Coxsackie virus
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]Associate Editor(s)-in-Chief: Usama Talib, BSc, MD [2]
|
Coxsackie Virus |
Overview
Coxsackie (virus) is a cytolytic virus of the picornaviridae family, an enterovirus (a group containing the polioviruses, coxsackieviruses, and echoviruses). There are 61 non-polio enteroviruses that can cause disease in humans, of which 23 are coxsackie A viruses (6 are Coxsackie B viruses). Enterovirus are the second most common viral infectious agents in humans (after the rhinoviruses)
Classification
Coxsackie viruses consist of coxsackie A virus and coxsackie B virus. Coxsackie B virus has 6 serotypes, one of the significant serotypes is called coxsackie B4 virus.
| Coxsackie Virus | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Coxsackie A virus | Coxsackie B virus[1] | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Common Coxsackie B virus diseases | Coxsackie B4 virus diseases | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
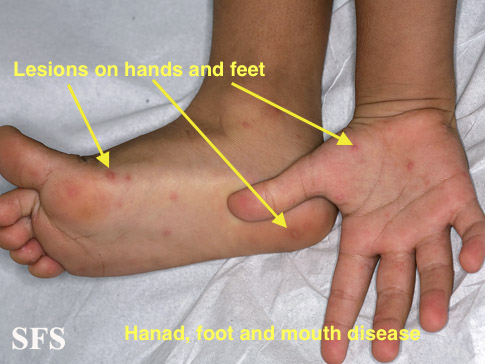
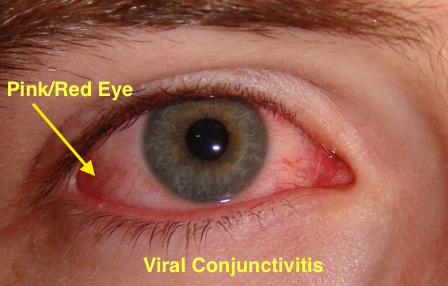
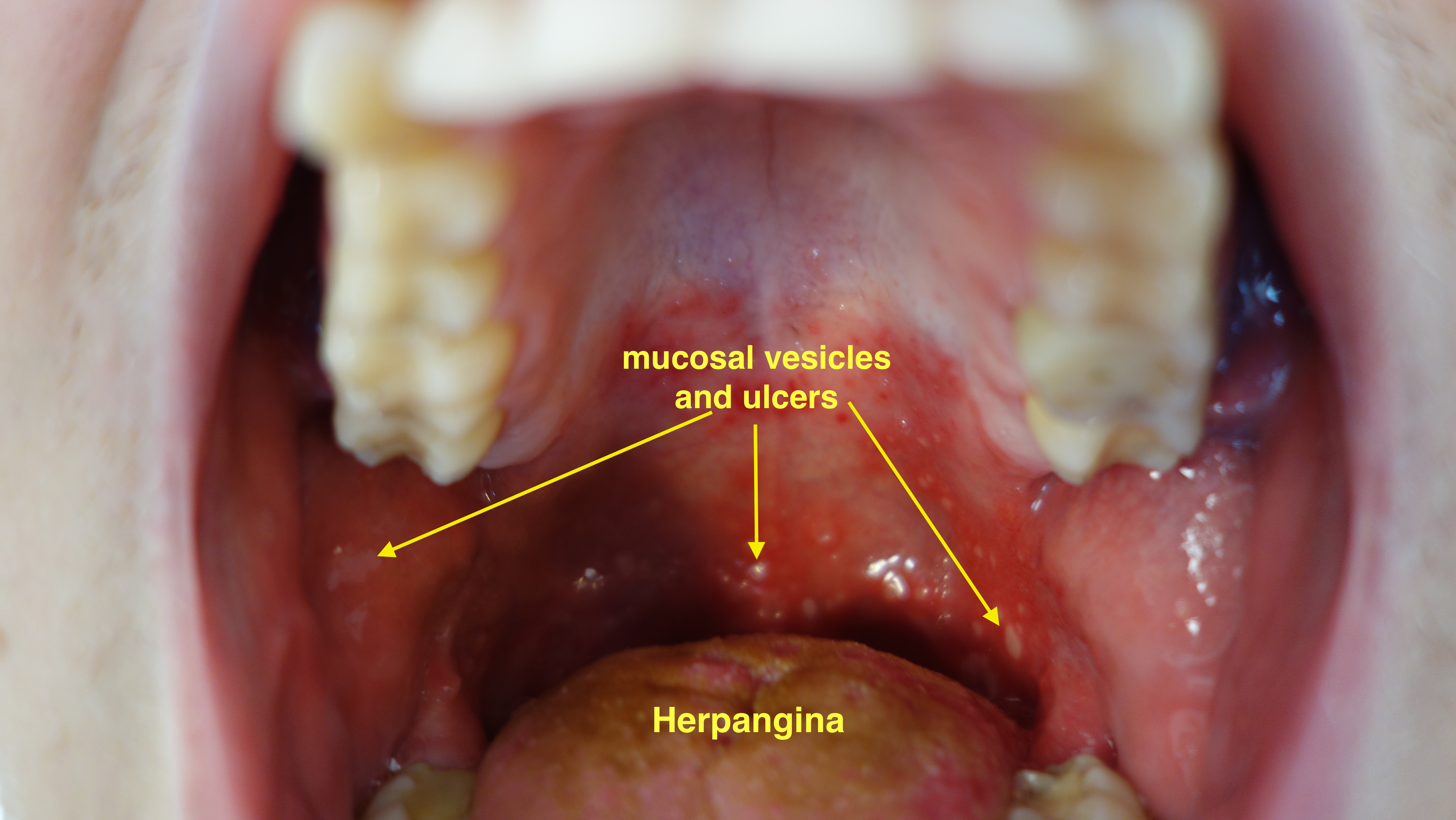
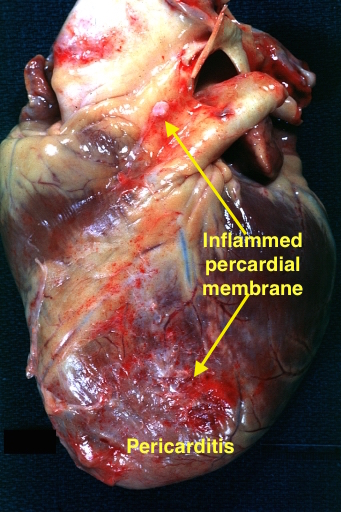
| • Hand, foot and mouth disease • Acute hemorrhagic conjunctivitis • Herpangina • Aseptic meningitis | • Pericarditis • Myocarditis • Pericardial effusion • Pleurodynia • Hepatitis • Sjogren's syndorme | • Diabetes mellitus • Acute flaccid myelitis[2] | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Differential Diagnosis
Coxsackie A virus and coxsackie B virus can cause multiple diseases in humans. The wide array of diseases caused by coxsackie viruses can be differentiated from one another easily on the basis of involvement of the organs systems, clinical presentation and diagnostic techniques.
