Sandbox:Affan: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| Line 1,129: | Line 1,129: | ||
|- | |- | ||
| rowspan="4" style="background: #DCDCDC; padding: 5px; text-align: center;" |'''Cysts''' | | rowspan="4" style="background: #DCDCDC; padding: 5px; text-align: center;" |'''Cysts''' | ||
| style="background: #DCDCDC; padding: 5px; text-align: center;" |Oral Lymphoepithelial cyst ([[Branchial cleft cyst]]) | | style="background: #DCDCDC; padding: 5px; text-align: center;" |Oral Lymphoepithelial cyst ([[Branchial cleft cyst]])<ref name="pmid28936296">{{cite journal |vauthors=Sykara M, Ntovas P, Kalogirou EM, Tosios KI, Sklavounou A |title=Oral lymphoepithelial cyst: A clinicopathological study of 26 cases and review of the literature |journal=J Clin Exp Dent |volume=9 |issue=8 |pages=e1035–e1043 |date=August 2017 |pmid=28936296 |pmc=5601105 |doi=10.4317/jced.54072 |url=}}</ref><ref name="pmid22452887">{{cite journal |vauthors=Stramandinoli-Zanicotti RT, de Castro Ávila LF, de Azevedo Izidoro AC, Izidoro FA, Schussel JL |title=Lymphoepithelial cysts of oral mucosa: two cases in different regions |journal=Bull. Tokyo Dent. Coll. |volume=53 |issue=1 |pages=17–22 |date=2012 |pmid=22452887 |doi= |url=}}</ref> | ||
| | | | ||
* Painless | * Painless | ||
* White to yellow | * White to yellow | ||
* Soft to firm | * Soft to firm submucosal nodule | ||
* Less than 1 cm | * Less than 1 cm | ||
| | | | ||
Revision as of 02:28, 19 February 2019
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Muhammad Affan M.D.[2]
| Surface oral lesions | |||||||
|---|---|---|---|---|---|---|---|
| Oral lesions | Appearance | Associated conditions | Location | Microscopic | Image | ||
| White Lesions | Leukoedema[1][2] |
|
|
|
|
 | |
| Fordyce granules[3][4][5][6] |
|
|
|
|
 | ||
| Benign migratory glossitis[7][8][9] |
|
|
|
|
 | ||
| Hairy tongue[10][11][12][13] |
|
|
|
 | |||
| Hairy leukoplakia[14][15] |
White patches
|
|
|
|

| ||
| White sponge nevus[16][17] |
|
||||||
| Lichen Planus[18][19] |
|
|
|
 | |||
| Frictional hyperkeratosis[20][21] |
|
|
|
|
 | ||
| Leukoplakia |
|
|
|
 | |||
| Erythroplakia |
|
|
|
 | |||
