Vorapaxar
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Alejandro Lemor, M.D. [2]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Black Box Warning
|
WARNING: BLEEDING RISK
See full prescribing information for complete Boxed Warning.
Bleeding: Do not use vorapaxar in patients with a history of stroke, transient ischemic attack (TIA), or intracranial hemorrhage (ICH); or active pathological bleeding.
Antiplatelet agents, including vorapaxar , increase the risk of bleeding, including ICH and fatal bleeding
|
Overview
Vorapaxar is a platelet aggregation inhibitor that is FDA approved for the prophylaxis of thrombotic cardiovascular events in patients with a history of myocardial infarction (MI) or with peripheral arterial disease (PAD). There is a Black Box Warning for this drug as shown here. Common adverse reactions include bleeding, anemia.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Thromboprophylaxis in Patients with History of Myocardial Infarction (MI) or with Peripheral Arterial Disease (PAD)
- Dosing Information
- 1 tablet of 2.08 mg PO once daily, with or without food.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Vorapaxar in adult patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Vorapaxar in adult patients.
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
There is limited information regarding Vorapaxar FDA-Labeled Indications and Dosage (Pediatric) in the drug label.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Vorapaxar in pediatric patients.
Non–Guideline-Supported Use
There is limited information regarding Off-Label Non–Guideline-Supported Use of Vorapaxar in pediatric patients.
Contraindications
History of Stroke, Transient Ischemic Attack (TIA), or Intracranial Hemorrhage (ICH)
- Vorapaxar is contraindicated in patients with a history of stroke, TIA, or ICH because of an increased risk of ICH in this population.
- Discontinue vorapaxar in patients who experience a stroke, TIA, or ICH.
Active Pathologic Bleeding
- Vorapaxar is contraindicated in patients with active pathological bleeding such as ICH or peptic ulcer.
Warnings
|
WARNING: BLEEDING RISK
See full prescribing information for complete Boxed Warning.
Bleeding: Do not use vorapaxar in patients with a history of stroke, transient ischemic attack (TIA), or intracranial hemorrhage (ICH); or active pathological bleeding.
Antiplatelet agents, including vorapaxar , increase the risk of bleeding, including ICH and fatal bleeding
|
General Risk of Bleeding
- Antiplatelet agents, including vorapaxar, increase the risk of bleeding, including ICHand fatal bleeding.
- Vorapaxar increases the risk of bleeding in proportion to the patient's underlying bleeding risk.
- Consider the underlying risk of bleeding before initiating vorapaxar. General risk factors for bleeding include older age, low body weight, reduced renal or hepatic function, history of bleeding disorders, and use of certain concomitant medications (e.g., anticoagulants, fibrinolytic therapy, chronic nonsteroidal anti-inflammatory drugs [NSAIDS], selective serotonin reuptake inhibitors, serotonin norepinephrine reuptake inhibitors) increases the risk of bleeding
- Avoid concomitant use of warfarin or other anticoagulants.
- Suspect bleeding in any patient who is hypotensive and has recently undergone coronary angiography, percutaneous coronary intervention (PCI), coronary artery bypass graft surgery (CABG), or other surgical procedures.
- Withholding vorapaxar for a brief period will not be useful in managing an acute bleeding event because of its long half-life.
- There is no known treatment to reverse the antiplatelet effect of vorapaxar.
- Significant inhibition of platelet aggregation remains 4 weeks after discontinuation.
Strong CYP3A Inhibitors or Inducers
- Strong CYP3A inhibitors increase and inducers decrease vorapaxar exposure.
- Avoid concomitant use of vorapaxar with strong CYP3A inhibitors or inducers
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Vorapaxar was evaluated for safety in 13,186 patients, including 2,187 patients treated for more than 3 years, in the Phase 3 study TRA 2°P TIMI 50 (Thrombin Receptor Antagonist in Secondary Prevention of Atherothrombotic Ischemic Events). The overall study population, patients who had evidence or a history of atherosclerosis involving the coronary (post-MI), cerebral (ischemic stroke), or peripheral vascular (documented history of PAD) systems, was treated once a day with vorapaxar (n=13,186) or placebo (n=13,166). Patients randomized to vorapaxar received treatment for a median of 2.3 years.
