|
|
| (75 intermediate revisions by 9 users not shown) |
| Line 1: |
Line 1: |
| | __NOTOC__ |
| {{Infobox_Disease | | | {{Infobox_Disease | |
| Name = Brugada syndrome | | | Name = Brugada syndrome | |
| Image = BrugadaS.jpg| | | Image = BrugadaS.jpg| |
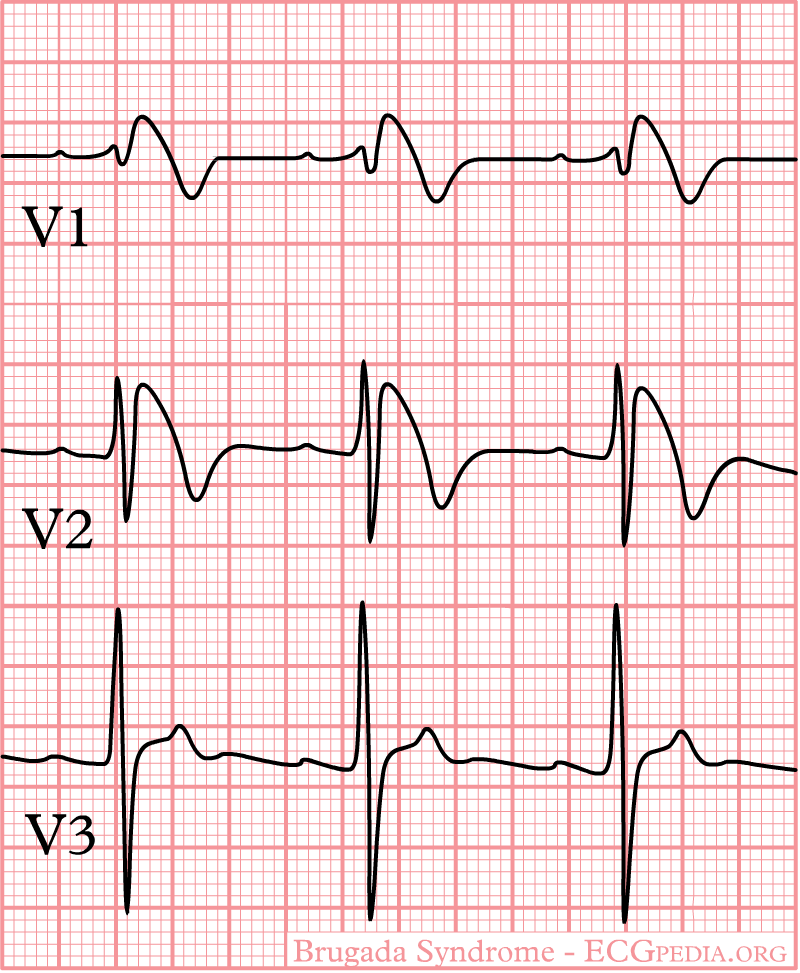
| Caption = ECG findings of Brugada Syndrome| | | Caption = ECG in Type I Brugada Pattern| |
| DiseasesDB = 31999 |
| |
| ICD10 = {{ICD10|I|42|8|i|30}} |
| |
| ICD9 = {{ICD9|746.89}} |
| |
| ICDO = |
| |
| OMIM = 601144 |
| |
| MedlinePlus = |
| |
| eMedicineSubj = |
| |
| eMedicineTopic = |
| |
| MeshID = D053840 |
| |
| }} | | }} |
| {{SI}}
| | '''For patient information, click [[Brugada syndrome (patient information)|here]]''' |
| {{WikiDoc Cardiology Network Infobox}}
| |
| {{CMG}}
| |
|
| |
|
| {{Editor Join}} | | {{Brugada syndrome}} |
|
| |
|
| ==Overview==
| | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
|
| |
|
| The '''Brugada syndrome''' is a genetic disease that is characterized by abnormal [[electrocardiogram]] (ECG) findings and an increased risk of [[sudden cardiac death]] in young adults, and occasionally in children and infants. It is also known as [[Bangungot|Sudden Unexpected Death Syndrome]]<ref>Hong K, Berruezo-Sanchez A, Poungvarin N, Oliva A, Vatta M, Brugada J, Brugada P, Towbin JA, Dumaine R, Pinero-Galvez C, Antzelevitch C, Brugada R. Phenotypic characterization of a large European family with Brugada syndrome displaying a sudden unexpected death syndrome mutation in SCN5A. J Cardiovasc Electrophysiol. 2004 Jan;15(1):64-9. PMID 15028074</ref> ('''SUDS'''), and is the most common cause of sudden death in young men without known underlying cardiac disease in Thailand and Laos<ref>Brugada J, Brugada P, Brugada R. The syndrome of right bundle branch block ST segment elevation in V1 to V3 and sudden death--the Brugada syndrome. Europace. 1999 Jul;1(3):156-66. PMID 11225790 </ref>.
