Oral candidiasis differential diagnosis: Difference between revisions
Jump to navigation
Jump to search
Ahmed Younes (talk | contribs) No edit summary |
Ahmed Younes (talk | contribs) No edit summary |
||
| Line 81: | Line 81: | ||
! | ! | ||
! | ! | ||
|- | |||
|Oral Candidiasis | |||
| | |||
* Dysphagia or odynphagia | |||
* White patches on the mouth and tongue | |||
| | |||
*[[Newborn]] babies | |||
*Denture users | |||
*Poorly controlled [[diabetes]] | |||
*As a side effect of medication, most commonly having taken [[antibiotic]]s. Inhaled [[corticosteroids]] for treatment of lung conditions (e.g, [[asthma]] or [[COPD]]) may also result in oral candidiasis which may be reduced by regularly rinsing the mouth with water after taking the medication. | |||
*People with poor [[nutrition]], specifically vitamin A, iron and folate deficiencies. | |||
*People with an [[immune deficiency]] (e.g. as a result of [[AIDS]]/[[HIV]] or [[chemotherapy]] treatment). | |||
*Women undergoing hormonal changes, like pregnancy or those on birth control pills. | |||
*Organ transplantation patients | |||
| | |||
* Clinical diagnosis | |||
* Confirmatory tests rarely needed | |||
|'''Localized candidiasis''' | |||
* Oral and esophageal candidasis | |||
* Candida vulvovaginitis | |||
* Chronic mucocutaneous candidiasis | |||
'''Invasive candidasis''' | |||
* Candidaemia | |||
* Candida endocarditis | |||
* Candida osteoarticular disease | |||
| | |||
* Oral candidiaisis is a benign self limiting disease unless accompanied by immunosuppression. | |||
| | |||
|- | |||
|Herpes simplex oral lesions | |||
| | |||
* Fever | |||
* Sore throat | |||
* Painful [[ulcer]]s | |||
| | |||
* Stress | |||
* Recent URTI | |||
* Female sex. | |||
| | |||
* Physical examination | |||
* Viral culture | |||
* Tzank smear | |||
| | |||
* Orofacial Infection | |||
* [[Herpes simplex anogenital infection|Anogenital Infection]] | |||
* [[Herpes simplex ocular infection|Ocular Infection]] | |||
* [[Herpes simplex encephalitis|Herpes Encephalitis]] | |||
* [[Herpes simplex neonatorum|Neonatal Herpes]] | |||
