Betrixaban
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Allison Tu [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete Boxed Warning.
|
Overview
Betrixaban is a factor Xa inhibitor that is FDA approved for the prophylaxis of venous thromboembolism (VTE) in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications due to moderate or severe restricted mobility and other risk factors for VTE. There is a Black Box Warning for this drug as shown here. Common adverse reactions include urinary tract infection, constipation, and hypokalemia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Betrixaban is indicated for the prophylaxis of venous thromboembolism (VTE) in adult patients hospitalized for an acute medical illness who are at risk for thromboembolic complications due to moderate or severe restricted mobility and other risk factors for VTE.
The safety and effectiveness of betrixaban have not been established in patients with prosthetic heart valves because this population has not been studied.
Dosing Information
- The recommended dose of betrixaban is an initial single dose of 160 mg, followed by 80 mg once daily. Daily oral doses should be given at the same time of day with food.
- The recommended duration of treatment is 35 to 42 days.
- Severe Renal Impairment
- For patients with severe renal impairment, (CrCl ≥ 15 to < 30 mL/min computed by Cockcroft-Gault using actual body weight) the recommended dose of betrixaban is an initial single dose of 80 mg followed by 40 mg once daily.
- The recommended duration of treatment is 35 to 42 days.
- Use with P-gp Inhibitors
- For patients receiving or starting concomitant P-gp inhibitors, the recommended dose of betrixaban is an initial single dose of 80 mg followed by 40 mg once daily.
- The recommended duration of treatment is 35 to 42 days.
- Missed Dose
- If a dose of betrixaban is not taken at the scheduled time, the dose should be taken as soon as possible on the same day.
- The betrixaban dose should not be doubled to make up for a missed dose.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of betrixaban in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of betrixaban in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding FDA-Labeled Indications and Dosage of betrixaban in pediatric patients.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of betrixaban in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use ofbetrixaban in pediatric patients.
Contraindications
Betrixaban is contraindicated in patients with:
- Active pathological bleeding
- Severe hypersensitivity reaction to betrixaban
Warnings
|
SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete Boxed Warning.
|
- Risk of Bleeding
- Betrixaban increases the risk of bleeding and can cause serious and potentially fatal bleeding. Promptly evaluate any signs or symptoms of blood loss.
- Concomitant use of drugs affecting hemostasis increases the risk of bleeding. These include aspirin and other antiplatelet agents, other anticoagulants, heparin, thrombolytic agents, selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors, and nonsteroidal anti-inflammatory drugs (NSAIDs).
- Advise patients of signs and symptoms of blood loss and to report them immediately and seek emergency care. Promptly evaluate any signs or symptoms of blood loss and consider the need for blood replacement. Discontinue betrixaban in patients with active pathological bleeding.
- There is no established way to reverse the anticoagulant effect of betrixaban, which can be expected to persist for at least 72 hours after the last dose.
- It is unknown whether hemodialysis removes betrixaban. Protamine sulfate, vitamin K, and tranexamic acid are not expected to reverse the anticoagulant activity of betrixaban.
- Spinal/Epidural Anesthesia or Puncture
- When neuraxial anesthesia (spinal/epidural anesthesia) or spinal/epidural puncture is employed, patients treated with antithrombotic agents for prevention of thromboembolic complications are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis.
- Do not remove an epidural catheter earlier than 72 hours after the last administration of betrixaban. Do not administer the next betrixaban dose earlier than 5 hours after the removal of the catheter.
- If traumatic puncture occurs, delay the administration of betrixaban for 72 hours.
- Monitor patients frequently for signs and symptoms of neurological impairment (e.g., numbness or weakness of the legs, bowel or bladder dysfunction).
- If neurological compromise is noted, urgent diagnosis and treatment is necessary. Prior to neuraxial intervention, consider the potential benefit versus the risk in anticoagulated patients or in patients to be anticoagulated for thromboprophylaxis.
- Use in Patients with Severe Renal Impairment
- Patients with severe renal impairment (CrCl ≥ 15 to < 30 mL/min computed by Cockcroft-Gault using actual body weight) taking betrixaban may have an increased risk of bleeding events.
