosing information
- Recommended dosage: 75 mg/day for 2-4 weeks[3]
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
Condition 1
- Dosing Information
- (Dosage)
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
Condition 1
- Developed by: (Organization)
- Class of Recommendation: (Class) (Link)
- Strength of Evidence: (Category A/B/C) (Link)
- Dosing Information/Recommendation
- (Dosage)
Non–Guideline-Supported Use
Prophylaxis of Arterial thrombosis
- Dosing Information
- Recommended dosage: 0.2 mg/kg/day[4]
Contraindications
- Active Bleeding
- Clopidogrel is contraindicated in patients with active pathological bleeding such as peptic ulcer or intracranial hemorrhage.
- Clopidogrel tablets are contraindicated in patients with hypersensitivity (e.g., anaphylaxis) to clopidogrel or any component of the product [see Adverse Reactions (6.2)].
Warnings
|
WARNING: DIMINISHED EFFECTIVENESS IN POOR METABOLIZERS
See full prescribing information for complete Boxed Warning.
* Effectiveness of clopidogrel depends on activation to an active metabolite by the cytochrome P450 (CYP) system, principally CYP2C19. (5.1)
|
- Diminished Antiplatelet Activity Due to Impaired CYP2C19 Function
- Clopidogrel is a prodrug. Inhibition of platelet aggregation by clopidogrel is achieved through an active metabolite. The metabolism of clopidogrel to its active metabolite can be impaired by genetic variations in CYP2C19 [see Boxed Warning] and by concomitant medications that interfere with CYP2C19.
Proton Pump Inhibitors
Avoid concomitant use of clopidogrel with omeprazole or esomeprazole because both significantly reduce the antiplatelet activity of clopidogrel [see Drug Interactions (7.1) andDosage and Administration (2.4)].
- General Risk of Bleeding
- Thienopyridines, including clopidogrel, increase the risk of bleeding. If a patient is to undergo surgery and an antiplatelet effect is not desired, discontinue clopidogrel five days prior to surgery. In patients who stopped therapy more than five days prior to CABG the rates of major bleeding were similar (event rate 4.4% clopidogrel + aspirin; 5.3% placebo + aspirin). In patients who remained on therapy within five days of CABG, the major bleeding rate was 9.6% for clopidogrel + aspirin, and 6.3% for placebo + aspirin.
- Thienopyridines inhibit platelet aggregation for the lifetime of the platelet (7 to 10 days), so withholding a dose will not be useful in managing a bleeding event or the risk of bleeding associated with an invasive procedure. Because the half-life of clopidogrel's active metabolite is short, it may be possible to restore hemostasis by administering exogenous platelets; however, platelet transfusions within 4 hours of the loading dose or 2 hours of the maintenance dose may be less effective.
- Discontinuation of Clopidogrel
- Avoid lapses in therapy, and if clopidogrel must be temporarily discontinued, restart as soon as possible. Premature discontinuation of clopidogrel may increase the risk of cardiovascular events.
- Patients With Recent Transient Ischemic Attack (TIA) or Stroke
- TTP, sometimes fatal, has been reported following use of clopidogrel, sometimes after a short exposure (< 2 weeks). TTP is a serious condition that requires urgent treatment including plasmapheresis (plasma exchange). It is characterized by thrombocytopenia, microangiopathic hemolytic anemia (schistocytes [fragmented RBCs] seen on peripheral smear), neurological findings, renal dysfunction, and fever [see Adverse Reactions (6.2)].
- Cross-Reactivity Among Thienopyridines
- Hypersensitivity including rash, angioedema or hematologic reaction have been reported in patients receiving clopidogrel, including patients with a history of hypersensitivity or hematologic reaction to other thienopyridines [see Contraindications (4.2) and Adverse Reactions (6.2)].
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions and durations of follow up, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice. Clopidogrel bisulfate has been evaluated for safety in more than 54,000 patients, including over 21,000 patients treated for 1 year or more. The clinically important adverse reactions observed in trials comparing clopidogrel plus aspirin to placebo plus aspirin and trials comparing clopidogrel bisulfate alone to aspirin alone are discussed below.
Bleeding
- CURE
- In CURE, clopidogrel bisulfate use with aspirin was associated with an increase in major bleeding (primarily gastrointestinal and at puncture sites) compared to placebo with aspirin (see Table 1). The incidence of intracranial hemorrhage (0.1%) and fatal bleeding (0.2%) were the same in both groups. Other bleeding events that were reported more frequently in the clopidogrel group were epistaxis, hematuria, and bruise.
The overall incidence of bleeding is described in Table 1. Ninety-two percent (92%) of the patients in the CURE study received heparin or low molecular weight heparin (LMWH), and the rate of bleeding in these patients was similar to the overall results.
- COMMIT
- In COMMIT, similar rates of major bleeding were observed in the clopidogrel bisulfate and placebo groups, both of which also received aspirin (see Table 2).

- Ninety-two percent (92%) of the patients in the CURE study received heparin or low molecular weight heparin (LMWH), and the rate of bleeding in these patients was similar to the overall results.
COMMIT In COMMIT, similar rates of major bleeding were observed in the clopidogrel bisulfate and placebo groups, both of which also received aspirin (see Table 2).

- CAPRIE (Clopidogrel bisulfate vs. Aspirin)
- In CAPRIE, gastrointestinal hemorrhage occurred at a rate of 2.0% in those taking clopidogrel bisulfate vs. 2.7% in those taking aspirin; bleeding requiring hospitalization occurred in 0.7% and 1.1%, respectively. The incidence of intracranial hemorrhage was 0.4% for clopidogrel bisulfate compared to 0.5% for aspirin.
