Aortic aneurysm: Difference between revisions
No edit summary |
No edit summary |
||
| Line 1: | Line 1: | ||
{{ | {{Template:Aortic aneurysm}} | ||
{{SI}} | {{SI}} | ||
{{WikiDoc Cardiology Network Infobox}} | {{WikiDoc Cardiology Network Infobox}} | ||
| Line 23: | Line 9: | ||
{{Editor Join}} | {{Editor Join}} | ||
==[[Aortic aneurysm overview|Overview]]== | |||
==Pathology== | ==Pathology== | ||
| Line 35: | Line 21: | ||
===Thoracic Aortic Aneurysm=== | ===Thoracic Aortic Aneurysm=== | ||
===Abdominal Aortic Aneurysm===< | |||
< | |||
==Screening== | ==Screening== | ||
| Line 167: | Line 27: | ||
==Medical Treatment== | ==Medical Treatment== | ||
==Surgical Treatment== | ==Surgical Treatment== | ||
===Endovascular treatment of AAA=== | ===Endovascular treatment of AAA=== | ||
Revision as of 17:24, 13 July 2011
|
Aortic aneurysm Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Aortic aneurysm On the Web |
|
WikiDoc Resources for Aortic aneurysm |
|
Articles |
|---|
|
Most recent articles on Aortic aneurysm Most cited articles on Aortic aneurysm |
|
Media |
|
Powerpoint slides on Aortic aneurysm |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Aortic aneurysm at Clinical Trials.gov Trial results on Aortic aneurysm Clinical Trials on Aortic aneurysm at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Aortic aneurysm NICE Guidance on Aortic aneurysm
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Aortic aneurysm Discussion groups on Aortic aneurysm Patient Handouts on Aortic aneurysm Directions to Hospitals Treating Aortic aneurysm Risk calculators and risk factors for Aortic aneurysm
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Aortic aneurysm |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
| Cardiology Network |
 Discuss Aortic aneurysm further in the WikiDoc Cardiology Network |
| Adult Congenital |
|---|
| Biomarkers |
| Cardiac Rehabilitation |
| Congestive Heart Failure |
| CT Angiography |
| Echocardiography |
| Electrophysiology |
| Cardiology General |
| Genetics |
| Health Economics |
| Hypertension |
| Interventional Cardiology |
| MRI |
| Nuclear Cardiology |
| Peripheral Arterial Disease |
| Prevention |
| Public Policy |