- Reduce dose of betrixaban, monitor patients closely, and promptly evaluate any signs or symptoms of blood loss in these patients.
- Use in Patients on Concomitant P-gp Inhibitors
- Patients on concomitant P-gp inhibitors with betrixaban may have an increased risk of bleeding. Reduce dose of betrixaban in patients receiving or starting P-gp inhibitors. Monitor patients closely and promptly evaluate any signs or symptoms of blood loss in these patients.
- Avoid use of betrixaban in patients with severe renal impairment receiving concomitant P-gp inhibitors.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of betrixaban was evaluated in the Acute Medically Ill Prevention with Extended Duration Betrixaban (APEX) Study, including 3,716 patients treated with betrixaban for a median of 36 days compared to 3,716 patients treated with enoxaparin for a median of 9 days. Patients in both treatment groups were followed for safety, including bleeding events, for up to 77 days.
Patients randomized to the betrixaban arm received betrixaban 160 mg orally on Day 1, then 80 mg once daily for 35 to 42 days AND enoxaparin subcutaneous placebo once daily for 6 to 14 days. Patients randomized to the enoxaparin arm received enoxaparin 40 mg subcutaneously once daily for 6 to 14 days AND betrixaban placebo orally once daily for 35 to 42 days.
Patients with severe renal impairment (creatinine clearance ≥ 15 and < 30 mL/min) received reduced doses of study medications (betrixaban 80 mg loading dose, then 40 mg once daily or enoxaparin 20 mg once daily) along with corresponding placebo.
Patients taking a concomitant P-gp inhibitor received betrixaban 80 mg loading dose, then 40 mg once daily or enoxaparin 40 mg subcutaneously once daily for 6 to 14 days along with corresponding placebo.
The most common adverse reactions with betrixaban were related to bleeding (> 5%) with major bleeding occurring in less than 1% of patients.
Overall, 54% of patients receiving betrixaban experienced at least one adverse reaction vs. 52% with enoxaparin. The frequency of patients reporting serious adverse reactions was similar between betrixaban (18%) and enoxaparin (17%). In the APEX trial, the most frequent reason for treatment discontinuation was bleeding, with an incidence rate of 2.4% for betrixaban vs. 1.2% for enoxaparin.
The primary and secondary safety outcomes in APEX were bleeding-related events.
A summary of major and clinically relevant non-major (CRNM) bleeding events in the overall safety population is shown in Table 1. Most CRNM events (86%) were mild to moderate in severity, and the majority (62%) did not require medical intervention.
The incidence of fatal bleeding was the same in the betrixaban and enoxaparin treatment groups (1 in each group).

A summary of major and CRNM bleeding events by dose is shown in Table 2 and Table 3.


The most common adverse reactions occurring in ≥ 2% of patients are shown in Table 4.

Other Adverse Reactions
- Hypersensitivity reactions: one patient experienced a serious adverse reaction of moderate hypersensitivity
Postmarketing Experience
There is limited information regarding Betrixaban Postmarketing Experience in the drug label.
Drug Interactions
Inhibitors of P-gp
Betrixaban is a substrate of P-gp and concomitant use of P-gp inhibitors (e.g., amiodarone, azithromycin, verapamil, ketoconazole, clarithromycin) results in an increased exposure of betrixaban.
Reduce the dose of betrixaban for patients receiving or starting concomitant P-gp inhibitors.
Anticoagulants, Antiplatelets, and Thrombolytics
Co-administration of anticoagulants, antiplatelet drugs, and thrombolytics may increase the risk of bleeding. Promptly evaluate any signs or symptoms of blood loss if patients are treated concomitantly with anticoagulants, aspirin, other platelet aggregation inhibitors, and/or NSAIDs.
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): Risk Summary
There are no data with the use of betrixaban in pregnant women, but treatment is likely to increase the risk of hemorrhage during pregnancy and delivery. Betrixaban was studied in reproductive and developmental toxicology studies in rats and rabbits during the period of organogenesis at exposures up to 44 times the recommended clinical dose of 80 mg daily. Although betrixaban was not associated with adverse developmental fetal outcomes in animals, maternal toxicity (i.e., hemorrhage) was identified in these studies. Betrixaban should be used during pregnancy only if the potential benefit outweighs the potential risk to the mother and fetus.
