Lichen planus
| Lichen planus | |
 |
|---|
|
WikiDoc Resources for Lichen planus |
|
Articles |
|---|
|
Most recent articles on Lichen planus Most cited articles on Lichen planus |
|
Media |
|
Powerpoint slides on Lichen planus |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Lichen planus at Clinical Trials.gov Trial results on Lichen planus Clinical Trials on Lichen planus at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Lichen planus NICE Guidance on Lichen planus
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Lichen planus Discussion groups on Lichen planus Patient Handouts on Lichen planus Directions to Hospitals Treating Lichen planus Risk calculators and risk factors for Lichen planus
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Lichen planus |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
For patient information, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1];Associate Editor(s)-in-Chief: Kiran Singh, M.D. [2]
Synonyms and keywords: Ruber planus; Wickham striae
Overview
Lichen planus is an inflammatory disease that affects the skin and the oral mucosa.
Historical Perspective
Classification
Lichen Planopilaris is the specific name given to lichen planus on the scalp that may cause permanent, scarring alopecia. If left untreated the scarring will cause permanent hair loss. The Cicatricial Alopecia Research Foundation is a non-profit organization that provides support and resources for people with lichen planopilaris.
Pathophysiology
Causes
Common Causes
The cause of lichen planus is not known; however, there are cases of lichen planus-type rashes (known as lichenoid reactions) occurring as allergic reactions to medications for high blood pressure, heart disease and arthritis. These lichenoid reactions are referred to as lichenoid mucositis (of the mucosa) or dermatitis (of the skin). Lichen planus has been reported as a complication of chronic hepatitis C virus infection and can be a sign of chronic graft-versus-host disease of the skin. It has been suggested that true lichen planus may respond to stress, where lesions may present on the mucosa or skin during times of stress in those with the disease.
Causes in Alphabetical Order
- Allergic reactions to medications for high blood pressure
- Arthritis
- Bendrofluazide
- Chloroquine
- Gold salts
- Graft-versus-host disease
- Heart disease
- Hepatitis C
- Hydrochlorothiazide
- Lichen planopilaris
- Lichen ruber moniliformis
- Mepacrine
- Methyldopa
- Methyldopate
- Penicillamine
- Stress
Differentiating lichen planus from other Diseases
The clinical presentation of lichen planus may also resemble other conditions, including:
- Lichenoid drug reaction
- Discoid lupus erythematosus
- Chronic ulcerative stomatitis
- Pemphigus vulgaris
- Benign mucous membrane pemphigoid
- Oral leukoplakia
- Frictional keratosis
A biopsy is useful in identifying histological features that help differentiate lichen planus from these conditions.
Epidemiology and Demographics
Age
Lichen planus in children is rare, and it occurs most often in middle-aged adults.
Gender
Lichen planus affects women more than men (at a ratio of 3:2).
Risk Factors
Some of the risk factors for lichen planus are as follows:
- Exposure to medications, dyes, and other chemical substances (including gold, antibiotics, arsenic, iodides, chloroquine, quinacrine, quinide, phenothiazines, and diuretics)
- Disorders such as hepatitis C
Natural History, Complications, and Prognosis
Lichen planus is usually not harmful and may get better with treatment. It usually clears up within 18 months. However it may last for weeks to months, and may come and go for years. If lichen planus is caused by a medication, the rash should go away once the medicine is stopped.
A possible complication that is associated with lichen planus is that mouth ulcers that are there for a long time may develop into oral cancer.