| Pulmonary Embolism |
| Stable Angina |
| Valvular Heart Disease |
| Vascular Medicine |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [3] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
Overview
Pathology
The physical change in the aortic diameter can occur secondary to an intrinsic defect in the protein construction of the aortic wall, trauma, infection, or due to progressive destruction of aortic proteins by enzymes.
Signs, symptoms and diagnosis
Most intact aortic aneurysms do not produce symptoms. As they enlarge, symptoms such as abdominal pain and back pain may develop. Compression of nerve roots may cause leg pain or numbness. Untreated, aneurysms tend to become progressively larger, although the rate of enlargement is unpredictable for any individual. Rarely, clotted blood which lines most aortic aneurysms can break off and result in an embolus. They may be found on physical examination. Medical imaging is necessary to confirm the diagnosis.
Thoracic Aortic Aneurysm
===Abdominal Aortic Aneurysm===<
Screening
Medical Treatment
Surgical Treatment
Endovascular treatment of AAA
In the recent years, the endoluminal treatment of Abdominal Aortic Aneurysms has emerged as a minimally invasive alternative to open surgery repair. The first endoluminal exclusion of an aneurysm took place in Argentina by Dr. Parodi and his colleagues in 1991. The endovascular treatment of aortic aneurysms involves the placement of an endo-vascular stent via a percutaneous technique (usually through the femoral arteries) into the diseased portion of the aorta. This technique has been reported to have a lower mortality rate compared to open surgical repair, and is now being widely used in individuals with co-morbid conditions that make them high risk patients for open surgery. Some centers also report very promising results for the specific method in patients that do not constitute a high surgical risk group.
There have also been many reports concerning the endovascular treatment of ruptured Abdominal Aortic Aneurysms, which are usually treated with an open surgery repair due to the patient's impaired overall condition. Mid-term results have been quite promising. However, according to the latest studies, the EVAR procedure doesn't carry any overall survival benefit. [1]