| Oral lesions | Appearance | Associated conditions | Location | Microscopic | Image | ||
| Pigmented lesions |
|
|
|
|
|
 | |
|
|
||||||
|
|
|
 | ||||
|
|
|
 | ||||
|
|
 | |||||
|
|
|
 | ||||
|
Intraorally |
|
 | ||||
|
|
|
 | ||||
|
|
||||||
|
|
|
 | ||||
| Oral lesions | Appearance | Associated conditions | Location | Microscopic | Image | ||
| Vesicular/Erythematous
Ulcerative lesions |
Infections | Herpes simplex virusinfections[40][41][42] |
|
|
|
 | |
| Herpes zoster[43][44][45] |
|
|
|
 | |||
| Hand foot mouth disease[46][47][48] |
|
|
|
|
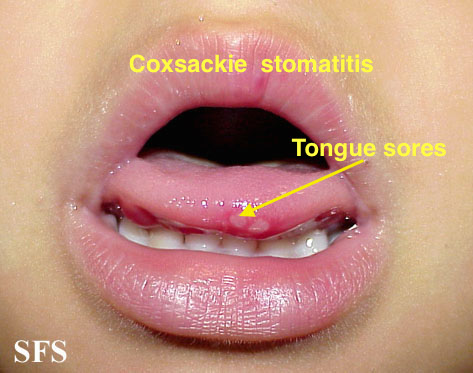 | ||
| Infectious mononucliosis[49][50] |
|
|
|
 | |||
| Erosive lichen planus[51][52][53] |
|
||||||
| Pseudomembranous candidiasis[54][55][56] |
|
|
|
 | |||
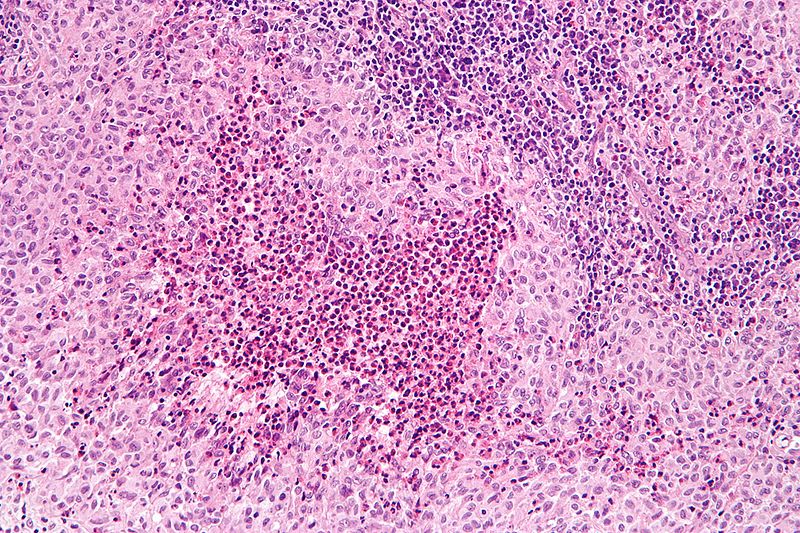
| Histoplasmosis[57][58][59][60][61] |
|
|
|
 | |||
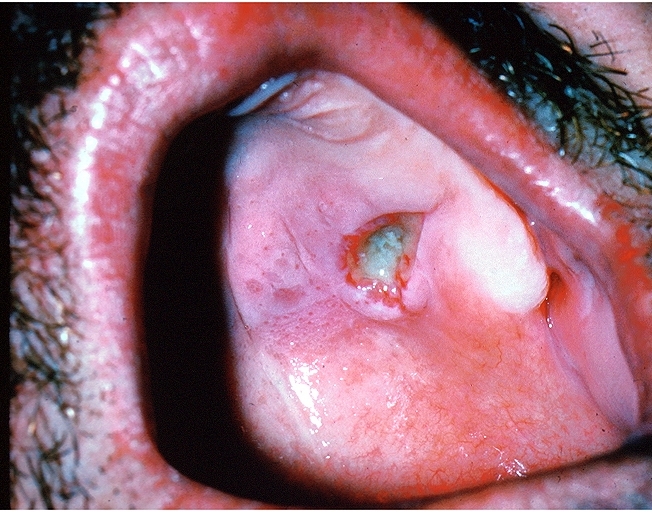
| Blastomycosis[62][63][64] |
|
|
|
Classic appearance on modified Wright's stain
|
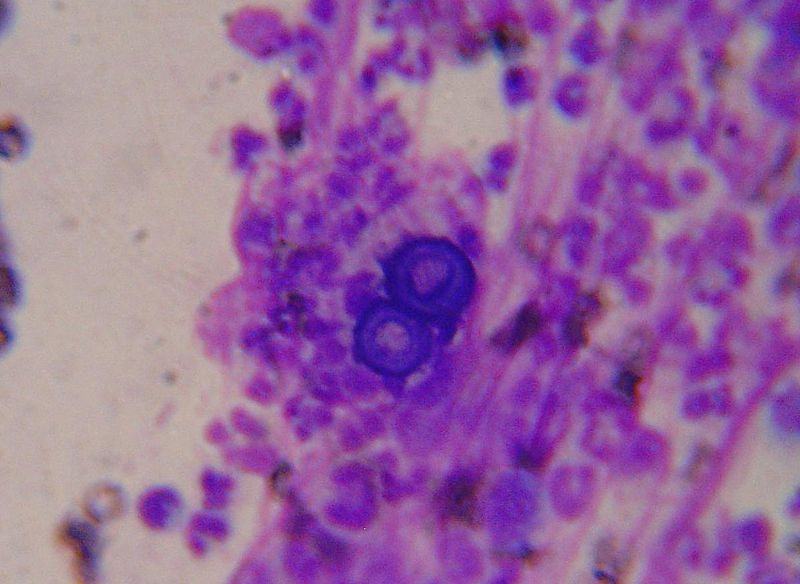 | ||
| Coccidiodomycosis[65][66][67][68] |
|
|
|
It is a dimorphic fungus and on microscopy, the following can be seen
|
 | ||
| Autoimmune diseases | Pemphigus vulgaris[69][70][71] |
|
|
|
 | ||
| Mucous membrane pemphigoid (Cicatricial pemphigoid)[72][73][74] |
|
|
|||||
| Aphthous ulcer[75][76][77] |
|
|
 | ||||
| Erythema multiforme[78][79] |
|
|
|
 | |||
| Sjogren's Syndrome |
Affects salivary and lacrimal glands
|
|
 | ||||
| Bullous pemphigoid |
|
|
|
 | |||
| Idiopathic conditions | Allergic contact stomatitis |
|
|
||||
| Irritant contact stomatitis | |||||||
| Soft tissue oral lesions | ||||||
|---|---|---|---|---|---|---|
| Reactive lesions | Appearance | Associated conditions | Location | Microscopic | Image | |
| Inflammatory papillary hyperplasia |
|
|
 | |||
| Fibrous hyperplasia |
|
|
|
|
||
| Mucocele |
|
|
|
|
 | |
| Necrotizing sialometaplasia |
|
|
|
 | ||
| Periodontal abscess |
|
|
|
 | ||
| Periapical abscess |
|
|
|
 | ||
| Tumors | Appearance | Associated conditions | Locations | Microscopic | Image | |
| Epithelial tumors | Squamous cell carcinoma |
|
|
Squamous cell carcinoma may be well, moderately or poorly differentiated.