| | {{SK}} Sudden unexpected death syndrome; sudden unexplained death syndrome; SUDS; sudden unexpected nocturnal death syndrome; sudden unexplained nocturnal death syndrome; SUNDS; in the Phillipines ''bangungut'' (to rise and moan in sleep); in Thailand ''lai tai''; in Laos ''Dab tsog'' and in Japan ''Pokkuri disease'' |
|
| |
|
| Although the ECG findings of Brugada syndrome were first reported<ref>Martini B, Nava A, Thiene G, Buja GF, Canciani B, Scognamiglio R, Daliento L, Dalla Volta S. Ventricular fibrillation without apparent heart disease: description of six cases. Am Heart J 1989 Dec;118(6):1203-9 PMID 2589161</ref> among survivors of cardiac arrest in 1989, it was only in 1992 that the Brugada brothers<ref>Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992 Nov 15;20(6):1391-6. PMID 1309182</ref> recognized it as a distinct clinical entity, causing sudden [[death]] by causing [[ventricular fibrillation]] (a lethal [[arrhythmia]]) in the [[heart]].
| | ==[[Brugada syndrome overview|Overview]]== |
|
| |
|
| ==Differential Diagnosis== | | ==[[Brugada syndrome classification|Classification]]== |
|
| |
|
| * Abnormalities that can lead to ST-segment elevation in the right precordial leads
| | ==[[Brugada syndrome historical perspective|Historical Perspective]]== |
| :* Acute myocardial ischemia or infarction
| |
| :* Acute myocarditis
| |
| :* Acute pulmonary thromboemboli
| |
| :* Arrhythmogenic right ventricular dysplasia / cardiomyopathy (ARVD/C)
| |
| :* Cocaine intoxication
| |
| :* Dissecting aortic aneurysm
| |
| :* Duchenne muscular dystrophy
| |
| :* Friedreich ataxia
| |
| :* Heterocyclic antidepressant overdose
| |
| :* Hypercalcemia
| |
| :* Hyperkalemia
| |
| :* Hypothermia, causing Osborn wave in ECGs and sometimes resembling Brugada syndrome
| |
| :* Left ventricular hypertrophy
| |
| :* Mediastinal tumor compressing the right ventricular outflow tract (RVOT)
| |
| :* Right or left bundle-branch block
| |
| :* Right ventricular infarction
| |
| :* Right ventricular ischemia
| |
| :* Thiamine deficiency
| |
| :* Various central and autonomic nervous system abnormalities
| |
| * Other conditions that can lead to ST-segment elevation in the right precordial leads
| |
| :* Early repolarization syndrome
| |
| :* Other normal variants (particularly in males)
| |
|
| |
|
| ==Epidemiology== | | ==[[Brugada syndrome pathophysiology|Pathophysiology]]== |
|
| |
|
| The average age at the time of initial diagnosis or sudden death is 40 ± 22 years, with the youngest patient diagnosed at 2 days of age and the oldest at 84 years. The prevalence of the Brugada syndrome is estimated at 1–5 per 10,000 inhabitants worldwide. The frequency is lower in western countries and higher (≥5 per 10,000) in Southeast Asia.