Endovascular treatment of other aortic aneurysms
The endoluminal exclusion of aortic aneurysms has seen a real revolution in the very recent years. It is now possible to treat thoracic aortic aneurysms, abdominal aortic aneurysms (please see above) and other aneurysms in most of the body's major arteries (such as the iliac and the femoral arteries) using endovascular stents and avoiding big incisions. Still, in most cases the technique is applied in patients at high risk for surgery as more trials are required in order to fully accept this method as the gold standard for the treatment of aneurysms.[2]
Complications of Endovascular Treatment
Endoleak
- Endoleak is a complication of endovascular aneurysm repair.
- The endoleaks may continue to perfuse and pressurize the aneurysm sac, thereby conferring an ongoing risk of aneursym enlargement and/or rupture.
- Endoleaks are classified by the source of blood flow, and organized into five categories.[3] [4]
- I: Attachment site leaks
- II: Collateral vessel leaks
- III: Graft failure (i.e. midgraft hole, junctional leak or disconnect)
- IV: Graft wall porosity
- V: Endotension (with or without endoleak)
Images shown below are courtesy of RadsWiki and copylefted
-
Endoleak after Abdominal aortic aneurysm repair
-
Endoleak after Abdominal aortic aneurysm repair
-
Endoleak after Abdominal aortic aneurysm repair
Prevention
Attention to patient's general blood pressure, smoking and cholesterol risks helps reduce the risk on an individual basis. There have been proposals to introduce ultrasound scans as a screening tool for those most at risk: men over the age of 65.[5] [6]. The tetracycline antibiotic Doxycycline is currently being investigated for use as a potential drug in the prevention of aortic aneurysm due to its metalloproteinase inhibitor and collagen stabilizing properties.
Research
Stanford University is conducting research to gather information on AAA risk factors, and to evaluate the effectiveness of an exercise program at preventing the growth of small AAAs in older individuals. [4]
See Also
Videos on Abdominal Aortic Aneurysm
