|
|
| (46 intermediate revisions by 8 users not shown) |
| Line 3: |
Line 3: |
| Name = Brugada syndrome | | | Name = Brugada syndrome | |
| Image = BrugadaS.jpg| | | Image = BrugadaS.jpg| |
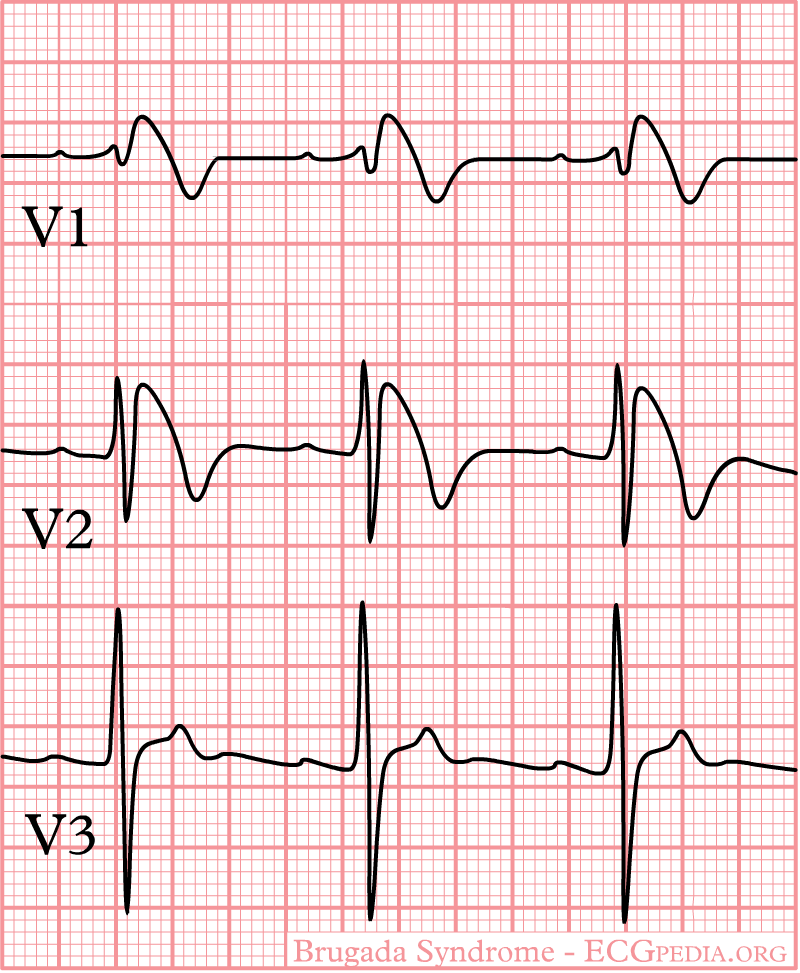
| Caption = ECG findings of Brugada Syndrome| | | Caption = ECG in Type I Brugada Pattern| |
| DiseasesDB = 31999 |
| |
| ICD10 = {{ICD10|I|42|8|i|30}} |
| |
| ICD9 = {{ICD9|746.89}} |
| |
| ICDO = |
| |
| OMIM = 601144 |
| |
| MedlinePlus = |
| |
| MeshID = D053840 |
| |
| }} | | }} |
| [[Image:Brugada 3.1.jpg|right|thumb|400px|right|ECG pattern in Brugada syndrome. According to a recent consensus document, type 1 ST segment elevation either spontaneously present or induced with [[Ajmaline]]/[[Flecainide]] test is considered diagnostic. Type 1 and 2 may lead to suspicion but drug challenge is required for diagnosis. The ECGs in the right and left panels are from the same patient before (right panel, type 1) and after (left panel, type 1) endovenous administration of 1 mg/kg of Ajmaline during 10 minutes.]] | | '''For patient information, click [[Brugada syndrome (patient information)|here]]''' |
| | |
| {{Brugada syndrome}} | | {{Brugada syndrome}} |
|
| |
|
| {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} | | {{CMG}}; '''Associate Editor-In-Chief:''' {{CZ}} |
|
| |
|
| {{SK}} Sudden unexpected death syndrome; SUDS | | {{SK}} Sudden unexpected death syndrome; sudden unexplained death syndrome; SUDS; sudden unexpected nocturnal death syndrome; sudden unexplained nocturnal death syndrome; SUNDS; in the Phillipines ''bangungut'' (to rise and moan in sleep); in Thailand ''lai tai''; in Laos ''Dab tsog'' and in Japan ''Pokkuri disease'' |
| ==Differential Diagnosis==
| |
| | |
| ==Electrocardiography==
| |
| | |
| In some cases, the disease can be detected by observing characteristic patterns on an [[electrocardiogram]], which may be present all the time, or might be elicited by the administration of particular drugs (e.g., Class IC antiarrythmic drugs that blocks sodium channels and causing appearance of ECG abnormalities - [[ajmaline]], [[flecainide]]) or resurface spontaneously due to as yet unclarified triggers. The pattern seen on the ECG is persistent ST elevations in the electrocardiographic leadsV<sub>1</sub>-V<sub>3</sub> with a [[right bundle branch block]] ([[RBBB]]) appearance with or without the terminal S waves in the lateral leads that are associated with a typical [[RBBB]]. A prolongation of the [[PR interval]] (a conduction disturbance in the heart) is also frequently seen.The electrocardiogram can fluctuate over time, depending on the autonomic balance and the administration of antiarrhythmic drugs. Adrenergic stimulation decreases the [[ST segment]] elevation, while vagal stimulation worsens it. (There is a case report of a patient who died while shaving, presumed due to the vagal stimulation of the carotid sinus massage!) The administration of class Ia, Ic and III drugs increases the [[ST segment]] elevation, and also fever. Exercise decreases [[ST segment]] elevation in some patients but increases it in others (after exercise when the body temperature has risen). The changes in heart rate induced by atrial pacing are accompanied by changes in the degree of [[ST segment]] elevation. When the heart rate decreases, the [[ST segment]] elevation increases and when the heart rate increases the [[ST segment]] elevation decreases. However, the contrary can also be observed.