* [[Herpetic whitlow|Herpetic Whitlow]] | |||
* [[Herpes gladiatorum|Herpes Gladiatorum]] | |||
| | |||
* The symptoms of primary HSV infection generally resolve within two weeks | |||
| | |||
|- | |||
|Aphthous ulcers | |||
| | |||
* Painful, red spot or bump that develops into an open [[ulcer]] | |||
| | |||
* Being a female | |||
* Between the ages of 10-40 | |||
* Family history of aphthous ulcers | |||
| | |||
* Physical examination | |||
* Diagnosis of exclusion | |||
| | |||
* Oral cavity | |||
| | |||
* Self-limiting , [[Pain]] decreases in 7 to 10 days, with complete healing in 1 to 3 weeks | |||
| | |||
|- | |- | ||
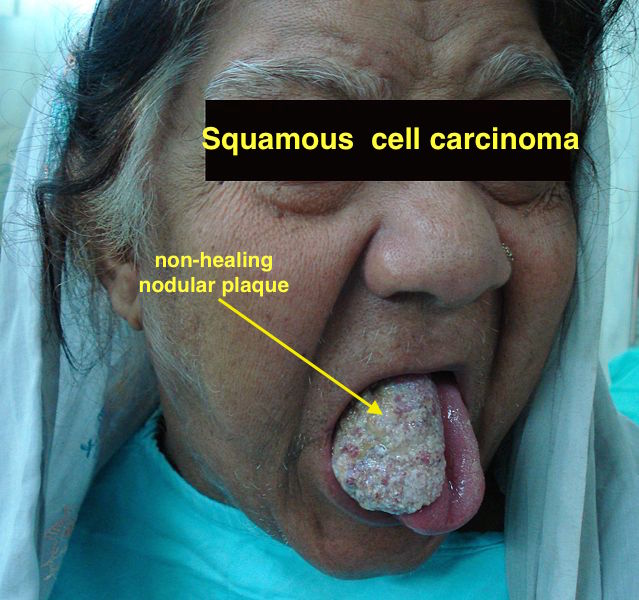
|[[Squamous cell carcinoma]] | |[[Squamous cell carcinoma]] | ||
Revision as of 16:30, 9 May 2017
|
Oral candidiasis Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Oral candidiasis differential diagnosis On the Web |
|
American Roentgen Ray Society Images of Oral candidiasis differential diagnosis |
|
Risk calculators and risk factors for Oral candidiasis differential diagnosis |