| | ==[[Brugada syndrome differential diagnosis|Differentiating Brugada syndrome from other Diseases]]== |
|
| |
|
| ==Genetics and pathophysiology== | | ==[[Brugada syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
|
| |
|
| Approximately 20% of the cases of Brugada syndrome have been shown to be associated with mutation(s) in the [[gene]] that encodes for the [[sodium]] [[ion channel]] in the [[cell (biology)|cell]] [[cell membrane|membrane]]s of the muscle cells of the heart (the [[myocyte]]s). The gene, named [[SCN5A]], is located on the short arm of the third [[chromosome]] (3p21). Loss-of-function mutations in this gene lead to a loss of the action potential dome of some epicardial areas of the right ventricle. This results in transmural and epicardial dispersion of repolarization. The transmural dispersion underlies ST-segment elevation and the development of a vulnerable window across the ventricular wall, whereas the epicardial dispersion of repolarization facilitates the development of phase 2 reentry, which generates a phase 2 reentrant extrasystole that captures the vulnerable window to precipitate ventricular tachycardia and/or fibrillation that often results in sudden cardiac death. At present time however, all the reported patients died because of the disease and submitted to detailed necropsy study, have shown a structural right ventricular pathology underlying the syndrome.
| | ==[[Brugada syndrome risk factors|Risk Factors]]== |
|
| |
|
| Over 160 mutations in the SCN5A gene have been discovered to date, each having varying mechanisms and effects on function, thereby explaining the varying degrees of penetration and expression of this disorder. <ref name="pmid16972995">{{cite journal |author=Napolitano C, Priori SG |title=Brugada syndrome |journal=Orphanet journal of rare diseases |volume=1 |issue= |pages=35 |year=2006 |pmid=16972995 |doi=10.1186/1750-1172-1-35}}</ref>
| | ==[[Brugada syndrome screening|Screening]]== |
|
| |
|
| An example of one of the mechanisms in which a loss of function of the sodium channel occurs is a mutation in the gene that disrupts the sodium channel's ability to bind properly to [[ankyrin]]-G, an important protein mediating interaction between ion channels and cytoskeletal elements. Very recently a mutation in a second gene, [[Glycerol-3-phosphate dehydrogenase]] 1-like gene ({{Gene|GPD1L}}) has been shown to result in Brugada Syndrome in a large multigenerational family (London, 2006). This gene acts as an ion channel modulator in the heart, although the exact mechanism is not yet understood.
| | ==[[Brugada syndrome natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
|
| |
|
| Recently Antzelevitch has identified mutations in the [[Voltage-dependent calcium channel|L-type calcium channel]] subunits ({{Gene|CACNA1C}} (A39V and G490R) and {{Gene|CACNB2}} (S481L)) leading to ST elevation and a relatively short QT interval (below 360 msec).<ref name="pmid17556198">{{cite journal |author=Antzelevitch C |title=Genetic basis of Brugada syndrome |journal=Heart rhythm : the official journal of the Heart Rhythm Society |volume=4 |issue=6 |pages=756–7 |year=2007 |pmid=17556198 |doi=10.1016/j.hrthm.2007.03.015}}</ref>
| | ==Brugada syndrome diagnosis|Diagnosis== |
| | | [[Brugada syndrome diagnostic criteria|Diagnostic Criteria]] | [[Brugada syndrome history and symptoms|History and Symptoms]] | [[Brugada syndrome physical examination|Physical Examination]] | [[Brugada syndrome laboratory findings|Laboratory Findings]] | [[Brugada syndrome electrocardiogram|Electrocardiogram]] | [[Brugada syndrome chest x ray|Chest X Ray]] | [[Brugada syndrome echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Brugada syndrome electrophysiologic studies|Electrophysiologic Studies]] | [[Brugada syndrome genetic testing|Genetic Testing]] |