SCC variants: Basaloid:
Verrucous
Papillary Spindle cell Adenosquamous Acantholytic Cunniculatum |
 | |
| Oral epithelial dysplasia |
|
Common sites:
|
Histopathologically it may be classified as
Mild:
Moderate:
Severe:
|
 | ||
| Proliferative verrucous leukoplakia |
|
|
The histopathological findings associated with PVL are as under:
|
 | ||
| Papillomas | Condyloma acuminatum |
|
HPV, most commonly types 6,11,16 and 18 | Several sessile, cauliflower-like swellings forming a cluster |  | |
| Verrucous vulgaris | Soft, pedunculated lesions formed by a cluster of finger-like fronds or a sessile, dome-shaped lesion with a nodular, papillary or verrucous surface | HPV subtype
2,4,6,7,10,40. |
Any oral site may be affected mostly:
|
|
 | |
| Multifocal epithelial hyperplasia |
|
HPV
13 and 32 |
|
|
 | |
| Salivary type tumors | Mucoepidermoid carcinoma |
|
|
Low power microscopy shows low-grade tumor with both cystic and solid areas and an inflamed, fibrous stroma | ||
| Pleomorphic adenoma | Painless, slow growing, submucosal masses, but when |
|
Histopathological findings shows cellular, and hyaline or plasmacytoid cell |  | ||
| Soft tissue and Neural tumors | Granular cell tumor |
|
|
Plump eosinophilic cells with central small dark nuclei and abundant granular cytoplasm |  | |
| Rhabdomyoma |
|
|
 | |||
| Lymphangioma |
|
Thin-walled, dilated lymphatic vessels of different size, which are lined by a flattened endothelium |  | |||
| Hemangioma[80][81][82] |
|
|
|
 | ||
| Kaposi sarcoma[83][84] | HIV and HHV-8 |
|
Spindle cells with minimal nuclear atypia |  | ||
| Myofibroblastic sarcoma |
|
|
||||
| Hematolymphoid tumors | Plasmablastic lymphoma[85][86][87] | It may appear as thickened ulcerative lesion that may invade the adjacent bone | Intraoally: |
|
||
| Langerhan cell histiocytosis[88][89][90] |
|
Associated with:
|
|
Biopsy shows ovoid langerhans cells
with deeply grooved nuclei, thin nuclear membrane and abundant eosinophilic cytoplasm |
 | |
| Extramedullary myeloid sarcoma[91][92][93] | Isolated tumor-forming intraoral mass | History of acute myeloid leukemia,
predominantly in the monocytic or myelomonocytic subtypes |
|
|||
| Tumors of uncertain histiogenesis | Congenital granular cell epulis |
|
|
|
|
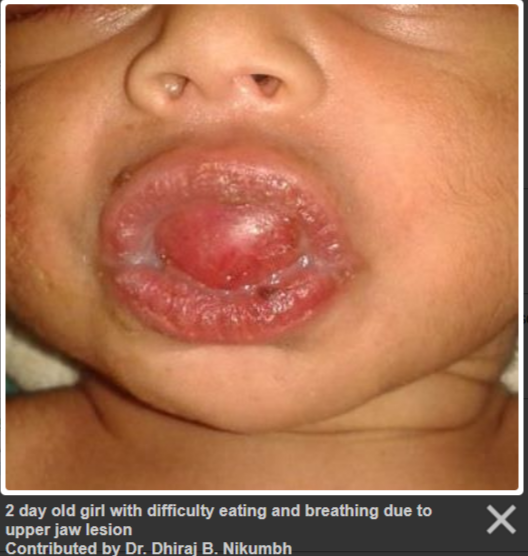 |
| Ectomesenchymal chondromyxoid tumor |
|
|
|
|||
| Cysts | Oral Lymphoepithelial cyst (Branchial cleft cyst)[94][95] |
|
|
Cystic cavity lined with:
|
||
| Oral Epidermoid cyst[96][97][98] |
|
|
Histopathologically:
|
|||
| Thyroglossal tract cyst |  | |||||
| Nasolabial cyst ( Klestadt cyst)[99][100][101] |
|
|||||
References
- ↑ Jahanbani J, Sandvik L, Lyberg T, Ahlfors E (March 2009). "Evaluation of oral mucosal lesions in 598 referred Iranian patients". Open Dent J. 3: 42–7. doi:10.2174/1874210600903010042. PMID 19444343.
- ↑ Abidullah M, Raghunath V, Karpe T, Akifuddin S, Imran S, Dhurjati VN, Aleem MA, Khatoon F (February 2016). "Clinicopathologic Correlation of White, Non scrapable Oral Mucosal Surface Lesions: A Study of 100 Cases". J Clin Diagn Res. 10 (2): ZC38–41. doi:10.7860/JCDR/2016/16950.7226. PMC 4800649. PMID 27042583.
- ↑ Lee JH, Lee JH, Kwon NH, Yu DS, Kim GM, Park CJ, Lee JD, Kim SY (February 2012). "Clinicopathologic Manifestations of Patients with Fordyce's Spots". Ann Dermatol. 24 (1): 103–6. doi:10.5021/ad.2012.24.1.103. PMC 3283840. PMID 22363169.
- ↑ Olivier JH (March 2006). "Fordyce granules on the prolabial and oral mucous membranes of a selected population". SADJ. 61 (2): 072–4. PMID 16711559.
- ↑ De Felice C, Parrini S, Chitano G, Gentile M, Dipaola L, Latini G (September 2005). "Fordyce granules and hereditary non-polyposis colorectal cancer syndrome". Gut. 54 (9): 1279–82. doi:10.1136/gut.2005.064881. PMID 15879014.
- ↑ Ponti G, Meschieri A, Pollio A, Ruini C, Manfredini M, Longo C, Mandel VD, Ciardo S, Tomasi A, Giannetti L, Pellacani G (August 2015). "Fordyce granules and hyperplastic mucosal sebaceous glands as distinctive stigmata in Muir-Torre syndrome patients: characterization with reflectance confocal microscopy". J. Oral Pathol. Med. 44 (7): 552–7. doi:10.1111/jop.12256. PMID 25213213.
- ↑ Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M (December 2002). "Benign migratory glossitis or geographic tongue: an enigmatic oral lesion". Am. J. Med. 113 (9): 751–5. PMID 12517366.