<youtube v=Sb1bM8MnpRk/>
<youtube v=9XPPbWsrtRA/>
<youtube v=ovGI2fYc_U8/>
Pathological Findings
-
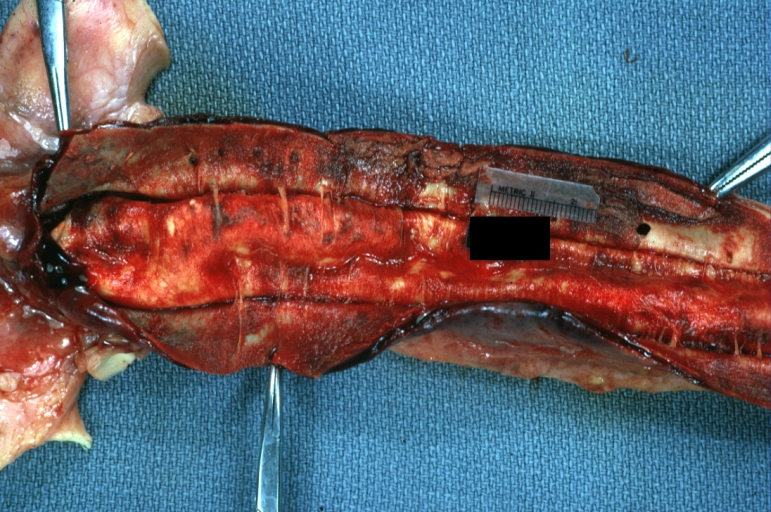
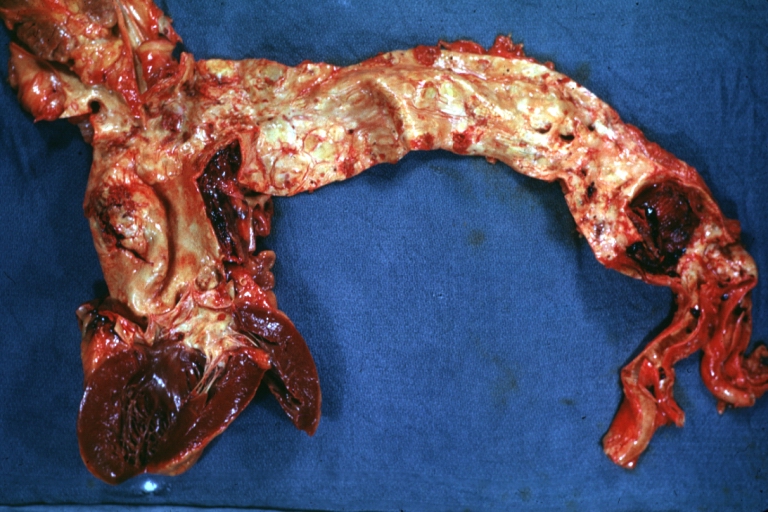
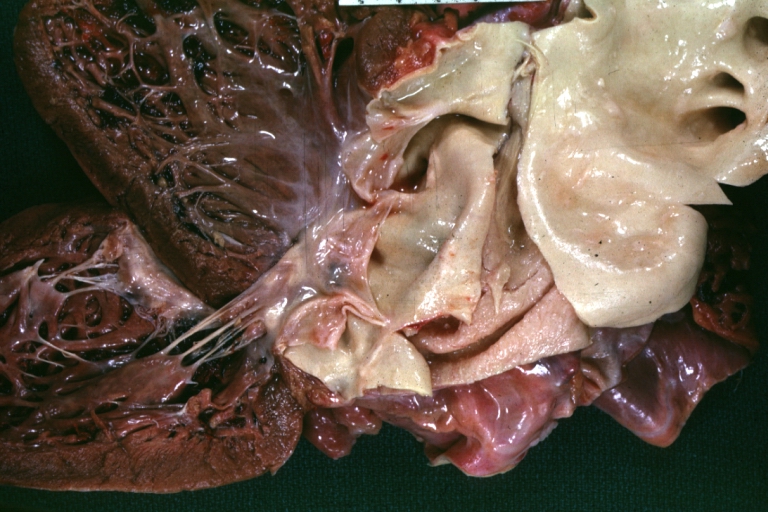
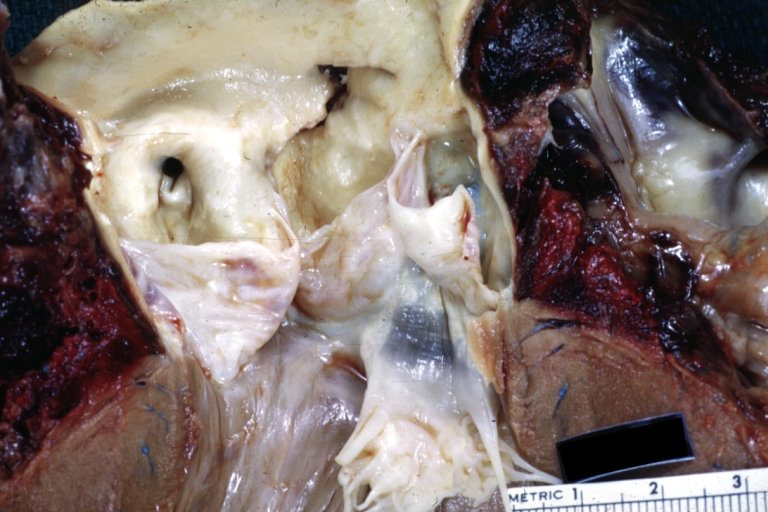
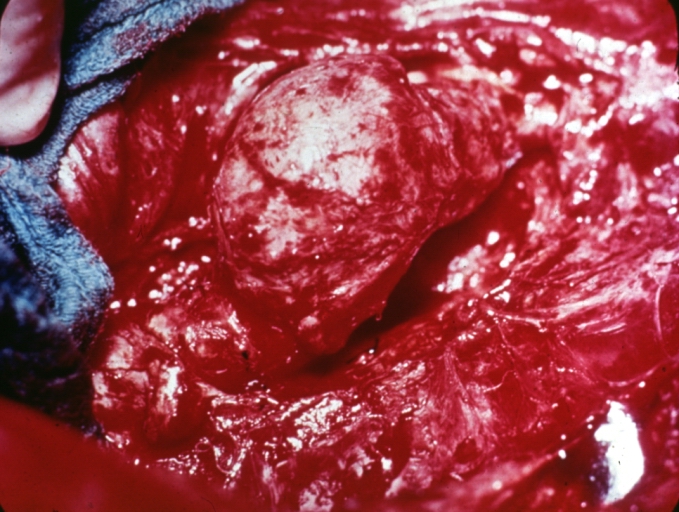
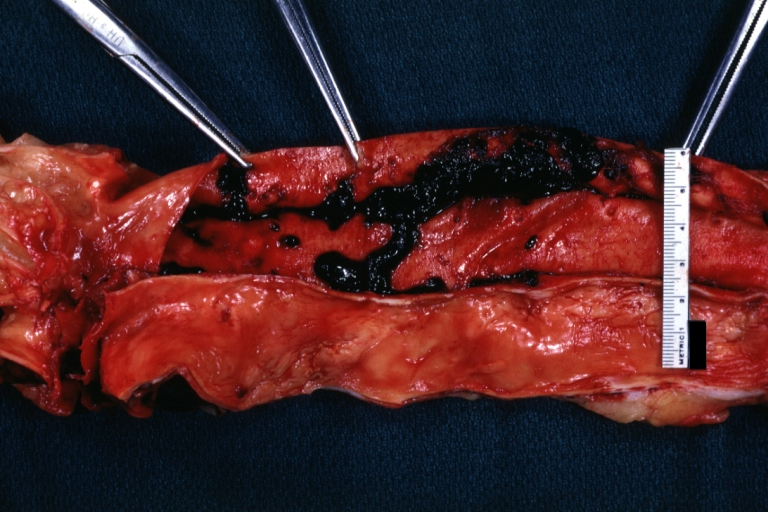
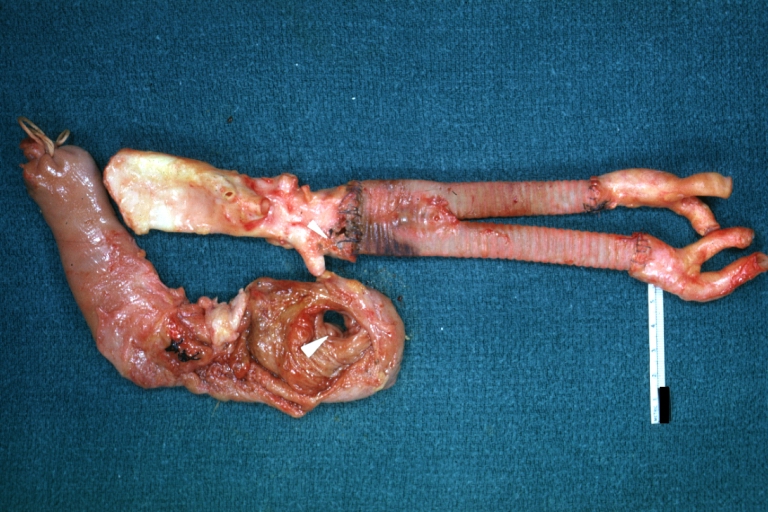
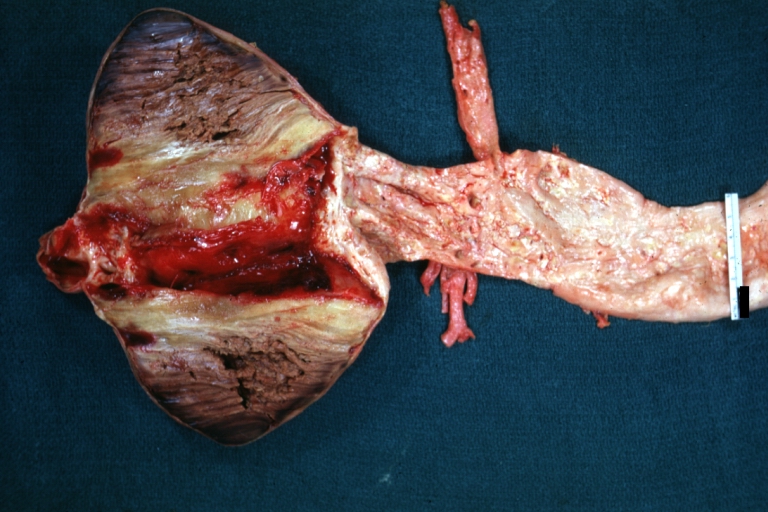
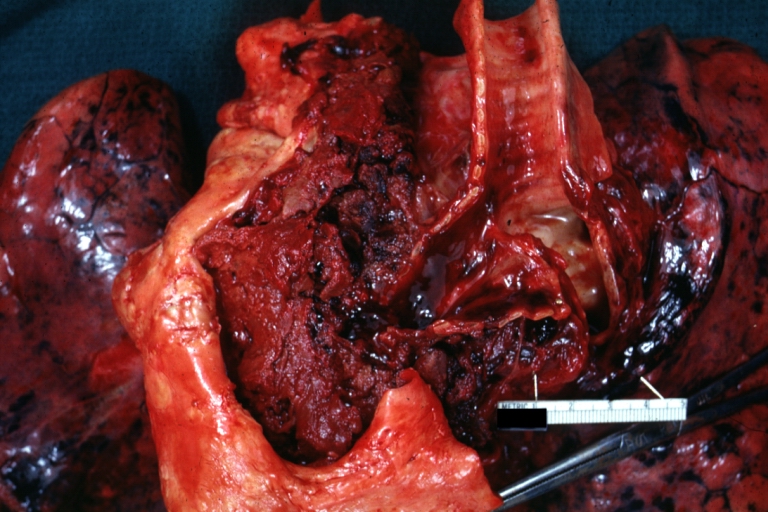
Dissecting Aneurysm: Gross very good example dissected channel has been opened
-
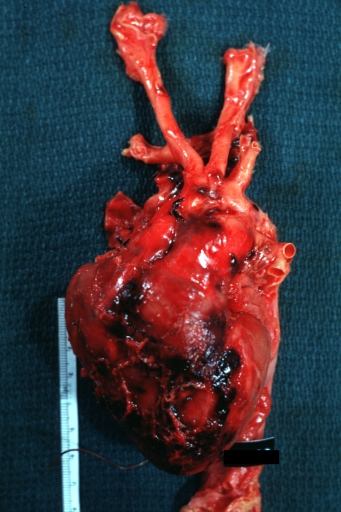
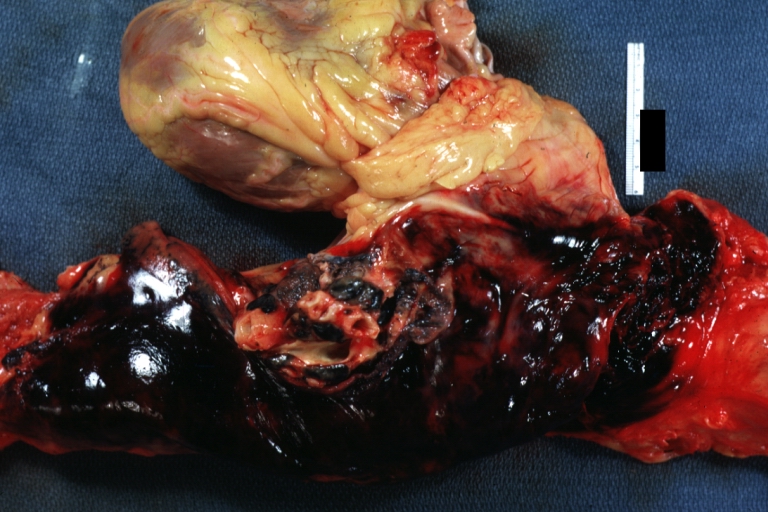
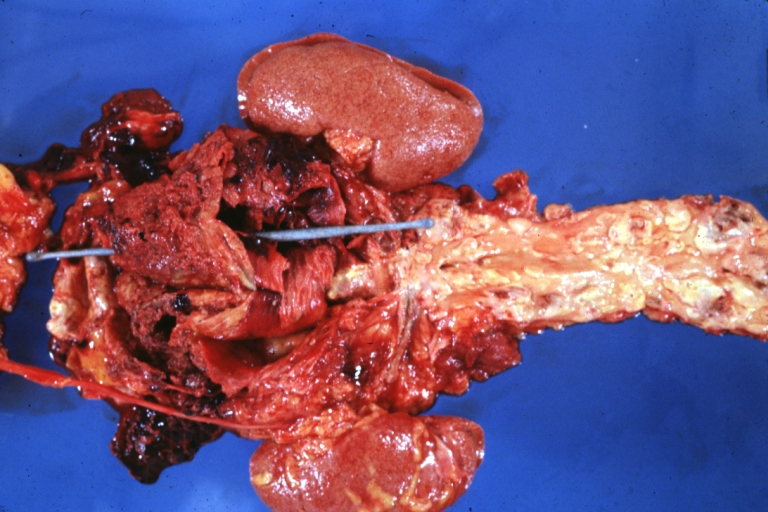
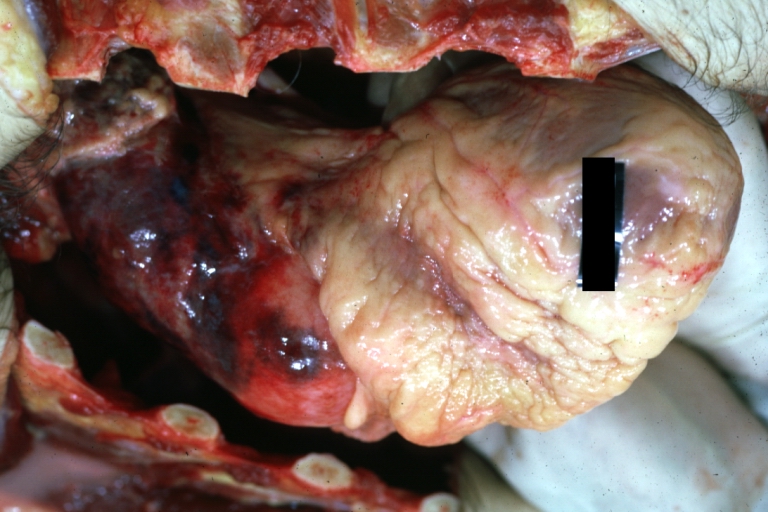
Dissecting Aneurysm: Gross external view good appearance from adventitia
-
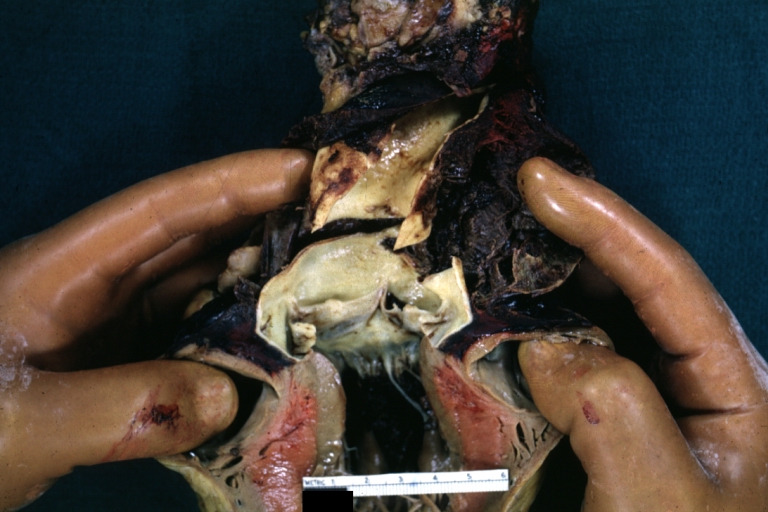
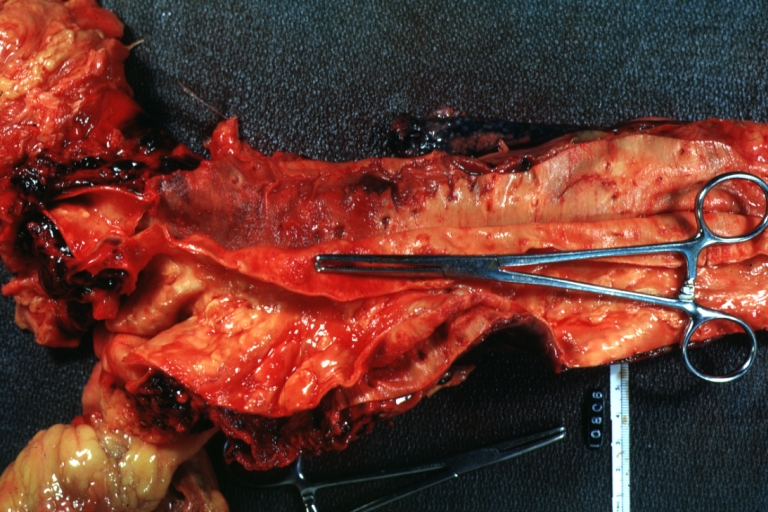
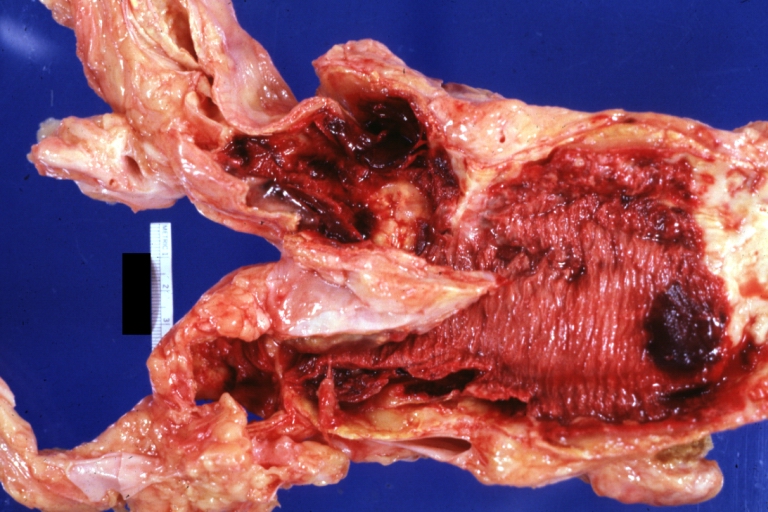
Dissecting Aneurysm: Gross opened false channel
-
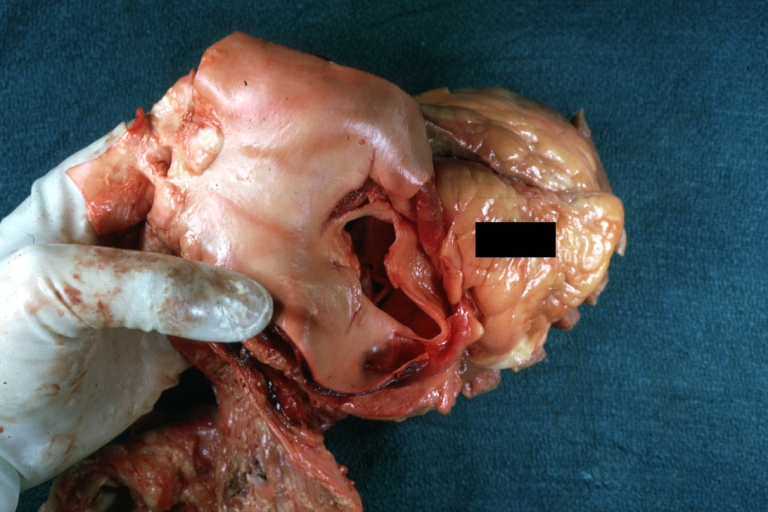
Dissecting Aneurysm: Gross good example dissection beginning at third portion aortic arch
-
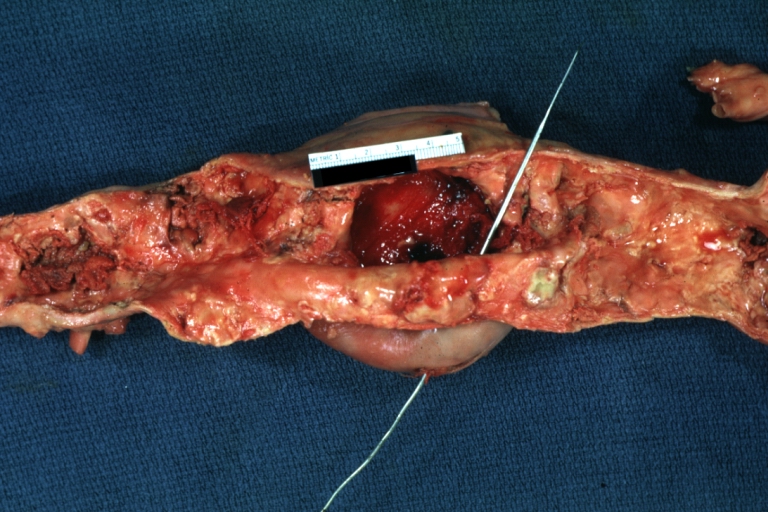
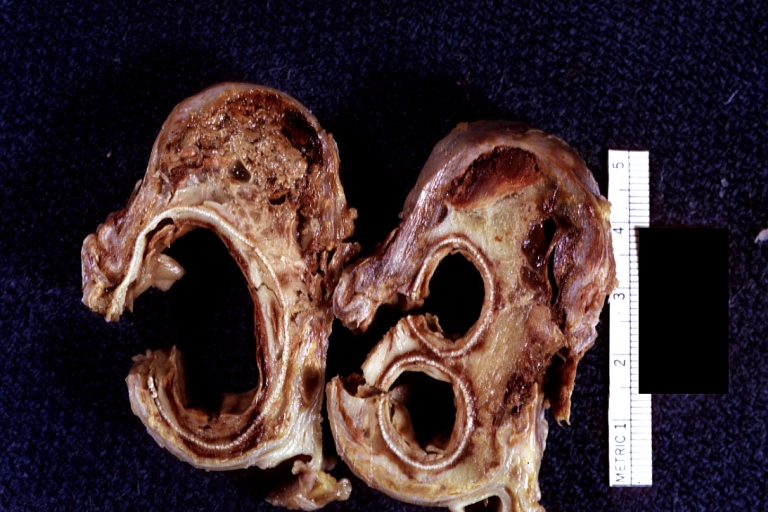
Dissecting Aneurysm: Gross cross sections showing thrombus in false lumen true lumen has been opened longitudinally
-
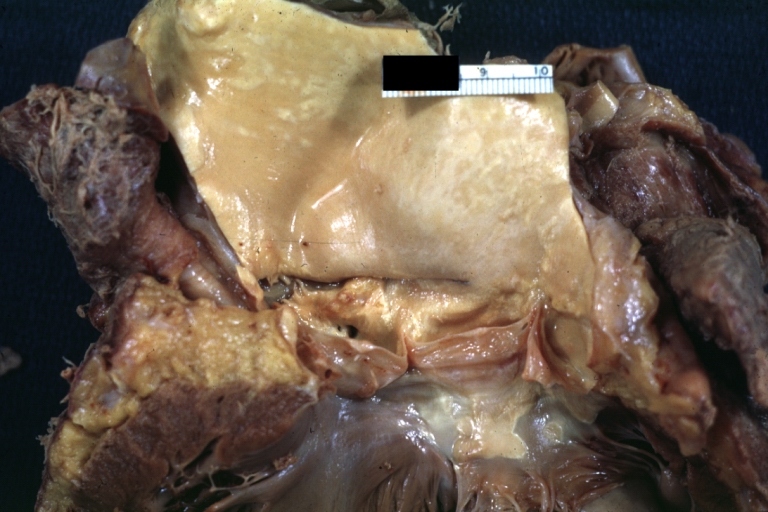
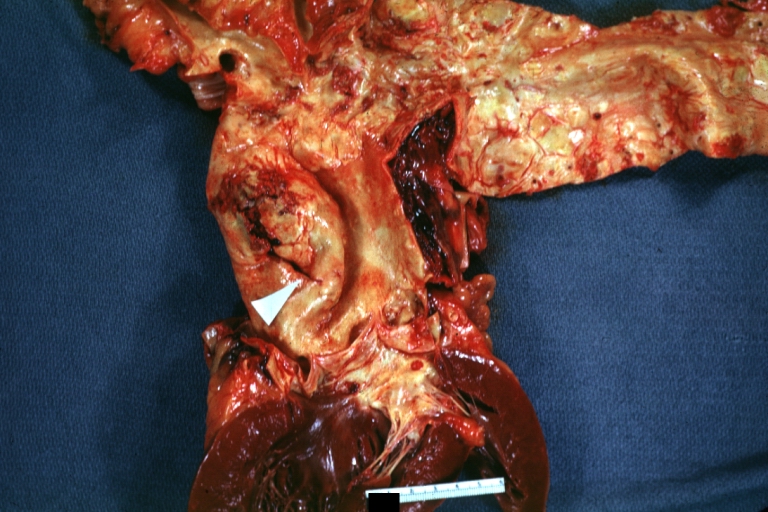
Dissecting Aneurysm: Gross shows origin just above aortic valve false channel shown in descending thoracic aorta (very good example)
-
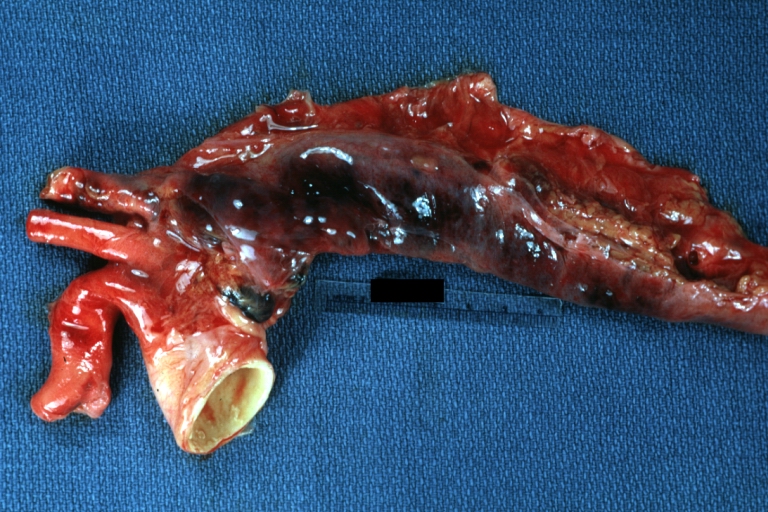
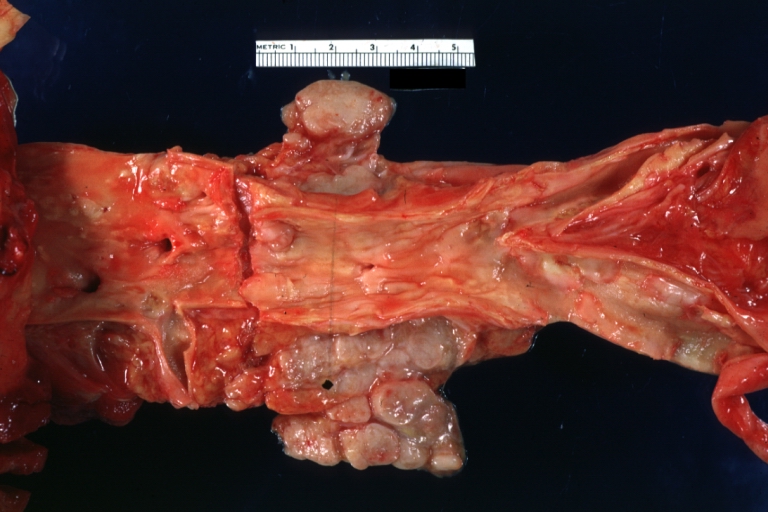
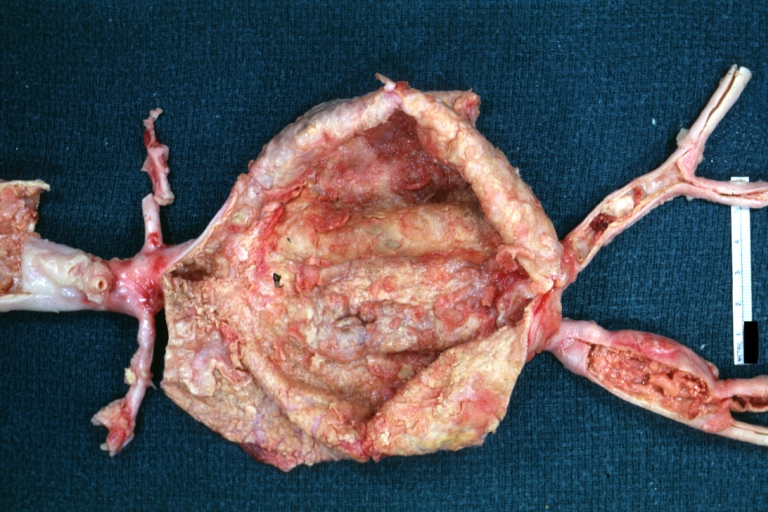
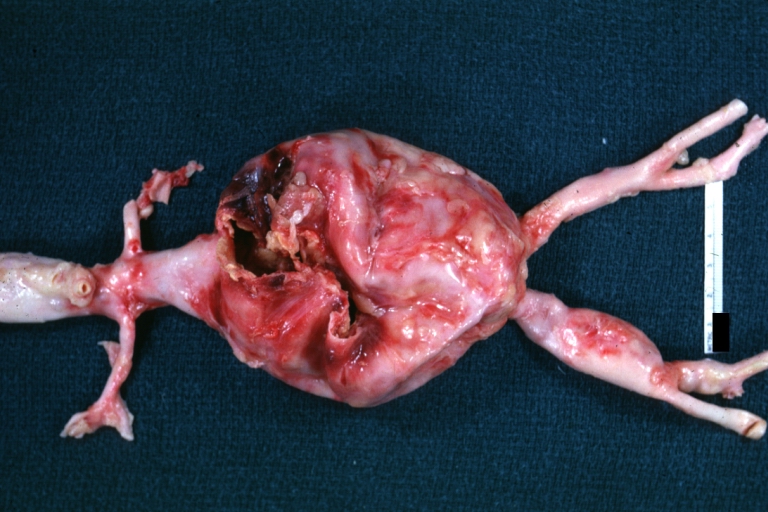
Atherosclerotic Aneurysm: Gross, a good example of typical abdominal aorta aneurysm with mural thrombus
-
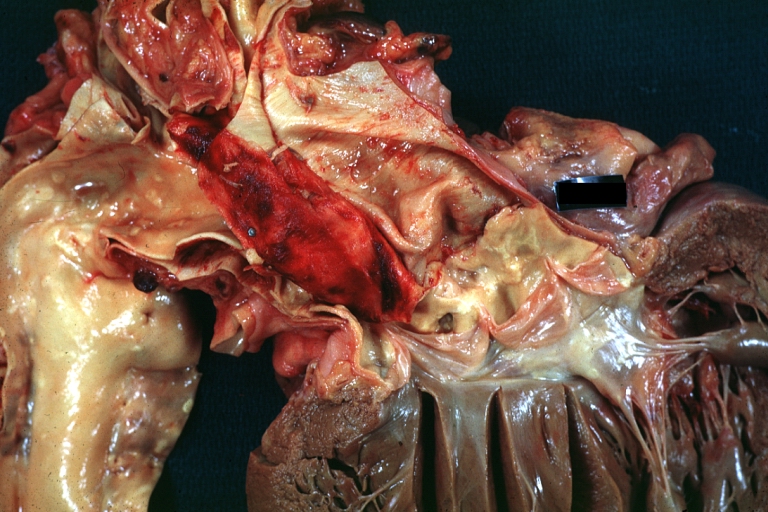
Dissecting Aneurysm: Gross, a very good example of dissection beginning just above aortic ring
-
Atherosclerotic Aneurysm: Gross, (rather) good example of abdominal aortic aneurysm
-
Dissecting Aneurysm: Gross, an excellent example, starting just above the aortic valve with reflection of aorta to show the dissection tract and some thrombus
-