Adverse outcomes in pregnancy occur regardless of the health of the mother or the use of medications. The background risk of major birth defects and miscarriage for the indicated population is unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Data
Animal Data
Embryo-fetal development studies were conducted in pregnant rats and rabbits during the period of organogenesis. In rats, no adverse embryofetal or teratogenic effects were seen when betrixaban was administered orally at doses up to 200 mg/kg/day, or 44 times the human dose of 80 mg/day when based on AUC. In rabbits, no adverse embryofetal or teratogenic effects were seen at doses up to 45 mg/kg/day, or 35 times the human exposure at a dose of 80 mg/day when based on AUC. Pregnant rabbits administered the highest dose of 150 mg/kg/day were terminated prematurely due to excessive maternal toxicities. Upon post-mortem examination, early and/or late resorptions and fetal deaths were observed at the 150 mg/kg dose, which may be linked to hemorrhage observed in various organs including the reproductive tract.
In a rat pre-and-post-natal developmental study, betrixaban was administered orally during the period of organogenesis and through lactation day 20 at doses up to 200 mg/kg/day. Maternal toxicities (including decreased body weight gain and food consumption and red/brown perivaginal substance) were observed at 200 mg/kg/day, which is approximately 44 times the human exposure when based on AUC. At a maternal dose up to 200 mg/kg/day, betrixaban did not have adverse effects on sexual maturation, reproductive performance, and behavioral development of the F1 generation.
Clinical Considerations
Maternal Adverse Reactions
Treatment is likely to increase the risk of hemorrhage during pregnancy and delivery. Consider the risks of bleeding and of stroke in using betrixaban in this setting.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Betrixaban in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Betrixaban during labor and delivery.
Nursing Mothers
Risk Summary
No data are available regarding the presence of betrixaban or its metabolites in human milk, the effects of the drug on the breast-fed infant, or the effects of the drug on milk production. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for betrixaban and any potential adverse effects on the breast-fed child from betrixaban or from the underlying maternal condition.
Pediatric Use
Safety and effectiveness in pediatric patients have not been established.
Geriatic Use
Of the total number of patients in the APEX clinical study 90% were 65 years and over, while 68.6% were greater than or equal to 75 years. No clinically significant differences in safety or effectiveness were observed between older and younger patients.
Gender
There is no FDA guidance on the use of Betrixaban with respect to specific gender populations.
Race
There is no FDA guidance on the use of Betrixaban with respect to specific racial populations.
Renal Impairment
Patients with severe renal impairment (CrCl ≥ 15 to < 30 mL/min computed by Cockcroft-Gault using actual body weight) may have an increased risk of bleeding events. Reduce the betrixaban dose for patients with severe renal impairment. Monitor patients closely and promptly evaluate any signs or symptoms of blood loss in these patients. No dose adjustment is needed for mild or moderate renal impairment (CrCl > 30 mL/min, computed by Cockcroft-Gault using actual body weight).
Hepatic Impairment
Betrixaban has not been evaluated in patients with hepatic impairment, because these patients may have intrinsic coagulation abnormalities. Therefore, the use of betrixaban is not recommended in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Betrixaban in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Betrixaban in patients who are immunocompromised.
Administration and Monitoring
Administration
The recommended duration of treatment is 35 to 42 days.
Monitoring
There is limited information regarding Betrixaban Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Betrixaban and IV administrations.
Overdosage
Overdose of betrixaban increases the risk of bleeding.
A specific reversal agent for betrixaban is not available. There is no experience with hemodialysis in individuals receiving betrixaban. Protamine sulfate, vitamin K, and tranexamic acid are not expected to reverse the anticoagulant activity of betrixaban.