- ↑ Picciani BL, Domingos TA, Teixeira-Souza T, Santos Vde C, Gonzaga HF, Cardoso-Oliveira J, Gripp AC, Dias EP, Carneiro S (2016). "Geographic tongue and psoriasis: clinical, histopathological, immunohistochemical and genetic correlation - a literature review". An Bras Dermatol. 91 (4): 410–21. doi:10.1590/abd1806-4841.20164288. PMC 4999097. PMID 27579734.
- ↑ Tarakji B, Umair A, Babaker Z, Sn A, Gazal G, Sarraj F (November 2014). "Relation between psoriasis and geographic tongue". J Clin Diagn Res. 8 (11): ZE06–7. doi:10.7860/JCDR/2014/9101.5171. PMC 4290356. PMID 25584342.
- ↑ Kobayashi K, Takei Y, Sawada M, Ishizaki S, Ito H, Tanaka M (2010). "Dermoscopic features of a black hairy tongue in 2 Japanese patients". Dermatol Res Pract. 2010. doi:10.1155/2010/145878. PMC 2913535. PMID 20706544.
- ↑ Jhaj R, Gour PR, Asati DP (2016). "Black hairy tongue with a fixed dose combination of olanzapine and fluoxetine". Indian J Pharmacol. 48 (3): 318–20. doi:10.4103/0253-7613.182894. PMC 4900008. PMID 27298505.
- ↑ Gurvits GE, Tan A (August 2014). "Black hairy tongue syndrome". World J. Gastroenterol. 20 (31): 10845–50. doi:10.3748/wjg.v20.i31.10845. PMC 4138463. PMID 25152586.
- ↑ Erriu M, Pili FM, Denotti G, Garau V (2016). "Black hairy tongue in a patient with amyotrophic lateral sclerosis". J Int Soc Prev Community Dent. 6 (1): 80–3. doi:10.4103/2231-0762.175408. PMC 4784070. PMID 27011938.
- ↑ Kreuter A, Wieland U (May 2011). "Oral hairy leukoplakia: a clinical indicator of immunosuppression". CMAJ. 183 (8): 932. doi:10.1503/cmaj.100841. PMC 3091903. PMID 21398239.
- ↑ Greenspan JS, Greenspan D, Webster-Cyriaque J (April 2016). "Hairy leukoplakia; lessons learned: 30-plus years". Oral Dis. 22 Suppl 1: 120–7. doi:10.1111/odi.12393. PMID 27109280.
- ↑ Aghbali A, Pouralibaba F, Eslami H, Pakdel F, Jamali Z (2009). "White sponge nevus: a case report". J Dent Res Dent Clin Dent Prospects. 3 (2): 70–2. doi:10.5681/joddd.2009.017. PMC 3517290. PMID 23230487.
- ↑ Nichols GE, Cooper PH, Underwood PB, Greer KE (September 1990). "White sponge nevus". Obstet Gynecol. 76 (3 Pt 2): 545–8. PMID 2381643.
- ↑ Gorouhi F, Davari P, Fazel N (2014). "Cutaneous and mucosal lichen planus: a comprehensive review of clinical subtypes, risk factors, diagnosis, and prognosis". ScientificWorldJournal. 2014: 742826. doi:10.1155/2014/742826. PMC 3929580. PMID 24672362.
- ↑ Gupta S, Jawanda MK (2015). "Oral Lichen Planus: An Update on Etiology, Pathogenesis, Clinical Presentation, Diagnosis and Management". Indian J Dermatol. 60 (3): 222–9. doi:10.4103/0019-5154.156315. PMC 4458931. PMID 26120146.
- ↑ Cam K, Santoro A, Lee JB (2012). "Oral frictional hyperkeratosis (morsicatio buccarum): an entity to be considered in the differential diagnosis of white oral mucosal lesions". Skinmed. 10 (2): 114–5. PMID 22545331.
- ↑ Mignogna MD, Fortuna G, Leuci S, Adamo D, Siano M, Makary C, Cafiero C (May 2011). "Frictional keratoses on the facial attached gingiva are rare clinical findings and do not belong to the category of leukoplakia". J. Oral Maxillofac. Surg. 69 (5): 1367–74. doi:10.1016/j.joms.2010.05.087. PMID 21216078.
- ↑ Carlos-Bregni R, Contreras E, Netto AC, Mosqueda-Taylor A, Vargas PA, Jorge J, León JE, de Almeida OP (September 2007). "Oral melanoacanthoma and oral melanotic macule: a report of 8 cases, review of the literature, and immunohistochemical analysis". Med Oral Patol Oral Cir Bucal. 12 (5): E374–9. PMID 17767102.
- ↑ Pais S, Hegde SK, Bhat SS (June 2004). "Oral melanotic macule--a case report". J Indian Soc Pedod Prev Dent. 22 (2): 73–5. PMID 15491090.
- ↑ Cantudo-Sanagustín E, Gutiérrez-Corrales A, Vigo-Martínez M, Serrera-Figallo MÁ, Torres-Lagares D, Gutiérrez-Pérez JL (July 2016). "Pathogenesis and clinicohistopathological caractheristics of melanoacanthoma: A systematic review". J Clin Exp Dent. 8 (3): e327–36. doi:10.4317/jced.52860. PMC 4930645. PMID 27398186.
- ↑ Peters SM, Mandel L, Perrino MA (March 2018). "Oral melanoacanthoma of the palate: An unusual presentation of an uncommon entity". JAAD Case Rep. 4 (2): 138–139. doi:10.1016/j.jdcr.2017.11.023. PMID 29387765.
- ↑ Gupta AA, Nainani P, Upadhyay B, Kavle P (September 2012). "Oral melanoacanthoma: A rare case of diffuse oral pigmentation". J Oral Maxillofac Pathol. 16 (3): 441–3. doi:10.4103/0973-029X.102514. PMID 23248484.