Other bleeding events that were reported more frequently in the clopidogrel bisulfate group were epistaxis and hematoma.
- Other Adverse Events
- In CURE and CHARISMA, which compared clopidogrel bisulfate plus aspirin to aspirin alone, there was no difference in the rate of adverse events (other than bleeding) between clopidogrel bisulfate and placebo.
- In CAPRIE, which compared clopidogrel bisulfate to aspirin, pruritus was more frequently reported in those taking clopidogrel bisulfate. No other difference in the rate of adverse events (other than bleeding) was reported.
Postmarketing Experience
The following adverse reactions have been identified during post-approval use of clopidogrel. Because these reactions are reported voluntarily from a population of an unknown size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. Blood and lymphatic system disorders: Agranulocytosis, aplastic anemia/pancytopenia, thrombotic thrombocytopenic purpura (TTP), acquired hemophilia A
- Eye disorders: Eye (conjunctival, ocular, retinal) bleeding
- Gastrointestinal disorders: Gastrointestinal and retroperitoneal hemorrhage with fatal outcome, colitis (including ulcerative or lymphocytic colitis), pancreatitis, stomatitis, gastric/duodenal ulcer, diarrhea
- General disorders and administration site condition: Fever, hemorrhage of operative wound
- Hepato-biliary disorders: Acute liver failure, hepatitis (non-infectious), abnormal liver function test
- Immune system disorders: Hypersensitivity reactions, anaphylactoid reactions, serum sickness
- Musculoskeletal, connective tissue and bone disorders: Musculoskeletal bleeding, myalgia, arthralgia, arthritis
- Nervous system disorders: Taste disorders, fatal intracranial bleeding, headache
- Psychiatric disorders: Confusion, hallucinations
- Respiratory, thoracic and mediastinal disorders: Bronchospasm, interstitial pneumonitis, respiratory tract bleeding, eosinophilic pneumonia
- Renal and urinary disorders: Increased creatinine levels
- Skin and subcutaneous tissue disorders: Maculopapular, erythematous or exfoliative rash, urticaria, bullous dermatitis, eczema, toxic epidermal necrolysis, Stevens-Johnson syndrome, angioedema, drug-induced hypersensitivity syndrome, drug rash with eosinophilia and systemic symptoms (DRESS), erythema multiforme, skin bleeding, lichen planus, generalized pruritus
- Vascular disorders: Vasculitis, hypotension
Drug Interactions
- CYP2C19 Inhibitors
- Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of certain drugs that inhibit the activity of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition [see Warnings and Precautions (5.1) and Dosage and Administration (2.4)].
Proton Pump Inhibitors (PPI) Avoid concomitant use of clopidogrel with omeprazole or esomeprazole. In clinical studies, omeprazole was shown to reduce the antiplatelet activity of clopidogrel when given concomitantly or 12 hours apart. A higher dose regimen of clopidogrel concomitantly administered with omeprazole increases antiplatelet response; an appropriate dose regimen has not been established. A similar reduction in antiplatelet activity was observed with esomeprazole when given concomitantly with clopidogrel. Consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite. Dexlansoprazole, lansoprazole and pantoprazole had less effect on the antiplatelet activity of clopidogrel than did omeprazole or esomeprazole [see Dosage and Administration (2.4), WarningsandPrecautions (5.1) and Clinical Pharmacology (12.3)].
- Coadministration of clopidogrel and NSAIDs increases the risk of gastrointestinal bleeding.
- Warfarin (CYP2C9 Substrates)
- Although the administration of clopidogrel 75 mg per day did not modify the pharmacokinetics of S-warfarin (a CYP2C9 substrate) or INR in patients receiving long-term warfarin therapy, coadministration of clopidogrel with warfarin increases the risk of bleeding because of independent effects on hemostasis.
- However, at high concentrations in vitro, clopidogrel inhibits CYP2C9.
- SSRIs and SNRIs
- Since selective serotonin reuptake inhibitors (SSRIs) and serotonin norepinephrine reuptake inhibitors (SNRIs) affect platelet activation, the concomitant administration of SSRIs and SNRIs with clopidogrel may increase the risk of bleeding.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B
Reproduction studies performed in rats and rabbits at doses up to 500 and 300 mg/kg/day, respectively (65 and 78 times the recommended daily human dose, respectively, on a mg/m2 basis), revealed no evidence of impaired fertility or fetotoxicity due to clopidogrel. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of a human response, clopidogrel should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Clopidogrel in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Clopidogrel during labor and delivery.
Nursing Mothers
Studies in rats have shown that clopidogrel and/or its metabolites are excreted in the milk. It is not known whether this drug is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from clopidogrel, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
Pediatric Use
Safety and effectiveness in pediatric populations have not been established. Additional information describing a clinical study in which efficacy was not demonstrated in neonates and infants is approved in the package insert for Bristol-Myers Squibb’s clopidogrel tablets. However, due to Bristol-Myers Squibb’s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
Geriatic Use
Of the total number of subjects in the CAPRIE and CURE controlled clinical studies, approximately 50% of patients treated with clopidogrel were 65 years of age and older, and 15% were 75 years and older. In COMMIT, approximately 58% of the patients treated with clopidogrel were 60 years and older, 26% of whom were 70 years and older. The observed risk of bleeding events with clopidogrel plus aspirin versus placebo plus aspirin by age category is provided in Table 1 and Table 2 for the CURE and COMMIT trials, respectively [see Adverse Reactions (6.1)]. No dosage adjustment is necessary in elderly patients.