The adverse events in the vorapaxar-treated (n=10,059) and placebo-treated (n=10,049) post-MI or PAD patients with no history of stroke or TIA are shown below.
Bleeding
GUSTO severe bleeding was defined as fatal, intracranial, or bleeding with hemodynamic compromise requiring intervention; GUSTO moderate bleeding was defined as bleeding requiring transfusion of whole blood or packed red blood cells without hemodynamic compromise. (GUSTO: Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Arteries.)
The results for the bleeding endpoints in the post-MI or PAD patients without a history of stroke or TIA are shown in Table 1. Vorapaxar increased GUSTO moderate or severe bleeding by 55%.

† Hazard ratio is vorapaxar group vs. placebo group.
‡K-M estimate at 1,080 days.
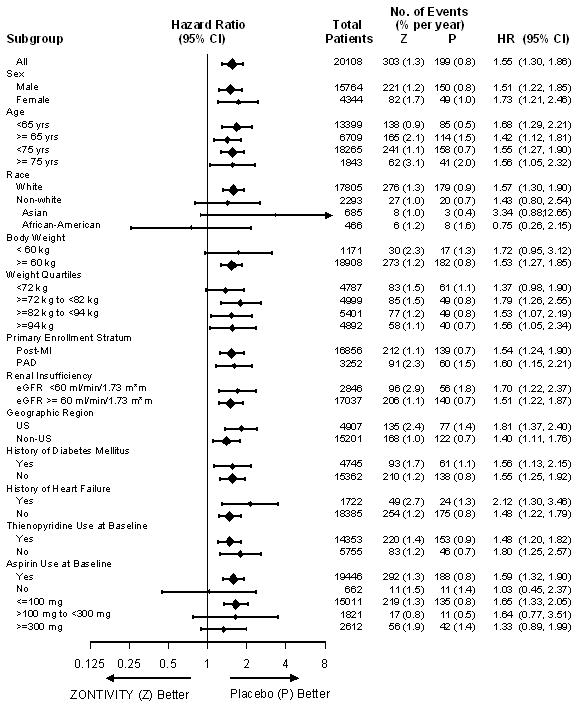
The effects of vorapaxar on bleeding were examined in a number of subsets based on demographic and other baseline characteristics. Many of these are shown in Figure 1. Such analyses must be interpreted cautiously, as differences can reflect the play of chance among a large number of analyses.
In TRA 2°P, 367 post-MI or PAD patients without a history of stroke or TIA underwent CABG surgery. Study investigators were encouraged not to discontinue treatment with study drug (i.e., vorapaxar or placebo) prior to surgery. Approximately 12.3% of patients discontinued vorapaxar more than 30 days prior to CABG. The relative risk for GUSTO moderate or severe bleeding was approximately 1.2 on vorapaxar vs. placebo.
Bleeding events that occurred on vorapaxar were treated in the same manner as for other antiplatelet agents.
Use in Patients with History of Stroke, TIA, or ICH
In the TRA 2°P study, patients with a history of ischemic stroke had a higher rate for ICH on vorapaxar than on placebo. Vorapaxar is contraindicated in patients with a history of stroke, TIA, or ICH.
Other Adverse Reactions
Adverse reactions other than bleeding were evaluated in 19,632 patients treated with vorapaxar [13,186 patients in the TRA 2°P study and 6,446 patients in the TRA•CER (Thrombin Receptor Antagonist for Clinical Event Reduction in Acute Coronary Syndrome) study]. Adverse events other than bleeding that occurred at a rate that was at least 2% in the vorapaxar group and also 10% greater than the rate in the placebo group are shown in Table 2.