Diagnosis
Symptoms
The microscopic appearance of lichen planus is pathognomonic for the condition
- Hyperparakeratosis with thickening of the granular cell layer
- Development of a "saw-tooth" appearance of the rete pegs
- Degeneration of the basal cell layer
- Infiltration of inflammatory cells into the subepithelial layer of connective tissue
Other symptoms such as:
- Cicatricial alopecia
- Genital ulcer
- Gum pathology
- Hyperkeratosis
- Koebner phenomenon
- Lichenoid dermatitis
- Mucosal leucoplakia
- Nail pitting
- Oral ulceration
- Pruritis
- Tongue abnormality
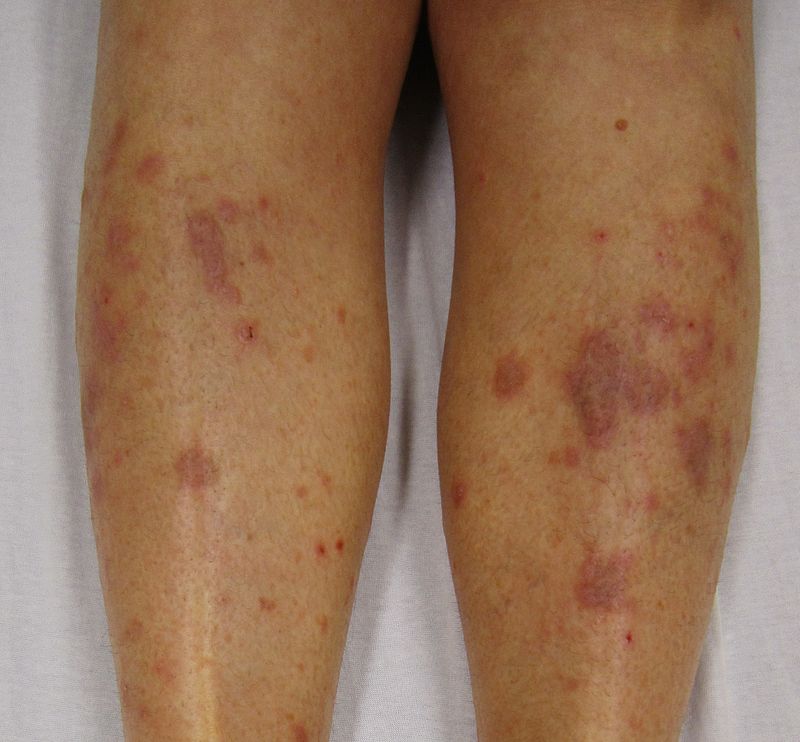
Physical Examination
The typical rash of lichen planus is well-described by the "5 P's": well-defined pruritic, planar, purple, polygonal papules. The commonly affected sites are near the wrist and the ankle. The rash tends to heal with prominent blue-black or brownish discoloration that persists for a long time. Besides the typical lesions, many morphological varieties of the rash may occur. The presence of cutaneous lesions is not constant and may wax and wane over time. Oral lesions tend to last far longer than cutaneous lichen planus lesions.
The following images show good examples of how lichen planus manifests on the body.
-
Lichen planus close up
-
Lichen planus on the arm
-
Lichen planus on the oral mucosa
-
Lichen planus on the hands
Skin
Trunk
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
Extremity
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
Oral cavity
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
Face
-
Lichen planus. Adapted from Dermatology Atlas.[1]
Lichen Planus Actinicus
Face
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
Trunk
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
Extremity
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
-
Lichen planus actinicus. Adapted from Dermatology Atlas.[1]
Lichen planus annular
Trunk
-
Lichen planus annular. Adapted from Dermatology Atlas.[1]
-
Lichen planus annular. Adapted from Dermatology Atlas.[1]
Lichen Planus Follicularis
Neck
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
Extremity
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
Scalp
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
-
Lichen planus follicularis. Adapted from Dermatology Atlas.[1]
Lichen Planus Linearis
Trunk
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
Extremity
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
-
Lichen planus linearis. Adapted from Dermatology Atlas.[1]
Lichen Planus Verrucosus
-
Lichen planus verrucosus . Adapted from Dermatology Atlas.[1]
-
Lichen planus verrucosus . Adapted from Dermatology Atlas.[1]
Lichen Planus Vesicular
Trunk
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
Extremity
-
Lichen planus vesicular. Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular. Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
-
Lichen planus vesicular . Adapted from Dermatology Atlas.[1]
Mucosal Lichen Planus
Oral cavity
-
Mucosal lichen planus. Adapted from Dermatology Atlas.[1]
-
Mucosal lichen planus . Adapted from Dermatology Atlas.[1]
-
Mucosal lichen planus . Adapted from Dermatology Atlas.[1]
Differential diagnosis
Lichen planus must be differentiated from other diseases that cause ust be differentiated from other diseases that cause rash and eczema such as secondary syphilis and pityriasis rosea.