Gender
There is no FDA guidance on the use of Clopidogrel with respect to specific gender populations.
Race
There is no FDA guidance on the use of Clopidogrel with respect to specific racial populations.
Renal Impairment
Experience is limited in patients with severe and moderate renal impairment [see Clinical Pharmacology (12.2)].
Hepatic Impairment
No dosage adjustment is necessary in patients with hepatic impairment [see Clinical Pharmacology (12.2)].
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Clopidogrel in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Clopidogrel in patients who are immunocompromised.
Administration and Monitoring
Administration
Acute Coronary Syndrome
Clopidogrel tablets USP can be administered with or without food [see Clinical Pharmacology (12.3)]. For patients with non-ST-elevation ACS (UA/NSTEMI), initiate clopidogrel tablets USP with a single 300 mg oral loading dose and then continue at 75 mg once daily. Initiate aspirin (75 to 325 mg once daily) and continue in combination with clopidogrel tablets USP [see Clinical Studies (14.1)]. For patients with STEMI, the recommended dose of clopidogrel tablets USP is 75 mg once daily orally, administered in combination with aspirin (75 to 325 mg once daily), with or without thrombolytics. Clopidogrel tablets USP may be initiated with or without a loading dose [see Clinical Studies (14.1)].
Recent MI, Recent Stroke, or Established Peripheral Arterial Disease
The recommended daily dose of clopidogrel tablets USP is 75 mg once daily orally, with or without food [see Clinical Pharmacology (12.3)].
CYP2C19 Poor Metabolizers
CYP2C19 poor metabolizer status is associated with diminished antiplatelet response to clopidogrel. Although a higher dose regimen in poor metabolizers increases antiplatelet response [see Clinical Pharmacology (12.5)], an appropriate dose regimen for this patient population has not been established.
Use With Proton Pump Inhibitors (PPI)
Avoid using omeprazole or esomeprazole with clopidogrel tablets USP. Omeprazole and esomeprazole significantly reduce the antiplatelet activity of clopidogrel tablets USP. When concomitant administration of a PPI is required, consider using another acid-reducing agent with minimal or no CYP2C19 inhibitory effect on the formation of clopidogrel active metabolite [see Warnings and Precautions (5.1), Drug Interactions (7.1) and Clinical Pharmacology (12.3)].
Monitoring
There is limited information regarding Clopidogrel Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Clopidogrel and IV administrations.
Overdosage
Platelet inhibition by clopidogrel is irreversible and will last for the life of the platelet. Overdose following clopidogrel administration may result in bleeding complications. A single oral dose of clopidogrel at 1500 or 2000 mg/kg was lethal to mice and to rats and at 3000 mg/kg to baboons. Symptoms of acute toxicity were vomiting, prostration, difficult breathing, and gastrointestinal hemorrhage in animals. Based on biological plausibility, platelet transfusion may restore clotting ability.
Pharmacology
There is limited information regarding Clopidogrel Pharmacology in the drug label.
Mechanism of Action
Clopidogrel is an inhibitor of platelet activation and aggregation through the irreversible binding of its active metabolite to the P2Y12 class of ADP receptors on platelets.
Structure
Clopidogrel bisulfate, USP is a thienopyridine class inhibitor of P2Y12 ADP platelet receptors. Chemically it is methyl (+)-(S)-α-(2-chlorophenyl)-6,7-dihydrothieno[3,2-c]pyridine-5(4H)-acetate sulfate (1:1). The structural formula is as follows:

C16H16ClNO2S•H2SO4 M.W. 419.9 Clopidogrel bisulfate, USP is a white to off-white powder. It is practically insoluble in water at neutral pH but freely soluble at pH 1. It also dissolves freely in methanol, dissolves sparingly in methylene chloride, and is practically insoluble in ethyl ether. It has a specific optical rotation of about +56°. Clopidogrel bisulfate, USP for oral administration is provided as light-pink to pink, debossed, film-coated, capsule shaped tablets containing 97.875 mg of clopidogrel bisulfate, USP which is the molar equivalent of 75 mg of clopidogrel base. Each tablet contains the following inactive ingredients: crospovidone, hydrogenated vegetable oil, hydroxypropyl cellulose, hypromellose, indigo carmine aluminum lake FD&C blue #2, iron oxide red, iron oxide yellow, lactose, lactose monohydrate, microcrystalline cellulose, polyethylene glycol, sodium lauryl sulfate, and titanium dioxide.
Pharmacodynamics
Clopidogrel must be metabolized by CYP450 enzymes to produce the active metabolite that inhibits platelet aggregation. The active metabolite of clopidogrel selectively inhibits the binding of adenosine diphosphate (ADP) to its platelet P2Y12 receptor and the subsequent ADP-mediated activation of the glycoprotein GPIIb/IIIa complex, thereby inhibiting platelet aggregation. This action is irreversible. Consequently, platelets exposed to clopidogrel’s active metabolite are affected for the remainder of their lifespan (about 7 to 10 days). Platelet aggregation induced by agonists other than ADP is also inhibited by blocking the amplification of platelet activation by released ADP. Dose-dependent inhibition of platelet aggregation can be seen 2 hours after single oral doses of clopidogrel. Repeated doses of 75 mg clopidogrel per day inhibit ADP-induced platelet aggregation on the first day, and inhibition reaches steady state between Day 3 and Day 7. At steady state, the average inhibition level observed with a dose of 75 mg clopidogrel per day was between 40% and 60%. Platelet aggregation and bleeding time gradually return to baseline values after treatment is discontinued, generally in about 5 days.
