Intertrigo
|
WikiDoc Resources for Intertrigo |
|
Articles |
|---|
|
Most recent articles on Intertrigo |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Intertrigo at Clinical Trials.gov Clinical Trials on Intertrigo at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Intertrigo
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Intertrigo Discussion groups on Intertrigo Patient Handouts on Intertrigo Directions to Hospitals Treating Intertrigo Risk calculators and risk factors for Intertrigo
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Intertrigo |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
An intertrigo is an inflammation (rash) of the body folds (adjacent areas of skin).
An intertrigo sometimes refers to a bacterial, fungal, or viral infection that has developed at the site of broken skin due to such inflammation.
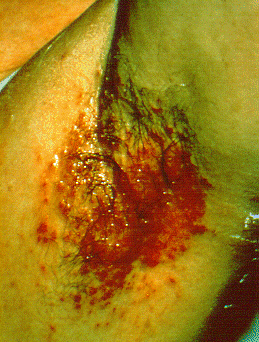
An intertrigo usually develops from the chafing of warm, moist skin in the areas of the inner thighs and genitalia, the armpits, under the breasts, the underside of the belly, behind the ears, and the web spaces between the toes and fingers. An intertrigo usually appears red and raw-looking, and may also itch, ooze, and be sore. Intertrigos occur more often among overweight individuals, those with diabetes, those restricted to bed rest or diaper use, and those who use medical devices, like artificial limbs, that trap moisture against the skin. Also, there are several skin diseases that can cause an intertrigo to develop, such as dermatitis or inverse psoriasis.