The following adverse reactions occurred at a rate less than 2% in the vorapaxar group but at least 40% greater than placebo. In descending order of rate in the vorapaxar group: iron deficiency, retinopathy or retinal disorder, and diplopia/oculomotor disturbances.
An increased rate of diplopia and related oculomotor disturbances was observed with vorapaxar treatment (30 subjects, 0.2%) vs. placebo (10 subjects, 0.06%). While some cases resolved during continued treatment, information on resolution of symptoms was not available for some cases.
Postmarketing Experience
There is limited information regarding Vorapaxar Postmarketing Experience in the drug label.
Drug Interactions
Vorapaxar is eliminated primarily by metabolism, with contributions from CYP3A4 and CYP2J2.
Strong CYP3A Inhibitors
Avoid concomitant use of vorapaxar with strong inhibitors of CYP3A (e.g., ketoconazole, itraconazole, posaconazole, clarithromycin, nefazodone, ritonavir, saquinavir, nelfinavir, indinavir, boceprevir, telaprevir, telithromycin and conivaptan).
Strong CYP3A Inducers
Avoid concomitant use of vorapaxar with strong inducers of CYP3A (e.g., rifampin, carbamazepine, St. John's Wort and phenytoin).
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B There are no adequate and well-controlled studies of vorapaxar use in pregnant women.
Risk Summary
Based on data in rats and rabbits, vorapaxar is predicted to have a low probability of increasing the risk of adverse developmental outcomes above background. No embryo/fetal toxicities, malformations or maternal toxicities were observed in rats exposed during gestation to 56 times the human systemic exposure at the recommended human dose (RHD). No embryo/fetal toxicities, malformations or maternal toxicities were observed in rabbits exposed during gestation to 26 times the human systemic exposure at the RHD. The No Adverse Effect Level (NOAEL) for decreased perinatal survival and body weight in off-spring exposed in utero and during lactation was 31 times the human systemic exposure at the RHD. Both male and female pups displayed transient effects on sensory function and neurobehavioral development at weaning at 67 times the human exposure at the RHD, whereas female pups displayed decreased memory at 31 times the human exposure at the RHD. However, animal studies are not always predictive of a human response. Vorapaxar should be used during pregnancy only if the potential benefit to the mother justifies the potential risk to the fetus.
Animal Data
In the rat embryo/fetal developmental toxicity study, pregnant rats received daily oral doses of vorapaxar at 0, 5, 25, and 75 mg/kg from implantation to closure of the fetal hard palate (6th to 17th day of gestation). Maternal systemic exposures were approximately 0, 7, 56, and 285 times greater than exposures in women treated at the RHD based on AUC. No embryo/fetal toxicities, malformations, or maternal toxicities were observed in rats receiving exposures up to 56 times the human systemic exposure at the RHD.
In the rabbit embryo/fetal developmental toxicity study, pregnant rabbits received daily oral doses of vorapaxar at 0, 2, 10, or 20 mg/kg from implantation to closure of the fetal hard palate (7th to 19th day of gestation). The NOAEL for maternal and fetal toxicity was equal to or above the highest dose tested. However, an overall increase in the number of litters with any malformation was observed at the highest dose, where systemic exposures were 89-fold higher than the human exposure at RHD.
The effects of vorapaxar on prenatal and postnatal development were assessed in pregnant rats dosed at 0, 5, 25, or 50 mg/kg/day from implantation through the end of lactation. Rat pups had decreased survival and body weight gain from birth to postnatal day 4 and decreased body weight gain for the overall pre-weaning period at exposures 67 times the human exposure at the RHD. Both male and female pups displayed effects on sensory function (acoustic startle) and neurobehavioral (locomotor assay) development on post-natal day (PND) 20 and 21, but not later (PND 60, 61) in development, whereas decreased memory was observed in female pups on PND 27 at 31 times the human exposure at the RHD. In utero and lactational exposure did not affect fertility or reproductive behavior of offspring at exposures up to 67 times the RHD.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Vorapaxar in women who are pregnant.
