Renal vein thrombosis
| Renal vein thrombosis | |
 | |
|---|---|
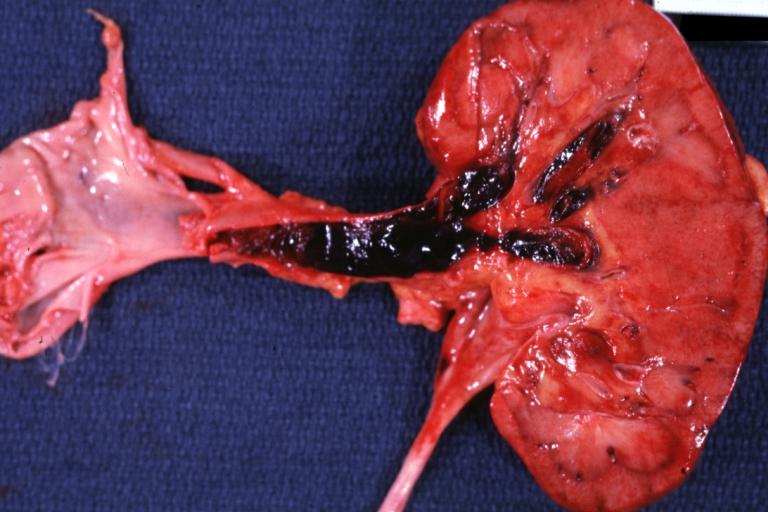
| Transplant with Renal Vein Thrombosis: Gross; natural color, opened kidney and vein. Image courtesy of Professor Peter Anderson DVM PhD and published with permission © PEIR, University of Alabama at Birmingham, Department of Pathology | |
| ICD-10 | I82.3 |
| ICD-9 | 453.3 |
| DiseasesDB | 11359 |
| MedlinePlus | 000513 |
For patient information page, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Saeedeh Kowsarnia M.D.[2]
Overview
Renal vein thrombosis (RVT) is the formation of a clot or thrombus obstructing the renal vein. Rayer was the first to describe thrombosis of renal vein in nephrotic patients during postpartum. Based on the onset of symptoms renal vein thrombosis can be classified into acute and chronic.
Historical perspectives
- In 1837, thrombosis of the renal vein was first described in nephrotic patients by Rayer in postmortem evaluations.
- In 1843, Robinson induced renal vein thrombosis in rats.
- In 1876, Buchwald and Litten observed renal vein thrombosis in dogs.
- In 1939, Derow, Schlesinger, and Savitz presented a case of renal vein thrombosis in nephrotic syndrome.
Classification
| Renal vein thrombosis | ||
|---|---|---|
| Onset | Presentation | Etiology |
| Acute |
|
|
| Chronic |
|
|
- Based on the location RVT may be unilateral or bilateral.
- Left renal vein involvement is more common than right renal vein.
Pathophysiology
Mechanisms which are responsible for developing renal vein thrombosis are classified into three categories: Vascular damage, venous stasis, and hypercoagulable state.
- Vascular endothelial damage: Vascular injury leads to exposure of tissue factor, collagen, and endothelium to the blood, causing activation of the extrinsic pathway of coagulation [4] [5].
- Stasis: Normal endothelium has anticoagulation activity driven by thrombomodulin, endothelial protein C receptor ( EPCR), tissue factor pathway inhibitor and heparin-like proteoglycans. The major determinant of anticoagulation activity in the blood is the ratio of endothelial cell surface to blood volume [6]. Stasis of blood in greater vessels means decreased exposure of anticoagulants of the endothelial surface to the blood which results in promoting thrombi formation.
- Hypercoagulable state: As a definition, any laboratory abnormalities or clinical conditions which can be associated with an increased risk of thrombosis or clinical presentation of recurrent thrombosis without predisposing factors is considered hypercoagulability. Hypercoagulability (thrombophilia) includes hereditary and acquired conditions which enhance a tendency for developing thrombi in the veins, arteries, or both. Renal vein thrombosis can also be secondary to nephrotic syndrome, particularly membranous nephropathy due to loss of proteins in urine like antithrombins.