Differentiating intertrigo from other diseases
Intertrigo should be differentiated from other diseases causing papulosquamous or erythmatosquamous rash. The differentials include:
| Disease | Rash Characteristics | Signs and Symptoms | Associated Conditions | Images |
|---|---|---|---|---|
| Cutaneous T cell lymphoma/Mycosis fungoides[1] |
|
|
||
| Pityriasis rosea[2] |
|
|
||
| Pityriasis lichenoides chronica |
|
|
||
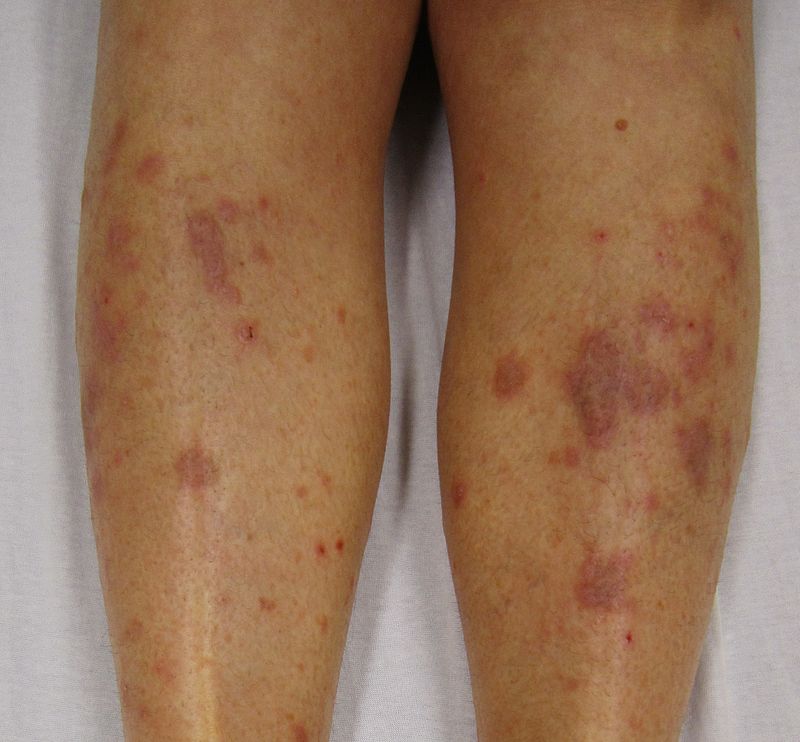
| Nummular dermatitis[5] |
|
|
|
|
| Secondary syphilis[6] |
|
|||
| Bowen’s disease[7] |
|
|
||
| Exanthematous pustulosis[9] |
|
|
||
| Hypertrophic lichen planus[11] |
|
|
|
|
| Sneddon–Wilkinson disease[13] |
|
|
||
| Small plaque parapsoriasis[17] |
|
|
|
|
| Intertrigo[19] |
|
|
||
| Langerhans cell histiocytosis[20] |
|
|
|
|
| Tinea manuum/pedum/capitis[24] |
|
|
|
|
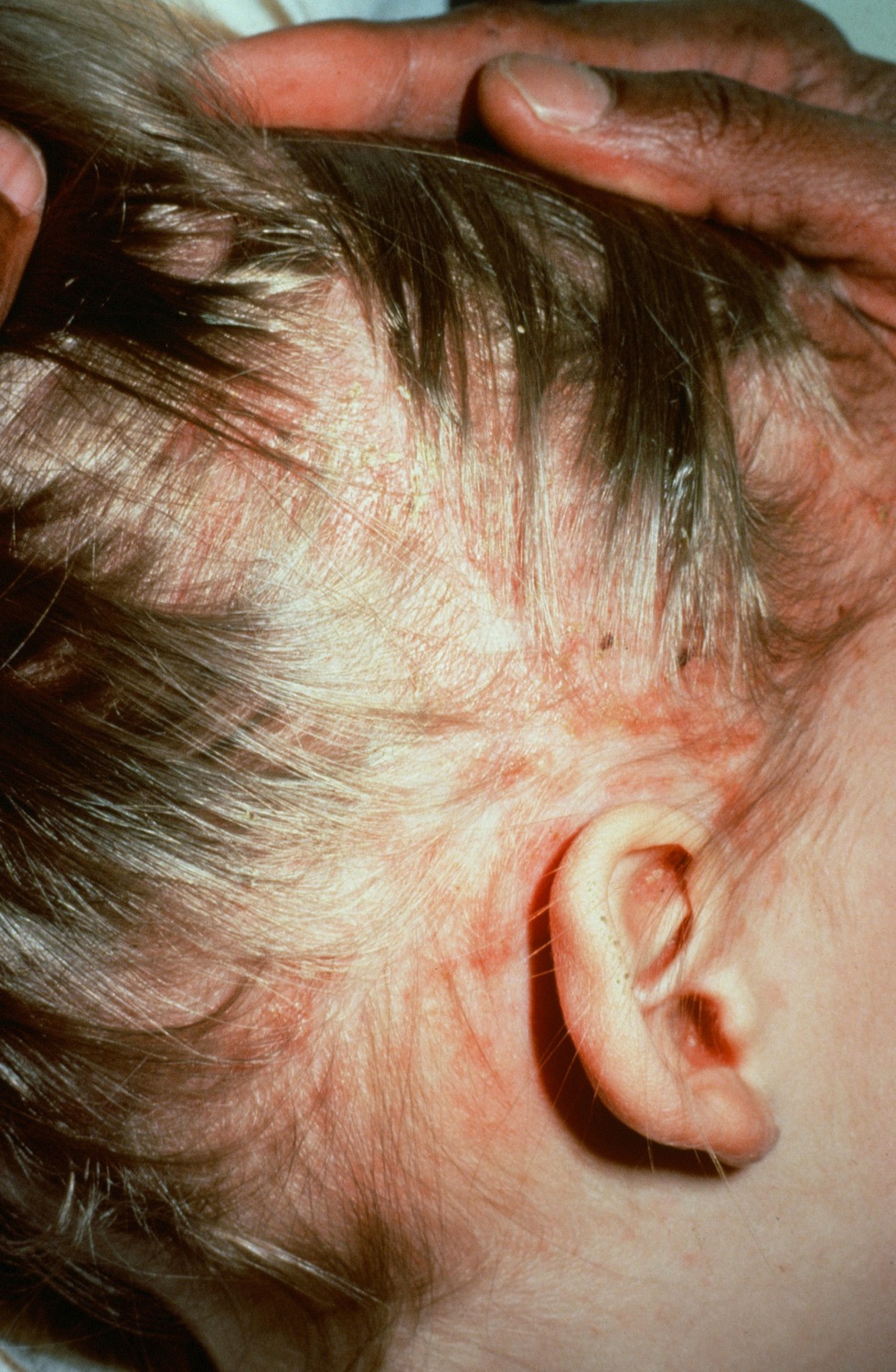
| Seborrheic dermatitis |
|
|
Treatments
In general, treatment for all skin rashes, less is more, and consult a dermatologist if it persists for more than a week. Infections can be treated with a topical and/or oral medication(s). The most common treatment being a baby diaper rash ointment such as a topical zinc oxide cream. Some commonly available over the counter brand names: Sudocrem, Desitin, Butt Paste, and Balmex. There are also many other generic diaper rash creams that may work. Also for a persistent intertrigo infection it is common for an anti-fungal cream, most commonly clotrimazole 1%, to be used in conjunction with a diaper rash ointment.