Labor and Delivery
There is no FDA guidance on use of Vorapaxar during labor and delivery.
Nursing Mothers
It is unknown whether vorapaxar or its metabolites are excreted in human milk, but it is actively secreted in milk of rats. Because many drugs are excreted in human milk, and because of the potential for serious adverse reactions in nursing infants from vorapaxar, discontinue nursing or discontinue vorapaxar.
Pediatric Use
The safety and effectiveness of vorapaxar in pediatric patients have not been established.
Geriatic Use
In TRA 2°P, in post-MI or PAD patients without a history of stroke or TIA, 33% of patients were ≥65 years of age and 9% were ≥75 years of age. The relative risk of bleeding (vorapaxar compared with placebo) was similar across age groups. No overall differences in safety or effectiveness were observed between these patients and younger patients. Vorapaxar increases the risk of bleeding in proportion to a patient's underlying risk. Because older patients are generally at a higher risk of bleeding, consider patient age before initiating vorapaxar
Gender
There is no FDA guidance on the use of Vorapaxar with respect to specific gender populations.
Race
There is no FDA guidance on the use of Vorapaxar with respect to specific racial populations.
Renal Impairment
No dose adjustment is required in patients with renal impairment
Hepatic Impairment
No dose adjustment is required in patients with mild and moderate hepatic impairment. Based on the increased inherent risk of bleeding in patients with severe hepatic impairment, vorapaxar is not recommended in such patients.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Vorapaxar in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Vorapaxar in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral, with or without food.
Monitoring
There is limited information regarding Vorapaxar Monitoring in the drug label.
IV Compatibility
There is limited information regarding the compatibility of Vorapaxar and IV administrations.
Overdosage
There is no known treatment to reverse the antiplatelet effect of vorapaxar, and neither dialysis nor platelet transfusion can be expected to be beneficial if bleeding occurs after overdose. Inhibition of platelet aggregation can be expected for weeks after discontinuation of normal dosing. There is no standard test available to assess the risk of bleeding in an overdose situation.
Pharmacology
Mechanism of Action
Vorapaxar is a reversible antagonist of the protease-activated receptor-1 (PAR-1) expressed on platelets, but its long half-life makes it effectively irreversible. Vorapaxar inhibits thrombin-induced and thrombin receptor agonist peptide (TRAP)-induced platelet aggregation in in vitro studies. Vorapaxar does not inhibit platelet aggregation induced by adenosine diphosphate (ADP), collagen or a thromboxane mimetic and does not affect coagulation parameters ex vivo. PAR-1 receptors are also expressed in a wide variety of cell types, including endothelial cells, neurons, and smooth muscle cells, but the pharmacodynamic effects of vorapaxar in these cell types have not been assessed.
Structure
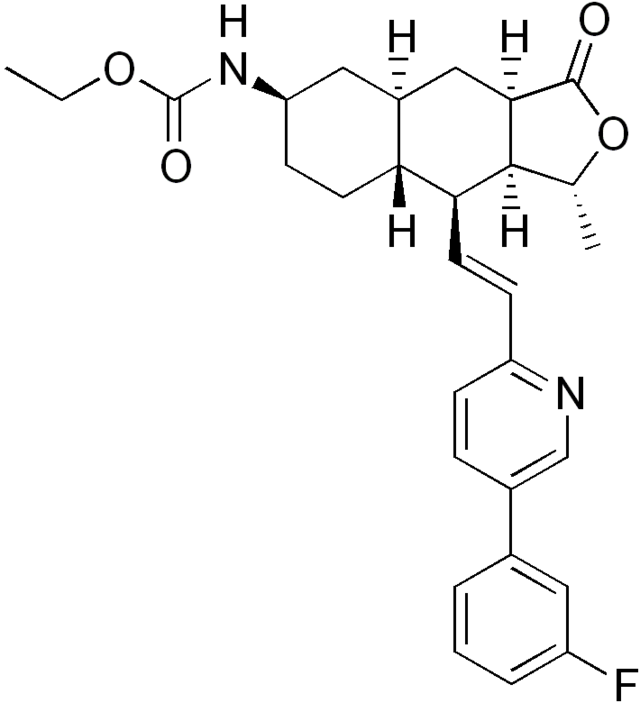
The chemical name of vorapaxar sulfate is ethyl [(1R,3aR,4aR,6R,8aR,9S,9aS)-9-{(1E)-2-[5-(3-fluorophenyl)pyridin-2-yl]ethen-1-yl}-1-methyl-3-oxododecahydronaphtho[2,3-c]furan-6-yl]carbamate sulfate. The empirical formula is C29H33FN2O4∙H2SO4, and its molecular weight is 590.7. The structural formula is:

Pharmacodynamics
At the recommended dose, vorapaxar achieves ≥80% inhibition of TRAP-induced platelet aggregation within one week of initiation of treatment. The duration of platelet inhibition is dose- and concentration-dependent. Inhibition of TRAP-induced platelet aggregation at a level of 50% can be expected at 4 weeks after discontinuation of daily doses of vorapaxar 2.08 mg, consistent with the terminal elimination half-life of vorapaxar.
In healthy volunteer studies, no changes in platelet P-selectin and soluble CD40 ligand (sCD40L) expression or coagulation test parameters (TT, PT, aPTT, ACT, ECT) occurred after single- or multiple- dose (28 days) administration of vorapaxar. No meaningful changes in P-selectin, sCD40L, or hs-CRP concentrations were observed in patients treated with vorapaxar in the phase 2/3 clinical trials.
Evaluation of Vorapaxar on QTc Interval
The effect of vorapaxar on the QTc interval was evaluated in a thorough QT study and in other studies. Vorapaxar had no effect on the QTc interval at single doses up to 48 times the recommended dose.
Pharmacokinetics
Vorapaxar exposure increases in an approximately dose-proportional manner following single doses up to 16 times the recommended dose. Vorapaxar pharmacokinetics are similar in healthy subjects and patients.
Absorption
After oral administration of a single vorapaxar 2.08 mg dose under fasted conditions, peak concentrations (Cmax) occur at 1 hour post-dose (range: 1 to 2 h). The mean absolute bioavailability as determined from a microdosing study is approximately 100%.
Ingestion of vorapaxar with a high-fat meal resulted in no meaningful change in AUC with a small (21%) decrease in Cmax and delayed time to peak concentration (45 minutes). Vorapaxar may be taken with or without food.
Distribution
The mean volume of distribution of vorapaxar is approximately 424 liters (95% CI: 351-512). Vorapaxar and the major circulating active metabolite, M20, are extensively bound (≥99%) to human plasma proteins. Vorapaxar is highly bound to human serum albumin and does not preferentially distribute into red blood cells.
Metabolism
Vorapaxar is eliminated by metabolism via CYP3A4 and CYP2J2. The major active circulating metabolite is M20 (monohydroxy metabolite) and the predominant metabolite identified in excreta is M19 (amine metabolite). The systemic exposure of M20 is ~20% of the exposure to vorapaxar.
Excretion
The primary route of elimination is through the feces. In a 6-week study, 84% of the administered radiolabeled dose was recovered as total radioactivity with 58% collected in feces and 25% in urine. Vorapaxar is eliminated primarily in the form of metabolites, with no unchanged vorapaxar detected in urine.
Vorapaxar exhibits multi-exponential disposition with an effective half-life of 3-4 days and an apparent terminal elimination half-life of 8 days. Steady-state is achieved by 21 days following once-daily dosing with an accumulation of 5- to 6-fold. The apparent terminal elimination half-life for vorapaxar is approximately 8 days (range 5-13 days) and is similar for the active metabolite. The terminal elimination half-life is important to determine the time to offset the pharmacodynamic effect.