Geriatric Patients
Elderly (≥ 75 years) and young healthy subjects had similar effects on platelet aggregation.
Renally-Impaired Patients
After repeated doses of 75 mg clopidogrel per day, patients with severe renal impairment (creatinine clearance from 5 to 15 mL/min) and moderate renal impairment (creatinine clearance from 30 to 60 mL/min) showed low (25%) inhibition of ADP-induced platelet aggregation.
Hepatically-Impaired Patients
After repeated doses of 75 mg clopidogrel per day for 10 days in patients with severe hepatic impairment, inhibition of ADP-induced platelet aggregation was similar to that observed in healthy subjects.
Gender
In a small study comparing men and women, less inhibition of ADP-induced platelet aggregation was observed in women.
Pharmacokinetics
Clopidogrel is a prodrug and is metabolized to a pharmacologically active metabolite and inactive metabolites. Absorption After single and repeated oral doses of 75 mg per day, clopidogrel is rapidly absorbed. Absorption is at least 50%, based on urinary excretion of clopidogrel metabolites. Effect of Food Clopidogrel can be administered with or without food. In a study in healthy male subjects when clopidogrel 75 mg per day was given with a standard breakfast, mean inhibition of ADP-induced platelet aggregation was reduced by less than 9%. The active metabolite AUC0-24 was unchanged in the presence of food, while there was a 57% decrease in active metabolite Cmax. Similar results were observed when a clopidogrel 300 mg loading dose was administered with a high-fat breakfast. Metabolism Clopidogrel is extensively metabolized by two main metabolic pathways: one mediated by esterases and leading to hydrolysis into an inactive carboxylic acid derivative (85% of circulating metabolites) and one mediated by multiple cytochrome P450 enzymes. Cytochromes first oxidize clopidogrel to a 2-oxo-clopidogrel intermediate metabolite. Subsequent metabolism of the 2-oxo-clopidogrel intermediate metabolite results in formation of the active metabolite, a thiol derivative of clopidogrel. This metabolic pathway is mediated by CYP2C19, CYP3A, CYP2B6 and CYP1A2. The active thiol metabolite binds rapidly and irreversibly to platelet receptors, thus inhibiting platelet aggregation for the lifespan of the platelet. The Cmax of the active metabolite is twice as high following a single 300 mg clopidogrel loading dose as it is after four days of 75 mg maintenance dose. Cmax occurs approximately 30 to 60 minutes after dosing. In the 75 to 300 mg dose range, the pharmacokinetics of the active metabolite deviates from dose proportionality: increasing the dose by a factor of four results in 2.0 and 2.7 fold increases in Cmax and AUC, respectively. Elimination Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% of total radioactivity was excreted in urine and approximately 46% in feces over the 5 days post-dosing. After a single, oral dose of 75 mg, clopidogrel has a half-life of approximately 6 hours. The half-life of the active metabolite is about 30 minutes. Drug Interactions Clopidogrel is metabolized to its active metabolite in part by CYP2C19. Concomitant use of certain inhibitors of this enzyme results in reduced plasma concentrations of the active metabolite of clopidogrel and a reduction in platelet inhibition. Proton Pump Inhibitors (PPI) The effect of proton pump inhibitors (PPI) on the systemic exposure to the clopidogrel active metabolite following multiple doses of clopidogrel 75 mg evaluated in dedicated drug interaction studies is presented in Figure 1.
Nonclinical Toxicology
There was no evidence of tumorigenicity when clopidogrel was administered for 78 weeks to mice and 104 weeks to rats at dosages up to 77 mg/kg per day, which afforded plasma exposures > 25 times that in humans at the recommended daily dose of 75 mg. Clopidogrel was not genotoxic in four in vitro tests (Ames test, DNA-repair test in rat hepatocytes, gene mutation assay in Chinese hamster fibroblasts, and metaphase chromosome analysis of human lymphocytes) and in one in vivo test (micronucleus test by oral route in mice). Clopidogrel was found to have no effect on fertility of male and female rats at oral doses up to 400 mg/kg per day (52 times the recommended human dose on a mg/m2 basis).
Clinical Studies
There is limited information regarding Clopidogrel Clinical Studies in the drug label.
How Supplied
There is limited information regarding Clopidogrel How Supplied in the drug label.
Storage
There is limited information regarding Clopidogrel Storage in the drug label.
Images
Drug Images
{{#ask: Page Name::Clopidogrel |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Clopidogrel |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
There is limited information regarding Clopidogrel Patient Counseling Information in the drug label.
Precautions with Alcohol
Alcohol-Clopidogrel interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
There is limited information regarding Clopidogrel Brand Names in the drug label.