Pharmacology
Betrixaban
| |
| Systematic (IUPAC) name | |
N-(5-chloropyridin-2-yl)-2-([4-(N,N-dimethylcarbamimidoyl)benzoyl]amino)-5-methoxybenzamide
 | |
| Identifiers | |
| CAS number | |
| ATC code | none |
| PubChem | |
| Chemical data | |
| Formula | Template:OrganicBox atomTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBox atomTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBoxTemplate:OrganicBox |
| Mol. mass | 451.905 g/mol |
| SMILES | & |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status |
Being evaluated in the global Phase 3 trial (APEX) |
| Routes | ? |
Mechanism of Action
Betrixaban is an oral FXa inhibitor that selectively blocks the active site of FXa and does not require a cofactor (such as Anti-thrombin III) for activity. Betrixaban inhibits free FXa and prothrombinase activity. By directly inhibiting FXa, betrixaban decreases thrombin generation (TG). Betrixaban has no direct effect on platelet aggregation.
Structure
Betrixaban, a factor Xa (FXa) inhibitor, is chemically described as N-(5-chloropyridin-2-yl)-2-[4-(N,N-dimethylcarbamimidoyl)-benzoylamino]-5-methoxybenzamide maleate. Its molecular formula (as maleate salt) is C27H26ClN5O7, which corresponds to a molecular weight of 567.98. Betrixaban (maleate salt) has the following structural formula:

Pharmacodynamics
Inhibition of FXa by betrixaban results in an inhibition of thrombin generation at clinically relevant concentrations, and the maximum inhibition of thrombin generation coincides with the time of peak betrixaban concentrations.
Cardiac Electrophysiology
In a study that evaluated the effect of betrixaban on the QT interval, a concentration-dependent increase in the QTc interval was observed. Based on the observed concentration-QTc relationship a mean (upper 95% CI) QTc prolongation of 4 ms (5 ms) is predicted for 80 mg betrixaban and 13 ms (16 ms) for a 4.7-fold increase in exposure.
Pharmacokinetics
Within the anticipated therapeutic dose range, a two-fold increase in dose resulted in a three-fold increase in exposure in the single ascending dose study. A two-fold increase in betrixaban exposure was observed after repeat dosing, and the time to steady-state is 6 days (without an initial loading dose).
Absorption
The oral bioavailability of betrixaban for an 80 mg dose is 34%, and peak concentrations occurred within 3 to 4 hours. Betrixaban is also a substrate of P-gp.
Effect of Food
When administered with a low-fat (900 calories, 20% fat) or high-fat (900 calories, 60% fat) meal, Cmax and AUC were reduced as compared to the fasting state by an average of 70% and 61% for low-fat and 50% and 48% for high-fat, respectively. The effect of food on betrixaban PK could be observed for up to 6 hours after meal intake.
Distribution
The apparent volume of distribution is 32 L/kg. In vitro plasma protein binding is 60%.
Elimination
The effective half-life of betrixaban is 19 to 27 hours.
Unchanged betrixaban is the predominant component found in human plasma. Two inactive major metabolites formed by CYP-independent hydrolysis comprise the other components in plasma, accounting for 15 to 18% of the circulating drug-related material. Less than 1% of the minor metabolites could be formed via metabolism by the following CYP enzymes; CYP1A1, CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, and CYP3A4.
Excretion
Following oral administration of radio-labeled betrixaban approximately 85% of the administered compound was recovered in the feces and 11% recovered in the urine. In a study of intravenous betrixaban, a median value of 17.8% of the absorbed dose was observed as unchanged betrixaban in urine.
Specific Populations
Male and Female Patients
No clinically significant changes in betrixaban pharmacokinetics were observed between males and females.
Patients with Renal Impairment
In a dedicated renal impairment study mean AUC0-24 on day 8 was increased by 1.89, 2.27 and 2.63-fold in mild (eGFRMDRD ≥ 60 to < 90 mL/min/1.73 m2), moderate (eGFRMDRD ≥ 30 to < 60 mL/min/1.73 m2) and severe (eGFRMDRD ≥ 15 to < 30 mL/min/1.73 m2) renal impaired patients respectively compared to healthy volunteers.
Patients with Hepatic Impairment
Studies with betrixaban in patients with hepatic impairment have not been conducted and the impact of hepatic impairment on the exposure to betrixaban has not been evaluated.
Drug Interaction Studies
The effects of coadministered drugs on the pharmacokinetics of betrixaban exposure based on drug interaction studies are summarized in Figure 1.

Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with betrixaban have not been performed.
Betrixaban was not mutagenic in bacteria (Ames-Test) or clastogenic in Chinese hamster ovary cells in vitro or in the rat micronucleus test in vivo.
In a study to assess fertility and early embryonic development to implantation, oral doses of betrixaban were administered to male and female rats. There was no evidence that betrixaban up to 150 mg/kg/day adversely affected male or female fertility, reproductive performance, or embryo-fetal viability.
Clinical Studies
The clinical evidence for the effectiveness of betrixaban is derived from the APEX clinical trial [NCT01583218]. APEX was a randomized, double-blind, multinational study comparing extended duration betrixaban (35 to 42 days) to short duration of enoxaparin (6 to 14 days) in the prevention of venous thromboembolic events (VTE) in an acutely medically ill hospitalized population with risk factors for VTE.
Eligible patients included adults who were at least 40 years of age, hospitalized for an acute medical illness, at risk for VTE due to moderate or severe immobility, and had additional risk factors for VTE (described below). Expected duration of hospitalization was at least 3 days and patients were expected to be moderately or severely immobilized for at least 24 hours. The causes for hospitalization included heart failure, respiratory failure, infectious disease, rheumatic disease, or ischemic stroke. At study initiation eligible patients were required to have one of the following additional risk factors for VTE:
- ≥ 75 years of age,
- 60 through 74 years of age with D-dimer ≥ 2 ULN, or
- 40 through 59 years of age with D-dimer ≥ 2 ULN and a history of either VTE or cancer
A total of 7,513 patients were randomized 1:1 to:
- Betrixaban arm (betrixaban 160 mg orally on Day 1, then 80 mg once daily for 35 to 42 days AND enoxaparin subcutaneous placebo once daily for 6 to 14 days),
OR
- Enoxaparin arm (enoxaparin 40 mg subcutaneously once daily for 6 to 14 days AND betrixaban placebo orally once daily for 35 to 42 days).
Patients with severe renal impairment (creatinine clearance ≥ 15 and < 30 mL/min) received reduced doses of study medications (betrixaban 80 mg loading dose, then 40 mg once daily or enoxaparin 20 mg once daily) along with corresponding placebo.
Patients taking a concomitant P-gp inhibitor received betrixaban 80 mg loading dose, then 40 mg once daily or enoxaparin 40 mg subcutaneously once daily for 6 to 14 days along with corresponding placebo.
Baseline characteristics were balanced between the treatment groups. The population was 55% female, 93% White, 2% Black, 0.2% Asian, and 5% others. The most prevalent acute medical illness at hospitalization was acutely decompensated heart failure (45%), followed by acute infection without septic shock (29%), acute respiratory failure (12%), acute ischemic stroke (11%) and acute rheumatic disorders (3%). The mean and median ages were 76.4 and 77 years, respectively, with 68% of patients ≥ 75 years of age, 97% were severely immobilized at study entry, and 62% had D-dimer ≥ 2 × ULN.
While the APEX Study was ongoing (after 35% enrollment), the study was amended to restrict further enrollment to patients ≥ 75 years of age or with D-dimer values ≥ 2 × ULN. The APEX trial excluded patients whose condition required prolonged anticoagulation (e.g., concurrent VTE, atrial fibrillation, cardiac valve prosthesis), were at increased risk of bleeding, had liver dysfunction, were on dual antiplatelet therapy, or patients who had both severe renal insufficiency (CrCl 15-29 ml/min) and required the concomitant use of a P-gp inhibitor.
The efficacy of betrixaban was based upon the composite outcome of the occurrence of any of the following events up to Day 35 visit:
- Asymptomatic proximal Deep Vein Thrombosis (DVT) (detected by ultrasound),
- Symptomatic proximal or distal DVT,
- Non-fatal Pulmonary Embolism (PE), or
- VTE-related death
Efficacy analyses were performed based on the modified Intent-to-Treat (mITT) population. The mITT population consisted of all patients who had taken at least one dose of study drug and who had follow-up assessment data on one or more primary or secondary efficacy outcome components. A total of 7,441 patients (N=3,721 for betrixaban and N=3,720 for enoxaparin) were included in the mITT population.