Specific Populations
In general, effects on the exposure of vorapaxar based on age, race, gender, weight, and moderate renal insufficiency were modest (20-40%). No dose adjustments are necessary based upon these factors. Because of the inherent bleeding risks in patients with severe hepatic impairment, vorapaxar is not recommended in such patients.

Effects of Other Drugs on Vorapaxar
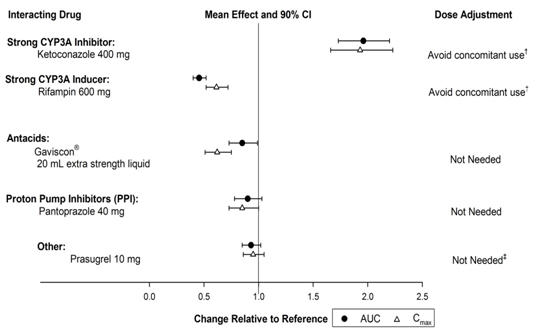
The effects of other drugs on the pharmacokinetics of vorapaxar are presented in Figure 3 as change relative to vorapaxar administered alone (test/reference). Phase 3 data suggest that coadministration of a weak or moderate CYP3A inhibitor with vorapaxar does not increase bleeding risk or alter the efficacy of vorapaxar. No dose adjustment for vorapaxar is required in patients taking weak to moderate inhibitors of CYP3A.
Effects of Vorapaxar on Other Drugs
In vitro metabolism studies demonstrate that vorapaxar or M20 is unlikely to cause clinically significant inhibition or induction of major CYP isoforms or inhibition of OATP1B1, OATP1B3, BCRP, OAT1, OAT3, and OCT2 transporters.
Specific in vivo effects on the pharmacokinetics of digoxin, warfarin, rosiglitazone and prasugrel are presented in Figure 4 as a change relative to the interacting drug administered alone (test/reference). Vorapaxar is a weak inhibitor of the intestinal P-glycoprotein (P-gp) transporter. No dosage adjustment of digoxin or vorapaxar is required.

Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Carcinogenicity studies were conducted in rats and mice dosed orally with vorapaxar for two years. Male and female rats dosed at 0, 3, 10 or 30 mg/kg/day showed no carcinogenic potential at systemic exposures (AUC) in males and females that were 9- and 29-fold, respectively, the human systemic exposure at the RHD. In male and female mice dosed at 0, 1, 5, and 15 mg/kg/day, vorapaxar showed no carcinogenic potential at systemic exposures (AUC) that were up to 30-fold the human systemic exposure.
Mutagenesis
Vorapaxar was not mutagenic in the Ames bacterial reverse mutation assay and not clastogenic in an in vitro human peripheral blood lymphocyte assay or an in vivo mouse micronucleus assay after intraperitoneal administration.
Impairment of Fertility
Fertility studies in rats showed that vorapaxar had no effect on either male or female fertility at doses up to 50 mg/kg/day, a dose resulting in systemic exposures (AUC) in male and female rats that are 40 and 67 times, respectively, the human systemic exposure at the RHD.
Animal Pharmacology
Vorapaxar did not increase bleeding time in non-human primates when administered alone. Bleeding time was prolonged slightly with administration of aspirin or aspirin plus vorapaxar. The combination of aspirin, vorapaxar, and clopidogrel produced significant prolongation of bleeding time. Transfusion of human platelet rich plasma normalized bleeding times with partial recovery of ex vivo platelet aggregation induced with arachidonic acid, but not induced with ADP or TRAP. Platelet poor plasma had no effect on bleeding times or platelet aggregation.
Clinical Studies
The clinical evidence for the effectiveness of vorapaxar is supported by TRA 2°P - TIMI 50. TRA 2°P was a multicenter, randomized, double-blind, placebo-controlled study conducted in patients who had evidence or a history of atherosclerosis involving the coronary (spontaneous MI ≥2 weeks but ≤12 months prior), cerebral (ischemic stroke), or peripheral vascular (documented peripheral arterial disease [PAD]) systems. Patients were randomized to receive daily treatment with vorapaxar (n=13,225) or placebo (n=13,224) in addition to standard of care. The study's primary endpoint was the composite of cardiovascular death, MI, stroke, and urgent coronary revascularization (UCR). The composite of cardiovascular death, MI, and stroke was assessed as key secondary endpoint. The median follow-up was 2.5 years (up to 4 years).
