Platelet
|
WikiDoc Resources for Platelet |
|
Articles |
|---|
|
Most recent articles on Platelet |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Platelet at Clinical Trials.gov Clinical Trials on Platelet at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Platelet
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Platelet Risk calculators and risk factors for Platelet
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Platelet |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |


|
WikiDoc Resources for Platelet |
|
Articles |
|---|
|
Most recent articles on Platelet |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Platelet at Clinical Trials.gov Clinical Trials on Platelet at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Platelet
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Platelet Risk calculators and risk factors for Platelet
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Platelet |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Platelets, or thrombocytes, are the cells circulating in the blood that are involved in the cellular mechanisms of primary hemostasis leading to the formation of blood clots. Dysfunction or low levels of platelets predisposes to bleeding, while high levels, although usually asymptomatic, may increase the risk of thrombosis. An abnormality or disease of the platelets is called a thrombocytopathy.
Histology
Like red blood cells, platelets in mammals are anuclear (no cell nucleus) and discoid (disc shaped); they measure 1.5–3.0 μm in diameter. The body has a very limited reserve of platelets, so they can be rapidly depleted. They contain RNA, mitochondria, a canalicular system, and several different types of granules: lysosomes (containing acid hydrolases), dense bodies (containing ADP, ATP, serotonin, histamine, and calcium) and alpha granules (containing fibrinogen, factor V, vitronectin, thrombospondin and von Willebrand factor). The contents of the granules are released upon activation of the platelet.
Production and degradation
Platelets are produced in hematopoiesis by budding off from megakaryocytes. Each megakaryocyte produces 5,000 and 10,000 platelets.
They circulate for approximately one week, and are then destroyed by the spleen and by Kuppfer cells in the liver.
Function
Functions of Platelets can be generalised into a number of categories:
- Adhesion
- Aggregation
- Clot retraction
- Pro-coagulation
- Cytokine signalling
- Phagocytosis[1]
Activation
Platelets are activated when brought into contact with collagen (which is exposed when the endothelial blood vessel lining is damaged), thrombin (primarily through PAR-1), ADP receptors (P2Y1 and P2Y12) expressed on platelets, a negatively charged surface (e.g. glass), or several other activating factors. Once activated, they release a number of different coagulation factors and platelet activating factors. Platelet activation further results in the scramblase-mediated transport of negatively charged phospholipids to the platelet surface. These phospholipids provide a catalytic surface (with the charge provided by phosphatidylserine and phosphatidylethanolamine) for the tenase and prothrombinase complexes.
Adhesion and aggregation
The platelets adhere to each other via adhesion receptors or integrins, and to the endothelial cells in the wall of the blood vessel forming a haemostatic plug in conjunction with fibrin. The high concentration of myosin and actin filaments in platelets are stimulated to contract during aggregation, further reinforcing the plug. The most abundant platelet adhesion receptor is glycoprotein (GP) IIb/IIIa; this is a calcium-dependent receptor for fibrinogen, fibronectin, vitronectin, thrombospondin and von Willebrand factor (vWF). Other receptors include GPIb-V-IX complex (vWF) and GPVI (collagen).
Platelet aggregation is stimulated by thromboxane and α2 receptor-activation, but inhibited by other inflammatory products like PGI2 and PGD2.
Cytokine signalling
Besides being the chief cellular effector of hemostasis, platelets are rapidly deployed to sites of injury or infection and potentially modulate inflammatory processes by interacting with leukocytes and by secreting cytokines, chemokines and other inflammatory mediators[2] [3] [4] [5].
It also secretes e.g. platelet-derived growth factor (PDGF).
Role in disease
High and low counts
A normal platelet count in a healthy person is between 150,000 and 400,000 per mm³ of blood (150–400 x 109/L). 95% of healthy people will have platelet counts in this range. Some will have statistically abnormal platelet counts while having no abnormality, although the likelihood increases if the platelet count is either very low or very high.
Both thrombocytopenia (or thrombopenia) and thrombocytosis may present with coagulation problems. Generally, low platelet counts increase bleeding risks (although there are exceptions, e.g. immune heparin-induced thrombocytopenia) and thrombocytosis (high counts) may lead to thrombosis (although this is mainly when the elevated count is due to myeloproliferative disorder).
Low platelet counts are generally not corrected by transfusion unless the patient is bleeding or the count has fallen below 5 x 109/L; it is contraindicated in thrombotic thrombocytopenic purpura (TTP) as it fuels the coagulopathy. In patients having surgery, a level below 50 x 109/L) is associated with abnormal surgical bleeding, and regional anaesthetic procedures such as epidurals are avoided for levels below 80-100.