Overview
Differential diagnosis
Oropharyngeal candidiasis must be differentiated from its different kinds and from various other diseases that can cause stomatitis or glossitis:[1][2]
- Aphthous ulcers
- Herpes simplex oral lesions
- Tumors of the tongue
- Autoimmune diseases[7]
- Behcet's syndrome[8]
- CMV oral ulcers
- Blastomycosis oral lesions
- Crohn's disease
- Agranulocytosis
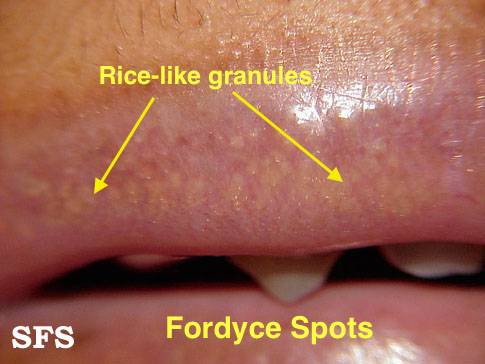
- Fordyce's spots
- Drug induced
- Burning mouth syndrome
- Syphilis
- Coxsackie virus accompanies involvement of the hands and the mouth
- HIV
- VZV or Chicken pox
| Disease | Presentation | Risk Factors | Diagnosis | Affected Organ Systems | Important features | Picture |
|---|---|---|---|---|---|---|
| Diseases predominantly affecting the oral cavity | ||||||
| Oral Candidiasis |
|
|
|
Localized candidiasis
Invasive candidasis
|
|
|
| Herpes simplex oral lesions |
|
|
|
|
||
| Aphthous ulcers |
|
|
|
|
|
|
| Squamous cell carcinoma |
|
|
| |||
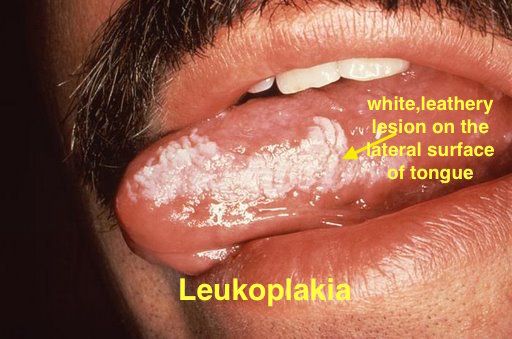
| Leukoplakia |