The findings in all randomized patients for the primary efficacy composite endpoint show a 3-year K-M event rate of 11.2% in the vorapaxar group compared to 12.4% in the placebo group (hazard ratio [HR]: 0.88; 95% confidence interval [CI], 0.82 to 0.95; p=0.001).
The findings for the key secondary efficacy endpoint show a 3-year Kaplan-Meier (K-M) event rate of 9.3% in the vorapaxar group compared to 10.5% in placebo group (HR 0.87; 95% CI, 0.80 to 0.94; p<0.001).
Although TRA 2°P was not designed to evaluate the relative benefits and risks of vorapaxar in individual patient subgroups, patients with a history of stroke or TIA showed an increased risk of ICH. Of the patients who comprised the post-MI and PAD strata and had no baseline history of stroke or TIA,10,080 were randomized to treatment with vorapaxar and 10,090 to placebo. These patients were 89% Caucasian, 22% female, and 33% ≥65 years of age, with a median age of 60 years. The population included patients with diabetes (24%) and patients with hypertension (65%). Of the patients who qualified for the trial with MI without a history of stroke or TIA, 98% were receiving aspirin, 78% were receiving a thienopyridine, and 77% were receiving both aspirin and a thienopyridine when they enrolled in the trial. Of the patients who qualified for the trial with PAD without a history of stroke or TIA, 88% were receiving aspirin, 35% were receiving a thienopyridine, and 27% were receiving both aspirin and a thienopyridine when they enrolled.
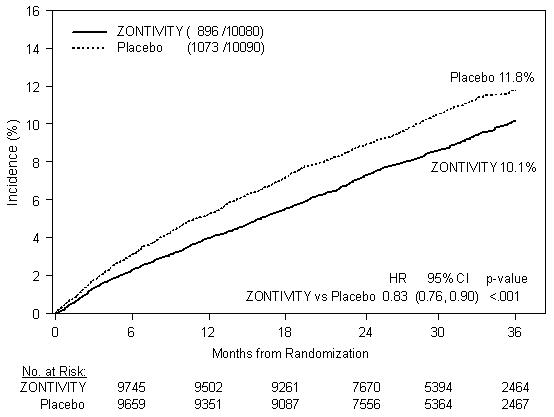
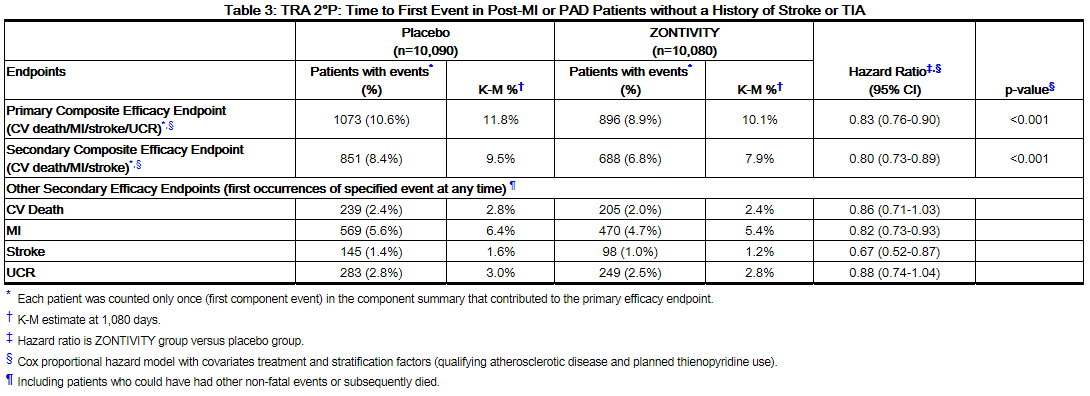
In post-MI or PAD patients without a history of stroke or TIA the 3-year K-M event rate for the primary efficacy endpoint (composite of time to first CV death, MI, stroke, or UCR) was of 10.1% in the vorapaxar group compared to 11.8% in the placebo group (HR 0.83; 95% CI, 0.76 to 0.90; p<0.001).