Normal platelet counts are not a guarantee of adequate function. In some states the platelets, while being adequate in number, are dysfunctional. For instance, aspirin irreversibly disrupts platelet function by inhibiting cyclooxygenase-1 (COX1), and hence normal hemostasis; normal platelet function may not return until the aspirin has ceased and all the affected platelets have been replaced by new ones, which can take over a week. Similarly, uremia (a consequence of renal failure) leads to platelet dysfunction that may be ameliorated by the administration of desmopressin.
Medications
Oral agents, often used to alter/suppress platelet function:
Intravenous agents, often used to alter/suppress platelet function:
Drugs that decreased platelets count:
Diseases
Disorders leading to a reduced platelet count:
- Thrombocytopenia
- Idiopathic thrombocytopenic purpura - also known as immune thrombocytopenic purpura (ITP)
- Thrombotic thrombocytopenic purpura
- Drug-induced thrombocytopenia, e.g. heparin-induced thrombocytopenia (HIT)
- Gaucher's disease
- Aplastic anemia
Alloimmune disorders
- Fetomaternal alloimmune thrombocytopenia
- Some transfusion reactions
Disorders leading to platelet dysfunction or reduced count:
- HELLP syndrome
- Hemolytic-uremic syndrome
- Chemotherapy
- Dengue
- Alpha–Delta platelet storage pool deficiency (αδSPD) is a rare inherited bleeding disorder.[6]
Disorders featuring an elevated count:
- Thrombocytosis, including benign essential thrombocytosis (elevated counts, either reactive or as an expression of myeloproliferative disease); may feature dysfunctional platelets
Disorders of platelet adhesion or aggregation:
- Bernard-Soulier syndrome
- Glanzmann's thrombasthenia
- Scott's syndrome
- von Willebrand disease
- Hermansky-Pudlak Syndrome
Disorders of platelet metabolism
- Decreased cyclooxygenase activity, induced or congenital
- Storage pool defects, acquired or congenital
Disorders that indirectly compromise platelet function:
Disorders in which platelets play a key role:
- Atherosclerosis
- Coronary artery disease, CAD and myocardial infarction, MI
- Cerebrovascular disease and Stroke, CVA (cerebrovascular accident)
- Peripheral artery occlusive disease (PAOD)
- Cancer [7]
Discovery
Brewer[8] traced the history of the discovery of the platelet. Although red blood cells had been known since van Leeuwenhoek, it was the German anatomist Max Schultze (1825-1874) who first offered a description of the platelet in his newly founded journal Archiv für mikroscopische Anatomie[9]. He describes "spherules" much smaller than red blood cells that are occasionally clumped and may participate in collections of fibrous material. He recommends further study of the findings.
Giulio Bizzozero (1846-1901), building on Schultze's findings, used "living circulation" to study blood cells of amphibians microscopically in vivo. One of his findings was the fact that platelets clump at the site of blood vessel injury, which precedes the formation of a blood clot. This observation confirmed the role of platelets in coagulation[10].
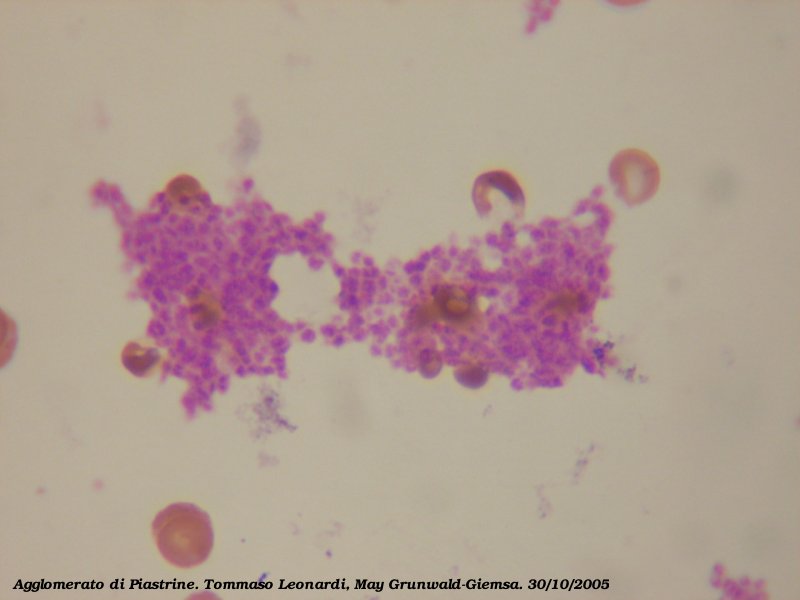
Additional images
-
Blood cell lineage
In transfusion medicine
Platelets are either isolated from collected units of Whole Blood and pooled to make a therapeutic dose or collected by Apheresis, sometimes concurrently with Plasma or Red Blood Cells. The industry standard is for platelets to be tested for bacteria before transfusion to avoid septic reactions, which can be fatal.