Look-Alike Drug Names
There is limited information regarding Clopidogrel Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ ACTIVE Investigators. Connolly SJ, Pogue J, Hart RG, Hohnloser SH, Pfeffer M et al. (2009) Effect of clopidogrel added to aspirin in patients with atrial fibrillation. N Engl J Med 360 (20):2066-78. DOI:10.1056/NEJMoa0901301 PMID: 19336502
- ↑ Massie BM, Collins JF, Ammon SE, Armstrong PW, Cleland JG, Ezekowitz M et al. (2009) Randomized trial of warfarin, aspirin, and clopidogrel in patients with chronic heart failure: the Warfarin and Antiplatelet Therapy in Chronic Heart Failure (WATCH) trial. Circulation 119 (12):1616-24. DOI:10.1161/CIRCULATIONAHA.108.801753 PMID: 19289640
- ↑ Bick RL, Scott RG (2001) Stasis ulcers refractory to therapy--accelerated healing by treatment with clopidogrel +/- dalteparin: a preliminary report. Clin Appl Thromb Hemost 7 (1):21-4. PMID: 11190899
- ↑ Li JS, Yow E, Berezny KY, Bokesch PM, Takahashi M, Graham TP et al. (2008) Dosing of clopidogrel for platelet inhibition in infants and young children: primary results of the Platelet Inhibition in Children On Clopidogrel (PICOLO) trial. Circulation 117 (4):553-9. DOI:10.1161/CIRCULATIONAHA.107.715821 PMID: 18195173
| File:S-Clopidogrel structure.svg | |
 | |
| Clinical data | |
|---|---|
| Trade names | Plavix |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a601040 |
| [[Regulation of therapeutic goods |Template:Engvar data]] | |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | >50% |
| Protein binding | 94–98% |
| Metabolism | Hepatic |
| Elimination half-life | 7–8 hours (inactive metabolite) |
| Excretion | 50% renal 46% biliary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C16H16ClNO2S |
| Molar mass | 321.82 g/mol |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [4]; Associate Editor(s)-in-Chief: Jesus Rosario Hernandez, M.D. [5]
For patient information about Clopidogrel, click here.
Synonyms / Brand Names: PLAVIX®
Overview
Clopidogrel is an oral, thienopyridine class antiplatelet agent used to inhibit blood clots in coronary artery disease, peripheral vascular disease, and cerebrovascular disease. It is marketed by Bristol-Myers Squibb and Sanofi under the trade name Plavix. The drug works by irreversibly inhibiting a receptor called P2Y12, an adenosine diphosphate (ADP) chemoreceptor on platelet cell membranes. Adverse effects include hemorrhage, severe neutropenia, and thrombotic thrombocytopenic purpura (TTP).
Category
Antiplatelets
FDA Package Insert
PLAVIX (clopidogrel bisulfate) tablet, film coated
Indications and Usage | Dosage and Administration | Dosage Forms and Strengths | Contraindications | Warnings and Precautions | Adverse Reactions | Drug Interactions | Use in Specific Populations | Overdosage | Description | Clinical Pharmacology | Nonclinical Toxicology | Clinical Studies | How Supplied/Storage and Handling | Patient Counseling Information | Labels and Packages
Medical Use
Clopidogrel is indicated for:[1]
- Prevention of vascular ischemic events in people with symptomatic atherosclerosis
- Acute coronary syndrome without ST-segment elevation (NSTEMI)
- ST elevation MI (STEMI)
It is also used, along with acetylsalicylic acid (ASA), for the prevention of thrombosis after placement of intracoronary stent[1] or as an alternative antiplatelet drug for people intolerant to ASA.[2]
Its benefit is primarily in those who smoke cigarettes, with only slight benefit in those who do not.[3]
International guidelines granted the highest grade of recommendation for NSTE-ACS, PCI and stent, for clopidogrel in addition to ASA. Consensus-based therapeutic guidelines also recommend the use of clopidogrel rather than ASA for antiplatelet therapy in patients with a history of gastric ulceration, as inhibition of the synthesis of prostaglandins by ASA can exacerbate this condition. A study has shown that, in patients with healed ASA-induced ulcers, however, patients receiving ASA plus the proton pump inhibitor esomeprazole had a lower incidence of recurrent ulcer bleeding than patients receiving clopidogrel.[4] However, a more recent study suggested that prophylaxis with proton pump inhibitors along with clopidogrel following acute coronary syndrome may increase adverse cardiac outcomes, possibly due to inhibition of CYP2C19, which is required for the conversion of clopidogrel to its active form.[5][6][7] The European Medicines Agency has issued a public statement on a possible interaction between clopidogrel and proton pump inhibitors.[8] However, several cardiologists have voiced concern that the studies on which these warnings are based have many limitations and that it is not certain whether there really is an interaction between clopidogrel and proton pump inhibitors.[9]
Adverse Effects
Serious adverse drug reactions associated with clopidogrel therapy include:
- Severe neutropenia (low white blood cells) (Incidence: 1/2,000)
- Thrombotic thrombocytopenic purpura (TTP) (Incidence: 4/1,000,000 patients treated)[10][11]
- Hemorrhage - The annual incidence of hemorrhage may be increased by the co-administration of aspirin.[12]
- Gastrointestinal hemorrhage (incidence: 2.0% annually)
- Cerebral hemorrhage (incidence: 0.1 to 0.4% annually)
- Use of nonsteroidal anti-inflammatory drugs is discouraged in those taking clopidogrel due to increased risk of digestive tract hemorrhage
- Bleeding in the postoperative period: This is especially a problem for patients after heart surgery, where clopidogrel is associated with a more than double the take-back for bleeding rate, as well as other complicatons. The take-back for bleeding occurs when chest tube clogging occurs in the setting of ongoing bleeding in early postoperative period. Often, if chest tube clogging can be avoided, and the chest tubes drain, the patient can be given platelets until the platelet defect is corrected and the bleeding ceases. But, if the bleeding continues, and the chest tubes occlude, then the patient will become hemodynamically unstable and may require an emergency take-back to the operating room. This impacts outcomes and costs of care.