| |
| | |
| ==Characteristics==
| |
|
| |
|
| *Characterized by a coved-type ST-segment elevation in the right precordial leads
| | ==[[Brugada syndrome overview|Overview]]== |
| *The Brugada ECG is often concealed, but can be unmasked or modulated by a number of drugs and pathophysiological states including sodium channel blockers, a febrile state, vagotonic agents, tricyclic antidepressants, as well as cocaine and Propranolol intoxication.
| |
|
| |
|
| ==Genetics== | | ==[[Brugada syndrome classification|Classification]]== |
|
| |
|
| # SCN5A is a gene that encodes the alpha sodium unit of the cardiac sodium channel. Mutations in SCN5A account for about 15-30% of Brugada syndrome cases. A negative genetic test for SCN5A does not exclude that SCN5A is causing the clinical syndrome because the genetic tests do not evaluate for mutations in promotors, cryptic splicing mutations, or gross rearrangements in the protein product.
| | ==[[Brugada syndrome historical perspective|Historical Perspective]]== |
| # Glycerol-3-phosphate dehydrogenase (GPD1L) is associated with progressive conduction disease and low sensitivity to procainamide resulting from decreased Isodium current. It has a relatively good prognosis.
| |
| # CACNA1C (alpha subunit of L-type cardiac calcium channel) and CACNB2b (beta subunit of L-type cardiac calcium channel) is associated with a shortened QT interval and a combinatin Brugada/Short QT interval syndrome.
| |
|
| |
|
| ==Lithium Treatment and Brugada Syndrome== | | ==[[Brugada syndrome pathophysiology|Pathophysiology]]== |
| Administration of [[Lithium]] can result in EKG manifestations of the Brugada syndrome. <ref>Pirotte MJ, Mueller JG, Poprawski T. A case report of Brugada-type electrocardiographic changes in a patient taking lithium. Am J Emerg Med. 2008; 26: 113.</ref><ref>Wright D, Salehian O. Brugada-Type Electrocardiographic Changes Induced by Long-Term Lithium Use. Circulation, FRCPC2010;122:e418-e419</ref>. [[Syncope]] and [[sudden cardiac death]] have been observed in these patients.<ref>Laske C, Soekadar SR, Laszlo R, Plewnia C. Brugada syndrome in a patient treated with lithium. Am J Psychiatry. 2007; 164: 1440–1441. </ref> The putative role of [[lithium]] has been suggested in so far as withdrawal of [[lithium]] results in either 1) normalization of the ECG or 2) conversion of the Brugada pattern to type 2 or 3. The appearance of Brugada type EKG patterns does not require toxic [[lithium]] levels.
| |
|
| |
|
| ==Brugada EKG== | | ==[[Brugada syndrome differential diagnosis|Differentiating Brugada syndrome from other Diseases]]== |
|
| |
|
| # Type 1 ST segment elevation is diagnostic of Brugada syndrome and is characterized by a coved ST-segment elevation ≥2 mm (0.2 mV) followed by a negative T wave.
