Ultrasound


|
WikiDoc Resources for Ultrasound |
|
Articles |
|---|
|
Most recent articles on Ultrasound |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Ultrasound at Clinical Trials.gov Clinical Trials on Ultrasound at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Ultrasound
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Ultrasound Discussion groups on Ultrasound Patient Handouts on Ultrasound Directions to Hospitals Treating Ultrasound Risk calculators and risk factors for Ultrasound
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Ultrasound |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor(s)-in-Chief: C. Michael Gibson, M.S.,M.D. [2] Phone:617-632-7753; Casey Glass, M.D. [3]
Overview
Ultrasound is cyclic sound pressure with a frequency greater than the upper limit of human hearing. Although this limit varies from person to person, it is approximately 20 kilohertz (20,000 hertz) in healthy, young adults and thus, 20 kHz serves as a useful lower limit in describing ultrasound. Ultrasound is manually produced in many different fields, typically to penetrate a medium and measure the reflection signature or supply focused energy. The reflection signature can reveal details about the inner structure of the medium. The most well known application of this technique is its use in sonography to produce pictures of fetuses in the human womb. There are a vast number of other applications as well.
Ability to hear ultrasound
The upper frequency limit in humans (approximately 20 kHz) is caused by the middle ear, which acts as a low-pass filter. If ultrasound is fed directly into the skull bone and reaches the cochlea without passing through the middle ear, much higher frequencies can be heard. This effect is discussed in ultrasonic hearing. Carefully-designed scientific studies have been performed and confirmed what they call the hypersonic effect - that even without consciously hearing it, high-frequency sound can have a measurable effect on the mind.
It is a fact in psychoacoustics that children can hear some high-pitched sounds that older adults cannot hear, because in humans the upper limit pitch of hearing tends to become lower with age.[1] [2] A cell phone company has used this to create ring signals supposedly only able to be heard by younger humans[3]; but many older people claim to be able to hear it, which is likely given the considerable variation of age-related deterioration in the upper hearing threshold.
Some animals – such as dogs, cats, dolphins, bats, and mice have an upper frequency limit that is greater than that of the human ear and thus can hear ultrasound.
Diagnostic sonography
Medical sonography (ultrasonography) is an ultrasound-based diagnostic medical imaging technique used to visualize muscles, tendons, and many internal organs, their size, structure and any pathological lesions with real time tomographic images. It is also used to visualize a fetus during routine and emergency prenatal care. Ultrasound scans are performed by medical health care professionals called sonographers. Obstetric sonography is commonly used during pregnancy. Ultrasound has been used to image the human body for at least 50 years. It is one of the most widely used diagnostic tools in modern medicine. The technology is relatively inexpensive and portable, especially when compared with modalities such as magnetic resonance imaging(MRI) and computed tomography (CT). As currently applied in the medical environment, ultrasound poses no known risks to the patient.[4]

Sonography is generally described as a "safe test" because it does not use ionizing radiation, which imposes hazards, such as cancer production and chromosome breakage. However, ultrasonic energy has two potential physiological effects: it enhances inflammatory response; and it can heat soft tissue.[5] Ultrasound energy produces a mechanical pressure wave through soft tissue. This pressure wave may cause microscopic bubbles in living tissues, and distortion of the cell membrane, influencing ion fluxes and intracellular activity. When ultrasound enters the body, it causes molecular friction and heats the tissues slightly. This effect is very minor as normal tissue perfusion dissipates heat. With high intensity, it can also cause small pockets of gas in body fluids or tissues to expand and contract/collapse in a phenomenon called cavitation (this is not known to occur at diagnostic power levels used by modern diagnostic ultrasound units). The long-term effects of tissue heating and cavitation are not known.[6] There are several studies that indicate the harmful side effects on animal fetuses associated with the use of sonography on pregnant mammals. A noteworthy study in 2006 suggests exposure to ultrasound can affect fetal brain development in mice. This misplacement of brain cells during their development is linked to disorders ranging "from mental retardation and childhood epilepsy to developmental dyslexia, autism spectrum disorders and schizophrenia, the researchers said. [7]

There is no link made yet between the test results on animals, such as mice, and the possible outcome to humans. Widespread clinical use of diagnostic ultrasound testing on humans has not been done for ethical reasons. The possibility exists that biological effects may be identified in the future, currently most doctors feel that based on available information the benefits to patients outweigh the risks.[8] Obstetric ultrasound can be used to identify many conditions that would be harmful to the mother and the baby. For this reason many health care professionals consider that the risk of leaving these conditions undiagnosed is much greater than the very small risk, if any, associated with undergoing the scan. According to Cochrane review, routine ultrasound in early pregnancy (less than 24 weeks) appears to enable better gestational age assessment, earlier detection of multiple pregnancies and earlier detection of clinically unsuspected fetal malformation at a time when termination of pregnancy is possible.[9]
Sonography is used routinely in obstetric appointments during pregnancy, but the FDA discourages its use for non-medical purposes such as fetal keepsake videos and photos, even though it is the same technology used in hospitals.