- Most studies researching clopidogrel do not compare patients on clopidogrel to patients taking placebo; rather, clopidogrel use is compared to aspirin use. Thus, attributing side effects directly to clopidogrel is difficult. Other side effects may include:
- Other gastrointestinal side effects
- Upper GI discomfort (27% vs 29% in patients taking aspirin alone)
- Gastric or duodenal ulcer, gastritis
- Diarrhea (4.5% of patients in the CAPRIE trial)[13]
- Rash (6% overall, 0.33% severe)[14]
- Respiratory (infrequent)
- Upper respiratory infections, rhinitis, shortness of breath, cough
- Cardiovascular
- chest pain
- edema (generalized swelling)
- Thrombocytopenia (reduction of platelets, 0.2% severe cases as compared to 0.1% under aspirin)
- Other gastrointestinal side effects
Interactions
Clopidogrel interacts with the following drugs: phenytoin (Dilantin); tamoxifen (Nolvadex); tolbutamide (Orinase); torsemide (Demadex); fluvastatin (Lescol); a blood thinner such as warfarin (Coumadin), heparin, ardeparin (Normiflo), dalteparin (Fragmin), danaparoid (Orgaran), enoxaparin (Lovenox), or tinzaparin (Innohep); (Activase), anistreplase (Eminase), dipyridamole (Persantine), streptokinase (Kabikinase, Streptase), ticlopidine (Ticlid), and urokinase (Abbokinase).
In November 2009, the FDA announced that clopidogrel should be used with caution in patients on proton pump inhibitors.[15][16] The newer antiplatelet agent, prasugrel has minimal interaction with proton pump inhibitors and hence might be a better antiplatelet agent (if there are no other contraindication) in patients who are on proton pump inhibitors.[17]
Pharmacology
Clopidogrel is a prodrug, which requires CYP2C19 for its activation.[18] It acts on the ADP receptor on platelet cell membranes. The drug specifically and irreversibly inhibits the P2Y12 subtype of ADP receptor, which is important in activation of platelets and eventual cross-linking by the protein fibrin.[19] Platelet inhibition can be demonstrated two hours after a single dose of oral clopidogrel, but the onset of action is slow, so that a loading-dose of either 600 or 300 mg is administered when a rapid effect is needed.
Pharmacokinetics and Metabolism
After repeated oral doses of 75 mg of clopidogrel (base), plasma concentrations of the parent compound, which has no platelet-inhibiting effect, are very low and, in general, are below the quantification limit (0.258 µg/L) beyond two hours after dosing.
Clopidogrel is a pro-drug activated in the liver by cytochrome P450 enzymes, including CYP2C19. Due to opening of the thiophene ring, the chemical structure of the active metabolite has three sites that are stereochemically relevant, making a total of eight possible isomers. These are: a stereocentre at C4 (attached to the —SH thiol group), a double bond at C3—C16, and the original stereocentre at C7. Only one of the eight structures is an active antiplatelet drug. This has the following configuration: Z configuration at the C3—C16 double bond, the original S configuration at C7, and, although the stereocentre at C4 cannot be directly determined, as the thiol group is too reactive, work with the active metabolite of the related drug prasugrel suggests that R-configuration of the C4 group is critical for P2Y12 and platelet-inhibitory activity.
The active metabolite has an elimination half-life of about 0.5 to 1 hour and acts by forming a disulfide bridge with the platelet ADP receptor. Patients with a variant allele of CYP2C19 are 1.5 to 3.5 times more likely to die or have complications than patients with the high-functioning allele.[20][21][22]
Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% was excreted in the urine and approximately 46% in the feces in the five days after dosing.
Effect of food: Administration of clopidogrel bisulfate with meals did not significantly modify the bioavailability of clopidogrel as assessed by the pharmacokinetics of the main circulating metabolite.
Absorption and distribution: Clopidogrel is rapidly absorbed after oral administration of repeated doses of 75-milligram clopidogrel (base), with peak plasma levels (approx. 3 mg/L) of the main circulating metabolite occurring approximately one hour after dosing. The pharmacokinetics of the main circulating metabolite are linear (plasma concentrations increased in proportion to dose) in the dose range of 50 to 150 mg of clopidogrel. Absorption is at least 50% based on urinary excretion of clopidogrel-related metabolites. Clopidogrel and the main circulating metabolite bind reversibly in vitro to human plasma proteins (98% and 94%, respectively). The binding is nonsaturable in vitro up to a concentration of 110 μg/mL.
Metabolism and elimination: In vitro and in vivo, clopidogrel undergoes rapid hydrolysis into its carboxylic acid derivative. In plasma and urine, the glucuronide of the carboxylic acid derivative is also observed.
In March 2010, the U.S. Food and Drug Administration (FDA) added a boxed warning to Plavix alerting that the drug can be less effective in people unable to metabolize the drug to convert it to its active form.[23][24]
Pharmacogenetics
CYP2C19 is an important drug-metabolizing enzyme that catalyzes the biotransformation of many clinically useful drugs including antidepressants, barbiturates, proton pump inhibitors, antimalarial and antitumor drugs. Clopidogrel is one of the drugs metabolized by this enzyme.