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[2] |
|
|
 | |
| Pityriasis rosea[3] |
|
|
 | |
| Pityriasis lichenoides chronica |
|
|
||
| Nummular dermatitis[6] |
|
|
|
|
| Secondary syphilis[7] |
|
 | ||
| Bowen’s disease[8] |
|
|
 | |
| Exanthematous pustulosis[10] |
|
|
 | |
| Hypertrophic lichen planus[12] |
|
|
|
 |
| Sneddon–Wilkinson disease[14] |
|
|
||
| Small plaque parapsoriasis[18] |
|
|
|
|
| Intertrigo[20] |
|
|
 | |
| Langerhans cell histiocytosis[21] |
|
|
|
|
| Tinea manuum/pedum/capitis[25] |
|
|
|
|
| Seborrheic dermatitis |
|
|
 |
Head
Oral lichen planus may present in one of three forms.
- The reticular form is the most common presentation and manifests as white lacy streaks on the mucosa (known as Wickham's striae) or as smaller papules (small raised area). The lesions tend to be bilateral and are asymptomatic. The lacy streaks may also be seen on other parts of the mouth, including the gingiva (gums), the tongue, palate and lips.
- The bullous form presents as fluid-filled vesicles which project from the surface.
- The erosive form presents with erythematous (red) areas that are ulcerated and uncomfortable. The erosion of the thin epithelium may occur in multiple areas of the mouth, or in one area, such as the gums, where they resemble desquamative gingivitis. Wickham's striae may also be seen near these ulcerated areas. This form may undergo malignant transformation.
Throat
Rarely, lichen planus shows esophageal involvement, where it can present with erosive esophagitis and stricturing. It has also been hypothesized that it is a precursor to squamous cell carcinoma of the esophagus.
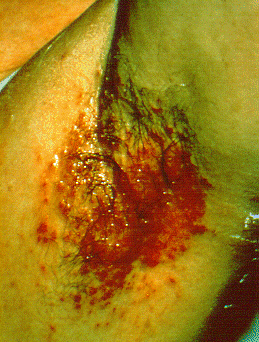
Genitals
Lichen planus may also affect the genital mucosa - vulvovaginal-gingival lichen planus. It can resemble other skin conditions such as atopic dermatitis and psoriasis.
Clinical experience suggests that Lichen planus of the skin alone is easier to treat as compared to one which is associated with oral and genital lesions.
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
-
Lichen planus. Adapted from Dermatology Atlas.[1]
Treatment
Currently there is no cure for lichen planus but there are certain types of medicines used to reduce the effects of the inflammation. Lichen planus may go into a dormant state after treatment. There are also reports that lichen planus can flare up years after it is considered cured.
Medical Therapy
Pharmacotherapy
Acute Pharmacotherapies
Chronic Pharmacotherapies
- Oral retinoids
- Immunosuppressant medications
Surgery
Prevention
References
- ↑ 1.000 1.001 1.002 1.003 1.004 1.005 1.006 1.007 1.008 1.009 1.010 1.011 1.012 1.013 1.014 1.015 1.016 1.017 1.018 1.019 1.020 1.021 1.022 1.023 1.024 1.025 1.026 1.027 1.028 1.029 1.030 1.031 1.032 1.033 1.034 1.035 1.036 1.037 1.038 1.039 1.040 1.041 1.042 1.043 1.044 1.045 1.046 1.047 1.048 1.049 1.050 1.051 1.052 1.053 1.054 1.055 1.056 1.057 1.058 1.059 1.060 1.061 1.062 1.063 1.064 1.065 1.066 1.067 1.068 1.069 1.070 1.071 1.072 1.073 1.074 1.075 1.076 1.077 1.078 1.079 1.080 1.081 1.082 1.083 1.084 1.085 1.086 1.087 1.088 1.089 1.090 1.091 1.092 1.093 1.094 1.095 1.096 1.097 1.098 1.099 1.100 1.101 1.102 1.103 1.104 1.105 1.106 1.107 1.108 1.109 1.110 1.111 1.112 1.113 1.114 1.115 1.116 1.117 1.118 1.119 1.120 1.121 1.122 1.123 1.124 1.125 1.126 1.127 1.128 1.129 1.130 1.131 1.132 1.133 1.134 1.135 1.136 1.137 "Dermatology Atlas".
- ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Tiglis M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinTescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.




![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/f/fc/Lichen_planus02.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/8/86/Lichen_planus03.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/8/87/Lichen_planus04.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/4/41/Lichen_planus08.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/5/5d/Lichen_planus10.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/04/Lichen_planus12.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/ad/Lichen_planus13.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/02/Lichen_planus14.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/a3/Lichen_planus17.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/3/33/Lichen_planus25.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/0a/Lichen_planus30.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/77/Lichen_planus33.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/14/Lichen_planus01.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/f/f9/Lichen_planus05.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/b8/Lichen_planus06.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/a1/Lichen_planus07.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/6/6a/Lichen_planus09.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/12/Lichen_planus11.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/10/Lichen_planus15.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/4/45/Lichen_planus16.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/1a/Lichen_planus18.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/bc/Lichen_planus19.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/2/29/Lichen_planus20.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/a5/Lichen_planus21.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/5/53/Lichen_planus22.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/a5/Lichen_planus23.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/ae/Lichen_planus24.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/c/c1/Lichen_planus26.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/5/56/Lichen_planus27.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/b2/Lichen_planus29.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/bf/Lichen_planus31.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/f/f4/Lichen_planus32.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/3/30/Lichen_planus41.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/e/e8/Lichen_planus42.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/a/af/Lichen_planus43.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/d/da/Lichen_planus44.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/0d/Lichen_planus45.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/f/f7/Lichen_planus46.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/79/Lichen_planus47.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/78/Lichen_planus48.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/d/db/Lichen_planus49.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/e/eb/Lichen_planus50.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/71/Lichen_planus51.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/8/86/Lichen_planus56.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/3/35/Lichen_planus57.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/4/40/Lichen_planus58.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/73/Lichen_planus59.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/9/91/Lichen_planus60.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/2/24/Lichen_planus61.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/0b/Lichen_planus62.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/7/7a/Lichen_planus63.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/8/86/Lichen_planus64.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/b0/Lichen_planus65.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/b/b4/Lichen_planus66.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/2/23/Lichen_planus34.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/04/Lichen_planus52.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/0/0f/Lichen_planus53.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/d/d5/Lichen_planus54.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/9/97/Lichen_planus55.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/d/dc/Lichen_planus68.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/1b/Lichen_planus69.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/8/8a/Lichen_planus70.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/d/d5/Lichen_planus71.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/1/16/Lichen_planus67.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/0/05/Lichen_planus_actinicus01.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/9/96/Lichen_planus_actinicus04.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/b/b6/Lichen_planus_actinicus02.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/2/2c/Lichen_planus_actinicus03.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/1/17/Lichen_planus_actinicus05.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/8/8d/Lichen_planus_actinicus06.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/b/b8/Lichen_planus_actinicus07.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/2/22/Lichen_planus_actinicus08.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/6/6d/Lichen_planus_actinicus09.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/5/57/Lichen_planus_actinicus10.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/f/fd/Lichen_planus_actinicus11.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/a/a7/Lichen_planus_actinicus12.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/7/79/Lichen_planus_actinicus13.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/8/8a/Lichen_planus_actinicus14.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/4/45/Lichen_planus_actinicus15.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/d/d5/Lichen_planus_actinicus16.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/e/ed/Lichen_planus_actinicus17.jpg)