Causes
Causes
| Classification | Conditions |
|---|---|
| Vascular damage | Homocystinuriaand (hyperhomocysteinemia), trauma (kidney biopsy, endovascular intervention), Kidney transplant, Liver transplant, surgery |
| Hypercoagulability | Contraceptives, Hypovolemia, systemic lupus erythematosus, antiphospholipid syndrome (the most prevalent hypercoagulable state), dehydration especially in male pediatric cases, inherited coagulopathy, anticoagulation therapy [7], thromboembolic events (septic emboli), factor V Leiden (FVL) mutation, prothrombin gene G20210A mutations, elevated factor VIII, protein C and protein S deficiency, nephrotic syndrome, collagen vascular disease, amyloidosis, disseminated malignancy, sepsis, myeloproliferative diseases (Polycythemia vera, essential thrombocythemia), paroxysmal nocturnal hemoglobinuria, Behçet's syndrome |
| Stasis | Compression (retroperitoneal processes such as retroperitoneal fibrosis and abdominal neoplasms), malignancy (especially renal cell carcinoma [8] [9]) |
Differentiating Renal vein thrombosis
| Conditions | Presentation | Lab finding | Diagnosis | |
|---|---|---|---|---|
| Renal infarction |
|
| ||
| Renal calculi |
|
| ||
| Pyelonephritis | Acute |
|
|
|
| Chronic |
|
|
| |
| Renal cell carcinoma | The unnamed parameter 2= is no longer supported. Please see the documentation for {{columns-list}}. 2 |
|
| |
| Renal papillary necrosis |
Predisposing factors: Diabetes, pyelonephritis, renal calculi, hemoglobinopathies, analgesic abuse, tuberculosis, renal transplant rejection, liver cirrhosis, tumors |
|
| |
| Renal artery dissection |
Predisposing factors: Trauma, endovascular intervention, fibromuscular dysplasia, atherosclerosis, smoking |
|
| |
| Ectopic pregnancy |
|
|
| |
| Loin pain hematuria syndrome |
|
|
| |
Epidemiology and Demographics
Malignancy especially renal cell carcinoma is the most common etiology consists of
Prevalence of renal vein thrombosis in nephrotic syndrome is 5 to 60% [10] .Membranous nephropathy is responsible for 20 to 60 % of the cases which makes it the most common cause of renal vain thrombosis among nephrotic syndromes. Other etiologies like minimal change disease, membranoproliferative glomerulonephritis, and focal segmental glomerulosclerosis cause 10 to 50 % of the cases [11] .
Risk Factors
Screening
- Screening should be done for patients
- Who present with signs of renal infarct
- Who has chronic bilateral RVT with worsening creatinine and proteinuria to see whether anticoagulation is necessary
- There is no beneficial evidence regarding screening in patients with nephrotic syndrome and overt embolism.
Natural History, Complications, and Prognosis
Complications:
- Acute renal failure
- End stage renal failure
- Pulmonary embolism
- DVT
- Portal vein occlusion (portal hypertension)
- Sepsis
- Ipsilateral adrenal gland hemorrahge
Factors that determine prognosis in renal vein thrombosis:
- Baseline renal function
- Renal function of the contralateral kidney
- Adequacy of treatment
- Speed of the developed thrombose
- Severity and progression of underlying causes
Diagnosis
Signs and Symptoms
Imaging
- Doppler ultrasonography: Diagnostic screening
- Renal venography: Gold standard test for RVT diagnosis
- CT angiography: 100% sensitive for diagnosis
- Spiral computed tomography (CT) with contrast
- Magnetic resonance imaging (MRI)
Treatment
Therapy in RVT [14] [15] [16] [17] [18] [19] [20] :
| Classification | Condition |
|---|---|
| Fibrinolytic therapy and catheter thrombectomy |
|
| Surgery |
|
| Anticoagulation therapy |
Prophylaxy:
|
|
Asymptomatic RVT | |
|
Thrombotic events: DVT or PE with or without RVT in high risk cases and acute RVT with or without other thrombotic events (DVT, PE)
|
† ATRIA risk score [21]= Anticoagulation and Risk Factors in Atrial Fibrillation
ATRIA score for predicting bleeding associated with warfarin:
low-risk = (0 to 3 points) patients have hemorrhage rates of 1% per year
Intermediate risk = patients have hemorrhage rates of less than 5% per year
High-risk = (5 to 10 points) patients have hemorrhage rates of more than 5% per year
Related Chapters
Renal vein thrombosis in pediatrics
Renal vein thrombosis as one of the venous thromboebolic event, is more common in pediatric population due to lower renal perfusion pressure, anticoagulant deficiency, and renal venous anatomy [22] [23] [24] [25] [26] [27] [28] [29] [30] [31] [32] [33] [34] [35] [36].
