Kallmann syndrome
For patient information click here
| Kallmann syndrome | |
 | |
|---|---|
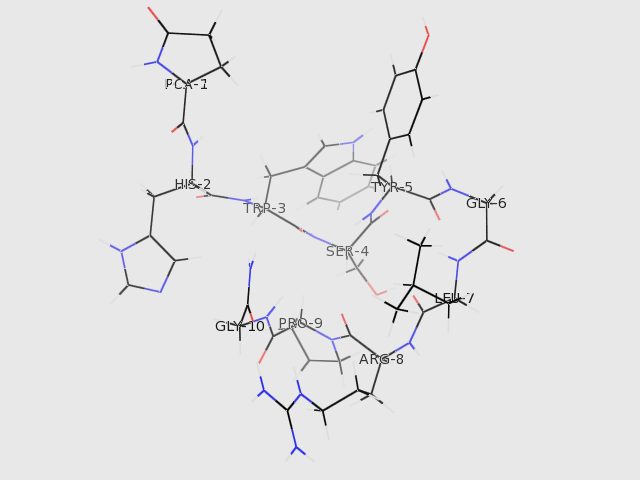
| The structure of GNRH1 (from PDB: 1YY1) | |
| ICD-10 | E23.0 |
| ICD-9 | 253.4 |
| OMIM | 308700 147950 244200 138850 607002 |
| DiseasesDB | 7091 |
| MeSH | D017436 |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
Kallmann syndrome is an example of hypogonadism (decreased functioning of the sex hormone-producing glands) caused by a deficiency of gonadotropin-releasing hormone (GnRH), which is created by the hypothalamus. Kallmann syndrome is also known as hypothalamic hypogonadism, familial hypogonadism with anosmia, or hypogonadotropic hypogonadism, reflecting its disease mechanism.
Kallmann syndrome is a form of secondary hypogonadism reflecting the fact the primary cause of the defect in sex hormone production lies within the pituitary and hypothalamus rather than a physical defect of the testes or ovaries themselves.
Kallmann syndrome was described in 1944 by Franz Josef Kallmann, a German-American geneticist.[1][2] However, others - such as the Spanish doctor Aureliano Maestre de San Juan - had noticed a correlation between anosmia and hypogonadism in 1856.
The most well known person who has Kallmann syndrome in modern times is the jazz vocalist Jimmy Scott. In 2004, Canadian writer Brian Brett published a memoir, Uproar's Your Only Music, about growing up with Kallmann syndrome.
Epidemiology
Kallmann syndrome occurs at a rate of 1 in 10,000 male births and 1 in 50,000 female births. It may be inherited as an X-linked condition, an autosomal dominant condition or as an autosomal recessive condition. Statistics are sparse, but it seems that autosomal dominant is the most common form of heredity.
One recent paper [3] quoted an incidence in males of 0.025%, or 1 in 4,000, with the female incidence being 3 to 5 times less.
Even though mutations in the KAL-1 gene on the X chromosome can cause Kallmann syndrome, only 11-14% of patients with Kallmann syndrome have detectable KAL-1 mutations.
Autosomal dominant mutations have been described with the FGFR-1 (8p12) gene, sometimes referred to as the KAL-2 gene. This is thought to cause about 10% of cases.
Autosomal recessive mutations of the GnRH receptor gene (4q13.2) have also been reported.[3] This defect appears to produce a wider spectrum of physical symptoms than with the other gene defects, and the defect lies in the ability of the pituitary gland to recognise GnRH, rather than the ability of the hypothalamus to produce GnRH. It is debatable as to whether this is in fact Kallmann syndrome since the GnRH receptor development is not related to anosmia.
There may also be no obvious family history of inheritance (sporadic cases). However, it is possible for Kallmann syndrome genes to be passed on to children of a sporadic case.
Pathophysiology
Under normal conditions, GnRH travels from the hypothalamus to the pituitary gland via the hypophyseal portal system, where it triggers production and release of gonadotropins (LH and FSH) from the gonadotropes. When GnRH is low, the pituitary does not create the normal amount of gonadotropins. The gonadotropins normally increase the production of gonadal steroids, so when they are low, these steroids will be low as well.