|
|
|
| ||
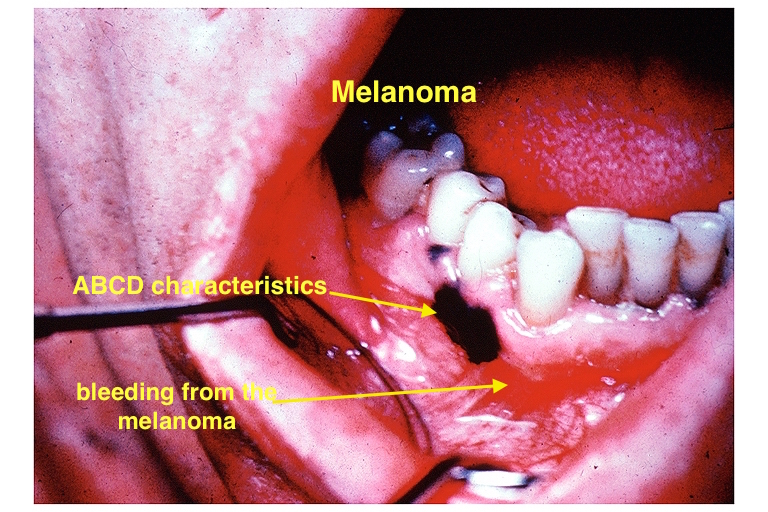
| Melanoma |
|
|
|
|
| |
| Fordyce spots |
|
|
|
|
| |
| Burning mouth syndrome |
|
|
||||
| Torus palatinus |
|
|
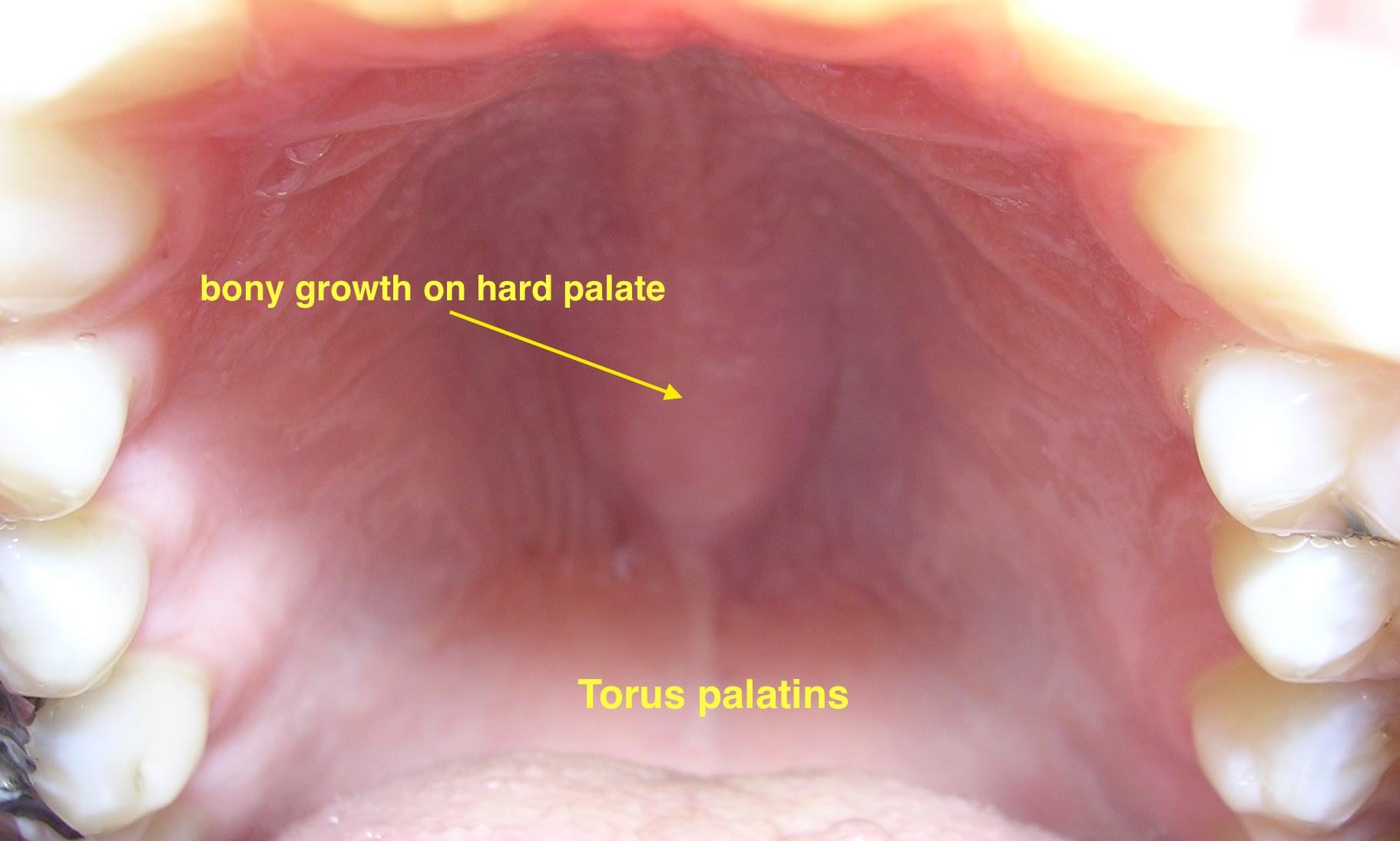
| |||
| Diseases involving oral cavity and other organ systems | ||||||
| Behcet's disease |
|
|
|
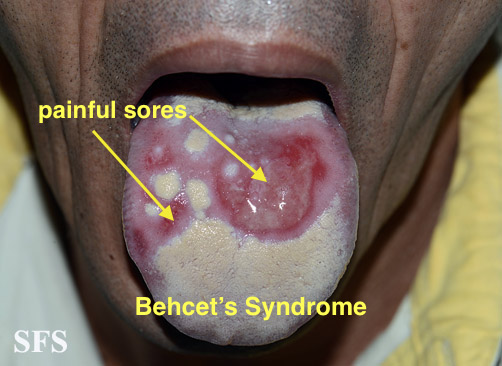
| ||
| Crohn's disease |
|
|
|
|
||
| Agranulocytosis |
|
|
||||
| Syphilis[11] |
|
|
|
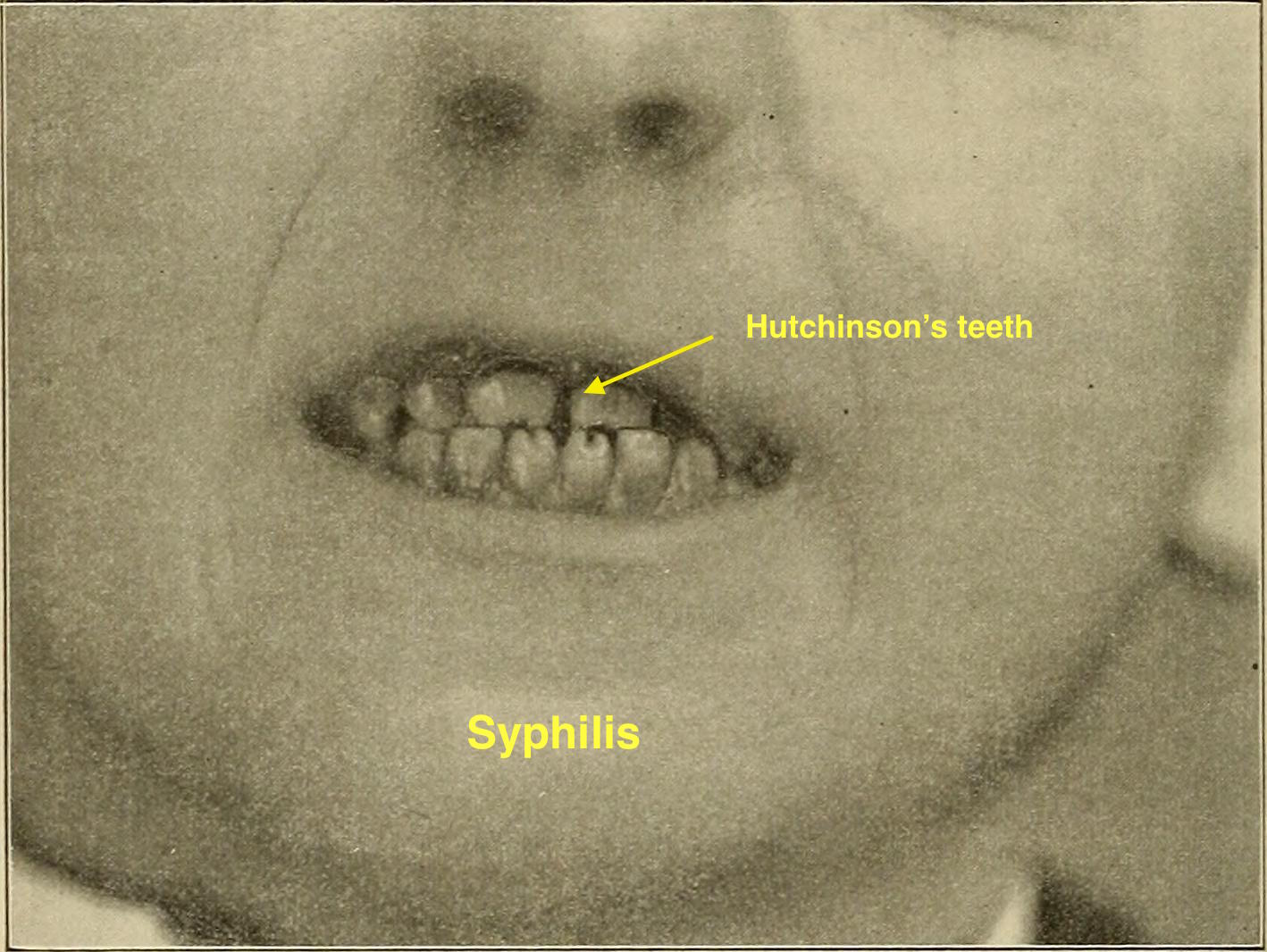
| ||
| Coxsackie virus |
|
|
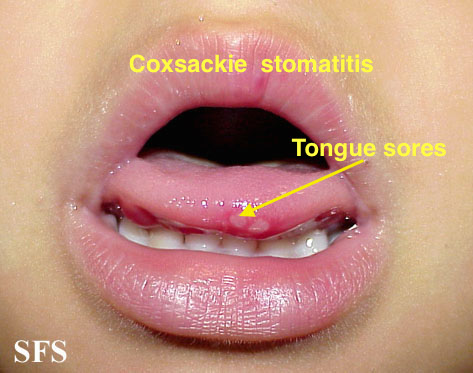
| |||
| Chicken pox |
|
|
|
|
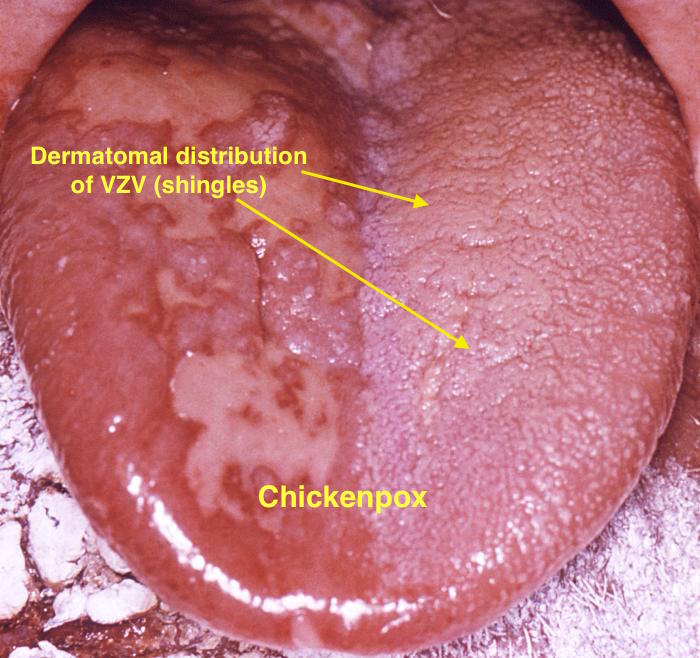
| |
| Measles |
|
|
|
|
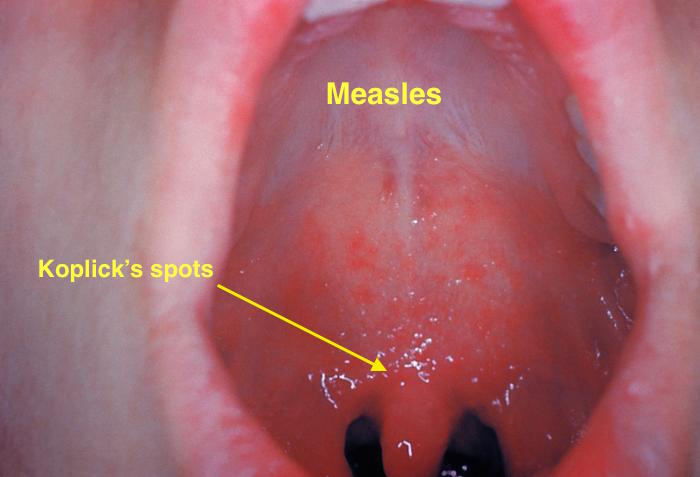
| |
References
- ↑ Mandell; Gouglas, Gordon; Bennett, John. Principles and Practice of Infectious Diseases. Harvard Medical School: WILEY MEDICAL. p. 383. ISBN 0-471-87643-7. Unknown parameter
|firs1t=ignored (help) - ↑ Scully C (1999). "A review of common mucocutaneous disorders affecting the mouth and lips". Ann Acad Med Singapore. 28 (5): 704–7. PMID 10597357.