| Virus Type | Disease | Clinical Features | Diagnosis | Image |
|---|---|---|---|---|
| Coxscakie A virus | Hand foot and mouth disease |
|
| |
| Acute hemorrhagic conjunctivitis |
|
|
| |
| Herpangina |
|
|
| |
| Aseptic Meningitis |
|
|||
| Coxsackie B virus | Pericarditis |
|
|
|
| Myocarditis |
|
|
Viral myocarditis | |
| Pericardial effusion |
|
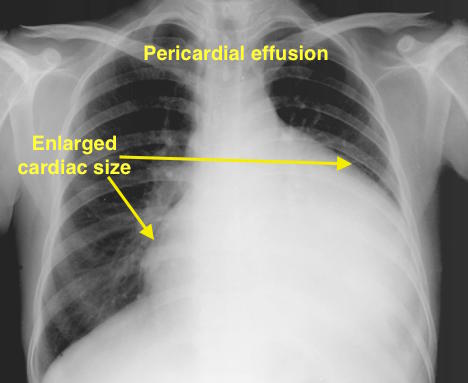
| ||
| Pleurodynia |
|
|
||
| Hepatitis |
|
|||
| Sjogren's syndrome |
|
|
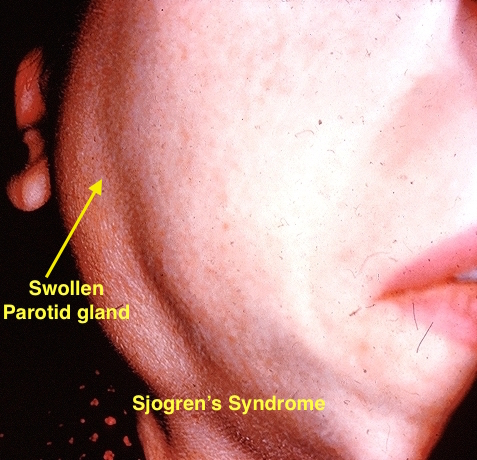
|
Template:Baltimore classification Template:Viral diseases
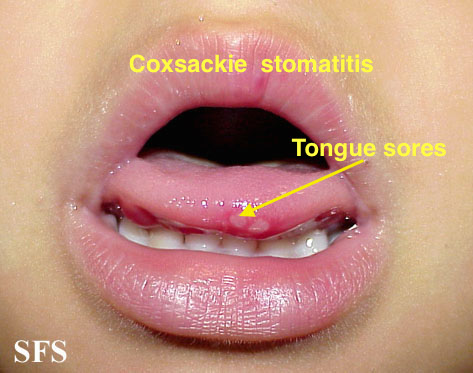
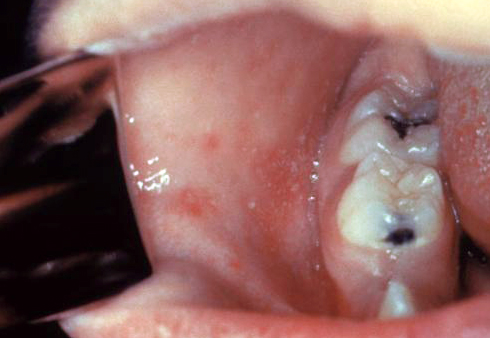
Coxsackie virus oral lesions must be differentiated from other mouth lesions such as oral candidiasis and aphthous ulcer
Oral Involvement
Oral lesions of coxackie virus infection must be differentiated from other diseases causing oral lesions such as leukoplakia and herpes simplex virus infection.
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis |
|
 |
| Herpes simplex oral lesions |
|
|
|
|
 | |
| Aphthous ulcers |
|
|
|
|
|
 |
| Squamous cell carcinoma |
|
|
 | |||