- ↑ Monteiro LS, Costa JA, da Câmara MI, Albuquerque R, Martins M, Pacheco JJ, Salazar F, Figueira F (2015). "Aesthetic Depigmentation of Gingival Smoker's Melanosis Using Carbon Dioxide Lasers". Case Rep Dent. 2015: 510589. doi:10.1155/2015/510589. PMC 4410537. PMID 25954535.
- ↑ Moravej-Salehi E, Moravej-Salehi E, Hajifattahi F (2015). "Relationship of Gingival Pigmentation with Passive Smoking in Women". Tanaffos. 14 (2): 107–14. PMC 4629424. PMID 26528364.
- ↑ Brown FH, Houston GD (August 1991). "Smoker's melanosis. A case report". J. Periodontol. 62 (8): 524–7. doi:10.1902/jop.1991.62.8.524. PMID 1920020.
- ↑ Puttanna A, Cunningham AR, Dainty P (July 2013). "Addison's disease and its associations". BMJ Case Rep. 2013. doi:10.1136/bcr-2013-010473. PMC 3736622. PMID 23893277.
- ↑ Sarkar SB, Sarkar S, Ghosh S, Bandyopadhyay S (October 2012). "Addison's disease". Contemp Clin Dent. 3 (4): 484–6. doi:10.4103/0976-237X.107450. PMC 3636818. PMID 23633816.
- ↑ Mozaffari HR, Rezaei F, Sharifi R, Mirbahari SG (2016). "Seven-Year Follow-Up of Peutz-Jeghers Syndrome". Case Rep Dent. 2016: 6052181. doi:10.1155/2016/6052181. PMC 4852371. PMID 27195155.
- ↑ Choi HS, Park YJ, Park JG (February 1999). "Peutz-Jeghers syndrome: a new understanding". J. Korean Med. Sci. 14 (1): 2–7. doi:10.3346/jkms.1999.14.1.2. PMC 3054160. PMID 10102516.
- ↑ Janardhanan M, Rakesh S, Vinod Kumar R (January 2011). "Intraoral presentation of multiple malignant peripheral nerve sheath tumors associated with neurofibromatosis-1". J Oral Maxillofac Pathol. 15 (1): 46–51. doi:10.4103/0973-029X.80025. PMC 3125655. PMID 21731277.
- ↑ Thammaiah S, Manjunath M, Rao K, Uma DH (January 2011). "Intraoral plexiform neurofibroma involving the maxilla - pathognomonic of neurofibromatosis type I". J Pediatr Neurosci. 6 (1): 65–8. doi:10.4103/1817-1745.84413. PMC 3173921. PMID 21977094.
- ↑ Janardhanan M, Rakesh S, Vinod Kumar R (January 2011). "Intraoral presentation of multiple malignant peripheral nerve sheath tumors associated with neurofibromatosis-1". J Oral Maxillofac Pathol. 15 (1): 46–51. doi:10.4103/0973-029X.80025. PMC 3125655. PMID 21731277.
- ↑ Thammaiah S, Manjunath M, Rao K, Uma DH (January 2011). "Intraoral plexiform neurofibroma involving the maxilla - pathognomonic of neurofibromatosis type I". J Pediatr Neurosci. 6 (1): 65–8. doi:10.4103/1817-1745.84413. PMC 3173921. PMID 21977094.
- ↑ Lundin K, Schmidt G, Bonde C (2013). "Amalgam tattoo mimicking mucosal melanoma: a diagnostic dilemma revisited". Case Rep Dent. 2013: 787294. doi:10.1155/2013/787294. PMC 3606745. PMID 23533829.
- ↑ Buchner A, Hansen LS (February 1980). "Amalgam pigmentation (amalgam tattoo) of the oral mucosa. A clinicopathologic study of 268 cases". Oral Surg. Oral Med. Oral Pathol. 49 (2): 139–47. PMID 6928285.
- ↑ Mohan RP, Verma S, Singh U, Agarwal N (July 2013). "Acute primary herpetic gingivostomatitis". BMJ Case Rep. 2013. doi:10.1136/bcr-2013-200074. PMC 3736476. PMID 23839615.
- ↑ Tovaru S, Parlatescu I, Tovaru M, Cionca L (February 2009). "Primary herpetic gingivostomatitis in children and adults". Quintessence Int. 40 (2): 119–24. PMID 19169443.
- ↑ Amir J, Nussinovitch M, Kleper R, Cohen HA, Varsano I (1997). "Primary herpes simplex virus type 1 gingivostomatitis in pediatric personnel". Infection. 25 (5): 310–2. PMID 9334868.
- ↑ Mohan RP, Verma S, Singh U, Agarwal N (June 2013). "Herpes zoster". BMJ Case Rep. 2013. doi:10.1136/bcr-2013-010246. PMC 3702907. PMID 23771975.
- ↑ Patil S, Srinivas K, Reddy BS, Gupta M (March 2013). "Prodromal herpes zoster mimicking odontalgia--a diagnostic challenge". Ethiop J Health Sci. 23 (1): 73–7. PMC 3613819. PMID 23559842.
- ↑ Kolokotronis A, Louloudiadis K, Fotiou G, Matiais A (2001). "Oral manifestations of infections of infections due to varicella zoster virus in otherwise healthy children". J Clin Pediatr Dent. 25 (2): 107–12. PMID 11314207.