Obstetric ultrasound is primarily used to:
- Date the pregnancy (gestational age)
- Confirm fetal viability
- Determine location of fetus, intrauterine vs ectopic
- Check the location of the placenta in relation to the cervix
- Check for the number of fetuses (multiple pregnancy)
- Check for major physical abnormalities.
- Assess fetal growth (for evidence of intrauterine growth restriction (IUGR))
- Check for fetal movement and heartbeat.
- Determine the sex of the baby
Unfortunately, results are occasionally wrong, producing a false positive (the Cochrane Collaboration is a relevant effort to improve the reliability of health care trials). False detection may result in patients being warned of birth defects when no such defect exists. Sex determination is only accurate after 12 weeks gestation [Ultrasound in Obstetrics and Gynecology 1999]. When balancing risk and reward, there are recommendations to avoid the use of routine ultrasound for low risk pregnancies [ACOG]. In many countries ultrasound is used routinely in the management of all pregnancies.
According to European Committee of Medical Ultrasound Safety (ECMUS) "Ultrasonic examinations should only be performed by competent personnel who are trained and updated in safety matters. Ultrasound produces heating, pressure changes and mechanical disturbances in tissue. Diagnostic levels of ultrasound can produce temperature rises that are hazardous to sensitive organs and the embryo/fetus. Biological effects of non-thermal origin have been reported in animals but, to date, no such effects have been demonstrated in humans, except when a microbubble contrast agent is present."[10]
A study on rodent fetus brains that are exposed to ultrasound showed signs of damage. Speculation on human fetuses can be in a range of no significant complications to a variety of mental and brain disorders. The study shows that rodent brain cells failed to grow to their proper position and remained scattered in incorrect parts of the brain. The conditions of this experiment are different from typical fetal scanning because of the long dwell times. [National Institute of Neurological Disorders; Proceedings of the National Academy of Sciences]. Care should be taken to use low power settings and avoid pulsed wave scanning of the fetal brain unless specifically indicated in high risk pregnancies.
It should be noted that obstetrics is not the only use of ultrasound. Soft tissue imaging of many other parts of the body is conducted with ultrasound. Other scans routinely conducted are cardiac, renal, liver and gallbladder (hepatic). Other common applications include musculo-skeletal imaging of muscles, ligaments and tendons, ophthalmic ultrasound (eye) scans and superficial structures such as testicle, thyroid, salivary glands and lymph nodes. Because of the real time nature of ultrasound, it is often used to guide interventional procedures such as fine needle aspiration FNA or biopsy of masses for cytology or histology testing in the breast, thyroid, liver, kidney, lymph nodes, muscles and joints.
Ultrasound scanners using pulsed wave and colour Doppler are used to visualize arteries and veins.
Figures released for the period 2005-2006 by UK Government (Department of Health) show that non-obstetric ultrasound examinations contributed to more than 65% of the total number of ultrasound scans conducted.
Biomedical ultrasonic applications
Ultrasound also has therapeutic applications, which can be highly beneficial when used with dosage precautions:[11]
- According to RadiologyInfo [12], ultrasounds are useful in the detection of Pelvic abnormalities and can involve techniques known as abdominal (transabdominal) ultrasound, vaginal (transvaginal or endovaginal) ultrasound in women, and also rectal (transrectal) ultrasound in men.
- Treating benign and malignant tumors and other disorders, via a process known as Focused Ultrasound Surgery (FUS) or HIFU, High Intensity Focused Ultrasound. These procedures generally use lower frequencies than medical diagnostic ultrasound (from 250 kHz to 2000 kHz), but significantly higher time-averaged intensities. The treatment is often guided by MRI, as in Magnetic Resonance guided Focused Ultrasound.
- Therapeutic ultrasound, a technique that uses more powerful ultrasound sources to generate local heating in biological tissue, e.g. in occupational therapy, physical therapy and cancer treatment.
- Delivering chemotherapy to brain cancer cells and various drugs to other tissues, via a process known as Acoustic Targeted Drug Delivery [13] These procedures generally use high frequency ultrasound (from 1 MHz to 10 MHz) and a range of intensities from 0-20 watts/cm2. The acoustic energy is focused on the tissue of interest to agitate its matrix and make it more permeable to therapeutic drugs.[14][15]
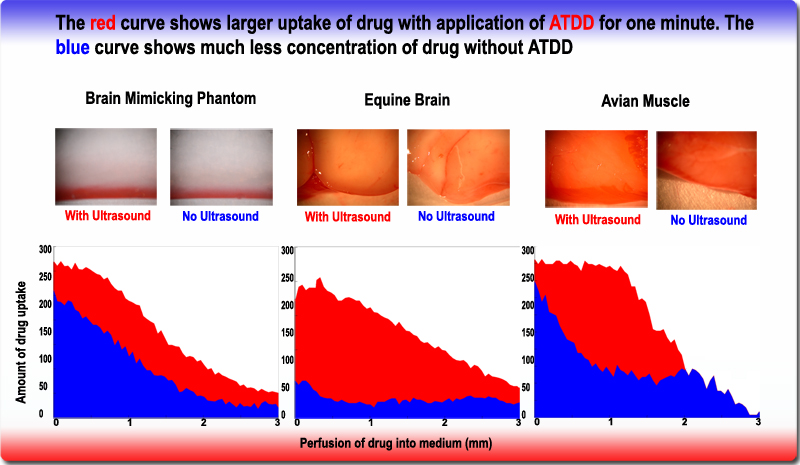
Enhanced drug uptake using Acoustic Targeted Drug Delivery
- Cleaning teeth in dental hygiene.