The efficacy results for the APEX trial are provided in Table 5 below.

For patients with D-dimer ≥ 2 ULN at baseline, the event rate is 5.7% in the betrixaban arm vs. 7.2% in the enoxaparin arm (relative risk = 0.79, 95% CI [0.63, 0.98]).
For patients with D-dimer ≥ 2 ULN at baseline or age ≥ 75 years, the event rate is 4.7% in the betrixaban arm vs. 6.0% in the enoxaparin arm (relative risk = 0.78, 95% CI [0.64, 0.96]).
Results for the primary efficacy analysis for subjects that were stratified at randomization to the 80 mg betrixaban dose group in the mITT population are shown in Table 6 below.
Patients who were randomized to receive 40 mg betrixaban (those with severe renal impairment or receiving P-gp inhibitors), had VTE rates similar to the enoxaparin arm (6 to 14 days followed by placebo) shown in Table 7 below.


How Supplied
Betrixaban capsules are available as listed below.
The 40 mg size 4 capsules are light grey with 40 printed in black, and have a light blue cap with PTLA printed in white.
- Bottles of 100 (NDC 69853-0202-1)
The 80 mg size 2 capsules are light grey with 80 printed in black, and have a blue cap with PTLA printed in white.
- Bottles of 100 (NDC 69853-0201-1)
Storage
Store at room temperature; 20°C to 25°C (68°F to 77°F).
Images
Drug Images
{{#ask: Page Name::Betrixaban |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel


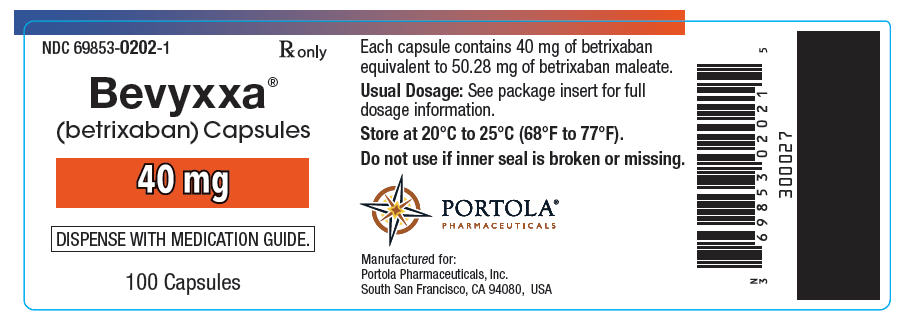

{{#ask: Label Page::Betrixaban |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
- Risk of Bleeding
- Advise patients that it might take longer than usual for bleeding to stop, and that they may bruise or bleed more easily when treated with betrixaban.
- Instruct patients to report any unusual bleeding to their physician.
- Instruct patients to tell their physicians and dentists that they are taking betrixaban, and/or any other products known to affect bleeding (including nonprescription products, such as aspirin or NSAIDs), before any surgery or medical or dental procedure is scheduled and before any new drug is taken.
- Use in Patients with Severe Renal Impairment
- Advise patients that the risk of bleeding is higher in people who have severe kidney problems (severe renal impairment).
- Spinal/Epidural Hematoma
- Advise patients having neuraxial anesthesia or spinal puncture to watch for signs and symptoms of spinal or epidural hematomas, such as numbness or weakness of the legs, or bowel or bladder dysfunction.
- Instruct patients to contact their physician immediately if any of these symptoms occur.
- Pregnancy and Lactation
- Advise female patients to inform their physicians if they are pregnant or plan to become pregnant or are breastfeeding or intend to breastfeed during treatment with betrixaban.
- How to Take Betrixaban
- Instruct patients to take betrixaban with food, and instruct patients on what to do if a dose is missed.
Precautions with Alcohol
Alcohol-Betrixaban interaction has not been established. Talk to your doctor regarding the effects of taking alcohol with this medication.
Brand Names
BEVYXXA
Look-Alike Drug Names
There is limited information regarding Betrixaban Look-Alike Drug Names in the drug label.
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.