| Renal vein thrombosis in childhood | |
|---|---|
| Rate | Prevalence: 15–20% of neonatal VTE
Incidence of neonatal RVT: ~2.2/100,000 live birth Nearly 21% failure of renal transplantation in pediatric is due to RVT (leading cause) Neonatal RVT: Unilateral in 70% of cases (64% of those occurred in left side), males in 67% of cases |
| Risk factors | Neonatal risk factor: Perinatal asphyxia, hypotension, sepsis, congenital heart disease, and thrombophilia, polycythemia
Maternal risk factors: Diabetes, hypertension, and polyhydramnios Graft-associated RVT: Young recipient age, pre-transplant peritoneal dialysis, previous transplant |
| Cause | Decreased renal blood flow, increased blood viscosity, hyperosmolality, hypercoagulability, sickle cell disease, indwelling catheter
Factor V Leiden the most common inherited coagulopathy in neonatal RVT |
| Presentation | Neonatal purpura fulminans: Extensive venous and arterial thromboses and ecchymoses, laboratory evidence of DIC
Macroscopic hematuria, thrombocytopenia, and palpable abdominal mass |
| Diagnosis | Doppler ultrasonography is the modality of choice |
| Natural history | First presentation: Enlarged kidney with loss of cortico-medullary differentiation and perivascular echogenic streaking within the arcuate and interlobular veins
Next: Thrombosis can be seen in the renal vein and IVC Eventually: Significant proportion of kidneys become atrophic |
| Outcome | kidney dimensions as predictive of outcome. Each 1 mm increase in kidney length predicts a 3 mL/min/1.73m2 loss in glomerular filtration rate |
| Complications | In the next 3.7 years: 71% progress renal atrophy, 19% develop hypertension, 3% require renal replacement therapy |
| Treatment | Supportive care with serial imaging, another approach is 6–12 weeks of anticoagulation use for unilateral RVT with no renal function impairment and no IVC involvement
Anticoagulation for unilateral RVT with extension into the IVC for 6–12 weeks Thrombolysis followed by anticoagulation, another recommendation is to use anticoagulation alone for bilateral RVT with evidence of renal function impairment RVT risk assessment scale for follow-up the cases has to be done biannually for ≥ 5 years to assess renal function [37] |
References
- ↑ F. Velasquez Forero, N. Garcia Prugue & N. Ruiz Morales (1988). "Idiopathic nephrotic syndrome of the adult with asymptomatic thrombosis of the renal vein". American journal of nephrology. 8 (6): 457–462. doi:10.1159/000167654. PMID 3218659.
- ↑ U. Kuhlmann, J. Steurer, A. Bollinger, G. Pouliadis, J. Briner & W. Siegenthaler (1981). "[Incidence and clinical significance of thromboses and thrombo-embolic complications in nephrotic syndrome patients]". Schweizerische medizinische Wochenschrift. 111 (27–28): 1034–1040. PMID 7268357. Unknown parameter
|month=ignored (help) - ↑ F. Llach, S. Papper & S. G. Massry (1980). "The clinical spectrum of renal vein thrombosis: acute and chronic". The American journal of medicine. 69 (6): 819–827. PMID 7446547. Unknown parameter
|month=ignored (help) - ↑ Palta, Sanjeev; Saroa, Richa; Palta, Anshu (2014). "Overview of the coagulation system". Indian Journal of Anaesthesia. 58 (5): 515. doi:10.4103/0019-5049.144643. ISSN 0019-5049.