| This condition is inherited in an [[autosomal dominant]] pattern and is more common in males. In addition it has a higher prevalence in most Asian populations.<ref>Brugada Syndrome. Charles Antzelevitch, PH.D. PACE 2006; 29:1130–1159</ref> <ref>Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: A distinct clinical and electrocardiographic syndrome: A multicenter report. J Am Coll Cardiol 1992; 20:1391–1396.</ref> <ref>Antzelevitch C, Brugada P, Brugada J, Brugada R, Shimizu W, Gussak I, Perez Riera AR. Brugada syndrome. A decade of progress. Circ Res 2002; 91:1114–1119.</ref> <ref>Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome: Consensus report. Eur Heart J 2002; 23:1648–1654.</ref> <ref>Wilde AA, Antzelevitch C, Borggrefe M, et al. Proposed diagnostic criteria for the Brugada syndrome: Consensus report. Circulation 2002; 106:2514–2519.</ref> <ref>Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome. Report of the second consensus conference. Endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation 2005; 111:659–670.</ref> <ref>Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome:Report of the second consensus conference. Heart Rhythm 2005; 2:429–440.</ref>
| |
| | |
| ==Electrocardiography==
| |
| | |
| In some cases, the disease can be detected by observing characteristic patterns on an [[electrocardiogram]], which may be present all the time, or might be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels and causing appearance of ECG abnormalities - [[ajmaline]], [[flecainide]]) or resurface spontaneously due to as yet unclarified triggers. The pattern seen on the ECG is persistent ST elevations in the electrocardiographic leadsV<sub>1</sub>-V<sub>3</sub> with a [[right bundle branch block]] ([[RBBB]]) appearance with or without the terminal S waves in the lateral leads that are associated with a typical [[RBBB]]. A prolongation of the [[PR interval]] (a conduction disturbance in the heart) is also frequently seen.The electrocardiogram can fluctuate over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the [[ST segment]] elevation, while vagal stimulation worsens it. (There is a case report of a patient who died while shaving, presumed due to the vagal stimulation of the carotid sinus massage!) The administration of class Ia, Ic and III drugs increases the [[ST segment]] elevation, and also fever. Exercise decreases [[ST segment]] elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of [[ST segment]] elevation. When the heart rate decreases, the [[ST segment]] elevation increases and when the heart rate increases the [[ST segment]] elevation decreases. However, the contrary can also be observed.
| |
| | |
| ==Characteristics==
| |
| | |
| *Characterized by a coved-type ST-segment elevation in the right precordial leads
| |
| *The Brugada ECG is often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including sodium channel blockers, a febrile state, vagotonic agents, tricyclic antidepressants, as well as cocaine and Propranolol intoxication.
| |
| | |
| ==Genetics==
| |
| | |
| # SCN5A is a gene that encodes the alpha sodium unit of the cardiac sodium channel. Mutations in SCN5A account for about 15-30% of Brugada syndrome cases. A negative genetic test for SCN5A does not exclude that SCN5A is causing the clinical syndrome because the genetic tests do not evaluate for mutations in promotors, cryptic splicing mutations, or gross rearrangements in the protein product.
| |
| # Glycerol-3-phosphate dehydrogenase (GPD1L) is associated with progressive conduction disease and low sensitivity to procainamide resulting from decreased Isodium current. It has a relatively good prognosis.
| |
| # CACNA1C (alpha subunit of L-type cardiac calcium channel) and CACNB2b (beta subunit of L-type cardiac calcium channel) is associated with a shortened QT interval and a combinatin Brugada/Short QT interval syndrome.
| |
| | |
| ==Brugada EKG==
| |
| | |
| # Type 1 ST segment elevation is diagnostic of Brugada syndrome and is characterized by a coved ST-segment elevation ≥2 mm (0.2 mV) followed by a negative T wave.
| |
| # Type 2 ST-segment elevation has a saddleback appearance with a high take-off ST-segment elevation of ≥2 mm followed by a trough displaying ≥1 mm ST elevation followed by either a positive or biphasic T wave.