- ↑ Muppa R, Bhupatiraju P, Duddu M, Dandempally A (2011). "Hand, foot and mouth disease". J Indian Soc Pedod Prev Dent. 29 (2): 165–7. doi:10.4103/0970-4388.84692. PMID 21911958.
- ↑ Kashyap RR, Kashyap RS (April 2015). "Hand, foot and mouth disease - a short case report". J Clin Exp Dent. 7 (2): e336–8. doi:10.4317/jced.52031. PMC 4483348. PMID 26155357.
- ↑ Liu B, Luo L, Yan S, Wen T, Bai W, Li H, Zhang G, Lu X, Liu Y, He L (2015). "Clinical Features for Mild Hand, Foot and Mouth Disease in China". PLoS ONE. 10 (8): e0135503. doi:10.1371/journal.pone.0135503. PMC 4547800. PMID 26302092.
- ↑ Odumade OA, Hogquist KA, Balfour HH (January 2011). "Progress and problems in understanding and managing primary Epstein-Barr virus infections". Clin. Microbiol. Rev. 24 (1): 193–209. doi:10.1128/CMR.00044-10. PMC 3021204. PMID 21233512.
- ↑ Grimm JM, Schmeling DO, Dunmire SK, Knight JA, Mullan BD, Ed JA, Brundage RC, Hogquist KA, Balfour HH (August 2016). "Prospective studies of infectious mononucleosis in university students". Clin Transl Immunology. 5 (8): e94. doi:10.1038/cti.2016.48. PMID 27588199.
- ↑ Omal P, Jacob V, Prathap A, Thomas NG (March 2012). "Prevalence of oral, skin, and oral and skin lesions of lichen planus in patients visiting a dental school in southern India". Indian J Dermatol. 57 (2): 107–9. doi:10.4103/0019-5154.94276. PMC 3352630. PMID 22615505.
- ↑ Belal MH (2015). "Management of symptomatic erosive-ulcerative lesions of oral lichen planus in an adult Egyptian population using Selenium-ACE combined with topical corticosteroids plus antifungal agent". Contemp Clin Dent. 6 (4): 454–60. doi:10.4103/0976-237X.169837. PMC 4678540. PMID 26681847.
- ↑ Chitturi RT, Sindhuja P, Parameswar RA, Nirmal RM, Reddy BV, Dineshshankar J, Yoithapprabhunath TR (August 2015). "A clinical study on oral lichen planus with special emphasis on hyperpigmentation". J Pharm Bioallied Sci. 7 (Suppl 2): S495–8. doi:10.4103/0975-7406.163513. PMC 4606647. PMID 26538905.
- ↑ Williams D, Lewis M (January 2011). "Pathogenesis and treatment of oral candidosis". J Oral Microbiol. 3. doi:10.3402/jom.v3i0.5771. PMC 3087208. PMID 21547018.
- ↑ Warrier SA, Sathasivasubramanian S (August 2015). "Human immunodeficiency virus induced oral candidiasis". J Pharm Bioallied Sci. 7 (Suppl 2): S812–4. doi:10.4103/0975-7406.163577. PMC 4606720. PMID 26538978.
- ↑ Byadarahally Raju S, Rajappa S (2011). "Isolation and identification of Candida from the oral cavity". ISRN Dent. 2011: 487921. doi:10.5402/2011/487921. PMC 3205665. PMID 22111010.
- ↑ Chatterjee D, Chatterjee A, Agarwal M, Mathur M, Mathur S, Mallikarjun R, Banerjee S (2017). "Disseminated Histoplasmosis with Oral Manifestation in an Immunocompetent Patient". Case Rep Dent. 2017: 1323514. doi:10.1155/2017/1323514. PMC 5306962. PMID 28255468.
- ↑ Vidyanath S, Shameena P, Sudha S, Nair RG (January 2013). "Disseminated histoplasmosis with oral and cutaneous manifestations". J Oral Maxillofac Pathol. 17 (1): 139–42. doi:10.4103/0973-029X.110722. PMC 3687172. PMID 23798850.
- ↑ Patil K, Mahima VG, Prathibha Rani RM (September 2009). "Oral histoplasmosis". J Indian Soc Periodontol. 13 (3): 157–9. doi:10.4103/0972-124X.60230. PMC 2848788. PMID 20379415.
- ↑ Brazão-Silva MT, Mancusi GW, Bazzoun FV, Ishisaki GY, Marcucci M (January 2013). "A gingival manifestation of histoplasmosis leading diagnosis". Contemp Clin Dent. 4 (1): 97–101. doi:10.4103/0976-237X.111621. PMC 3703707. PMID 23853464.
- ↑ Souza BC, Munerato MC (2017). "Oral manifestation of histoplasmosis on the palate". An Bras Dermatol. 92 (5 Suppl 1): 107–109. doi:10.1590/abd1806-4841.20175751. PMC 5726694. PMID 29267463.
- ↑ Kruse AL, Zwahlen RA, Bredell MG, Gengler C, Dannemann C, Grätz KW (January 2010). "Primary blastomycosis of oral cavity". J Craniofac Surg. 21 (1): 121–3. doi:10.1097/SCS.0b013e3181c4680c. PMID 20072023.
- ↑ Thomas J, Munson E, Christianson JC (August 2014). "Unexpected Blastomyces dermatitidis etiology of fungal sinusitis and erosive palatal infection in a diabetic patient". J. Clin. Microbiol. 52 (8): 3130–3. doi:10.1128/JCM.01392-14. PMC 4136175. PMID 24899035.
- ↑ Webber LP, Martins MD, de Oliveira MG, Munhoz EA, Carrard VC (April 2014). "Disseminated paracoccidioidomycosis diagnosis based on oral lesions". Contemp Clin Dent. 5 (2): 213–6. doi:10.4103/0976-237X.132340. PMC 4067786. PMID 24963249.