- ↑ Owens, A. Phillip; Mackman, Nigel (2017). "Tissue factor and thrombosis: The clot starts here". Thrombosis and Haemostasis. 104 (09): 432–439. doi:10.1160/TH09-11-0771. ISSN 0340-6245.
- ↑ C. T. Esmon (1989). "The roles of protein C and thrombomodulin in the regulation of blood coagulation". The Journal of biological chemistry. 264 (9): 4743–4746. PMID 2538457. Unknown parameter
|month=ignored (help) - ↑ Shinji Onda, Hiroaki Shiba, Yuki Takano, Kenei Furukawa, Taigo Hata & Katsuhiko Yanaga (2018). "Renal Infarction during Anticoagulant Therapy after Living Donor Liver Transplantation". Case reports in gastroenterology. 12 (1): 165–169. doi:10.1159/000488526. PMID 29805361. Unknown parameter
|month=ignored (help) - ↑ Kahan, Scott, Smith, Ellen G. In A Page: Signs and Symptoms. Malden, Massachusetts: Blackwell Publishing, 2004:68 ISBN 140510368X
- ↑ Sailer, Christian, Wasner, Susanne. Differential Diagnosis Pocket. Hermosa Beach, CA: Borm Bruckmeir Publishing LLC, 2002:77 ISBN 1591032016
- ↑ Rajni Singhal & K. Scott Brimble (2006). "Thromboembolic complications in the nephrotic syndrome: pathophysiology and clinical management". Thrombosis research. 118 (3): 397–407. doi:10.1016/j.thromres.2005.03.030. PMID 15990160.
- ↑ F. Llach (1985). "Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome". Kidney international. 28 (3): 429–439. PMID 3906225. Unknown parameter
|month=ignored (help) - ↑ T. J. Rabelink, J. J. Zwaginga, H. A. Koomans & J. J. Sixma (1994). "Thrombosis and hemostasis in renal disease". Kidney international. 46 (2): 287–296. PMID 7967339. Unknown parameter
|month=ignored (help) - ↑ F. Llach (1985). "Hypercoagulability, renal vein thrombosis, and other thrombotic complications of nephrotic syndrome". Kidney international. 28 (3): 429–439. PMID 3906225. Unknown parameter
|month=ignored (help) - ↑ Natalie Weger, Stanislaw P. Stawicki, Garrett Roll, Kevin M. Hoddinott & John J. Lukaszczyk (2006). "Bilateral renal vein thrombosis secondary to membraneous glomerulonephritis: successful treatment with thrombolytic therapy". Annals of vascular surgery. 20 (3): 411–414. doi:10.1007/s10016-006-9029-8. PMID 16604403. Unknown parameter
|month=ignored (help) - ↑ Hyun S. Kim, Derek M. Fine & Mohamed G. Atta (2006). "Catheter-directed thrombectomy and thrombolysis for acute renal vein thrombosis". Journal of vascular and interventional radiology : JVIR. 17 (5): 815–822. doi:10.1097/01.RVI.0000209341.88873.26. PMID 16687747. Unknown parameter
|month=ignored (help) - ↑ C. R. Burrow, W. G. Walker, W. R. Bell & O. B. Gatewood (1984). "Streptokinase salvage of renal function after renal vein thrombosis". Annals of internal medicine. 100 (2): 237–238. PMID 6691668. Unknown parameter
|month=ignored (help) - ↑ G. Rostoker, I. Durand-Zaleski, M. Petit-Phar, A. Ben Maadi, N. Jazaerli, C. Radier, A. Rahmouni, D. Mathieu, N. Vasile & J. Rosso (1995). "Prevention of thrombotic complications of the nephrotic syndrome by the low-molecular-weight heparin enoxaparin". Nephron. 69 (1): 20–28. doi:10.1159/000188355. PMID 7891793.