| | ==[[Brugada syndrome epidemiology and demographics|Epidemiology and Demographics]]== |
| # Type 2 ST-segment elevation has a saddleback appearance with a high take-off ST-segment elevation of ≥2 mm followed by a trough displaying ≥1 mm ST elevation followed by either a positive or biphasic T wave.
| |
| # Type 3 ST-segment elevation has either a saddleback or coved appearance with an ST-segment elevation of <1 mm.
| |
|
| |
|
| <div align="left">
| | ==[[Brugada syndrome risk factors|Risk Factors]]== |
| <gallery heights="125" widths="125">
| |
| Image:BrugadaS.jpg|General characteristics
| |
| Image:Brugada.jpg|EKG of a Patient with Brugada Syndrome
| |
| Image:Brugada_lead_placement.jpg|Lead placements
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| <div align="left">
| | ==[[Brugada syndrome screening|Screening]]== |
| <gallery heights="125" widths="125">
| |
| Image:Brugada_syndrome_type1_example.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example2.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example3.jpg|Brugada Type 1
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| <div align="left">
| | ==[[Brugada syndrome natural history, complications and prognosis|Natural History, Complications and Prognosis]]== |
| <gallery heights="125" widths="125">
| |
| Image:Brugada_syndrome_type1_example4.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example5.jpg|Brugada Type 1
| |
| Image:Brugada_syndrome_type1_example6.jpg|Brugada Type 1
| |
| </gallery>
| |
| </div>
| |
|
| |
|
| <div align="left">
| | ==Brugada syndrome diagnosis|Diagnosis== |
| <gallery heights="125" widths="125">
| | [[Brugada syndrome diagnostic criteria|Diagnostic Criteria]] | [[Brugada syndrome history and symptoms|History and Symptoms]] | [[Brugada syndrome physical examination|Physical Examination]] | [[Brugada syndrome laboratory findings|Laboratory Findings]] | [[Brugada syndrome electrocardiogram|Electrocardiogram]] | [[Brugada syndrome chest x ray|Chest X Ray]] | [[Brugada syndrome echocardiography or ultrasound|Echocardiography or Ultrasound]] | [[Brugada syndrome electrophysiologic studies|Electrophysiologic Studies]] | [[Brugada syndrome genetic testing|Genetic Testing]] |
| Image:Brugada_syndrome_type2_example1.jpg|Brugada Type 2
| |
| Image:Brugada_syndrome_type2_example2.jpg|Brugada Type 2
| |
| Image:Brugada EKG Schema.jpg|(A) Normal electrocardiogram pattern in the precordial leads V<sub>1-3</sub>, (B) changes in Brugada syndrome (type B)
| |
| </gallery>
| |
| </div>
| |
| | |
| ==Diagnosis==
| |
| | |
| * Diagnosed when a Type 1 ST-segment elevation is observed in more than one right precordial lead (V1-V3), in the presence or absence of sodium channel blocking agent, and in conjunction with one or more of the following:
| |
| # Family history of SCD (<45 years old)
| |
| # Documented VF
| |
| # Polymorphic ventricular tachycardia
| |
| # Coved-type ECGs in family members
| |
| # Inducibility of VT with programmed electrical stimulation (PES)
| |
| # Syncope
| |
| # Nocturnal agonal respiration
| |
| * Diagnosis is also considered positive when a Type 2 (saddleback pattern) or Type 3 ST-segment elevation is observed in more than one right precordial lead under baseline conditions and can be converted to the diagnostic Type 1 pattern occurs upon exposure to sodium channel blocker.
| |
| | |
| ==Sodium Challenge==
| |
| | |
| * Drugs that can be used
| |
| ** Ajmaline 1 mg/kg/5 min IV
| |
| ** Flecainide 2 mg/kg/10 min IV or 400 mg PO
| |
| ** Procainamide 10 mg/kg/10 min IV
| |
| ** Pilsicainide 1 mg/kg/10 min IV
| |
| * The sodium challenge should be terminated when
| |
| # Diagnostic Type 1 ST-segment elevation or Brugada ECG, develops
| |
| # ST segment in Type 2 increases by ≥2 mm
| |
| # Premature ventricular beats or other arrhythmias develop
| |
| # QRS widens to ≥130% of baseline
| |
| | |
| ==Arrhythmias==
| |
| | |
| # Polymorphic VT resembling a rapid Torsade de Pointes (TdP)
| |
| # Monomorphic VT is observed infrequently
| |
| # VT/VF often terminates spontaneously in patients with the Brugada syndrome which may explain why patients wake up at night after episodes of agonal respiration caused by the arrhythmia.