Dissecting Aneurysm: Gross shows dilated aorta with extensive atherosclerosis dissection is seen, a small abdominal aorta atherosclerotic aneurysm is present good for association of dilation with dissection
-
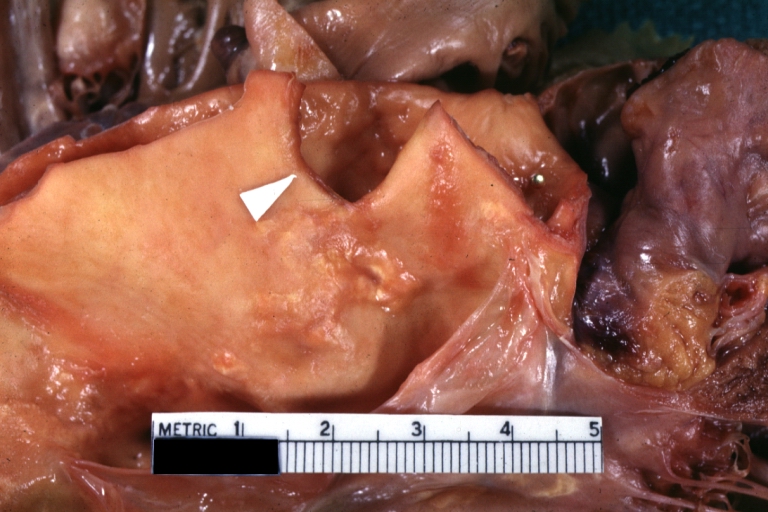
Dissecting Aneurysm: Gross arrow points to start of dissection in first portion aortic arch good but not the best example shows dilation
-
Dissecting Aneurysm: Gross, very good to show start of dissection above aortic valve and blood in false channel
-
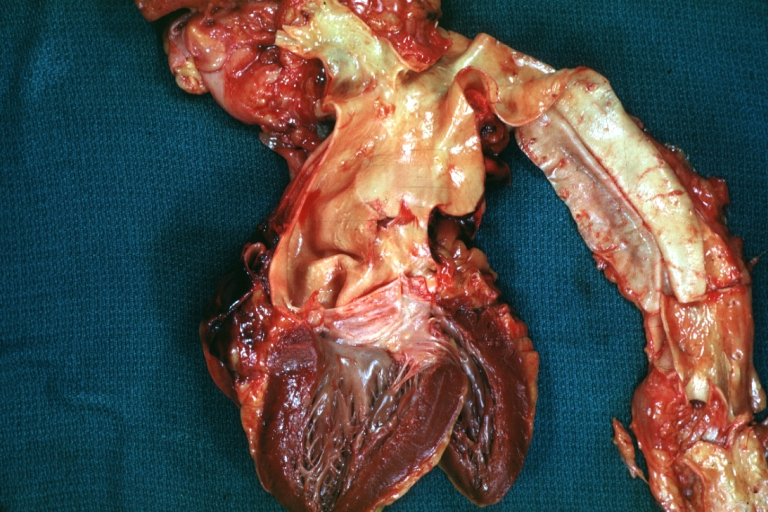
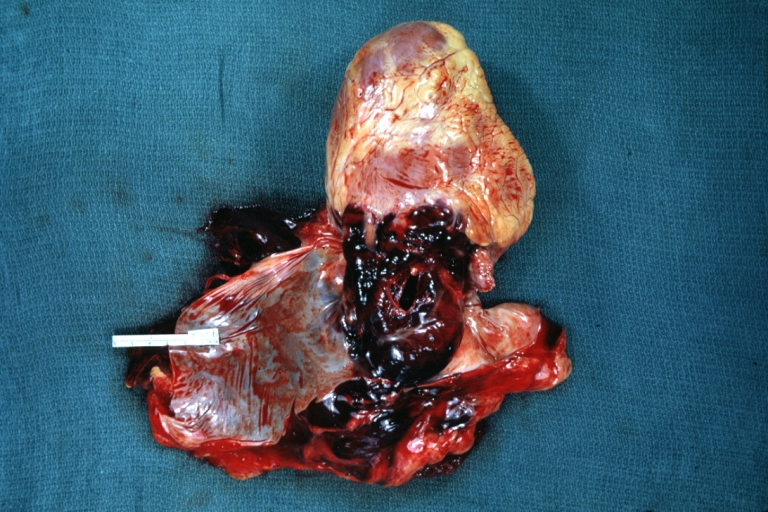
Dissecting Aneurysm: Gross, heart with root of aorta to show hemorrhage into pericardium (a very good example)
-
Dissecting Aneurysm: Gross, of heart and aorta with dissection and large false channel (a good example)
-
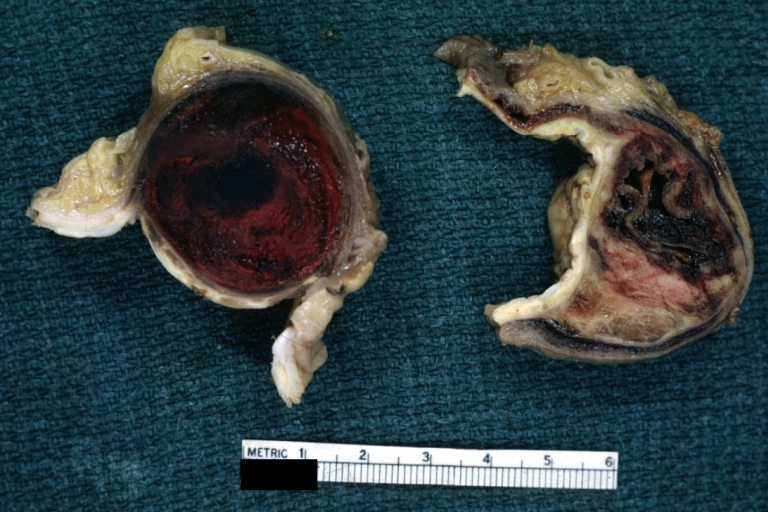
Dissecting Aneurysm: Gross cross section of aorta with two channels (a good example)
-
Atherosclerotic Aneurysm: Gross, a nice view of cross section of abdominal aorta aneurysm
-
Dissecting Aneurysm: Gross good example of typical angular tear above aortic valve
-
Dissecting Aneurysm: Gross good example angular tear above aortic valve
-
Atherosclerotic Aneurysm: Gross, external natural color very good example of an atherosclerotic thoracic aorta aneurysm with focal rupture
-
Atherosclerotic Aneurysm: Gross, excellent color, opened thoracic segment of aorta with two saccular atherosclerotic ruptured aneurysms
-
Atherosclerotic Aneurysm: Gross, an excellent example, natural color, external view of typical thoracic aortic aneurysms
-
Atherosclerotic Aneurysm: Gross unopened lesion natural color
-
Dissecting Aneurysm: Gross dissection first portion of arch fixed specimen (a good example)
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
Dissecting Aneurysm: Gross, rather well shown dissection in first portion of the aortic arch
-
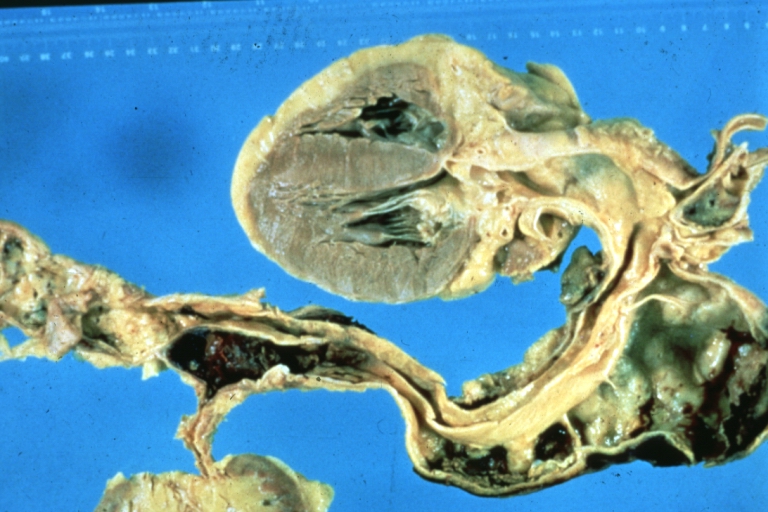
Dissecting Aneurysm: Gross, an excellent example of type I lesion
-
Dissecting Aneurysm: Gross, external view, an excellent example
-
Dissecting Aneurysm: Gross, Type I shows false channel
-
Dissecting Aneurysm: Gross, opened to show false channel (good example)
-