- ↑ Richard J. Glassock (2007). "Prophylactic anticoagulation in nephrotic syndrome: a clinical conundrum". Journal of the American Society of Nephrology : JASN. 18 (8): 2221–2225. doi:10.1681/ASN.2006111300. PMID 17599972. Unknown parameter
|month=ignored (help) - ↑ Taewoo Lee, Andrea K. Biddle, Sofia Lionaki, Vimal K. Derebail, Sean J. Barbour, Sameer Tannous, Michelle A. Hladunewich, Yichun Hu, Caroline J. Poulton, Shannon L. Mahoney, J. Charles Jennette, Susan L. Hogan, Ronald J. Falk, Daniel C. Cattran, Heather N. Reich & Patrick H. Nachman (2014). "Personalized prophylactic anticoagulation decision analysis in patients with membranous nephropathy". Kidney international. 85 (6): 1412–1420. doi:10.1038/ki.2013.476. PMID 24336031. Unknown parameter
|month=ignored (help) - ↑ Nicholas Medjeral-Thomas, Stela Ziaj, Marie Condon, Jack Galliford, Jeremy Levy, Tom Cairns & Megan Griffith (2014). "Retrospective analysis of a novel regimen for the prevention of venous thromboembolism in nephrotic syndrome". Clinical journal of the American Society of Nephrology : CJASN. 9 (3): 478–483. doi:10.2215/CJN.07190713. PMID 24334865. Unknown parameter
|month=ignored (help) - ↑ Margaret C. Fang, Alan S. Go, Yuchiao Chang, Leila H. Borowsky, Niela K. Pomernacki, Natalia Udaltsova & Daniel E. Singer (2011). "A new risk scheme to predict warfarin-associated hemorrhage: The ATRIA (Anticoagulation and Risk Factors in Atrial Fibrillation) Study". Journal of the American College of Cardiology. 58 (4): 395–401. doi:10.1016/j.jacc.2011.03.031. PMID 21757117. Unknown parameter
|month=ignored (help) - ↑ Rajpurkar, M.; Sharathkumar, A.; Williams, S.; Lau, K.; Ling, S. C.; Chan, A. K. C. (2015). "Recommendations for the assessment of non-extremity venous thromboembolism outcomes: communication from the SSC of the ISTH". Journal of Thrombosis and Haemostasis. 13 (3): 477–480. doi:10.1111/jth.12809. ISSN 1538-7933.
- ↑ McDonald, Ruth A.; Smith, Jodi M.; Stablein, Donald; Harmon, William E. (2003). "Pretransplant peritoneal dialysis and graft thrombosis following pediatric kidney transplantation: A NAPRTCS report". Pediatric Transplantation. 7 (3): 204–208. doi:10.1034/j.1399-3046.2003.00075.x. ISSN 1397-3142.
- ↑ Lau, K. K.; Stoffman, J. M.; Williams, S.; McCusker, P.; Brandao, L.; Patel, S.; Chan, A. K.C. (2007). "Neonatal Renal Vein Thrombosis: Review of the English-Language Literature Between 1992 and 2006". PEDIATRICS. 120 (5): e1278–e1284. doi:10.1542/peds.2007-0510. ISSN 0031-4005.
- ↑ Bökenkamp, A.; von Kries, R.; Nowak-Göttl, U.; Göbel, U.; Hoyer, P. F. (2000). "Neonatal renal venous thrombosis in Germany between 1992 and 1994: epidemiology, treatment and outcome". European Journal of Pediatrics. 159 (1–2): 44–48. doi:10.1007/s004310050008. ISSN 0340-6199.
- ↑ Brandão, Leonardo R.; Simpson, Ewurabena A.; Lau, Keith K. (2011). "Neonatal renal vein thrombosis". Seminars in Fetal and Neonatal Medicine. 16 (6): 323–328. doi:10.1016/j.siny.2011.08.004. ISSN 1744-165X.