Pooled Whole Blood Platelets, sometimes called "random" platelets, are made by taking a unit of Whole Blood from a donor that has not been cooled and placing it into a large centrifuge in what is referred to as a "soft spin." This splits the blood into three layers: the plasma, a "buffy coat" layer which includes the platelets, and the red blood cells. These are expressed into different bags for storage. From four to six of these are typically pooled into a single bag for a therapeutic dose, though individual components can also be used.
Apheresis Platelets are collected using a device which draws blood from the donor and centrifuges the collected blood to separate out the platelets and other components to be collected. The remaining blood is returned to the donor. The advantage to this method is that a single donation provides at least one therapeutic dose, as opposed to the multiple donations for Whole Blood Platelets. This means that a recipient is not exposed to as many different donors and has less risk of transfusion transmitted disease and other complications. Sometimes a person such as a cancer patient who requires routine transfusions of platelets will receive repeated donations from a specific donor to further minimize the risk.
Platelets are not crossmatched unless they contain a significant amount of RBCs, which results in a reddish-orange color to the product. This is usually associated with whole blood platelets, as apheresis methods are more efficient than "soft spin" centrifugation at isolating the specific components of blood. An effort is usually made to issue type specific platelets, but this is not as critical as it is with Red Blood Cells.
Platelets collected by either method have a very short shelf life, typically five or seven days depending on the system used. This results in frequent problems with short supply, as testing the donations often uses up a full day of this time. Since there are no effective preservative solutions for platelets, they lose potency quickly and are best when fresh.
Platelets, either apheresis or random donor platelets, can be processed through a volume reduction process. In this process, the platelets are spun in a centrifuge and the excess plasma is removed, leaving 10 to 100 ml of platelet concentrate. Volume reduced platelets are normally only transfused to neonatal and pediatric patients when a large volume of plasma could overload the child's small circulatory system. The lower volume of plasma also reduces the chances of an adverse transfusion reaction to plasma protiens.[11] Volume reduced platelets have a shelf life of only four hours.[12]
References
- ↑ Movat H.Z; et al. (1965). "Platelet Phagocytosis and Aggregation". Journal of Cell Biology. 27: 531–543.
- ↑ Weyrich A.S.; et al. (2004). "Platelets: signaling cells in the immune continuum". Trends Immunol. 25: 489–495. External link in
|journal=(help) - ↑ Wagner D.D.; et al. (2003). "Platelets in inflammation and thrombosis". Thromb Vasc Biol. 23: 2131–2137. External link in
|journal=(help) - ↑ Diacovo T.G.; et al. (1996). "Platelet-mediated lymphocyte delivery to high endothelial venules". Science. 273: 252–255. External link in
|journal=(help) - ↑ Iannacone M.; et al. (2005). "Platelets mediate cytotoxic T lymphocyte-induced liver damage". Nat Med. 11: 1167–1169. External link in
|journal=(help) - ↑ http://www.informaworld.com/smpp/content~content=a770733890~db=all~jumptype=rss
- ↑ McCarty OJT.; et al. (2000). "Immobilized platelets support human colon carcinoma cell tethering, rolling, and firm adhesion under dynamic flow conditions". Blood. 96: 1789–1197. External link in
|journal=(help) - ↑ Brewer DB. Max Schultze (1865), G. Bizzozero (1882) and the discovery of the platelet. Br J Haematol 2006;133:251-8. PMID 16643426.
- ↑ Schultze M. Ein heizbarer Objecttisch und seine Verwendung bei Untersuchungen des Blutes. Arch Mikrosc Anat 1865;1:1-42.
- ↑ Bizzozero J. Über einen neuen Forrnbestandteil des Blutes und dessen Rolle bei der Thrombose und Blutgerinnung. Arch Pathol Anat Phys Klin Med 1882;90:261-332.
- ↑ Schoenfeld H, Spies C, Jakob C (2006). "Volume-reduced platelet concentrates". Curr. Hematol. Rep. 5 (1): 82–8. PMID 16537051.
- ↑ http://www.cbbsweb.org/enf/2001/pltwashvol.html
See also
Template:Hematology Template:SIB
ar:صفيحة دموية bn:অণুচক্রিকা bg:Тромбоцит ca:Plaqueta cs:Krevní destička da:Blodplade de:Thrombozyt dv:ޕްލޭޓްލިޓް eo:Trombocito eu:Plaketa gl:Plaqueta ko:혈소판 hr:Trombociti id:Keping darah ia:Plachetta is:Blóðflaga it:Piastrina he:טסית דם la:Thrombociti lt:Trombocitas mk:Тромбоцит nl:Bloedplaatje nds:Bloodplattken qu:Yawar llukllunacha sq:Trombociti simple:Platelet sk:Krvná doštička sr:Крвне плочице su:Trombosit fi:Verihiutale sv:Trombocyter ta:இரத்தத் தட்டு uk:Тромбоцити