Atherosclerotic Aneurysm: Gross, very good example of ruptured thoracic segment
-
Dissecting Aneurysm: Gross, coagulum of blood in false channel
-
Dissecting Aneurysm: Gross, aortic valve area dissection (well shown, typical lesion)
-
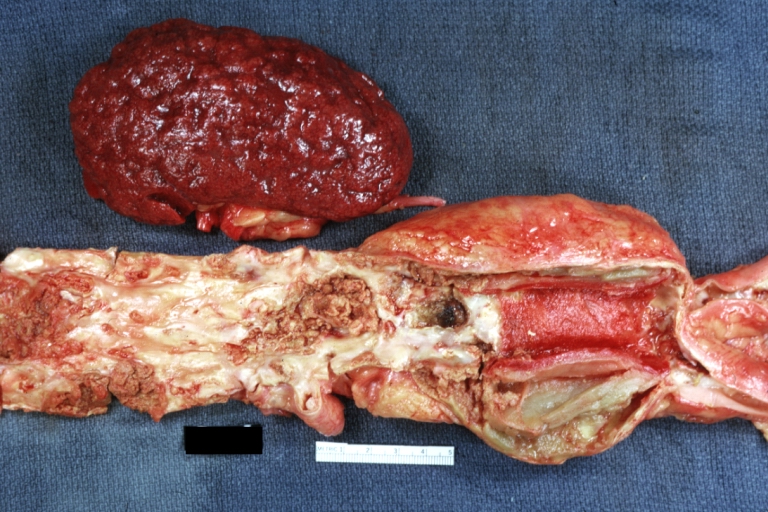
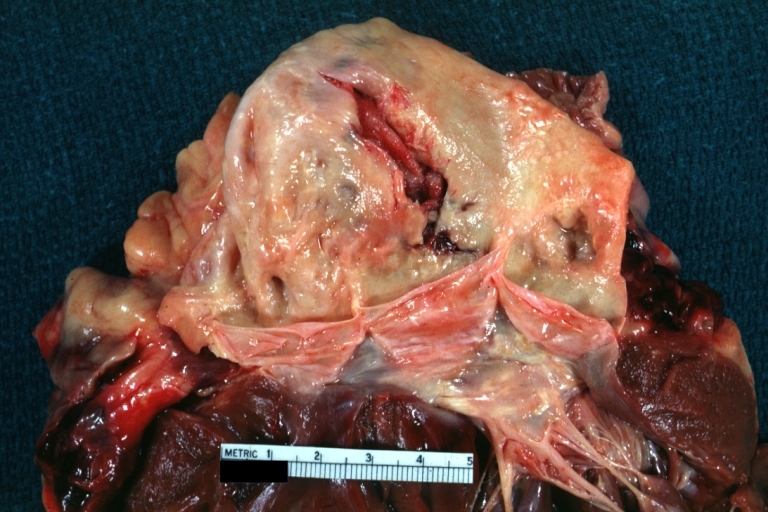
Abdominal Aneurysm Ruptured: Gross (good example) opened kidneys in marked place, atherosclerosis in lower thoracic aorta
-
Abdominal Aneurysm: Gross, (very good example) opened lesion with mural thrombus
-
Dissecting Aneurysm: Gross, large tear in first portion of aortic arch, annuloaortic ectasis
-
Dissecting Aneurysm: Gross, external view of heart and first portion of aortic arch, annuloaortic ectasia, hemorrhage beneath adventitia is evidence of dissection
-
Atherosclerotic Aneurysm Infected: Gross, infected abdominal aneurysm at superior suture line with rupture into duodenum
-
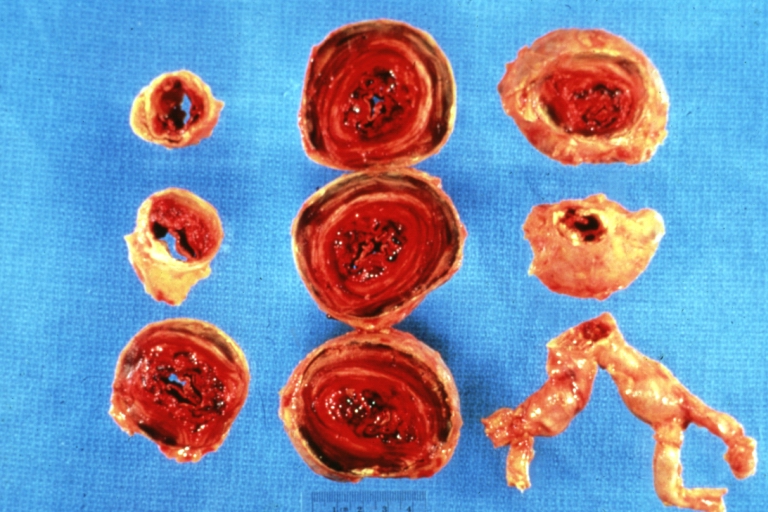
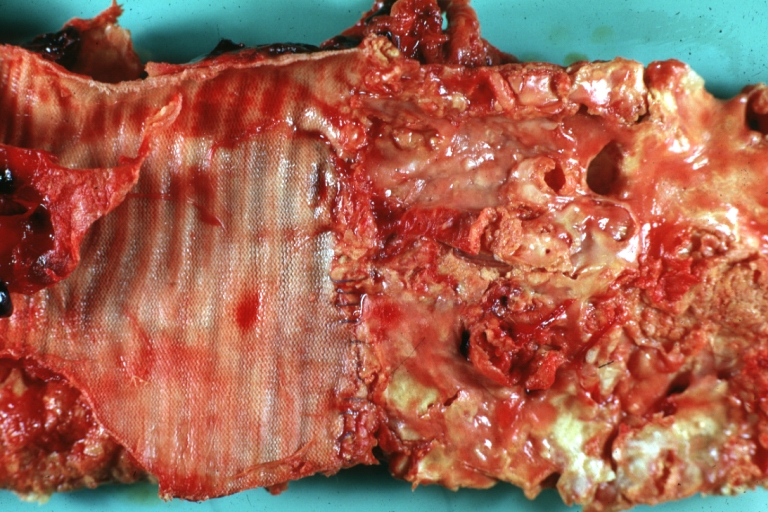
Atherosclerotic Aneurysm: Gross, cross sections of repaired aneurysm showing Dacron graft and old mural thrombus. A nice example of fibrin layer in graft
-
Ruptured Syphilitic Aneurysm
-
Dissecting Aneurysm in a patient with Marfan's syndrome
-
Traumatic Aneurysm
-
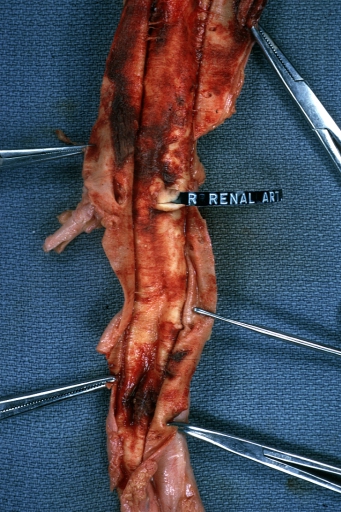
Kidney: Arteriosclerosis: Gross aorta with well shown renal artery containing large plaque and kidney with multiple cortical scars and atrophy also abdominal aorta aneurysm with mural thrombus (excellent example for renovascular hypertension)
-
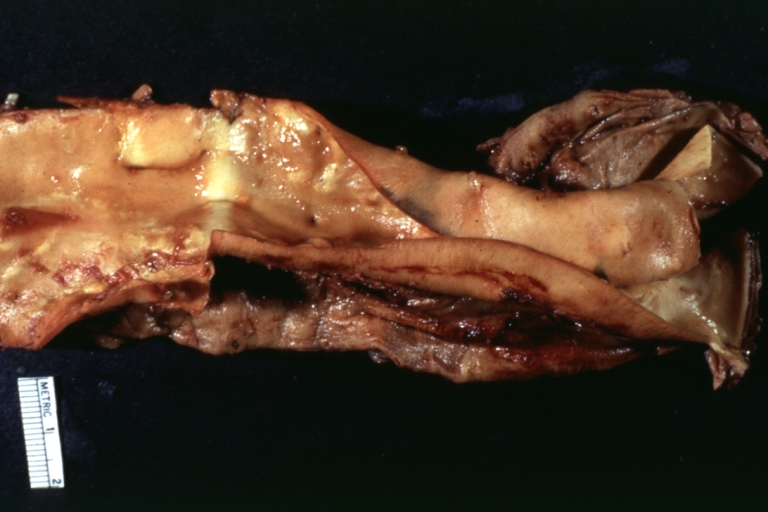
Dissecting Aneurysm: Gross, fixed tissue, descending thoracic segment dissection opened to show the false channel. The true surface is also visible
-
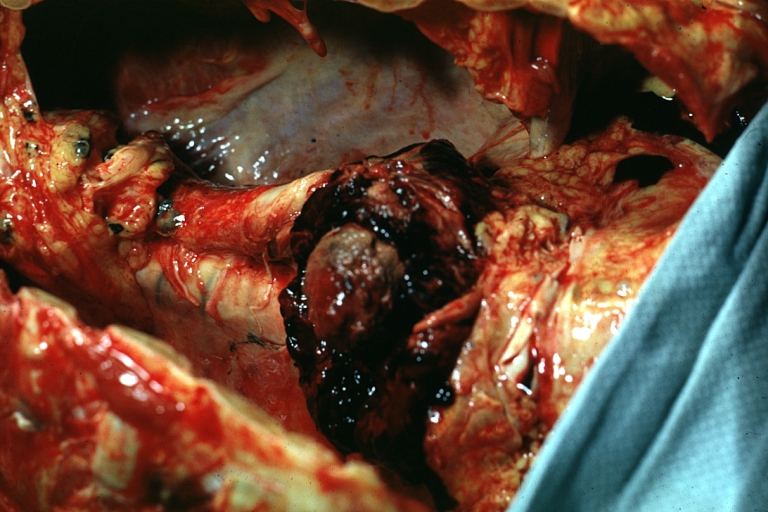
Aneurysm: Gross, ruptured thoracic aorta aneurysm, in situ lower thoracic portion (probably due to atherosclerosis)
-
Abdominal Aneurysm Graft Repair: Gross, natural color, close-up view, an excellent example of Dacron graft that has been in place for years with pseudointima and atherosclerosis
-
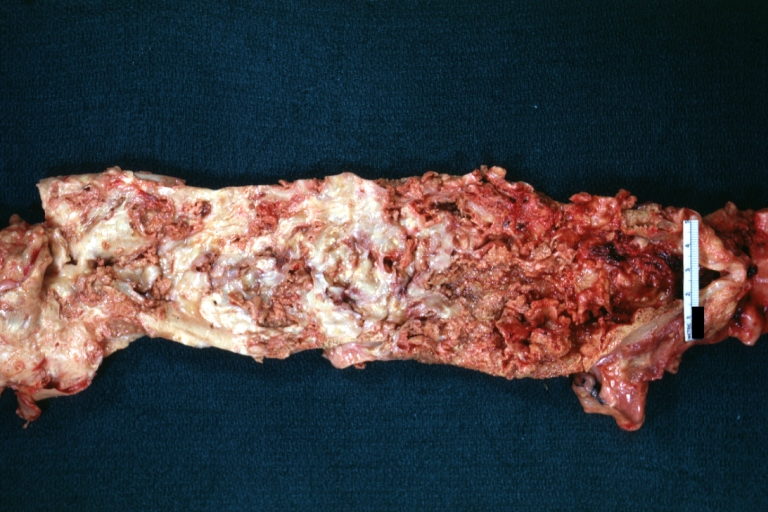
Dacron Graft: Gross, close-up Dacron graft to repair aneurysm. Aorta completely covered with a calcified and ulcerated plaque with small mural thrombi (an excellent depiction of proximal suture line)
