Secondary adrenal insufficiency
| Adrenal insufficiency | |
 | |
|---|---|
| Adrenal gland | |
| ICD-10 | E27.1-E27.4 |
| ICD-9 | 255.4 |
| MeSH | D000309 |
For patient information click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and keywords: hypocortisolism; hypocorticism; adrenocortical hypofunction
Overview
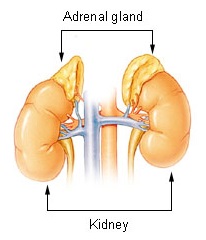
Adrenal insufficiency is a condition in which the adrenal glands, located above the kidneys, do not produce adequate amounts of steroid hormones (chemicals produced by the body that regulate organ function), primarily cortisol, but may also include impaired aldosterone production (a mineralocorticoid) which regulates sodium, potassium and water retention.[1][2] Craving for salt or salty foods due to the urinary losses of sodium is common.[3]
Addison's disease and congenital adrenal hyperplasia can manifest as adrenal insufficiency. If not treated, adrenal insufficiency may result in severe abdominal pains, diarrhea, vomiting, profound muscle weakness and fatigue, depression, extremely low blood pressure (hypotension), weight loss, kidney failure, changes in mood and personality, and shock (adrenal crisis).[4] An adrenal crisis often occurs if the body is subjected to stress, such as an accident, injury, surgery, or severe infection; death may quickly follow.[4]
Adrenal insufficiency can also occur when the hypothalamus or the pituitary gland, both located at the base of the skull, does not make adequate amounts of the hormones that assist in regulating adrenal function.[1][5][6] This is called secondary adrenal insufficiency and is caused by lack of production of ACTH in the pituitary or lack of CRH in the hypothalamus.[7]
Classification
There are three major types of adrenal insufficiency.
- Primary adrenal insufficiency is due to impairment of the adrenal glands.
- One subtype is called idiopathic or unknown cause of adrenal insufficiency.
- 80% are due to an autoimmune disease called Addison's disease or autoimmune adrenalitis.
- Other cases are due to congenital adrenal hyperplasia or an adenoma (tumor) of the adrenal gland.
- Secondary adrenal insufficiency is caused by impairment of the pituitary gland or hypothalamus.[8] The most common cause in the United States is exogenous steroid use. Other causes are a pituitary adenoma or microadenoma, hypothalamic tumor (surgical removal of a pituitary tumor can also suppress production of ACTH and lead to adrenal deficiency); Sheehan's syndrome, which is associated with impairment of only the pituitary gland.
- Tertiary adrenal insufficiency is due to hypothalamic disease and decrease in corticotropin releasing factor (CRF).[9]
Causes
Common Causes
- Acute adrenal insufficiency
- Addison's disease (autoimmune adrenalitis)
- Septic shock
- Waterhouse-Friderichsen syndrome
- Addisonian crisis in case of:
- Discontinuing corticosteroid therapy without tapering the dosage
- Surgery, illness or any other form of stress in patients with long-term corticosteroid therapy
- Chronic adrenal insufficiency
Causes by Organ System
Causes in Alphabetical Order
Diagnosis
Symptoms
There is often the slow insidious onset of the following symptoms (in alphabetical order):
- Dehydration
- Diarrhea
- Disorientation
- Dizziness
- Hypoglycemia
- Muscle aches
- Nausea
- Tanning of the skin that may be patchy or even all over the body. Characteristic sites of tanning are skin creases (e.g. of the hands) and the inside of the cheek (buccal mucosa).
- Tiredness
- Vomiting
- Weakness
- Weight loss
Physical Examination
Vital Signs
- Low blood pressure that falls further when standing (orthostatic hypotension)
- Cardiovascular collapse may be present
Skin
- There can be tanning of the skin. Tanning of the skin that may be patchy or even all over the body. Characteristic sites of tanning are skin creases (e.g. of the hands) and the inside of the cheek (buccal mucosa).