- ↑ Mendez LA, Flores SA, Martinez R, de Almeida OP (2017). "Ulcerated Lesion of the Tongue as Manifestation of Systemic Coccidioidomycosis". Case Rep Med. 2017: 1489501. doi:10.1155/2017/1489501. PMC 5366790. PMID 28386282.
- ↑ Rodriguez RA, Konia T (January 2005). "Coccidioidomycosis of the tongue". Arch. Pathol. Lab. Med. 129 (1): e4–6. doi:10.1043/1543-2165(2005)129<e4:COTT>2.0.CO;2. PMID 15628927.
- ↑ McConnell MF, Shi A, Lasco TM, Yoon L (March 2017). "Disseminated coccidioidomycosis with multifocal musculoskeletal disease involvement". Radiol Case Rep. 12 (1): 141–145. doi:10.1016/j.radcr.2016.11.017. PMC 5310389. PMID 28228898.
- ↑ Valdivia L, Nix D, Wright M, Lindberg E, Fagan T, Lieberman D, Stoffer T, Ampel NM, Galgiani JN (June 2006). "Coccidioidomycosis as a common cause of community-acquired pneumonia". Emerging Infect. Dis. 12 (6): 958–62. PMC 3373055. PMID 16707052.
- ↑ Arpita R, Monica A, Venkatesh N, Atul S, Varun M (October 2015). "Oral Pemphigus Vulgaris: Case Report". Ethiop J Health Sci. 25 (4): 367–72. PMID 26949302.
- ↑ Kumar SJ, Nehru Anand SP, Gunasekaran N, Krishnan R (2016). "Oral pemphigus vulgaris: A case report with direct immunofluorescence study". J Oral Maxillofac Pathol. 20 (3): 549. doi:10.4103/0973-029X.190979. PMID 27721634.
- ↑ Rath SK, Reenesh M (October 2012). "Gingival pemphigus vulgaris preceding cutaneous lesion: A rare case report". J Indian Soc Periodontol. 16 (4): 588–91. doi:10.4103/0972-124X.106922. PMC 3590732. PMID 23493851.
- ↑ Vijayan V, Paul A, Babu K, Madhan B (2016). "Desquamative gingivitis as only presenting sign of mucous membrane pemphigoid". J Indian Soc Periodontol. 20 (3): 340–3. doi:10.4103/0972-124X.182602. PMID 27563211.
- ↑ Trimarchi M, Bellini C, Fabiano B, Gerevini S, Bussi M (August 2009). "Multiple mucosal involvement in cicatricial pemphigoid". Acta Otorhinolaryngol Ital. 29 (4): 222–5. PMC 2816372. PMID 20161882.
- ↑ Schellinck AE, Rees TD, Plemons JM, Kessler HP, Rivera-Hidalgo F, Solomon ES (November 2009). "A comparison of the periodontal status in patients with mucous membrane pemphigoid: a 5-year follow-up". J. Periodontol. 80 (11): 1765–73. doi:10.1902/jop.2009.090244. PMID 19905946.
- ↑ Altenburg A, El-Haj N, Micheli C, Puttkammer M, Abdel-Naser MB, Zouboulis CC (October 2014). "The treatment of chronic recurrent oral aphthous ulcers". Dtsch Arztebl Int. 111 (40): 665–73. doi:10.3238/arztebl.2014.0665. PMC 4215084. PMID 25346356.
- ↑ Vaillant L, Samimi M (February 2016). "[Aphthous ulcers and oral ulcerations]". Presse Med (in French). 45 (2): 215–26. doi:10.1016/j.lpm.2016.01.005. PMID 26880080.
- ↑ Bucci P, Carile F, Sangianantoni A, Sangianantoni A, D'Angiò F, Santarelli A, Lo Muzio L (February 2006). "Oral aphthous ulcers and dental enamel defects in children with coeliac disease". Acta Paediatr. 95 (2): 203–7. doi:10.1080/08035250500355022. PMID 16449028.
- ↑ Scully C, Bagan J (March 2008). "Oral mucosal diseases: erythema multiforme". Br J Oral Maxillofac Surg. 46 (2): 90–5. doi:10.1016/j.bjoms.2007.07.202. PMID 17767983.
- ↑ Joseph TI, Vargheese G, George D, Sathyan P (January 2012). "Drug induced oral erythema multiforme: A rare and less recognized variant of erythema multiforme". J Oral Maxillofac Pathol. 16 (1): 145–8. doi:10.4103/0973-029X.92995. PMC 3303512. PMID 22434953.
- ↑ da Silva WB, Ribeiro AL, de Menezes SA, de Jesus Viana Pinheiro J, de Melo Alves-Junior S (December 2014). "Oral capillary hemangioma: a clinical protocol of diagnosis and treatment in adults". Oral Maxillofac Surg. 18 (4): 431–7. doi:10.1007/s10006-013-0436-z. PMID 24263242.
- ↑ Dilsiz A, Aydin T, Gursan N (September 2009). "Capillary hemangioma as a rare benign tumor of the oral cavity: a case report". Cases J. 2: 8622. doi:10.1186/1757-1626-0002-0000008622. PMC 2827094. PMID 20181211.
- ↑ Agarwal S (September 2012). "Treatment of oral hemangioma with 3% sodium tetradecyl sulfate: study of 20 cases". Indian J Otolaryngol Head Neck Surg. 64 (3): 205–7. doi:10.1007/s12070-011-0249-z. PMC 3431531. PMID 23998020.