In Kallmann syndrome, the GnRH neurons do not migrate properly from the olfactory placode to the hypothalamus during development. The olfactory bulbs also fail to form or have hypoplasia, leading to anosmia or hyposmia.
Kallmann syndrome can be inherited as an X-linked recessive trait, in which case there is a defect in the KAL1 gene, which maps to chromosome Xp22.3.[4] KAL encodes a neural cell adhesion molecule, anosmin-1. Anosmin-1 is normally expressed in the brain, facial mesenchyme, mesonephros and metanephros. It is required to promote migration of GnRH neurons into the hypothalamus. It also allows migration of olfactory neurons from the olfactory bulbs to the hypothalamus.
An autosomal dominant gene on chromosome 8 {8p12} (KAL-2 or FGFR-1 (fibroblast growth factor receptor 1)) is thought to cause about 10% of cases. There is some recent evidence to suggest a degree of linkage between the KAL-1 and FGFR-1 genes.
An additional autosomal cause of Kallmann syndrome has been reported[5] by a mutations in the prokineticin receptor-2 gene (PROKR2)(KAL-3) at position 20p13 and its ligand prokineticin 2 (PROK2)(KAL-4) at position 3p21.1. It was noted that mutations in these genes brought about various degrees of olfactory and reproductive dysfunction, but not the other symptoms seen in KAL-1 and KAL-2 forms of Kallmann Syndrome. The authors of the paper suggested that up to 30% of all Kallmann Syndrome cases can be linked to known genetic mutations.
Features
Kallmann syndrome is characterized by:
- Hypogonadotropic hypogonadism (a lack of the pituitary hormones LH and FSH)
- Congenital (present from birth) anosmia (complete inability to smell) or hyposmia (decreased ability to smell)
It can occasionally be associated with optic problems, such as colour blindness or optic atrophy, nerve deafness, cleft palate, cryptorchidism, renal agenesis, and mirror movement disorder. However, it is not clear at this time how or if these other problems have the same cause as the hypogonadism and anosmia. These problems are more often present in those without Kallmann syndrome.
Males present with delayed puberty and may have micropenis (although congenital micropenis is not present in the majority of male KS cases).
Females present with delayed puberty (i.e. primary amenorrhea) and lack of secondary sex characteristics, such as breast development.
Diagnosis
The diagnosis is often one of exclusion found during the workup of delayed puberty. The presence of anosmia together with micropenis in boys should suggest Kallmann syndrome (although micropenis alone may have other causes).
Treatment
Treatment is directed at restoring the deficient hormones -- known as hormone replacement therapy (HRT). Males are administered human chorionic gonadotropin (hCG) or testosterone. Females are treated with oestrogen and progestins.
To induce fertility in males or females, GnRH (aka LHRH) is administered by an infusion pump, or hCG/hMG/FSH/LH combinations are administered through regular injections. Fertility is only maintained whilst actually being treated with these hormones. Once fertility treatment stops it is necessary to revert to the normal HRT of testosterone for men and oestrogen + progestins for women.
The main health risk, for both men and women, of untreated Kallmann Syndrome is osteoporosis. Therefore, regular bone density scans (every 2 years or so) are advisable, even if being treated with HRT. Additional medication specifically for osteoporosis is necessary in some cases.
Differential Diagnosis
Kallmann's Syndrome should be differentiated from other causes of gonadotropin (FSH/LH) deficiency. The following table outlines the major differentials:[6][7][8][9][10][11][12][13][14][15]
| Diseases | Clinical findings | Diagnosis | Manangement | |
|---|---|---|---|---|
| Congenital diseases | Klinefelter syndrome | Clinical features of Klinefelter syndrome are as the following:[6]
|
|
|
| Kallmann syndrome | Clinical features of Kallmann syndrome include:
|
| ||
| Cryptorchidism | Clinical features of cryptorchidism include:[7]
|
|
| |
| Male diseases | Testicular torsion | Patients of testicular torsion usually present with following:[8] |
|
Management is mainly surgical through detorsion and fixation of the affected testes. |
| Orchitis | Clincial features of orchitis include the following:[9][10]
|
|
| |
| Female diseases | Polycystic ovarian syndrome (PCOS) | Possible clinical findings in cases of PCOS:[11] |
|
|
| Pelvic inflammatory disease | Patients usually present with the following:[13][14]
|
|
| |
| Endometriosis | Clinical features of endometriosis include the following:[15]
|
|
Medical therapy:
Surgery:
| |
References
- ↑ Kallmann FJ, Schönfeld WA, Barrera SE. The genetic aspects of primary eunuchoidism. Am J Ment Defic 1943-1944;48:203-236.