- ↑ Winyard, P J D (2006). "Perinatal renal venous thrombosis: presenting renal length predicts outcome". Archives of Disease in Childhood - Fetal and Neonatal Edition. 91 (4): F273–F278. doi:10.1136/adc.2005.083717. ISSN 1359-2998.
- ↑ Marks, Stephen D.; Massicotte, M. Patricia; Steele, Brian T.; Matsell, Douglas G.; Filler, Guido; Shah, Prakesh S.; Perlman, Max; Rosenblum, Norman D.; Shah, Vibhuti S. (2005). "Neonatal Renal Venous Thrombosis: Clinical Outcomes and Prevalence of Prothrombotic Disorders". The Journal of Pediatrics. 146 (6): 811–816. doi:10.1016/j.jpeds.2005.02.022. ISSN 0022-3476.
- ↑ Monagle, Paul; Chan, Anthony K.C.; Goldenberg, Neil A.; Ichord, Rebecca N.; Journeycake, Janna M.; Nowak-Göttl, Ulrike; Vesely, Sara K. (2012). "Antithrombotic Therapy in Neonates and Children". Chest. 141 (2): e737S–e801S. doi:10.1378/chest.11-2308. ISSN 0012-3692.
- ↑ Rajpurkar, M.; Sharathkumar, A.; Williams, S.; Lau, K.; Ling, S. C.; Chan, A. K. C. (2015). "Recommendations for the assessment of non-extremity venous thromboembolism outcomes: communication from the SSC of the ISTH". Journal of Thrombosis and Haemostasis. 13 (3): 477–480. doi:10.1111/jth.12809. ISSN 1538-7933.
- ↑ Zigman, Andrew; Yazbeck, Salam; Emil, Sherif; Nguyen, Luong (2000). "Renal vein thrombosis: A 10-year review". Journal of Pediatric Surgery. 35 (11): 1540–1542. doi:10.1053/jpsu.2000.18302. ISSN 0022-3468.
- ↑ Kerlin, B. A.; Ayoob, R.; Smoyer, W. E. (2012). "Epidemiology and Pathophysiology of Nephrotic Syndrome-Associated Thromboembolic Disease". Clinical Journal of the American Society of Nephrology. 7 (3): 513–520. doi:10.2215/CJN.10131011. ISSN 1555-9041.
- ↑ Kuhle, Stefan; Massicotte, Patti; Chan, Anthony; Mitchell, Lesley (2004). "A case series of 72 neonates with renal vein thrombosis data from the 1-800-NO-CLOTS registry". Thrombosis and Haemostasis. doi:10.1160/TH04-02-0131. ISSN 0340-6245.
- ↑ Marks, Stephen D.; Massicotte, M. Patricia; Steele, Brian T.; Matsell, Douglas G.; Filler, Guido; Shah, Prakesh S.; Perlman, Max; Rosenblum, Norman D.; Shah, Vibhuti S. (2005). "Neonatal Renal Venous Thrombosis: Clinical Outcomes and Prevalence of Prothrombotic Disorders". The Journal of Pediatrics. 146 (6): 811–816. doi:10.1016/j.jpeds.2005.02.022. ISSN 0022-3476.
- ↑ U. Nowak-Gottl, R. von Kries & U. Gobel (1997). "Neonatal symptomatic thromboembolism in Germany: two year survey". Archives of disease in childhood. Fetal and neonatal edition. 76 (3): F163–F167. PMID 9175945. Unknown parameter
|month=ignored (help) - ↑ B. Schmidt & M. Andrew (1995). "Neonatal thrombosis: report of a prospective Canadian and international registry". Pediatrics. 96 (5 Pt 1): 939–943. PMID 7478839. Unknown parameter
|month=ignored (help) - ↑ Rajpurkar, M.; Sharathkumar, A.; Williams, S.; Lau, K.; Ling, S. C.; Chan, A. K. C. (2015). "Recommendations for the assessment of non-extremity venous thromboembolism outcomes: communication from the SSC of the ISTH". Journal of Thrombosis and Haemostasis. 13 (3): 477–480. doi:10.1111/jth.12809. ISSN 1538-7933.