- ↑ Arul AS, Kumar AR, Verma S, Arul AS (2015). "Oral Kaposi's sarcoma: Sole presentation in HIV seropositive patient". J Nat Sci Biol Med. 6 (2): 459–61. doi:10.4103/0976-9668.160041. PMID 26283853.
- ↑ Mehta S, Garg A, Gupta LK, Mittal A, Khare AK, Kuldeep CM (July 2011). "Kaposi's sarcoma as a presenting manifestation of HIV". Indian J Sex Transm Dis AIDS. 32 (2): 108–10. doi:10.4103/0253-7184.85415. PMC 3195171. PMID 22021973.
- ↑ Castillo JJ, Bibas M, Miranda RN (April 2015). "The biology and treatment of plasmablastic lymphoma". Blood. 125 (15): 2323–30. doi:10.1182/blood-2014-10-567479. PMID 25636338.
- ↑ Vega F, Chang CC, Medeiros LJ, Udden MM, Cho-Vega JH, Lau CC, Finch CJ, Vilchez RA, McGregor D, Jorgensen JL (June 2005). "Plasmablastic lymphomas and plasmablastic plasma cell myelomas have nearly identical immunophenotypic profiles". Mod. Pathol. 18 (6): 806–15. doi:10.1038/modpathol.3800355. PMID 15578069.
- ↑ Castillo J, Pantanowitz L, Dezube BJ (October 2008). "HIV-associated plasmablastic lymphoma: lessons learned from 112 published cases". Am. J. Hematol. 83 (10): 804–9. doi:10.1002/ajh.21250. PMID 18756521.
- ↑ Aricò M, Girschikofsky M, Généreau T, Klersy C, McClain K, Grois N, Emile JF, Lukina E, De Juli E, Danesino C (November 2003). "Langerhans cell histiocytosis in adults. Report from the International Registry of the Histiocyte Society". Eur. J. Cancer. 39 (16): 2341–8. PMID 14556926.
- ↑ Piattelli A, Paolantonio M (August 1995). "Eosinophilic granuloma of the mandible involving the periodontal tissues. A case report". J. Periodontol. 66 (8): 731–6. doi:10.1902/jop.1995.66.8.731. PMID 7473016.
- ↑ Eckardt A, Schultze A (October 2003). "Maxillofacial manifestations of Langerhans cell histiocytosis: a clinical and therapeutic analysis of 10 patients". Oral Oncol. 39 (7): 687–94. PMID 12907208.
- ↑ Kurdoğlu B, Oztemel A, Barış E, Sengüven B (September 2013). "Primary oral myeloid sarcoma: Report of a case". J Oral Maxillofac Pathol. 17 (3): 413–6. doi:10.4103/0973-029X.125209. PMC 3927345. PMID 24574662.
- ↑ Kumar P, Singh H, Khurana N, Urs AB, Augustine J, Tomar R (March 2017). "Diagnostic challenges with intraoral myeloid sarcoma: report of two cases & review of world literature". Exp. Oncol. 39 (1): 78–85. PMID 28361861.
- ↑ Papamanthos MK, Kolokotronis AE, Skulakis HE, Fericean AM, Zorba MT, Matiakis AT (June 2010). "Acute myeloid leukaemia diagnosed by intra-oral myeloid sarcoma. A case report". Head Neck Pathol. 4 (2): 132–5. doi:10.1007/s12105-010-0163-9. PMC 2878628. PMID 20512638.
- ↑ Sykara M, Ntovas P, Kalogirou EM, Tosios KI, Sklavounou A (August 2017). "Oral lymphoepithelial cyst: A clinicopathological study of 26 cases and review of the literature". J Clin Exp Dent. 9 (8): e1035–e1043. doi:10.4317/jced.54072. PMC 5601105. PMID 28936296.
- ↑ Stramandinoli-Zanicotti RT, de Castro Ávila LF, de Azevedo Izidoro AC, Izidoro FA, Schussel JL (2012). "Lymphoepithelial cysts of oral mucosa: two cases in different regions". Bull. Tokyo Dent. Coll. 53 (1): 17–22. PMID 22452887.
- ↑ De Ponte FS, Brunelli A, Marchetti E, Bottini DJ (March 2002). "Sublingual epidermoid cyst". J Craniofac Surg. 13 (2): 308–10. PMID 12000893.
- ↑ Ozan F, Polat HB, Ay S, Goze F (March 2007). "Epidermoid cyst of the buccal mucosa: a case report". J Contemp Dent Pract. 8 (3): 90–6. PMID 17351686.
- ↑ Puranik SR, Puranik RS, Prakash S, Bimba M (2016). "Epidermoid cyst: Report of two cases". J Oral Maxillofac Pathol. 20 (3): 546. doi:10.4103/0973-029X.190965. PMC 5051311. PMID 27721628.
- ↑ Zucker SH, Altman R (August 1973). "An on-the-job vocational training program for adolescent trainable retardates". Train Sch Bull (Vinel). 70 (2): 106–10. PMID 4745964.
- ↑ Sato M, Morita K, Kabasawa Y, Harada H (September 2016). "Bilateral nasolabial cysts: a case report". J Med Case Rep. 10 (1): 246. doi:10.1186/s13256-016-1024-2. PMC 5015322. PMID 27604349.
- ↑ Sumer AP, Celenk P, Sumer M, Telcioglu NT, Gunhan O (February 2010). "Nasolabial cyst: case report with CT and MRI findings". Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 109 (2): e92–4. doi:10.1016/j.tripleo.2009.09.034. PMID 20034824.