| |
| | |
| ==Risk Statification==
| |
| | |
| * Patients with syncope and an abnormal Type 1 ECG are at higher risk
| |
| * Asymptomatic patients at risk can be identified
| |
| ** Presence of spontaneous Type 1 ST-segment elevation
| |
| ** Characteristics of the S wave
| |
| ** Presence of late potentials
| |
| ** Inducibility of VT/VF using PES.
| |
|
| |
|
| ==Treatment== | | ==Treatment== |
| | [[Brugada syndrome medical therapy|Medical Therapy]] | [[Brugada syndrome drugs to avoid|Drugs to Avoid]] | [[Brugada syndrome drugs to preferably avoid|Drugs to Preferably Avoid]] | [[Brugada syndrome cost-effectiveness of therapy|Cost-Effectiveness of Therapy]] | [[Brugada syndrome future or investigational therapies|Future or Investigational Therapies]] |
|
| |
|
| The cause of death in Brugada syndrome is [[ventricular fibrillation]].The episodes of syncope (fainting) and sudden death (aborted or not) are caused by fast polymorphic ventricular tachycardias or ventricular fibrillation. These arrhythmias appear with no warning. While there is no exact treatment modality that reliably and totally prevents ventricular fibrillation from occurring in this syndrome, treatment lies in termination of this lethal [[arrhythmia]] before it causes death. This is done via implantation of an [[implantable cardioverter-defibrillator]] (ICD), which continuously monitors the heart rhythm and will [[defibrillation|defibrillate]] an individual if ventricular fibrillation is noted. Some recently performed studies had evaluated the role of quinidine, a Class Ia antiarrythmic drug, for decreasing VF episodes occurring in this syndrome. Quinidine was found to decrease number of VF episodes and correcting spontaneous ECG changes, possibly via inhibiting I</sup>to channels.<ref name="pmid15381640">{{cite journal |author=Belhassen B, Glick A, Viskin S |title=Efficacy of quinidine in high-risk patients with Brugada syndrome |journal=Circulation |volume=110 |issue=13 |pages=1731–7 |year=2004 |pmid=15381640 |doi=10.1161/01.CIR.0000143159.30585.90}}</ref> Those with risk factors for [[coronary artery disease]] may require an angiogram before ICD implantation.
| | ==Case Studies== |
| | [[Brugada syndrome case study one|Case #1]] |
|
| |
|
| * Aborted sudden death are at high risk for recurrence and should receive an ICD
| | ==Related Chapters== |
| * VT storm has been successfully treated with Isoproterenol. The mechanism is thought to be augmenting the cardiac L type channel.
| |
| * Asymptomatic patients require risk stratification and clinical judegement to help guide therapy
| |
| * Quinidine (class IA sodium channel blocker) blocks the Ito current and is proven to suppress spontaneous VF
| |
| * Cilostazol (phosphodiesterase III inhibitor that increases inward L type calcium channel current and reported to suppress spontaneous VF
| |
| * Bepridil suppress spontaneous VF probably through blocking Ito current
| |
| * Medical therapy alone with the above agents is currently not evaluated in randomized trials and should not be used as loan therapy.
| |
| | |
| ==See also== | |
| * [[Cardiac action potential]] | | * [[Cardiac action potential]] |
| * [[Genetics]] | | * [[Genetics]] |
| * [[Ion channel]] | | * [[Ion channel]] |
| * [[Tambocor]] | | * [[Tambocor]] |
|
| |
| ==References==
| |
| {{Reflist|2}}
| |
|
| |
| ==External links==
| |
| * [http://www.genetests.org/profiles/brugada GeneReviews: Brugada syndrome]
| |
| * Algado et al: http://www.medspain.com/ant/n13_jun00/Brugada.htm
| |
| * Behr: http://www.c-r-y.org.uk/long_qt_syndrome.htm
| |
| * [http://www.brugada.org The Ramon Brugada Senior Foundation ]
| |
| * http://digilander.libero.it/martini_syndrome/
| |
|
| |
|
| {{Electrocardiography}} | | {{Electrocardiography}} |
| Line 158: |
Line 60: |
| [[zh:布魯格達氏症候群]] | | [[zh:布魯格達氏症候群]] |
| [[tr:Brugada sendromu]] | | [[tr:Brugada sendromu]] |
| | |
| | {{WikiDoc Help Menu}} |
| | {{WikiDoc Sources}} |
| | [[CME Category::Cardiology]] |
|
| |
|
| [[Category:Electrophysiology]] | | [[Category:Electrophysiology]] |
| Line 163: |
Line 69: |
| [[Category:Channelopathy]] | | [[Category:Channelopathy]] |
| [[Category:Genetic disorders]] | | [[Category:Genetic disorders]] |
|
| |
| {{WikiDoc Help Menu}}
| |
| {{WikiDoc Sources}}
| |