- Vitiligo may also be present.[4]
Neck
Goitre may be present
Laboratory Findings
ACTH Stimulation Test
If the person is in adrenal crisis, the ACTH stimulation test[10] may be given. If not in crisis, cortisol, ACTH, aldosterone, renin, potassium and sodium are tested from a blood sample before the decision is made if the ACTH stimulation test needs to be performed. X-rays or CT of the adrenals may also be done.[1] The best test for adrenal insufficiency of autoimmune origin, representing more than ninety percent of all cases in a Western population, is measurement of 21-hydroxylase autoantibodies.
| Source of pathology | CRH | ACTH | DHEA | DHEA-S | cortisol | aldosterone | renin | Na | K | Causes5 |
| hypothalamus (tertiary)1 |
low | low | low | low | low3 | low | low | low | low | tumor of the hypothalamus (adenoma), antibodies, environment (i.e. toxins), head injury |
| pituitary (secondary) |
high2 | low | low | low | low3 | low | low | low | low | tumor of the pituitary (adenoma), antibodies, environment, head injury, surgical removal6, Sheehan's syndrome |
| adrenal glands (primary)7 |
high | high | high | high | low4 | low | high | low | high | tumor of the adrenal (adenoma), stress, antibodies, environment, Addison's Disease, trauma, surgical removal (resection), miliary tuberculosis of the adrenal |
| 1 | Automatically includes diagnosis of secondary (hypopituitarism) |
| 2 | Only if CRH production in the hypothalamus is intact |
| 3 | Value doubles or more in stimulation |
| 4 | Value less than doubles in stimulation |
| 5 | Most common, does not include all possible causes |
| 6 | Usually because of very large tumor (macroadenoma) |
| 7 | Includes Addison's disease |
Treatment
- Adrenal crisis
- Intravenous fluids[4]
- Intravenous steroid (Solu-Cortef/injectable hydrocortisone) later hydrocortisone, prednisone or methylpredisolone tablets[4]
- Rest
- Cortisol deficiency (primary and secondary)
- Hydrocortisone (Cortef)
- Prednisone (Deltasone)
- Prednisolone (Delta-Cortef)
- Methylprednisolone (Medrol)
- Dexamethasone (Decadron)
- Mineralocorticoid deficiency (low aldosterone)
- Fludrocortisone Acetate
(To balance sodium, potassium and increase water retention)[4]
See also
- Addison disease, primary adrenocortical insufficiency
- ACTH stimulation test
- Cushing's syndrome, overproduction of cortisol
- Insulin tolerance test, another test used to identify sub-types of adrenal insufficiency
- Adrenal fatigue (hypoadrenia), a term used in alternative medicine to describe a believed exhaustion of the adrenal glands
References
- ↑ 1.0 1.1 1.2 Eileen K. Corrigan (2007). "Adrenal Insufficiency (Secondary Addison's or Addison's Disease)". NIH Publication No. 90-3054.
- ↑ Adrenal+Insufficiency at the US National Library of Medicine Medical Subject Headings (MeSH)
- ↑ Ten S, New M, Maclaren N (2001). "Clinical review 130: Addison's disease 2001". J. Clin. Endocrinol. Metab. 86 (7): 2909–22. doi:10.1210/jc.86.7.2909. PMID 11443143.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Ashley B. Grossman, MD (2007). "Addison's Disease". Adrenal Gland Disorders.
- ↑ Brender E, Lynm C, Glass RM (2005). "JAMA patient page. Adrenal insufficiency". JAMA. 294 (19): 2528. doi:10.1001/jama.294.19.2528. PMID 16287965.
- ↑ "Dorlands Medical Dictionary:adrenal insufficiency".
- ↑ "Secondary Adrenal Insufficiency: Adrenal Disorders: Merck Manual Professional".
- ↑ "hypopituitary". 2006.
- ↑ http://www.endotext.org/adrenal/adrenal13/adrenal13.htm
- ↑ Henzen C (2011). "[Adrenal insufficiency--diagnosis and treatment in clinical practice]". Ther Umsch. 68 (6): 337–43. doi:10.1024/0040-5930/a000174. PMID 21656493. Unknown parameter
|month=ignored (help)
ca:Insuficiència suprarenal de:Nebennierenrindeninsuffizienz he:תת פעילות בלוטת יותרת הכליה