| Leukoplakia |
|
|
|
|
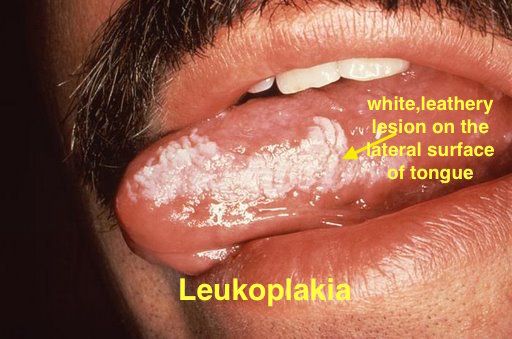 | |
| Melanoma |
|
|
|
|
 | |
| Fordyce spots |
|
|
|
|
 | |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
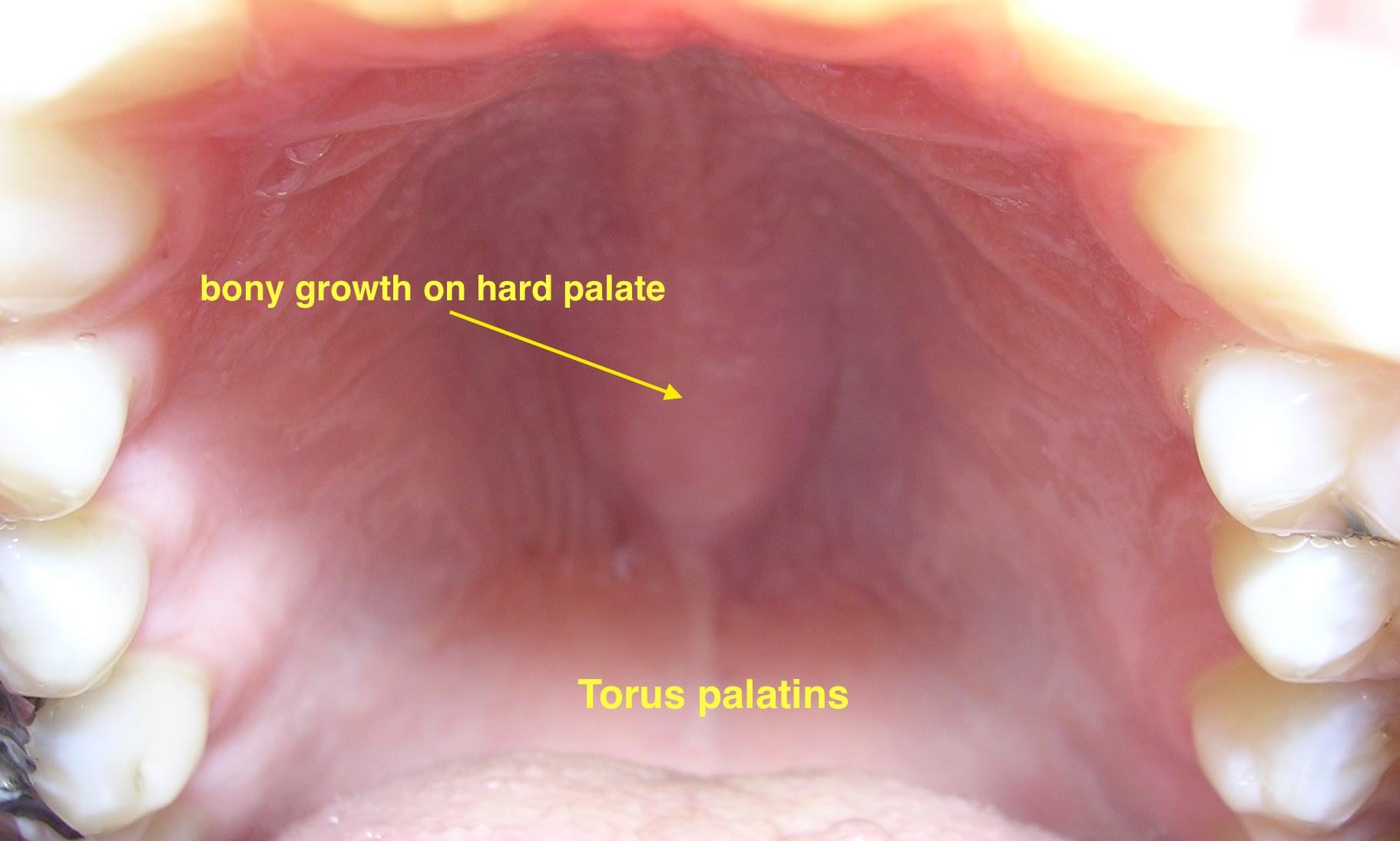 | ||||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
 | ||
| Crohn's disease |
|
|
|
|||
| Agranulocytosis |
|
|
||||
| Syphilis[6] |
|
|
|
 | ||
| Coxsackie virus |
|
|
 | |||
| Chicken pox |
|
|
|
|
 | |
| Measles |
|
|
|
 | ||
- ↑ Fields, Bernard N. (1985). Fields Virology. New York: Raven Press. pp. 739–794. ISBN 0-88167-026-X. Unknown parameter
|coauthors=ignored (help) - ↑ Cho SM, MacDonald S, Frontera JA (2017). "Coxsackie B3/B4-Related Acute Flaccid Myelitis". Neurocrit Care. doi:10.1007/s12028-017-0377-8. PMID 28324262.
- ↑ Smith SC, Ladenson JH, Mason JW, Jaffe AS (1997). "Elevations of cardiac troponin I associated with myocarditis. Experimental and clinical correlates". Circulation. 95 (1): 163–8. PMID 8994432.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File:A_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ "Dermatology Atlas".
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.