- Focused ultrasound sources may be used for cataract treatment by phacoemulsification.
- Additional physiological effects of low-intensity ultrasound have recently been discovered, e.g. the ability to stimulate bone-growth and its potential to disrupt the blood-brain barrier for drug delivery.
- Ultrasound is used in UAL (ultrasound-assisted lipectomy), or liposuction.
- Doppler ultrasound is being tested for use in aiding tissue plasminogen activator treatment in stroke sufferers. This procedure is called Ultrasound-Enhanced Systemic Thrombolysis.
- Low intensity pulsed ultrasound is used for therapeutic tooth and bone regeneration.
- Ultrasound can also be used for elastography. This can be useful in medical diagnoses, as elasticity can discern healthy from unhealthy tissue for specific organs/growths. In some cases unhealthy tissue may have a lower system Q, meaning that the system acts more like a large heavy spring as compared to higher values of system Q (healthy tissue) that respond to higher forcing frequencies. Ultrasonic elastography is different from conventional ultrasound, as a transceiver (pair) and a transmitter are used instead of only a transceiver. One transducer (a single element {or array of elements} acts as both the transmitter and receiver to image the region of interest over time. The extra transmitter is a very low frequency transmitter, and perturbs the system so the unhealthy tissue oscillates at a low frequency and the healthy tissue does not. The transceiver, which operates at a high frequency (typically MHz) then measures the displacement of the unhealthy tissue (oscillating at a much lower frequency). The movement of the slowly oscillating tissue is used to determine the elasticity of the material, which can then be used to distinguish healthy tissue from the unhealthy tissue.
- Ultrasound has been shown to act synergistically with antibiotics in bacterial cell killing.[16]
- Ultrasound has been postulated to allow thicker eukaryotic cell tissue cultures by promoting nutrient penetration.Scientific Article
- Ultrasound in the low MHz range in the form of standing waves is an emerging tool for contactless separation, concentration and manipulation of microparticles and biological cells. The basis is the acoustic radiation force, a non-linear effect which causes particles to be attracted to either the nodes or anti-nodes of the standing wave depending on the acoustic contrast factor, which is a function of the sound velocities and densities of the particle and of the medium in which the particle is immersed.
See also
- Acoustics
- Infrasound — sound at extremely low frequencies
- Medical ultrasonography
- Picosecond Ultrasonics
- Sound
- Waves
- Light
References
- ↑ Takeda S et al (1992)
- ↑ "Age variation in the upper limit of hearing".European Journal of Applied Physiology 65(5), 403-408
- ↑ "A Ring Tone Meant to Fall on Deaf Ears" (New York Times article)
- ↑ [1]
- ↑ Watson, T. (2006). "Therapeutic Ultrasound". (see here for a pdf version with the author and date information)
- ↑ http://www.fda.gov/cdrh/radhealth/products/ultrasound-imaging.html
- ↑ http://www.livescience.com/health/060807_ap_baby_ultrasound.html
- ↑ http://www.aium.org/patient/aboutExam/safety.asp
- ↑ "Ultrasound for fetal assessment in early pregnancy".
- ↑ http://www.efsumb.org/efsumb/committees/Safety_Committee/Safety_Eng/Clinical%20Safety%20Statement%202006.pdf
- ↑ Essentials of Medical Ultrasound: A Practical Introduction to the Principles, Techniques and Biomedical Applications, edited by M. H. Rapacholi, Humana Press 1982
- ↑ "Ultrasound - Pelvis".
- ↑ "Acoustic targeted drug delivery in neurological tissue".
- ↑ "A phantom feasibility study of acoustic enhanced drug delivery to neurological tissue".
- ↑ "Acoustics and brain cancer".
- ↑ "Citation list".
af:Ultraklank ast:Ultrasoníu bs:Ultrazvuk bg:Ултразвук cs:Ultrazvuk da:Ultralyd de:Ultraschall et:Ultraheli eo:Ultrasono ko:초음파 hr:Ultrazvuk id:Ultrasonik it:Controllo ultrasonoro he:אולטרה סאונד lt:Ultragarsas hu:Ultrahang nl:Ultrageluid no:Ultralyd nn:Ultralyd simple:Ultrasound sk:Ultrazvuk sl:Ultrazvok fi:Ultraääni sv:Ultraljud ta:மீயொலி th:การตรวจอัลตร้าซาวด์ uk:Ультразвук ur:بالاصوت