- ↑ R. Morgan, J. Tsang, N. Harrington & L. Fook (2001). "Survey of hospital doctors' attitudes and knowledge of oral conditions in older patients". Postgraduate medical journal. 77 (908): 392–394. PMID 11375454. Unknown parameter
|month=ignored (help) - ↑ D. Grady, J. Greene, T. E. Daniels, V. L. Ernster, P. B. Robertson, W. Hauck, D. Greenspan, J. Greenspan & S. Jr Silverman (1990). "Oral mucosal lesions found in smokeless tobacco users". Journal of the American Dental Association (1939). 121 (1): 117–123. PMID 2370378. Unknown parameter
|month=ignored (help) - ↑ P. DeMatos, D. S. Tyler & H. F. Seigler (1998). "Malignant melanoma of the mucous membranes: a review of 119 cases". Annals of surgical oncology. 5 (8): 733–742. PMID 9869521. Unknown parameter
|month=ignored (help) - ↑ Barry Ladizinski & Kachiu C. Lee (2014). "A nodular protuberance on the hard palate". JAMA. 311 (15): 1558–1559. doi:10.1001/jama.2014.271. PMID 24737369. Unknown parameter
|month=ignored (help) - ↑ Magliocca KR, Fitzpatrick SG (2017) Autoimmune Disease Manifestations in the Oral Cavity. Surg Pathol Clin 10 (1):57-88. DOI:10.1016/j.path.2016.11.001 PMID: 28153136
- ↑ Dalghous AM, Freysdottir J, Fortune F (2006). "Expression of cytokines, chemokines, and chemokine receptors in oral ulcers of patients with Behcet's disease (BD) and recurrent aphthous stomatitis is Th1-associated, although Th2-association is also observed in patients with BD". Scand J Rheumatol. 35 (6): 472–5. PMID 17343257.
- ↑ Ann M. Gillenwater, Nadarajah Vigneswaran, Hanadi Fatani, Pierre Saintigny & Adel K. El-Naggar (2013). "Proliferative verrucous leukoplakia (PVL): a review of an elusive pathologic entity!". Advances in anatomic pathology. 20 (6): 416–423. doi:10.1097/PAP.0b013e3182a92df1. PMID 24113312. Unknown parameter
|month=ignored (help) - ↑ Andrès E, Zimmer J, Affenberger S, Federici L, Alt M, Maloisel F. (2006). "Idiosyncratic drug-induced agranulocytosis: Update of an old disorder". Eur J Intern Med. 17 (8): 529–35. Text "pmid 17142169" ignored (help)
- ↑ title="By Internet Archive Book Images [No restrictions], via Wikimedia Commons" href="https://commons.wikimedia.org/wiki/File%3AA_manual_of_syphilis_and_the_venereal_diseases%2C_(1900)_(14595882378).jpg"
- ↑ Feikin DR, Lezotte DC, Hamman RF, Salmon DA, Chen RT, Hoffman RE (2000). "Individual and community risks of measles and pertussis associated with personal exemptions to immunization". JAMA. 284 (24): 3145–50. PMID 11135778.
- ↑ Ratnam S, West R, Gadag V, Williams B, Oates E (1996). "Immunity against measles in school-aged children: implications for measles revaccination strategies". Can J Public Health. 87 (6): 407–10. PMID 9009400.