It is suggested to use a paper towel to apply the zinc oxide cream and/or anti-fungal ointment(s) to avoid excessive hand washing, as it is very difficult to wash zinc oxide ointment from the hands because it resists water. Other ingredients in baby rash ointments that are beneficial to relief of intertrigo is cod liver oil and shark liver oil. These oils are also available in pill forms that may also help the infection (see links).
Hydrocortisone available at drug stores and over the counter in low dosages is beneficial in relieving the pain and symptoms of the infection but does not cure the infection.
Keeping the area of the intertrigo dry and exposed to the air can help prevent recurrences. If the individual is overweight, losing weight can help. Using antibacterial soap, surrounding the skin with absorbent cotton or a band of cotton fabric, and treating the skin with absorbent body powders and even antiperspirants will all help prevent future occurrences. Relapses of intertrigos are common, however, and require periodic care from a dermatologist.
Prescription Medicines
These prescriptions are very dangerous and are usually only prescribed by a doctor for extreme cases.
See also
External links
- A.O.C.D.: Intertrigo
- eMedicine: Intertrigo (by Samuel Selden, M.D.)
- DERMAdoctor: Intertrigo (by Audrey Kunin, M.D.)
Template:WH Template:WikiDoc Sources
- ↑ "Mycosis Fungoides and the Sézary Syndrome Treatment (PDQ®)—Patient Version - National Cancer Institute".
- ↑ Mahajan K, Relhan V, Relhan AK, Garg VK (2016). "Pityriasis Rosea: An Update on Etiopathogenesis and Management of Difficult Aspects". Indian J Dermatol. 61 (4): 375–84. doi:10.4103/0019-5154.185699. PMC 4966395. PMID 27512182.
- ↑ Prantsidis A, Rigopoulos D, Papatheodorou G, Menounos P, Gregoriou S, Alexiou-Mousatou I, Katsambas A (2009). "Detection of human herpesvirus 8 in the skin of patients with pityriasis rosea". Acta Derm. Venereol. 89 (6): 604–6. doi:10.2340/00015555-0703. PMID 19997691.
- ↑ Smith KJ, Nelson A, Skelton H, Yeager J, Wagner KF (1997). "Pityriasis lichenoides et varioliformis acuta in HIV-1+ patients: a marker of early stage disease. The Military Medical Consortium for the Advancement of Retroviral Research (MMCARR)". Int. J. Dermatol. 36 (2): 104–9. PMID 9109005.
- ↑ Jiamton S, Tangjaturonrusamee C, Kulthanan K (2013). "Clinical features and aggravating factors in nummular eczema in Thais". Asian Pac. J. Allergy Immunol. 31 (1): 36–42. PMID 23517392.
- ↑ "STD Facts - Syphilis".
- ↑ Neagu TP, Ţigliş M, Botezatu D, Enache V, Cobilinschi CO, Vâlcea-Precup MS, GrinŢescu IM (2017). "Clinical, histological and therapeutic features of Bowen's disease". Rom J Morphol Embryol. 58 (1): 33–40. PMID 28523295.
- ↑ Murao K, Yoshioka R, Kubo Y (2014). "Human papillomavirus infection in Bowen disease: negative p53 expression, not p16(INK4a) overexpression, is correlated with human papillomavirus-associated Bowen disease". J. Dermatol. 41 (10): 878–84. doi:10.1111/1346-8138.12613. PMID 25201325.
- ↑ Szatkowski J, Schwartz RA (2015). "Acute generalized exanthematous pustulosis (AGEP): A review and update". J. Am. Acad. Dermatol. 73 (5): 843–8. doi:10.1016/j.jaad.2015.07.017. PMID 26354880.
- ↑ Schmid S, Kuechler PC, Britschgi M, Steiner UC, Yawalkar N, Limat A, Baltensperger K, Braathen L, Pichler WJ (2002). "Acute generalized exanthematous pustulosis: role of cytotoxic T cells in pustule formation". Am. J. Pathol. 161 (6): 2079–86. doi:10.1016/S0002-9440(10)64486-0. PMC 1850901. PMID 12466124.