-
Dissecting Aneurysm: Gross natural color descending aorta opened into false channel
-
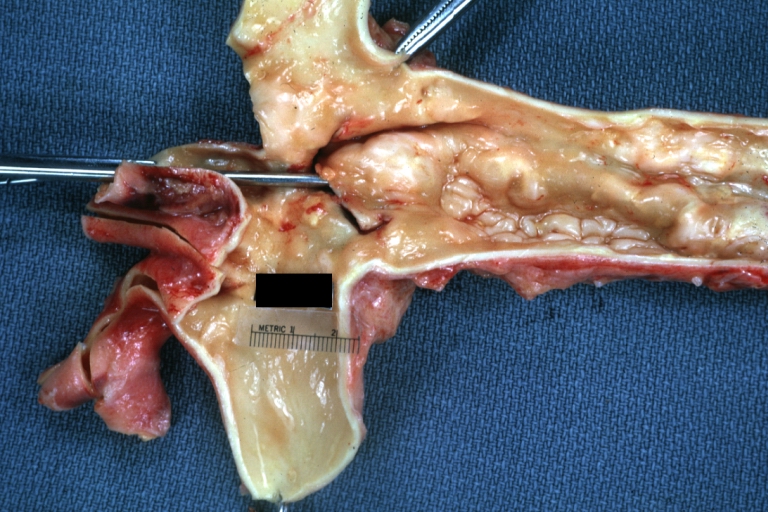
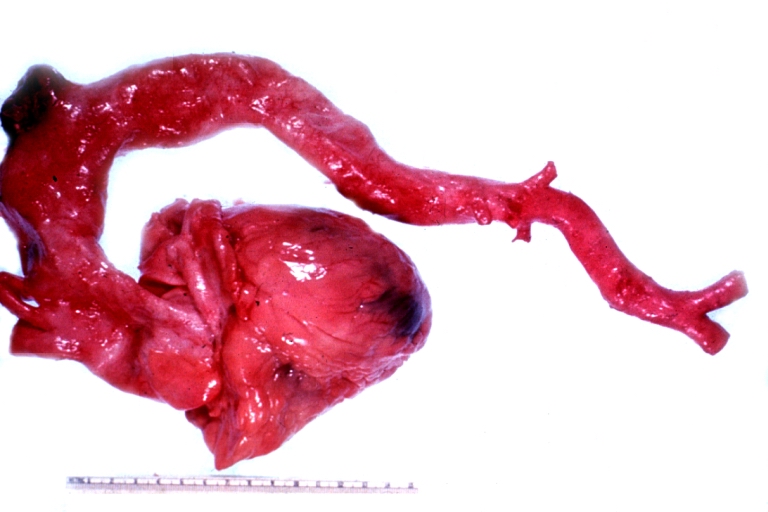
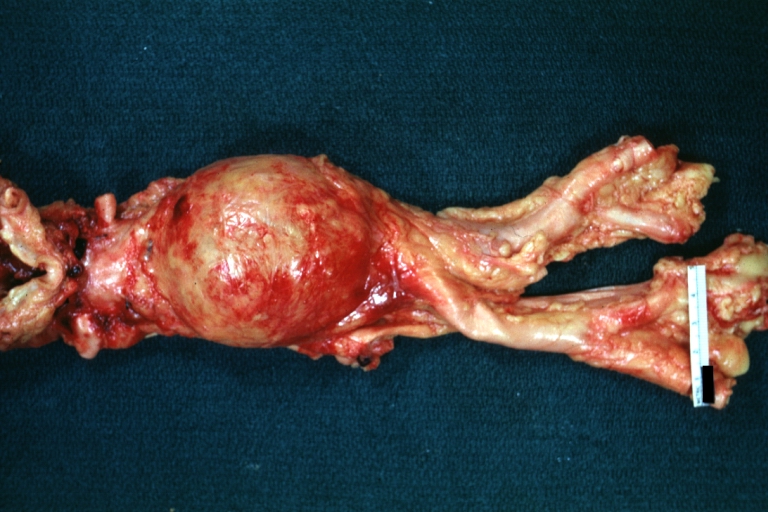
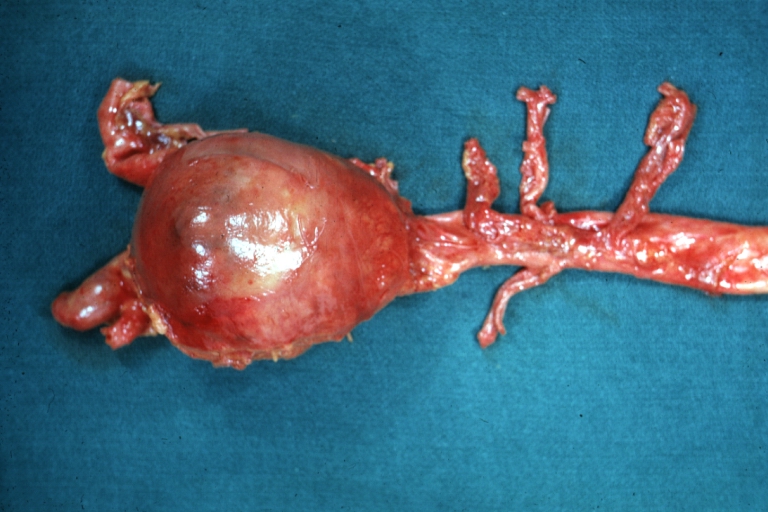
Abdominal Aneurysm: Gross, natural color, unopened specimen with about a six centimeter aneurysm between renals and bifurcation (a very good example of opened aneurysm)
-
Abdominal Aneurysm: Gross, natural color, an opened aneurysm showing quite well laminated thrombus
-
Atherosclerosis with Mural Thrombi: Gross, natural color, a nice photo of descending thoracic aorta with extensive ulcerated plaques and mural thrombi in distal portion. The case also has an abdominal aneurysm
-
Pseudoaneurysm Ruptured Into Duodenum: Gross natural color aorta and duodenum with arrow pointing to rupture point of aortobifemoral bypass pseudoaneurysm rupture and another in duodenum a very good demonstration of this very well known complication of aortic prostheses
-
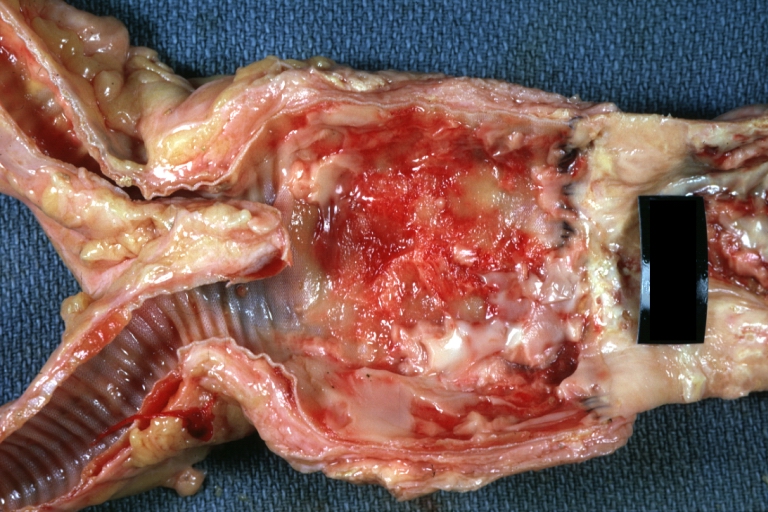
Abdominal Aneurysm: Gross, natural color, large aneurysm opened showing sessile calcified plaques with no mural thrombus. Lesion extends from renal arteries to the bifurcation (the same lesion seen externally with focus of rupture)
-
Abdominal Aneurysm Ruptured: Gross, natural color, external view with large area of apparent rupture. Aorta is opened to show this aneurysm)
-
Abdominal Aneurysm: Gross, natural color, unopened large and quite typical aneurysm extending from below renal arteries to bifurcation
-
Abdominal Aneurysm: Gross, natural color, opened aneurysm with well shown and typical laminated thrombus (external view)
-
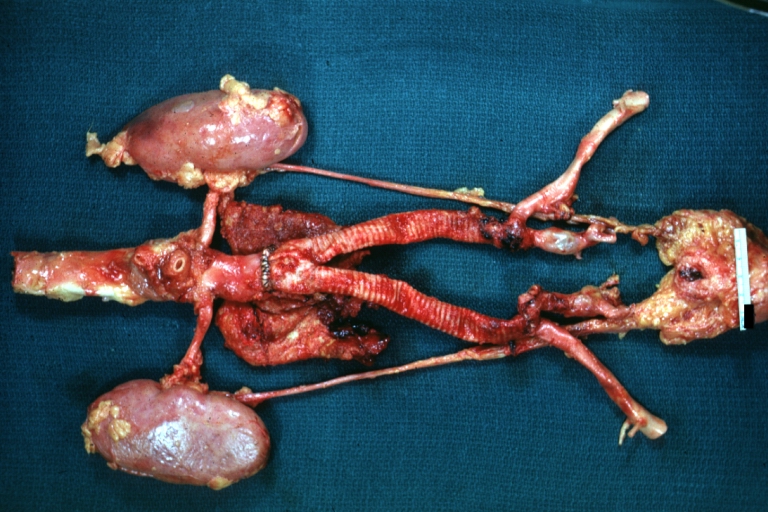
Aortobifemoral Prosthesis: Gross, natural color, nice dissection showing Dacron prosthesis replacing abdominal segment of aorta with portion of atherosclerotic aneurysm with renal arteries and kidneys
-
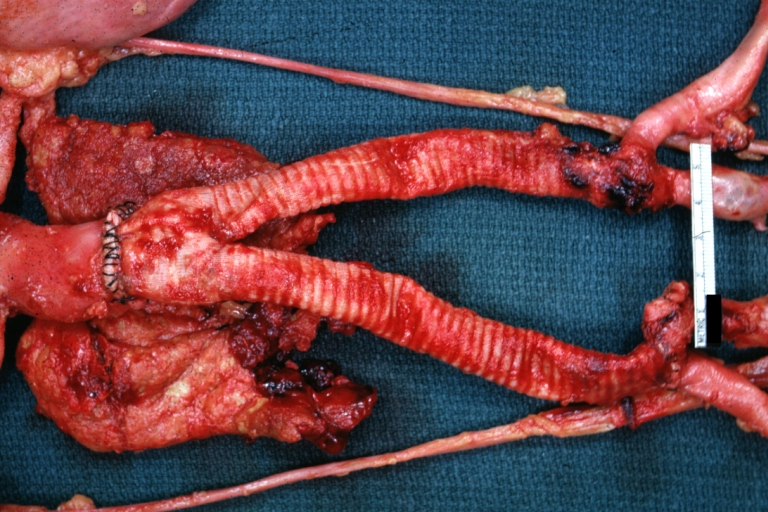
Aortobifemoral Prosthesis: Gross natural color close-up view of nicely dissected prosthesis extending from below renals to common iliac arteries portion of atherosclerotic aneurysm behind prosthesis
