Fibrinolysis
|
WikiDoc Resources for Fibrinolysis |
|
Articles |
|---|
|
Most recent articles on Fibrinolysis Most cited articles on Fibrinolysis |
|
Media |
|
Powerpoint slides on Fibrinolysis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Fibrinolysis at Clinical Trials.gov Clinical Trials on Fibrinolysis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Fibrinolysis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Fibrinolysis Discussion groups on Fibrinolysis Patient Handouts on Fibrinolysis Directions to Hospitals Treating Fibrinolysis Risk calculators and risk factors for Fibrinolysis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Fibrinolysis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
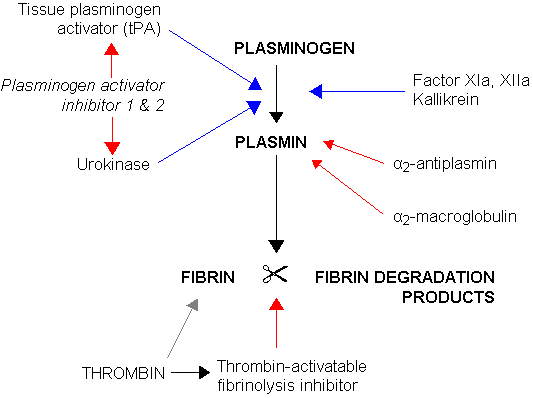
Fibrinolysis is the process where a fibrin clot, the product of coagulation, is broken down. Its main enzyme, plasmin, cuts the fibrin mesh at various places, leading to the production of circulating fragments that are cleared by other proteinases or by the kidney and liver.
Physiology
Plasmin is produced in an inactive form, plasminogen, in the liver. Although plasminogen cannot cleave fibrin, it still has an affinity for it, and is incorporated into the clot when it is formed.
Plasminogen contains secondary structure motifs known as kringles, which bind specifically to lysine and arginine residues on fibrin(ogen). When converted from plasminogen into plasmin it functions as a serine protease, cutting specifically C-terminal to these lysine and arginine residues. Fibrin monomers, when polymerized, form protofibrils. These protofibrils contain two strands, anti-parallel, associated non-covalently. Within a single strand, the fibrin monomers are covalently linked through the actions of coagulation factor XIII. Thus, plasmin action on a clot initially creates nicks in the fibrin; further digestion leads to solubilization (Walker & Nesheim 1999).
Tissue plasminogen activator (t-PA) and urokinase are the agents that convert plasminogen to the active plasmin, thus allowing fibrinolysis to occur. t-PA is released into the blood very slowly by the damaged endothelium of the blood vessels, such that after several days (when the bleeding has stopped) the clot is broken down. This occurs because plasminogen became entrapped within the clot when it formed; as it is slowly activated, it breaks down the fibrin mesh. t-PA and urokinase are themselves inhibited by plasminogen activator inhibitor-1 and plasminogen activator inhibitor-2 (PAI-1 and PAI-2). In contrast, plasmin further stimulates plasmin generation by producing more active forms of both tPA and urokinase.
Alpha 2-antiplasmin and alpha 2-macroglobulin inactivate plasmin. Plasmin activity is also reduced by thrombin-activatable fibrinolysis inhibitor (TAFI), which modifies fibrin to make a less potent cofactor for the tPA-mediated plasminogen activation.
Measurement
When plasmin breaks down fibrin, a number of soluble parts are produced. These are called fibrin degradation products (FDPs). FDPs compete with thrombin, and so slow down the conversion of fibrinogen to fibrin (and thus slows down clot formation). This effect can be seen in the thrombin clotting time (TCT) test, which is prolonged in a person who has active fibrinolysis.
FDPs, and a specific FDP, the D-dimer, can be measured using antibody-antigen technology. This is more specific than the TCT, and virtually confirms that fibrinolysis has occurred. It is therefore used to indicate deep vein thrombosis or a pulmonary embolism.
Role in disease
Few disorders of the fibrinolytic system have been documented. Nevertheless, excess levels of PAI and alpha 2-antiplasmin have been implicated in the metabolic syndrome and various other disease states.
The fibrinolytic system is closely linked to control of inflammation, and plays a role in disease states associated with inflammation. Plasmin, in addition to lysing fibrin clots, also cleaves the complement system component C3, and fibrin degradation products have some vascular permeability inducing effects.
Pharmacology
Fibrinolytic drugs are given after a heart attack to dissolve the thrombus blocking the coronary artery, experimentally in stroke to reperfuse the affected part of the brain, and in massive pulmonary embolism. The process is called thrombolysis.
Antifibrinolytics, such as aminocaproic acid (ε-aminocaproic acid) and tranexamic acid are used as inhibitors of fibrinolysis
References
- Cesarman-Maus G, Hajjar KA. Molecular mechanisms of fibrinolysis. Br J Haematol 2005;129:307-21. PMID 15842654.
- Kumar: Robbins and Cotran: Pathologic Basis of Disease, 7th ed., Copyright © 2005 Saunders
- Walker JB, Nesheim ME. The molecular weights, mass distribution, chain composition, and structure of soluble fibrin degradation products released from a fibrin clot perfused with plasmin. J Biol Chem. 1999;274:5201 - 5212. PMID 9988770.
External link
- Graphical representation of the fibrinolytic pathway