- ↑ Ankad BS, Beergouder SL (2016). "Hypertrophic lichen planus versus prurigo nodularis: a dermoscopic perspective". Dermatol Pract Concept. 6 (2): 9–15. doi:10.5826/dpc.0602a03. PMC 4866621. PMID 27222766.
- ↑ Shengyuan L, Songpo Y, Wen W, Wenjing T, Haitao Z, Binyou W (2009). "Hepatitis C virus and lichen planus: a reciprocal association determined by a meta-analysis". Arch Dermatol. 145 (9): 1040–7. doi:10.1001/archdermatol.2009.200. PMID 19770446.
- ↑ Lutz ME, Daoud MS, McEvoy MT, Gibson LE (1998). "Subcorneal pustular dermatosis: a clinical study of ten patients". Cutis. 61 (4): 203–8. PMID 9564592.
- ↑ Kasha EE, Epinette WW (1988). "Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) in association with a monoclonal IgA gammopathy: a report and review of the literature". J. Am. Acad. Dermatol. 19 (5 Pt 1): 854–8. PMID 3056995.
- ↑ Delaporte E, Colombel JF, Nguyen-Mailfer C, Piette F, Cortot A, Bergoend H (1992). "Subcorneal pustular dermatosis in a patient with Crohn's disease". Acta Derm. Venereol. 72 (4): 301–2. PMID 1357895.
- ↑ Sauder MB, Glassman SJ (2013). "Palmoplantar subcorneal pustular dermatosis following adalimumab therapy for rheumatoid arthritis". Int. J. Dermatol. 52 (5): 624–8. doi:10.1111/j.1365-4632.2012.05707.x. PMID 23489057.
- ↑ Lambert WC, Everett MA (1981). "The nosology of parapsoriasis". J. Am. Acad. Dermatol. 5 (4): 373–95. PMID 7026622.
- ↑ Väkevä L, Sarna S, Vaalasti A, Pukkala E, Kariniemi AL, Ranki A (2005). "A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides". Acta Derm. Venereol. 85 (4): 318–23. doi:10.1080/00015550510030087. PMID 16191852.
- ↑ Janniger CK, Schwartz RA, Szepietowski JC, Reich A (2005). "Intertrigo and common secondary skin infections". Am Fam Physician. 72 (5): 833–8. PMID 16156342.
- ↑ Satter EK, High WA (2008). "Langerhans cell histiocytosis: a review of the current recommendations of the Histiocyte Society". Pediatr Dermatol. 25 (3): 291–5. doi:10.1111/j.1525-1470.2008.00669.x. PMID 18577030.
- ↑ Stull MA, Kransdorf MJ, Devaney KO (1992). "Langerhans cell histiocytosis of bone". Radiographics. 12 (4): 801–23. doi:10.1148/radiographics.12.4.1636041. PMID 1636041.
- ↑ Sholl LM, Hornick JL, Pinkus JL, Pinkus GS, Padera RF (2007). "Immunohistochemical analysis of langerin in langerhans cell histiocytosis and pulmonary inflammatory and infectious diseases". Am. J. Surg. Pathol. 31 (6): 947–52. doi:10.1097/01.pas.0000249443.82971.bb. PMID 17527085.
- ↑ Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H (2006). "Risk factors for diabetes insipidus in langerhans cell histiocytosis". Pediatr Blood Cancer. 46 (2): 228–33. doi:10.1002/pbc.20425. PMID 16047354.
- ↑ Al Hasan M, Fitzgerald SM, Saoudian M, Krishnaswamy G (2004). "Dermatology for the practicing allergist: Tinea pedis and its complications". Clin Mol Allergy. 2 (1): 5. doi:10.1186/1476-7961-2-5. PMC 419368. PMID 15050029.
- ↑ Schwartz RA, Janusz CA, Janniger CK (2006). "Seborrheic dermatitis: an overview". Am Fam Physician. 74 (1): 125–30. PMID 16848386.
- ↑ Misery L, Touboul S, Vinçot C, Dutray S, Rolland-Jacob G, Consoli SG, Farcet Y, Feton-Danou N, Cardinaud F, Callot V, De La Chapelle C, Pomey-Rey D, Consoli SM (2007). "[Stress and seborrheic dermatitis]". Ann Dermatol Venereol (in French). 134 (11): 833–7. PMID 18033062.