-
Dissecting Aneurysm: Gross natural color close-up view of aortic valve and proximal aortic arch with ruptured intima rather good illustration of this lesion
-
Syphilitic Aneurysm: Gross natural color rather a close-up view and outstanding photo of aneurysm ruptured into the left main stem bronchus
-
Syphilitic Aneurysm: Gross natural color typical tree barking in aorta aneurysm opening is seen in which is a thrombus aneurysm ruptured into left main stem bronchus (shown very well)
-
Dissecting Aneurysm Chronic: Gross natural color first portion of aortic arch with intimal rent well shown with healed margins and view into false channel that shows a surface looking like atherosclerosis which is known to develop in a chronic dissection
-
Dissecting Aneurysm Chronic: Gross, natural color, closer view of the previous one (a very good example)
References
- ↑ Rutherford RB.: Randomized EVAR Trials and Advent of Level I Evidence: A Paradigm Shift in Management of Large Abdominal Aortic Aneurysms? (abstract) Semin Vasc Surg. 2006 Jun;19(2):69-74. PMID: 16782510
- ↑ Saratzis N, Melas N, Lazaridis J, Ginis G, Antonitsis P, Lykopoulos D, Lioupis A, Gitas C, Kiskinis D. Endovascular AAA repair with the aortomonoiliac EndoFit stent-graft: two years' experience. J Endovasc Ther. 2005 Jun;12(3):280-7
- ↑ Baum, Richard A., Stavropoulos, S. William, Fairman, Ronald M., Carpenter, Jeffrey P. Endoleaks after Endovascular Repair of Abdominal Aortic Aneurysms. J Vasc Interv Radiol 2003 14: 1111-1117.
- ↑ Stavropoulos, S. William, Clark, Timothy W.I., Carpenter, Jeffrey P., Fairman, Ronald M., Litt, Harold, Velazquez, Omaida C., Insko, Erik, Farner, Michael, Baum, Richard A. Use of CT Angiography to Classify Endoleaks after Endovascular Repair of Abdominal Aortic Aneurysms. J Vasc Interv Radiol 2005 16: 663-667.
- ↑ Routine screening in the management of AAA, UK Department of Health study Report
- ↑ Abdominal Aortic Aneurysm screening, a review by Bandolier, a UK independent source of evidence-based healthcare information for both healthcare professionals and consumers. Bandolier 27-3 Article
Template:SIB it:Aneurisma aortico fi:Aortta-aneurysma