Several recent landmark studies have proven the importance of 2C19 genotyping in treatment using clopidogrel or Plavix. In March 2010, the FDA put a black box warning on Plavix to make patients and healthcare providers aware that CYP2C19 poor metabolizers, representing up to 14% of patients, are at high risk of treatment failure and that testing is available.[23] Researchers have found that patients with variants in cytochrome P-450 2C19 (CYP2C19) have lower levels of the active metabolite of clopidogrel, less inhibition of platelets, and a 3.58 times greater risk for major adverse cardiovascular events such as death, heart attack, and stroke; the risk was greatest in CYP2C19 poor metabolizers.[25]
Marketing and Litigation

Plavix is marketed worldwide in nearly 110 countries, with sales of US$6.6 billion in 2009.[26] It had been the second-top-selling drug in the world for a few years as of 2007[27] and was still growing by over 20% in 2007. U.S. sales were US$3.8 billion in 2008.[28]
In 2006, generic clopidogrel was briefly marketed by Apotex, a Canadian generic pharmaceutical company before a court order halted further production until resolution of a patent infringement case brought by Bristol-Myers Squibb.[29] The court ruled that Bristol-Myers Squibb's patent was valid and provided protection until November 2011.[30] The FDA extended the patent protection of clopidogrel by six months, giving exclusivity that would expire on May 17, 2012.[31] The FDA approved generic versions of Plavix on May 17, 2012.[32]
In June 2009, the European Medicines Agency (EMEA) gave authorisation to six generic versions of clopidogrel bisulfate and the drug is now available in several European countries, including the United Kingdom.[33]
Generic clopidogrel is produced by several pharmaceutical companies in India and elsewhere, and often sold under its INN clopidogrel. Clopidogrel is marketed by Cipla under the trade name Clopivas, by Sun Pharmaceuticals as Clopilet, by Ranbaxy Laboratories as Ceruvin, under the name "Clavix" by Intas Pharmaceuticals and under the name "Deplatt" by Torrent Pharmaceuticals. In India, it is sold as Clopivas AP, by Cipla, Clopigrel A, by USV, Clopitab A, by Lupin by Lupin(mixed with aspirin).
Generic clopidogrel is produced in Slovenia (European Union) under the trade names Zyllt, Kardogrel and Clopidogrel Krka by Krka d.d., Novo Mesto.
Another Generic clopidogrel is produced for Julphar brand (Gulf Pharmaceutical industries) UAE (GCC) under name of Lavigard by EGIS Pharmaceuticals PLC, Budabest, Hungary ingredient listed as Clopidogrel.
Dosage Forms
Clopidogrel is marketed as clopidogrel bisulfate (clopidogrel hydrogen sulfate), most commonly under the trade names Plavix, as 75 mg and 300 mg oral tablets.[34]
References
- ↑ 1.0 1.1 Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- ↑ Michael D Randall; Karen E Neil (2004). Disease management. 2nd ed. London: Pharmaceutical Press. 159.
- ↑ Gagne, JJ (Sep 17, 2013). "Effect of smoking on comparative efficacy of antiplatelet agents: systematic review, meta-analysis, and indirect comparison". BMJ (Clinical research ed.). 347: f5307. PMID 24046285. Unknown parameter
|coauthors=ignored (help) - ↑ Chan FK (2005). "Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding" (PDF). N. Engl. J. Med. 352 (3): 238–44. doi:10.1056/NEJMoa042087. PMID 15659723. Unknown parameter
|coauthors=ignored (help) - ↑ Mistry SD, Trivedi HR, Parmar DM, Dalvi PS, Jiyo C. (2011). "Impact of [[proton pump inhibitor]]s on efficacy of clopidogrel: Review of evidence". Indian Journal of Pharmacology. 43 (2): 183–6. doi:10.4103/0253-7613.77360. PMC 3081459. PMID 21572655. URL–wikilink conflict (help)
- ↑ Ho PM, Maddox TM, Wang L, Fihn SD, Jesse RL, Peterson ED, Rumsfeld JS. (2009). "Risk of adverse outcomes associated with concomitant use of clopidogrel and proton pump inhibitors following acute coronary syndrome". Journal of the American Medical Association. 301 (9): 937–44. doi:10.1001/jama.2009.261. PMID 19258584.
- ↑ Stockl, KM (April 2010). "Risk of rehospitalization for patients using clopidogrel with a proton pump inhibitor" (PDF). Arch Intern Med. 170 (8): 704–10. doi:10.1001/archinternmed.2010.34. ISSN 1538-3679. PMID 20421557. Unknown parameter
|coauthors=ignored (help) - ↑ Wathion, Noël. "Public statement on possible interaction between clopidogrel and proton pump inhibitors" (PDF). Retrieved 31 March 2011.
- ↑ Hughes, Sue. "EMEA issues warning on possible clopidogrel-PPI interaction, but is there really a problem?". Retrieved 31 March 2011.
- ↑ Zakarija A (2004). "Clopidogrel-Associated TTP An Update of Pharmacovigilance Efforts Conducted by Independent Researchers, Pharmaceutical Suppliers, and the Food and Drug Administration" (PDF). Stroke. 35 (2): 533–8. doi:10.1161/01.STR.0000109253.66918.5E. PMID 14707231. Unknown parameter
|coauthors=ignored (help) - ↑ Plavix prescribing information. Bristol-Myers Squibb / Sanofi.
- ↑ Diener HC (2004). "Aspirin and clopidogrel compared with clopidogrel alone after recent ischaemic stroke or transient ischaemic attack in high-risk patients (MATCH): randomised, double-blind, placebo-controlled trial". The Lancet. 364 (9431): 331–7. doi:10.1016/S0140-6736(04)16721-4. PMID 15276392. Unknown parameter
|coauthors=ignored (help) - ↑ Harker LA, Boissel JP, Pilgrim AJ, Gent M (October 1999). "Comparative safety and tolerability of clopidogrel and aspirin: results from CAPRIE. CAPRIE Steering Committee and Investigators. Clopidogrel versus aspirin in patients at risk of ischaemic events". Drug Saf. 21 (4): 325–35. doi:10.2165/00002018-199921040-00007. PMID 10514023.