| |
| # Type 3 ST-segment elevation has either a saddleback or coved appearance with an ST-segment elevation of <1 mm.
| |
| | |
| <div align="left">
| |
| <gallery heights="125" widths="125">
| |
| Image:BrugadaS.jpg|General characteristics
| |
| Image:Brugada.jpg|EKG of a Patient with Brugada Syndrome
| |
| Image:Brugada_lead_placement.jpg|Lead placements
| |
| </gallery>
| |
| </div>
| |
| | |
| <div align="left">
| |
| <gallery heights="125" widths="125">
| |
| Image:Brugada_syndrome_type1_example.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example2.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example3.jpg|Brugada Type 1
| |
| </gallery>
| |
| </div>
| |
| | |
| <div align="left">
| |
| <gallery heights="125" widths="125">
| |
| Image:Brugada_syndrome_type1_example4.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example5.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example6.jpg|Brugada Type 1
| |
| </gallery>
| |
| </div>
| |
| | |
| <div align="left">
| |
| <gallery heights="125" widths="125">
| |
| Image:Brugada_syndrome_type2_example1.jpg|Brugada Type 2
| |
| Image:Brugada_syndrome_type2_example2.jpg|Brugada Type 2
| |
| </gallery>
| |
| </div>
| |
| | |
| | |
| ==Diagnosis==
| |
| | |
| * Diagnosed when a Type 1 ST-segment elevation is observed in more than one right precordial lead (V1-V3), in the presence or absence of sodium channel blocking agent, and in conjunction with one or more of the following:
| |
| # Family history of SCD (<45 years old)
| |
| # Documented VF
| |
| # Polymorphic ventricular tachycardia
| |
| # Coved-type ECGs in family members
| |
| # Inducibility of VT with programmed electrical stimulation (PES)
| |
| # Syncope
| |
| # Nocturnal agonal respiration
| |
| * Diagnosis is also considered positive when a Type 2 (saddleback pattern) or Type 3 ST-segment elevation is observed in more than one right precordial lead under baseline conditions and can be converted to the diagnostic Type 1 pattern occurs upon exposure to sodium channel blocker.
| |
| | |
| ==Sodium Challenge==
| |
| | |
| * Drugs that can be used
| |
| ** Ajmaline 1 mg/kg/5 min IV
| |
| ** Flecainide 2 mg/kg/10 min IV or 400 mg PO
| |
| ** Procainamide 10 mg/kg/10 min IV
| |
| ** Pilsicainide 1 mg/kg/10 min IV
| |
| * The sodium challenge should be terminated when
| |
| # Diagnostic Type 1 ST-segment elevation or Brugada ECG, develops
| |
| # ST segment in Type 2 increases by ≥2 mm
| |
| # Premature ventricular beats or other arrhythmias develop
| |
| # QRS widens to ≥130% of baseline
| |
| | |
| ==Arrhythmias==
| |
| | |
| # Polymorphic VT resembling a rapid Torsade de Pointes (TdP)
| |
| # Monomorphic VT is observed infrequently
| |
| # VT/VF often terminates spontaneously in patients with the Brugada syndrome which may explain why patients wake up at night after episodes of agonal respiration caused by the arrhythmia.