- ↑ Template:WhoNamedIt
- ↑ 3.0 3.1 Quinton R. Topical Endocrinology 22. (15-20)
- ↑ MacColl G, Bouloux P, Quinton R (2002). "Kallmann syndrome: adhesion, afferents, and anosmia". Neuron. 34 (5): 675–8. PMID 12062015.
- ↑ Dode C, et al. Kallmann syndrome: mutations in the genes encoding prokineticin-2 and prokineticin receptor-2. PLoS Genet.2: e175, 2006.
- ↑ 6.0 6.1 Denschlag, Dominik, MD; Clemens, Tempfer, MD; Kunze, Myriam, MD; Wolff, Gerhard, MD; Keck, Christoph, MD (October 2004), "Assisted reproductive techniques in patients with Klinefelter syndrome: A critical review", Fertility and Sterility, 82 (4): 775–779, doi:10.1016/j.fertnstert.2003.09.085
- ↑ 7.0 7.1 Virtanen HE, Bjerknes R, Cortes D, Jørgensen N, Rajpert-De Meyts E, Thorsson AV; et al. (2007). "Cryptorchidism: classification, prevalence and long-term consequences". Acta Paediatr. 96 (5): 611–6. doi:10.1111/j.1651-2227.2007.00241.x. PMID 17462053.
- ↑ 8.0 8.1 Schmitz D, Safranek S (2009). "Clinical inquiries. How useful is a physical exam in diagnosing testicular torsion?". J Fam Pract. 58 (8): 433–4. PMID 19679025.
- ↑ 9.0 9.1 Trojian TH, Lishnak TS, Heiman D (2009). "Epididymitis and orchitis: an overview". Am Fam Physician. 79 (7): 583–7. PMID 19378875.
- ↑ 10.0 10.1 Stewart A, Ubee SS, Davies H (2011). "Epididymo-orchitis". BMJ. 342: d1543. PMID 21490048.
- ↑ 11.0 11.1 Christine Cortet-Rudelli, Didier Dewailly (2006). "Diagnosis of Hyperandrogenism in Female Adolescents". Hyperandrogenism in Adolescent Girls. Armenian Health Network, Health.am. Unknown parameter
|month=ignored (help) - ↑ Legro RS, Barnhart HX, Schlaff WD (2007). "Clomiphene, Metformin, or Both for Infertility in the Polycystic Ovary Syndrome". N Engl J Med. 356 (6): 551–566. PMID 17287476.
- ↑ 13.0 13.1 Brunham RC, Gottlieb SL, Paavonen J (2015). "Pelvic inflammatory disease". N. Engl. J. Med. 372 (21): 2039–48. doi:10.1056/NEJMra1411426. PMID 25992748.
- ↑ 14.0 14.1 Ford GW, Decker CF (2016). "Pelvic inflammatory disease". Dis Mon. 62 (8): 301–5. doi:10.1016/j.disamonth.2016.03.015. PMID 27107781.
- ↑ 15.0 15.1 Murphy AA (2002). "Clinical aspects of endometriosis". Ann N Y Acad Sci. 955: 1–10, discussion 34-6, 396–406. PMID 11949938.
- ↑ Legro RS, Barnhart HX, Schlaff WD (2007). "Clomiphene, Metformin, or Both for Infertility in the Polycystic Ovary Syndrome". N Engl J Med. 356 (6): 551–566. PMID 17287476.
External links
- Kallmann's Syndrome Mailing List
- Information web site on Kallmann's syndrome
- Man, 33, seeks puberty The case of Lawrence Koomson a physician who was treated for the condition as filmed in the documentary. (BBC)
de:Kallmann-Syndrom it:Sindrome di Kallmann he:תסמונת קלמן nl:Syndroom van Kallmann fi:Kallmannin oireyhtymä