- ↑ none listed (November 1996). "A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee". The Lancet. 16 (9038): 1329–39. PMID 8918275.
- ↑ DeNoon, Daniel J. "FDA Warns Plavix Patients of Drug Interactions", WebMD, 2009-11-19. Retrieved 2009-11-23.
- ↑ "Public Health Advisory: Updated Safety Information about a drug interaction between Clopidogrel Bisulfate (marketed as Plavix) and Omeprazole (marketed as Prilosec and Prilosec OTC)". Food and Drug Administration (FDA). November 17, 2009. Archived from the original on 2009-12-29. Retrieved March 13, 2010.
- ↑ John, Jinu (2012). "Current Oral Antiplatelets: Focus Update on Prasugrel". Journal of american board of family medicine. 25: 343–349. doi:10.3122/jabfm.2012.03.100270. Unknown parameter
|coauthors=ignored (help) - ↑ http://www.ncbi.nlm.nih.gov/pubmed/23046071
- ↑ Savi, P (July 2006). "The active metabolite of Clopidogrel disrupts P2Y12 receptor oligomers and partitions them out of lipid rafts" (PDF). Proceedings of the National Academy of Sciences of the USA. 103 (29): 11069–11074. doi:10.1073/pnas.0510446103. PMC 1635153. PMID 16835302. Unknown parameter
|coauthors=ignored (help) - ↑ Mega JL; Close, SL; Wiviott, SD; Shen, L; Hockett, RD; Brandt, JT; Walker, JR; Antman, EM; MacIas, W (January 2009). "Cytochrome p-450 polymorphisms and response to clopidogrel" (PDF). The New England Journal of Medicine. 360 (4): 354–62. doi:10.1056/NEJMoa0809171. PMID 19106084.
- ↑ Simon T; Verstuyft, C; Mary-Krause, M; Quteineh, L; Drouet, E; Méneveau, N; Steg, PG; Ferrières, J; Danchin, N (January 2009). "Genetic Determinants of Response to Clopidogrel and Cardiovascular Events" (PDF). The New England Journal of Medicine. 360 (4): 363–75. doi:10.1056/NEJMoa0808227. PMID 19106083.
- ↑ Collet, J; Hulot, JS; Pena, A; Villard, E; Esteve, JB; Silvain, J; Payot, L; Brugier, D; Cayla, G (January 2009). "Cytochrome P450 2C19 polymorphism in young patients treated with clopidogrel after myocardial infarction: a cohort study". The Lancet. 373 (9660): 309–17. doi:10.1016/S0140-6736(08)61845-0. PMID 19108880.
- ↑ 23.0 23.1 "FDA Announces New Boxed Warning on Plavix: Alerts patients, health care professionals to potential for reduced effectiveness" (Press release). Food and Drug Administration (FDA). March 12, 2010. Retrieved March 13, 2010.
- ↑ "FDA Drug Safety Communication: Reduced effectiveness of Plavix (clopidogrel) in patients who are poor metabolizers of the drug". Food and Drug Administration (FDA). March 12, 2010. Retrieved March 13, 2010.
- ↑ PGxNews.Org (June 2009). "FDA updates Plavix label with PGx data". PGxNews.Org. Retrieved 2009-06-13.[dead link]
- ↑ "New products and markets fuel growth in 2005". IMS Health. Retrieved 2009-03-02.[dead link]
- ↑ "Top Ten Global Products - 2007" (PDF). IMS Health. 2008-02-26. Retrieved 2009-03-02.
- ↑ "Details for Plavix".[verification needed]
- ↑ "Preliminary Injunction Against Apotex Upheld on Appeal" (Press release). Bristol-Myers Squibb. December 8, 2006. Retrieved 2010-03-14.
- ↑ "U.S. judge upholds Bristol, Sanofi patent on Plavix". Reuters. June 19, 2007. Retrieved 2007-09-05.
- ↑ "FDA Gives Plavix a 6 Month Extension-Patent Now Expires on May 17, 2012". January 26, 2011. Retrieved 2012-01-12.
- ↑ "FDA approves generic versions of blood thinner Plavix" (Press release). Food and Drug Administration (FDA). May 17, 2012.
- ↑ Generic Clopidogrel http://www.genericclopidogrel.com/generic-clopidogrel/
- ↑ Joint Royal Colleges Ambulance liaison committee Clinical Practise Guideines Guidelines
External Links
- Plavix official website Bristol-Myers Squibb/Sanofi
- Plavix prescribing information Bristol-Myers Squibb/Sanofi
- Plavix, Aspirin and Stents : Patients' Forum : Angioplasty.Org
- Drug promises end to migraine misery
- U.S. National Library of Medicine: Drug Information Portal - Clopidogrel
- Krka official website
- Pages with script errors
- Pages with citations using unsupported parameters
- CS1 errors: URL–wikilink conflict
- CS1 maint: Multiple names: authors list
- All articles with dead external links
- Articles with dead external links from October 2010
- Articles with invalid date parameter in template
- Articles with dead external links from May 2012
- All pages needing factual verification
- Wikipedia articles needing factual verification from May 2012
- Pages with broken file links
- Template:drugs.com link with non-standard subpage
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- ADP receptor inhibitors
- Carboxylate esters
- Organochlorides
- Prodrugs
- Cardiovascular Drugs
- Drugs