The results for the key secondary efficacy endpoint (composite of time to first CV death, MI, or stroke) show a 3-year K-M event rate of 7.9% in the vorapaxar group compared to 9.5% in the placebo group (HR 0.80; 95% CI, 0.73 to 0.89; p<0.001).
The effect of chronic dosing with vorapaxar on the primary and key secondary endpoints was maintained for the duration of the trial (median follow up 2.5 years, up to 4 years).
In post-MI or PAD patients who survived an on-study efficacy event, the incidence of subsequent events was lower with vorapaxar.
The time from the prior MI to randomization had no relationship to the treatment benefit for the primary study outcome.
A range of demographic, concurrent baseline medications, and other treatment differences were examined for their influence on outcomes as shown in Figure 6. Such analyses must be interpreted cautiously, as differences can reflect the play of chance among a large number of analyses.

How Supplied
Vorapaxar tablets, 2.08 mg vorapaxar, are yellow, oval-shaped, film-coated tablets with "351" on one side and the Merck logo on the other side.
They are supplied as follows:
- NDC 0006-0351-31 bottles of 30 tablets
- NDC 0006-0351-54 bottles of 90 tablets
- NDC 0006-0351-48 unit dose packages of 100 tablets (one carton containing 10 10-count blister cards)
Storage
Storage of bottles
Store at 20-25°C (68-77°F), excursions permitted between 15-30°C (between 59-86°F). Store tablets in the original package with the bottle tightly closed. Keep the desiccant in the bottle to protect from moisture.
Storage of blisters
Store at 20-25°C (68-77°F), excursions permitted between 15-30°C (between 59-86°F). Store in the original package until use.
Images
Drug Images
{{#ask: Page Name::Vorapaxar |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Vorapaxar |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Advise the patient to read the FDA-approved Patient Labeling (Medication Guide).
Benefits and Risks
- Summarize the benefits and potential side effects of vorapaxar.
- Tell patients to take vorapaxar exactly as prescribed.
- Inform patients not to discontinue vorapaxar without discussing it with the prescribing physician.
- Tell patients to read the Medication Guide.
Bleeding
Inform patients that they:
- May bleed and bruise more easily.
- Should report any unanticipated, prolonged or excessive bleeding, or blood in their stool or urine.
Invasive Procedures
Instruct patients to:
- Inform physicians and dentists that they are taking vorapaxar before any surgery or dental procedure.
- Tell the doctor performing any surgery or dental procedure to talk to the prescribing physician before stopping vorapaxar.
Concomitant Medications
- Tell patients to list all prescription medications, over-the-counter medications, or dietary supplements they are taking or plan to take so that the physician knows about other treatments that may affect bleeding risk.
Precautions with Alcohol
Alcohol-Vorapaxar interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication.
Brand Names
- Zontivity
Look-Alike Drug Names
There is limited information regarding Vorapaxar Look-Alike Drug Names in the drug label.
Drug Shortage Status
Drug Shortage
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ "Vorapaxar Tablets 2.08 mg, for oral use. Full Prescribing Information" (PDF). Merck & Co., Inc. Initial U.S. Approval: 05/2014. Retrieved 17 June 2014.
{{#subobject:
|Label Page=Vorapaxar |Label Name=Vorapaxar label.jpg
}}
{{#subobject:
|Label Page=Vorapaxar |Label Name=Vorapaxar FDA panel.png
}}
{{#subobject:
|Label Page=Vorapaxar |Label Name=Vorapaxar FDA panel2.png
}}