![Lichen planus actinicus. Adapted from Dermatology Atlas.[1]](/images/1/1a/Lichen_planus_actinicus19.jpg)
![Lichen planus annular. Adapted from Dermatology Atlas.[1]](/images/d/dc/Lichen_planus_annular03.jpg)
![Lichen planus annular. Adapted from Dermatology Atlas.[1]](/images/1/12/Lichen_planus_annular04.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/2/25/Lichen_planus_follicularis01.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/2/26/Lichen_planus_follicularis02.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/7/7b/Lichen_planus_follicularis03.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/6/65/Lichen_planus_follicularis04.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/1/19/Lichen_planus_follicularis05.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/a/a3/Lichen_planus_follicularis06.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/c/c5/Lichen_planus_follicularis07.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/6/66/Lichen_planus_follicularis08.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/e/ee/Lichen_planus_follicularis18.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/6/62/Lichen_planus_follicularis09.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/a/a2/Lichen_planus_follicularis11.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/c/c7/Lichen_planus_follicularis12.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/f/f0/Lichen_planus_follicularis13.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/d/d4/Lichen_planus_follicularis14.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/1/1f/Lichen_planus_follicularis15.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/2/23/Lichen_planus_follicularis16.jpg)
![Lichen planus follicularis. Adapted from Dermatology Atlas.[1]](/images/7/74/Lichen_planus_follicularis17.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/e/e3/Lichen_planus_linearis04.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/1/1b/Lichen_planus_linearis12.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/3/31/Lichen_planus_linearis01.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/5/51/Lichen_planus_linearis02.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/2/27/Lichen_planus_linearis06.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/e/ed/Lichen_planus_linearis07.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/1/1a/Lichen_planus_linearis08.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/f/f1/Lichen_planus_linearis09.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/4/41/Lichen_planus_linearis03.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/2/24/Lichen_planus_linearis05.jpg)
![Lichen planus linearis. Adapted from Dermatology Atlas.[1]](/images/3/30/Lichen_planus_linearis10.jpg)
![Lichen planus verrucosus . Adapted from Dermatology Atlas.[1]](/images/6/6f/Lichen_planus_verrucosus01.jpg)
![Lichen planus verrucosus . Adapted from Dermatology Atlas.[1]](/images/8/87/Lichen_planus_verrucosus02.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/1/12/Lichen_planus_vesicular01.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/4/41/Lichen_planus_vesicular02.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/6/6e/Lichen_planus_vesicular03.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/a/a1/Lichen_planus_vesicular08.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/5/51/Lichen_planus_vesicular09.jpg)
![Lichen planus vesicular. Adapted from Dermatology Atlas.[1]](/images/d/d0/Lichen_planus_vesicular04.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/b/bc/Lichen_planus_vesicular05.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/f/f2/Lichen_planus_vesicular06.jpg)
![Lichen planus vesicular. Adapted from Dermatology Atlas.[1]](/images/7/73/Lichen_planus_vesicular07.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/b/bd/Lichen_planus_vesicular10.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/2/2c/Lichen_planus_vesicular11.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/f/f6/Lichen_planus_vesicular12.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/3/39/Lichen_planus_vesicular13.jpg)
![Lichen planus vesicular . Adapted from Dermatology Atlas.[1]](/images/7/73/Lichen_planus_vesicular14.jpg)
![Mucosal lichen planus. Adapted from Dermatology Atlas.[1]](/images/9/99/Mucosal_lichen_planus01.jpg)
![Mucosal lichen planus . Adapted from Dermatology Atlas.[1]](/images/0/00/Mucosal_lichen_planus02.jpg)
![Mucosal lichen planus . Adapted from Dermatology Atlas.[1]](/images/a/a2/Mucosal_lichen_planus03.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/e/e6/Lichen_planus35.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/5/5c/Lichen_planus36.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/4/41/Lichen_planus37.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/c/c7/Lichen_planus39.jpg)
![Lichen planus. Adapted from Dermatology Atlas.[1]](/images/2/2e/Lichen_planus40.jpg)