| |
| | |
| ==Risk Statification==
| |
| | |
| * Patients with syncope and an abnormal Type 1 ECG are at higher risk
| |
| * Asymptomatic patients at risk can be identified
| |
| ** Presence of spontaneous Type 1 ST-segment elevation
| |
| ** Characteristics of the S wave
| |
| ** Presence of late potentials
| |
| ** Inducibility of VT/VF using PES.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Brugada syndrome medical therapy|Medical Therapy]] | [[Brugada syndrome drugs to avoid|Drugs to Avoid]] | [[Brugada syndrome drugs to preferably avoid|Drugs to Preferably Avoid]] | [[Brugada syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Brugada syndrome future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| The cause of death in Brugada syndrome is [[ventricular fibrillation]].The episodes of syncope (fainting) and sudden death (aborted or not) are caused by fast polymorphic ventricular tachycardias or ventricular fibrillation. These arrhythmias appear with no warning. While there is no exact treatment modality that reliably and totally prevents ventricular fibrillation from occurring in this syndrome, treatment lies in termination of this lethal [[arrhythmia]] before it causes death. This is done via implantation of an [[implantable cardioverter-defibrillator]] (ICD), which continuously monitors the heart rhythm and will [[defibrillation|defibrillate]] an individual if ventricular fibrillation is noted. Some recently performed studies had evaluated the role of quinidine, a Class Ia antiarrythmic drug, for decreasing VF episodes occurring in this syndrome. Quinidine was found to decrease number of VF episodes and correcting spontaneous ECG changes, possibly via inhibiting I</sup>to channels.<ref name="pmid15381640">{{cite journal |author=Belhassen B, Glick A, Viskin S |title=Efficacy of quinidine in high-risk patients with Brugada syndrome |journal=Circulation |volume=110 |issue=13 |pages=1731–7 |year=2004 |pmid=15381640 |doi=10.1161/01.CIR.0000143159.30585.90}}</ref> Those with risk factors for [[coronary artery disease]] may require an angiogram before ICD implantation.
| | ==Case Studies== |
| | | [[Brugada syndrome case study one|Case #1]] |
| * Aborted sudden death are at high risk for recurrence and should receive an ICD
| |
| * VT storm has been successfully treated with Isoproterenol. The mechanism is thought to be augmenting the cardiac L type channel.
| |
| * Asymptomatic patients require risk stratification and clinical judegement to help guide therapy
| |
| * Quinidine (class IA sodium channel blocker) blocks the Ito current and is proven to suppress spontaneous VF
| |
| * Cilostazol (phosphodiesterase III inhibitor that increases inward L type calcium channel current and reported to suppress spontaneous VF
| |
| * Bepridil suppress spontaneous VF probably through blocking Ito current
| |
| * Medical therapy alone with the above agents is currently not evaluated in randomized trials and should not be used as loan therapy.
| |
|
| |
|
| ==See also== | | ==Related Chapters== |
| * [[Cardiac action potential]] | | * [[Cardiac action potential]] |
| * [[Genetics]] | | * [[Genetics]] |
| Line 178: |
Line 46: |
| * [[Tambocor]] | | * [[Tambocor]] |
|
| |
|
| ==References==
| | {{Electrocardiography}} |
| {{Reflist|2}} | |
| | |
| ==External links==
| |
| * [http://www.genetests.org/profiles/brugada GeneReviews: Brugada syndrome]
| |
| * Algado et al: http://www.medspain.com/ant/n13_jun00/Brugada.htm
| |
| * Behr: http://www.c-r-y.org.uk/long_qt_syndrome.htm
| |
| * [http://www.brugada.org The Ramon Brugada Senior Foundation ]
| |
| * http://digilander.libero.it/martini_syndrome/
| |
|
| |
|
| {{Electrocardiography}}
| |
| {{SIB}}
| |
| <br> | | <br> |
| [[de:Brugada-Syndrom]] | | [[de:Brugada-Syndrom]] |
| Line 202: |
Line 60: |
| [[zh:布魯格達氏症候群]] | | [[zh:布魯格達氏症候群]] |
| [[tr:Brugada sendromu]] | | [[tr:Brugada sendromu]] |
| | |
| | {{WikiDoc Help Menu}} |
| | {{WikiDoc Sources}} |
| | [[CME Category::Cardiology]] |
|
| |
|
| [[Category:Electrophysiology]] | | [[Category:Electrophysiology]] |
| Line 207: |
Line 69: |
| [[Category:Channelopathy]] | | [[Category:Channelopathy]] |
| [[Category:Genetic disorders]] | | [[Category:Genetic disorders]] |
|
| |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |