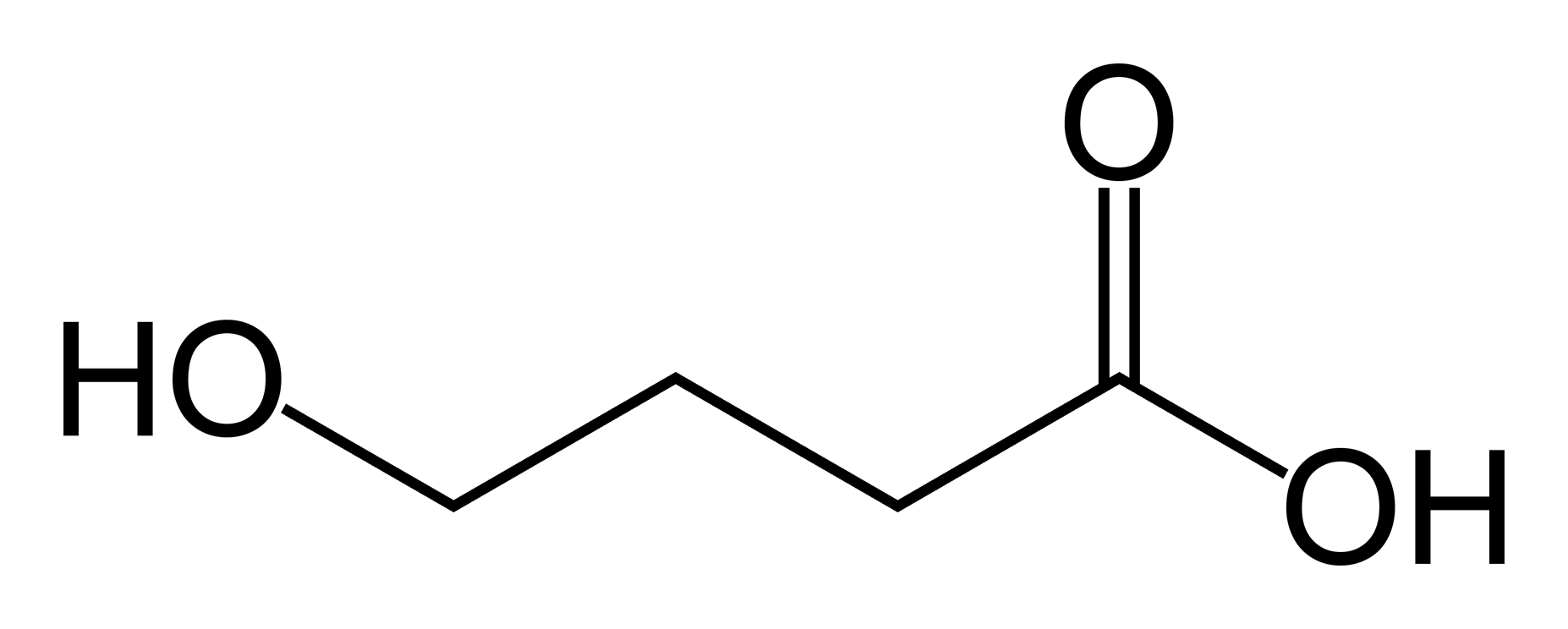
Gamma-Hydroxybutyric acid
 | |
| File:GHB-3D-balls.png | |
| Clinical data | |
|---|---|
| Synonyms | γ-Hydroxybutyric acid γ-Hydroxybutyrate GHB |
| Pregnancy category |
|
| Routes of administration | Usually oral; intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 25% (oral) |
| Metabolism | 95%, mainly Hepatic, also in blood and tissues |
| Elimination half-life | 30–60 minutes |
| Excretion | 5%, renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
| Formula | C4H8O3 |
| Molar mass | 104.10 g/mol (GHB) 126.09 g/mol (sodium salt) 142.19 g/mol (potassium salt) |
| 3D model (JSmol) | |
| |
| (verify) | |
γ-Hydroxybutyric acid (GHB), also known as 4-hydroxybutanoic acid and sodium oxybate (INN) when used for medicinal purposes,[1] is a naturally occurring substance found in the central nervous system, wine, beef, small citrus fruits, and almost all animals in small amounts.[2] It is also categorized as an illegal drug in many countries.[3] It is currently regulated in Australia and New Zealand, Canada, most of Europe and in the US. GHB as the sodium salt, known as sodium oxybate, is sold by Jazz Pharmaceuticals under the name Xyrem[4] to treat cataplexy and excessive daytime sleepiness in patients with narcolepsy.
GHB has been used in a medical setting as a general anesthetic, to treat conditions such as insomnia, clinical depression, narcolepsy, and alcoholism, and to improve athletic performance.[5] It is also used as an intoxicant (illegally in many jurisdictions) or as a date rape drug.[6] GHB is naturally produced in the human body's cells and is structurally related to the ketone body beta-hydroxybutyrate. As a supplement/drug, it is used most commonly in the form of a salt.[7] GHB is also produced as a result of fermentation, and so is found in small quantities in some beers and wines. Succinic semialdehyde dehydrogenase deficiency is a disease that causes GHB to accumulate in the blood.
History
Synthesis of the chemical GHB was first reported in 1874 by Alexander Zaytsev,[8] but the first major research into its use in humans was conducted in the early 1960s by Dr. Henri Laborit to use in studying the neurotransmitter GABA.[9] It quickly found a wide range of uses due to its minimal side-effects and short duration of action, the only difficulties being the narrow therapeutic dosage range (despite an unusually high Template:LD50)[citation needed] and the dangers presented by its combination with alcohol and other central nervous system depressants.
GHB was widely used in France, Italy, and other European countries for several decades as a sleeping agent and an anesthetic in childbirth but problems with its abuse potential and development of newer drugs have led to a decrease in legitimate medical use of GHB in recent times. In the Netherlands, GHB could be bought as aphrodisiac and euphoriant in a smartshop for several years, until several incidents caused it to become regulated which no longer made it possible to buy it at smartshops. The only common medical applications for GHB today are in the treatment of narcolepsy and more rarely alcoholism. In the typical scenario, GHB has been synthesized from γ-butyrolactone (GBL) by adding sodium hydroxide (lye) in ethanol or water. As of late, GBL has become controlled in many countries and more circuitous routes have to be taken, such as those starting with tetrahydrofuran (THF).
A popular children's toy, Bindeez (also known as Aqua Dots, in the United States), produced by Melbourne company Moose, was banned in Australia in early November 2007 when it was discovered that 1,4-butanediol (1,4-B), which is metabolized into GHB, had been substituted for the non-toxic plasticiser 1,5-pentanediol in the bead manufacturing process. Three young children were hospitalized as a result of ingesting a large number of the beads, and the toy was recalled.[10]
Pharmacology
GHB has at least two distinct binding sites[11] in the central nervous system. GHB is an agonist at the newly-characterized GHB receptor, which is excitatory,[12][13] and it is a weak agonist at the GABAB receptor, which is inhibitory.[13] GHB is a naturally-occurring substance that acts in a similar fashion to some neurotransmitters in the mammalian brain.[14] GHB is probably synthesized from GABA in GABAergic neurons, and released when the neurons fire.[13]
GHB induces the accumulation of either a derivative of tryptophan or tryptophan itself in the extracellular space, possibly by increasing tryptophan transport across the blood-brain barrier. The blood content of certain neutral amino-acids, including tryptophan, is also increased by peripheral GHB administration. GHB-induced stimulation of tissue serotonin turnover may be due to an increase in tryptophan transport to the brain and in its uptake by serotonergic cells. As the serotonergic system may be involved in the regulation of sleep, mood, and anxiety, the stimulation of this system by high doses of GHB may be involved in certain neuropharmacological events induced by GHB administration.
If taken orally, GABA itself does not effectively cross the blood-brain-barrier.[15] Since GABA is naturally synthesized in the brain, a higher-than-normal concentration would be quickly metabolized.[16]
However, at pharmacological doses, GHB reaches much higher concentrations in the brain and activates GABAB receptors, which are primarily responsible for its sedative effects.[17] GHB's sedative effects are blocked by GABAB antagonists.
The role of the GHB receptor in the behavioural effects induced by GHB is more complex. GHB receptors are densely expressed in many areas of the brain, including the cortex and hippocampus, and these are the receptors that GHB displays the highest affinity for. There has been somewhat limited research into the GHB receptor; however, there is evidence that activation of the GHB receptor in some brain areas results in the release of glutamate, the principal excitatory neurotransmitter.[18] Drugs that selectively activate the GHB receptor cause absence seizures in high doses, as do GHB and GABA(B) agonists.[19]
Activation of both the GHB receptor and GABA(B) is responsible for the addictive profile of GHB. GHB's effect on dopamine release is biphasic,[20] low concentrations stimulate dopamine release via the GHB receptor.[21] Higher concentrations inhibit dopamine release via GABA(B) receptors as do other GABA(B) agonists such as baclofen and phenibut.[22] After an initial phase of inhibition, dopamine release is then increased via the GHB receptor. Both the inhibition and increase of dopamine release by GHB are inhibited by opioid antagonists such as naloxone and naltrexone. Dynorphin may play a role in the inhibition of dopamine release via kappa opioid receptors.[23]
This explains the paradoxical mix of sedative and stimulatory properties of GHB, as well as the so-called "rebound" effect, experienced by individuals using GHB as a sleeping agent, wherein they awake suddenly after several hours of GHB-induced deep sleep. That is to say that, over time, the concentration of GHB in the system decreases below the threshold for significant GABAB receptor activation and activates predominantly the GHB receptor, leading to wakefulness.
Recently, analogs of GHB, such as 4-hydroxy-4-methylpentanoic acid have been synthesised and tested on animals, in order to gain a better understanding of GHB's mode of action.[24] Analogues of GHB such as 3-methyl-GHB, 4-methyl-GHB and 4-phenyl-GHB have been shown to produce similar effects to GHB in some animal studies, but these compounds are even less well researched than GHB itself. Of these analogues, only 4-methyl-GHB (γ-hydroxyvaleric acid, GHV) and its prodrug form gamma-valerolactone (GVL) have been reported as drugs of abuse in humans, and on the available evidence seem to be less potent but more toxic than GHB, with a particular tendency to cause nausea and vomiting.
Other prodrug ester forms of GHB have also rarely been encountered by law enforcement, including 1,4-diacetoxybutane, methyl-4-acetoxybutanoate, and ethyl-4-acetoxybutanoate, but these are, in general, covered by analogue laws in jurisdictions where GHB is illegal, and little is known about them beyond their delayed onset and longer duration of action. The intermediate compound 4-hydroxybutaldehyde is also a prodrug for GHB; however, as with all aldehydes this compound is caustic and is strong-smelling and foul-tasting; actual use of this compound as an intoxicant is likely to be unpleasant and result in severe nausea and vomiting.
Also note that both of the metabolic breakdown pathways shown for GHB can run in either direction, depending on the concentrations of the substances involved, so the body can make its own GHB either from GABA or from succinic semialdehyde. Under normal physiological conditions, the concentration of GHB in the body is rather low, and the pathways would run in the reverse direction to what is shown here to produce endogenous GHB. However, when GHB is consumed for recreational or health promotion purposes, its concentration in the body is much higher than normal, which changes the enzyme kinetics so that these pathways operate to metabolise GHB rather than producing it.
Medical use
GHB has been used as a general anesthetic in the 1960s,[5] as a hypnotic in the treatment of insomnia, to treat depression, and to improve athletic performance. In Italy, under the trade name Alcover (ATC code N07BB), GHB is used in the treatment of alcoholism (50 to 100 milligrams per kilogram per day, in 3 or more divided doses), both for acute alcohol withdrawal and medium- to long-term detoxification.[25]
GHB is the active ingredient in a prescription medication called Xyrem (sodium oxybate) oral solution. Xyrem is approved by the U.S. Food and Drug Administration (FDA) for the treatment of cataplexy associated with narcolepsy [26] and Excessive Daytime Sleepiness (EDS) associated with narcolepsy .[27] The American Academy of Sleep Medicine (AASM) recommends Xyrem as a standard of care for the treatment of cataplexy, daytime sleepiness, and disrupted sleep due to narcolepsy in its Practice Parameters for the Treatment of Narcolepsy and other Hypersomnias of Central Origin. These recommendations are based upon careful review of the medical literature, and the designation “standard” of care “reflects a high degree of clinical certainty” based on strong empirical evidence.[28]
In clinical trials Xyrem significantly reduced cataplexy attacks at a dose of 6-9g per night, which is generally divided between two doses. This is about a third the dose used recreationally, but almost all narcolepsy patients in the clinical trials were already stabilized on CNS stimulants such as modafinil; in patients not prescribed modafinil, this dosage could be dangerous and should be reduced appropriately. Also, the prescribing information for Xyrem states that patients should take the dose immediately before going to bed, and then a second dose 3–4 hours later. The maximum dose taken at one time should not exceed 4500 mg. Patients with hepatic insufficiency (compromised liver function) have slower clearance of GHB and require reduced doses, typically half the normal dose. Xyrem oral solution is standardised to 500 mg Na.GHB/1 mL water, buffered to pH 7.5 with malic acid.</ref>
When GHB is used in its sodium or potassium salt form, a significant quantity of excess sodium or potassium may be consumed, which should be taken into consideration by people with heart conditions, hypertension or compromised renal function. The bioavailability of sodium GHB is considerably reduced when it is consumed with food, and so it is advised to wait at least two hours after eating before consuming the dose. Because of its strong sedative effects, patients should not drive or operate heavy machinery for at least six hours after taking sodium GHB.
Adverse effects from Xyrem in clinical trials included: headache, nausea, dizziness, nasopharyngitis, somnolence, vomiting, urinary incontinence, confusion, dyspnea, hypoesthesia, paresthesia, tremor, vertigo, and blurred vision. Out of the 717 patients and 182 healthy volunteers who took part in the trials (899 total), two of them died from drug overdoses, although only one of these involved GHB.[29]
In January 2008, Jazz Pharmaceuticals completed enrollment in the second Phase III trial for a modified version of sodium oxybate, known as JZP-6, for use by people with fibromyalgia.[30][31] The company completed one of the Phase III clinical trials in September 2008.[32]
On October 11, 2010, the U.S. Food and Drug Administration denied approval of JZP-6.[33]
Non-medical use

GHB is a CNS depressant used as an intoxicant. It has many street names, including "Georgia Home Boy", "Liquid Ecstasy", "Liquid X", and "Liquid G", as well as "Fantasy" and the reordered initialism GBH. Its effects have been described anecdotally as comparable to alcohol and ecstasy use, such as euphoria, disinhibition, enhanced sensuality and empathogenesis. At higher doses, GHB may induce nausea, dizziness, drowsiness, agitation, visual disturbances, depressed breathing, amnesia, unconsciousness, and death. The effects of GHB can last from 1.5 to 3 hours, or even longer if large doses have been consumed or if it is mixed with alcohol.[34]
In general, the doses used recreationally are between 500 mg and 3,000 mg. When used as a recreational drug, GHB may be found as the sodium or potassium salt, which is a white crystalline powder, or as GHB salt dissolved in water to form a clear solution. The sodium salt of GHB has a salty taste.[34] Other salt forms such as calcium GHB and magnesium GHB have also been reported, but the sodium salt is by far the most common.
Some chemicals convert to GHB in the stomach and blood stream. GBL, or gamma-butyrolactone, is one such prodrug. Other prodrugs include 1,4-butanediol. There may be additional toxicity concerns with these precursors. 1,4-B and GBL are normally found as pure liquids, although they may be mixed with other more harmful solvents when intended for industrial use, e.g., as paint stripper or varnish thinner.
GHB can be produced in clandestine labs, and it is claimed that most of the GHB used in the U.S. is illegally manufactured within its borders. While available as a prescription for sleep disorders in some other countries, GHB was banned (in the U.S.) by the FDA in 1990. However, on 17 July 2002, GHB was approved for treatment of cataplexy, often associated with narcolepsy. GHB is "colourless and odorless".[35]
Drug
Club scene or "rave"
Since the 1970s club scene, club-goers have used a range of drugs to enhance their experience on the dance floor such as amyl nitrite "poppers" and cocaine. In the 1990s, newer "club drugs" became popular, such as ketamine and "designer" phenethylamines designed to circumvent contemporary drug laws, "ecstasy" (chemically MDMA, 3,4-methylenedioxy methamphetamine, or 3,4-methylenedioxy methyl alpha-methyl phenethylamine) and 2C-I (chemically 2,5-dimethoxy-4-iodophenethylamine) being prominent examples. When the laws "catch up" to certain drugs, clandestine chemists manufacture another drug, designed to affect the user in the same way as the now-banned drug. Since most of these drugs are congeners of the banned drugs, the Federal Analogue Act was introduced in the US to ban these substances proactively, based on the proclivity of a said chemical to mimic either the structure or the effects of the banned drug.
Like these other "club drugs," GHB is taken because users feel that it enhances the experience of being in a club or at a party; small doses of GHB are thought to act as a stimulant and aphrodisiac. GHB is sometimes referred to as liquid ecstasy, liquid X, or liquid E due to its tendency to produce euphoria and sociability and its use in the dance party scene.[36] Despite this nickname, GHB has entirely separate chemical and pharmacological modes of action compared to ecstasy.
Date rape
The drug has been identified as a date rape drug,[6] much the same way as alcohol and potent benzodiazepines, often known colloquially as "Rohypnol", the trade name of a certain potent hypnotic benzodiazepine, flunitrazepam. It has a salty taste but, as it is colourless and odorless,[35] it has been described as "very easy to add to drinks"[35] that mask the flavor. GHB has been used in cases of drug-related sexual assault, usually when the victim is vulnerable due to intoxication with a sedative, generally alcohol.[37] However it is difficult to establish how often GHB is used to facilitate rape as it is difficult to detect in a urine sample after a day, and many victims may not recall the rape until some time after this.[38][39] However cases of GHB being used as a date rape drug are quite rare, see the date rape drug article for more information.
GHB, produced as a sodium salt (sodium oxybate), may provide a noticeable salty character to the drink, although individual sensitivity to the taste of salt varies.[40] GHB can also be produced as different salts, some of which may not have a taste as distinctive as the sodium salt (e.g., magnesium oxybate), or much less commonly in the unstable free-acid form.[41]
Bodybuilding
Some athletes and bodybuilders also use GHB, as GHB has been shown to elevate human growth hormone in vivo.[42] The growth hormone elevating effects of GHB are mediated through muscarinic acetylcholine receptors and can be prevented by prior administration of pirenzepine, a muscarinic acetylcholine receptor blocking agent.[43]
As certain succinate salts have been shown to elevate growth hormone in vitro,[44] and because GHB is metabolized into succinate some people have suggested this may play a role in the growth hormone elevations from GHB. There is however currently no evidence to show that succinate plays any role in the growth hormone elevations from GHB.
Endogenous production by the body
Cells produce GHB by reduction of succinic semialdehyde via the enzyme succinic semialdehyde dehydrogenase. This enzyme appears to be induced by cAMP levels,[45] meaning substances that elevate cAMP, such as forskolin and vinpocetine, may increase GHB synthesis and release. People with the disorder known as succinic semialdehyde dehydrogenase deficiency, also known as gamma-hydroxybutyric aciduria, have elevated levels of GHB in their urine, blood plasma and cerebrospinal fluid.[46]
The precise function of GHB in the body is not clear. It is known, however, that the brain expresses a large amount of receptors that are activated by GHB.[47] These receptors are excitatory and not responsible for the sedative effects of GHB - they have been shown to elevate the principle excitatory neurotransmitter—glutamate.[18] The benzamide antipsychotics—amisulpride, sulpiride—have been shown to bind to this receptor in vivo.[48] Other antipsychotics were tested and were not found to have an affinity for this receptor.
It is a precursor to GABA, glutamate, and glycine in certain brain areas.[49]
GHB has neuroprotective properties and has been found to protect cells from hypoxia.[50]
Natural fermentation by-product
GHB is also produced as a result of fermentation and so is found in small quantities in some beers and wines, in particular fruit wines. However, the amount of GHB found in wine is insignificant and not sufficient to produce any effects.[51]
Adverse effects
Combination with alcohol
In humans, GHB has been shown to inhibit the elimination rate of alcohol. This may explain the respiratory arrest that has been reported after ingestion of both drugs.[52] A review of the details of 194 deaths attributed to or related to GHB over a ten-year period found that most were from respiratory depression caused by interaction with alcohol or other drugs.[53]
Reported deaths
One report has suggested that Xyrem (pharmaceutical GHB, or "Sodium Oxybate") overdose may be fatal, based on deaths of three patients who had been prescribed the drug.[54] However, for two of the three cases, post-mortem GHB concentrations were 141 and 110 mg/L, which is within the expected range of concentrations for GHB after death, and the third case was a patient with a history of intentional drug overdose.[55]
One publication has investigated 226 deaths attributed to GHB.[56] Of 226 deaths included, 213 suffered cardiorespiratory arrest and 13 suffered fatal accidents. Seventy-one deaths (34%) had no co-intoxicants. Postmortem blood GHB was 18–4400 mg/L (median=347) in deaths negative for co-intoxicants.
GHB is produced in the body in very small amounts, and blood levels may climb after death to levels in the range of 30–50 mg/L.[57] Levels higher than this are found in GHB deaths. Levels lower than this may be due to GHB or to postmortem endogenous elevations.
A UK parliamentary committee commissioned report found the use of GHB to be less dangerous than tobacco and alcohol in social harms, physical harm and addiction.[58]
Treatment of overdose
Template:Ref improve section Overdose of GHB can be difficult to treat because of its multiple effects on the body.[5][59][60] GHB tends to cause rapid unconsciousness at doses above 3500 mg, with single doses over 7000 mg often causing life-threatening respiratory depression, and higher doses still inducing bradycardia and cardiac arrest. Other side-effects include convulsions (especially when combined with stimulants), and nausea/vomiting (especially when combined with alcohol).
The greatest life threat due to GHB overdose (with or without other substances) is respiratory arrest.[61] Other relatively common causes of death due to GHB ingestion include aspiration of vomitus, positional asphyxia, and trauma sustained while intoxicated (e.g., motor vehicle accidents while driving under the influence of GHB).[61] The risk of aspiration pneumonia and positional asphyxia risk can be reduced by laying the patient down in the recovery position. People are most likely to vomit as they become unconscious, and as they wake up. GHB overdose is a medical emergency and assessment in an emergency department is needed.
Convulsions from GHB can be treated with diazepam or lorazepam, even though these are also CNS depressants they are GABAA agonists, whereas GHB is primarily a GABAB agonist, so the benzodiazepines do not worsen CNS depression as much as might be expected.[citation needed]
Most stimulants are not effective at counteracting the unconsciousness from GHB.[citation needed]
Because of the faster and more complete absorption of GBL relative to GHB, its dose-response curve is steeper, and overdoses of GBL tend to be more dangerous and problematic than overdoses involving only GHB or 1,4-B. Any GHB/GBL overdose is a medical emergency and should be cared for by appropriately trained personnel.
A newer synthetic drug SCH-50911, which acts as a selective GABAB antagonist, quickly reverses GHB overdose in mice.[62] However this treatment has yet to be tried in humans, and it is unlikely that it will be researched for this purpose in humans due to the illegal nature of clinical trials of GHB, and the lack of medical indemnity coverage inherent in using an untested treatment for a life-threatening overdose.OR
Detection of use
GHB may be quantitated in blood or plasma to confirm a diagnosis of poisoning in hospitalized patients, provide evidence in an impaired driving arrest or to assist in a medicolegal death investigation. Blood or plasma GHB concentrations are usually in a range of 50–250 mg/L in persons receiving the drug therapeutically (during general anesthesia), 30–100 mg/L in those arrested for impaired driving, 50–500 mg/L in acutely intoxicated patients and 100–1000 mg/L in victims of fatal overdosage. Urine is often the preferred specimen for routine drug abuse monitoring purposes. Both gamma-butyrolactone (GBL) and 1,4-butanediol are converted to GHB in the body.[63][64][65]
Neurotoxicity
In multiple studies, GHB has been found to impair spatial and working learning and memory in rats with chronic administration.[66][67][68][69] These effects are associated with decreased NMDA receptor expression in the cerebral cortex and possibly other areas as well.[66]
Pedraza et al. (2009) found that repeated administration of GHB to rats for 15 days drastically reduced the number of neurons and non-neuronal cells in the CA1 region of the hippocampus and in the prefrontal cortex. With doses of 10 mg/kg of GHB, they were decreased by 61% in the CA1 region and 32% in the prefrontal cortex, and with 100 mg/kg, they were decreased by 38% and 9%, respectively. It is interesting to note that GHB has biphasic effects on neuronal loss, with lower doses (10 mg/kg) producing the most neurotoxicity, and higher doses (100 mg/kg) producing less.
Pretreatment with NCS-382, a GHB receptor antagonist, prevents both learning/memory deficits and neuronal loss in GHB-treated animals, suggesting that GHB's neurotoxic actions are mediated via activation of the GHB receptor.[69] In addition, the neurotoxicity appears to be caused by oxidative stress.[69][70][71]
Addiction
Although there have been reported fatalities due to GHB withdrawal, reports are inconclusive and further research is needed.[72] Addiction occurs when repeated drug use disrupts the normal balance of brain circuits that control rewards, memory and cognition, ultimately leading to compulsive drug taking.[73][74]
Colombo reports that rats forced to consume massive doses of GHB will intermittently prefer GHB solution to water, but notes that "no rat showed any sign of withdrawal when GHB was finally removed at the end of the 20-week period" or during periods of voluntary abstinence.[75][76]
Withdrawal
GHB has also been associated with a withdrawal syndrome of insomnia, anxiety, and tremor that usually resolves within three to twelve days.[72] Treatment with benzodiazepines can be used, although extremely high doses may be required (e.g. > 100 mg/d of diazepam). With the exception of baclofen, other treatments are often ineffective. Evidence shows that baclofen is the most effective drug for GHB withdrawal. GHB and baclofen are agonists for the GABAb receptor.[77] Benzodiazepines do not affect GABAB receptors and thus have no cross-tolerance with GHB; baclofen which works via GABAB receptors is cross-tolerant with GHB and is effective in alleviating withdrawal effects of GHB.[78] Thus baclofen can be used to substitute for GHB and gradually titrated to reduce withdrawal severity.
GHB withdrawal is not widely discussed in text books and as a result most psychiatrists are not familiar with this withdrawal syndrome.[79]
Legal status
In the United States, it was placed on Schedule I of the Controlled Substances Act in March 2000. However, when sold as Xyrem, it is considered Schedule III, one of several drugs that are listed in multiple schedules.[3][80] On 20 March 2001, the Commission on Narcotic Drugs placed GHB in Schedule IV of the 1971 Convention on Psychotropic Substances.[81] In the UK it was made a class C drug in June 2003.
In Hong Kong, GHB is regulated under Schedule 1 of Hong Kong's Chapter 134 Dangerous Drugs Ordinance. It can only be used legally by health professionals and for university research purposes. The substance can be given by pharmacists under a prescription. Anyone who supplies the substance without prescription can be fined HK$10000. The penalty for trafficking or manufacturing the substance is a HK$5,000,000 fine and life imprisonment. Possession of the substance for consumption without license from the Department of Health is illegal with a HK$1,000,000 fine and/or 7 years of jail time.
In New Zealand and Australia, GHB, 1,4-B and GBL are all Class B illegal drugs, along with any possible esters, ethers and aldehydes. GABA itself is also listed as an illegal drug in these jurisdictions, which seems unusual given its failure to cross the blood-brain barrier, but there was a perception among legislators that all known analogues should be covered as far as this was possible. Attempts to circumvent the illegal status of GHB have led to the sale of derivatives such as 4-methyl-GHB (gamma-hydroxyvaleric acid, GHV) and its prodrug form gamma-valerolactone (GVL), but these are also covered under the law by virtue of their being "substantially similar" to GHB or GBL and; so importation, sale, possession and use of these compounds is also considered to be illegal.
In Norway[82] and in Switzerland,[83] GHB is considered a narcotic and is only available by prescription under the trade name Xyrem (Union Chimique Belge S.A.).
See also
- 1,4-Butanediol (1,4-BD)
- gamma-Butyrolactone (GBL)
- gamma-Hydroxyvaleric acid (GHV)
- gamma-Valerolactone (GVL)
References
- ↑ "Sodium Oxybate: MedlinePlus Drug Information". Nlm.nih.gov. 2010-07-28. Retrieved 2010-08-01.
- ↑ Weil, Andrew (1993). "Depressants". From Chocolate to Morphine (2nd ed.). Boston/New York: Houghton Mifflin Company. p. 77. ISBN 0-395-66079-3. Unknown parameter
|coauthors=ignored (help) - ↑ 3.0 3.1 Erowid GHB Vault : Legal Status.
- ↑ http://stocks.us.reuters.com/stocks/fullDescription.asp?rpc=66&symbol=JAZZ.O. Missing or empty
|title=(help) - ↑ 5.0 5.1 5.2 Theodore I Benzer (8 January 2007). "Toxicity, Gamma-Hydroxybutyrate". eMedicine.
- ↑ 6.0 6.1 GHB, GBL and 1,4BD as Date Rape Drugs.
- ↑ e.g., sodium gamma-hydroxybutyrate (Na.GHB, sodium oxybate) or potassium gamma-hydroxybutyrate (K.GHB).
- ↑ Alexander Saytzeff (1874). "Über die Reduction des Succinylchlorids". Liebigs Annalen der Chemie (in German). 171: 258–290. doi:10.1002/jlac.18741710216.
- ↑ H. Laborit, J.M. Jouany, J. Gerald, F. Fabiani (1960). "Generalities concernant l'etude experimentale de l'emploi clinique du gamma hydroxybutyrate de Na". Aggressologie (in French). 1: 407. PMID 13758011.
- ↑ Michael Perry, James Pomfret, Roger Crabb (7 November 2007). "Australia bans China-made toy on toxic drug risk". Reuter.
- ↑ Wu Y, Ali S, Ahmadian G; et al. (2004). "Gamma-hydroxybutyric acid (GHB) and gamma-aminobutyric acidB receptor (GABABR) binding sites are distinctive from one another: molecular evidence". Neuropharmacology. 47 (8): 1146–56. doi:10.1016/j.neuropharm.2004.08.019. PMID 15567424. Unknown parameter
|month=ignored (help) - ↑ Cash, C (1999). "γ-hydroxybutyrate receptor function studied by the modulation of nitric oxide synthase activity in rat frontal cortex punches". Biochemical Pharmacology. 58: 1815. doi:10.1016/S0006-2952(99)00265-8.
- ↑ 13.0 13.1 13.2 Maitre M, Humbert JP, Kemmel V, Aunis D, Andriamampandry C (2005). "[A mechanism for gamma-hydroxybutyrate (GHB) as a drug and a substance of abuse]". Med Sci (Paris) (in French). 21 (3): 284–9. PMID 15745703. Unknown parameter
|month=ignored (help) - ↑ Waszkielewicz A, Bojarski J (2004). "Gamma-hydrobutyric acid (GHB) and its chemical modifications: a review of the GHBergic system" (PDF). Pol J Pharmacol. 56 (1): 43–9. PMID 15047976.
- ↑ Kuriyama K, Sze PY (1971). "Blood-brain barrier to H3-gamma-aminobutyric acid in normal and amino oxyacetic acid-treated animals". Neuropharmacology. 10 (1): 103–8. doi:10.1016/0028-3908(71)90013-X. PMID 5569303. Unknown parameter
|month=ignored (help) - ↑ OTC GABA and the Blood-Brain Barrier.
- ↑ Dimitrijevic N, Dzitoyeva S, Satta R, Imbesi M, Yildiz S, Manev H (2005). "Drosophila GABA(B) receptors are involved in behavioral effects of gamma-hydroxybutyric acid (GHB)". Eur. J. Pharmacol. 519 (3): 246–52. doi:10.1016/j.ejphar.2005.07.016. PMID 16129424. Unknown parameter
|month=ignored (help) - ↑ 18.0 18.1 Castelli MP, Ferraro L, Mocci I; et al. (2003). "Selective gamma-hydroxybutyric acid receptor ligands increase extracellular glutamate in the hippocampus, but fail to activate G protein and to produce the sedative/hypnotic effect of gamma-hydroxybutyric acid". J. Neurochem. 87 (3): 722–32. doi:10.1046/j.1471-4159.2003.02037.x. PMID 14535954. Unknown parameter
|month=ignored (help) - ↑ Banerjee PK, Snead OC (1995). "Presynaptic gamma-hydroxybutyric acid (GHB) and gamma-aminobutyric acidB (GABAB) receptor-mediated release of GABA and glutamate (GLU) in rat thalamic ventrobasal nucleus (VB): a possible mechanism for the generation of absence-like seizures induced by GHB". J. Pharmacol. Exp. Ther. 273 (3): 1534–43. PMID 7791129. Unknown parameter
|month=ignored (help) - ↑ Hechler V, Gobaille S, Bourguignon JJ, Maitre M (1991). "Extracellular events induced by gamma-hydroxybutyrate in striatum: a microdialysis study". J. Neurochem. 56 (3): 938–44. doi:10.1111/j.1471-4159.1991.tb02012.x. PMID 1847191. Unknown parameter
|month=ignored (help) - ↑ Maitre M, Hechler V, Vayer P; et al. (1990). "A specific gamma-hydroxybutyrate receptor ligand possesses both antagonistic and anticonvulsant properties". J. Pharmacol. Exp. Ther. 255 (2): 657–63. PMID 2173754. Unknown parameter
|month=ignored (help) - ↑ Smolders I, De Klippel N, Sarre S, Ebinger G, Michotte Y (1995). "Tonic GABA-ergic modulation of striatal dopamine release studied by in vivo microdialysis in the freely moving rat". Eur. J. Pharmacol. 284 (1–2): 83–91. doi:10.1016/0014-2999(95)00369-V. PMID 8549640. Unknown parameter
|month=ignored (help) - ↑ Mamelak M (1989). "Gammahydroxybutyrate: an endogenous regulator of energy metabolism". Neurosci Biobehav Rev. 13 (4): 187–98. doi:10.1016/S0149-7634(89)80053-3. PMID 2691926.
- ↑ Wu, H.; Zink, N; Carter, LP; Mehta, AK; Hernandez, RJ; Ticku, MK; Lamb, R; France, CP; Coop, A (2003). "A Tertiary Alcohol Analog of gamma-Hydroxybutyric Acid as a Specific gamma -Hydroxybutyric Acid Receptor Ligand". Journal of Pharmacology and Experimental Therapeutics. 305 (2): 675. doi:10.1124/jpet.102.046797. PMID 12606613.
- ↑ An author/scientist Gian Luigi Gessa has been researching alcoholism and the effects of various drugs to persons afflicted with said disease for the past ten years. His studies in 1998 note that GHB, as a pharmaceutical aid, can be much less toxic and much more effective than the leading pharmaceutical compound (disulfiram).
- ↑ "FDA Approval Letter for Xyrem; Indication: Cataplexy associated with narcolepsy; 17 July 2002" (PDF).
- ↑ "FDA Approval Letter for Xyrem; Indication: EDS (Excessive Daytime Sleepiness) associated with narcolepsy; 18 November 2005" (PDF).
- ↑ "Practice Parameters for the Treatment of Narcolepsy and other Hypersomnias of Central Origin (Morgenthaler et al. Sleep. 2007;30:1705)" (PDF).
- ↑ Xyrem drug data sheet.
- ↑ "Reuters.com". Reuters.com. Retrieved 2010-08-01.
- ↑ "JazzPharma - Investors - News Release". Investor.jazzpharma.com. Retrieved 2010-08-01.
- ↑ "65-center trial of sodium oxybate for fibromyalgia pain completed; second phase III trial still recruiting in US and UK". Prohealth.com. 2008-09-11. Retrieved 2010-08-01.
- ↑ The Associated Press (2010-10-12). "FDA Says No to Jazz Pharma Fibromyalgia Drug". The New York Times. Retrieved 2010-10-12.
- ↑ 34.0 34.1 Galloway GP, Frederick-Osborne SL, Seymour R, Contini SE, Smith DE (2000). "Abuse and therapeutic potential of gamma-hydroxybutyric acid". Alcohol. 20 (3): 263–9. doi:10.1016/S0741-8329(99)00090-7. PMID 10869868. Unknown parameter
|month=ignored (help) - ↑ 35.0 35.1 35.2 Jones, C. (2001). "Suspicious death related to gamma-hydroxybutyrate (GHB) toxicity (2001)". Journal of Clinical Forensic Medicine. 8 (2): 74. doi:10.1054/jcfm.2001.0473. PMID 15274975.
- ↑ Mary Klein, Frances Kramer, "Rave drugs: Pharmacological considerations", AANA Journal, Vol. 72 (2004), 61–67.
- ↑ ElSohly MA, Salamone SJ (1999). "Prevalence of drugs used in cases of alleged sexual assault". J Anal Toxicol. 23 (3): 141–6. PMID 10369321.
- ↑ S.O.S. - Date Rape Drugs.
- ↑ "Labs making date-rape drug raided", The Independent World, 10 July 2008.
- ↑ Pangborn RM, Pecore SD (1982). "Taste perception of sodium chloride in relation to dietary intake of salt". Am. J. Clin. Nutr. 35 (3): 510–20. PMID 7064902. Unknown parameter
|month=ignored (help) - ↑ Witkowski, Mark R.; Ciolino, Laura A.; De Francesco, James V. (2006). "GHB Free Acid: II. Isolation and Spectroscopic Characterization for Forensic Analysis". Journal of Forensic Sciences. 51 (2): 330. doi:10.1111/j.1556-4029.2006.00074.x. PMID 16566766.
- ↑ Riccardo Volpi, Paolo Chiodera, Paolo Caffarra, Augusto Scaglioni, Antonella Saccani and Vittorio Coiro (1997). "Different control mechanisms of growth hormone (GH) secretion between γ-amino- and γ-hydroxy-butyric acid: neuroendocrine evidence in parkinson's disease". Psychoneuroendocrinology. 22 (7): 531–538. doi:10.1016/S0306-4530(97)00055-3.
- ↑ Volpi, R (2000). "Muscarinic cholinergic mediation of the GH response to gamma-hydroxybutyric acid: neuroendocrine evidence in normal and parkinsonian subjects". Psychoneuroendocrinology. 25: 179. doi:10.1016/S0306-4530(99)00048-7.
- ↑ Badamchian, M; Spangelos, B; Hagiwara, Y; Hagiwara, H; Ueyama, H; Goldstein, A (1995). "Alpha-Tocopherol Succinate, But Not Alpha-Tocopherol Or Other Vitamin E Analogs Stimulates Prolactin And Growth Hormone Release From Rat Anterior Pituitary Cells in vitro". The Journal of Nutritional Biochemistry. 6: 340. doi:10.1016/0955-2863(95)00044-Z.
- ↑ Kemmel V, Taleb O, Perard A; et al. (1998). "Neurochemical and electrophysiological evidence for the existence of a functional gamma-hydroxybutyrate system in NCB-20 neurons". Neuroscience. 86 (3): 989–1000. doi:10.1016/S0306-4522(98)00085-2. PMID 9692734. Unknown parameter
|month=ignored (help) - ↑ National Organization for Rare Disorders. Succinic Semialdehyde Dehydrogenase Deficiency. Retrieved 6 March 2010.
- ↑ C. Andriamampandry, O. Taleb, S. Viry, C. Muller, J. P. Humbert, S. Gobaille, D. Aunis and M. Maitre (2003). "Cloning and characterization of a rat brain receptor that binds the endogenous neuromodulator γ-hydroxybutyrate". The FASEB Journal. 17 (12): 1691–3. doi:10.1096/fj.02-0846fje. PMID 12958178.
- ↑ Maitre M, Ratomponirina C, Gobaille S, Hodé Y, Hechler V (1994). "Displacement of [3H] gamma-hydroxybutyrate binding by benzamide neuroleptics and prochlorperazine but not by other antipsychotics". Eur. J. Pharmacol. 256 (2): 211–4. doi:10.1016/0014-2999(94)90248-8. PMID 7914168. Unknown parameter
|month=ignored (help) - ↑ Gobaille S, Hechler V, Andriamampandry C, Kemmel V, Maitre M (1999). "gamma-Hydroxybutyrate modulates synthesis and extracellular concentration of gamma-aminobutyric acid in discrete rat brain regions in vivo". J. Pharmacol. Exp. Ther. 290 (1): 303–9. PMID 10381791. Unknown parameter
|month=ignored (help) - ↑ Ottani A, Saltini S, Bartiromo M; et al. (2003). "Effect of gamma-hydroxybutyrate in two rat models of focal cerebral damage". Brain Res. 986 (1–2): 181–90. doi:10.1016/S0006-8993(03)03252-9. PMID 12965243. Unknown parameter
|month=ignored (help) - ↑ Elliott S, Burgess V. "The presence of gamma-hydroxybutyric acid (GHB) and gamma-butyrolactone (GBL) in alcoholic and non-alcoholic beverages". Forensic Science International. 2005 July 16;151(2–3):289–92.
- ↑ Poldrugo F, Addolorato G (1999). "The role of gamma-hydroxybutyric acid in the treatment of alcoholism: from animal to clinical studies". Alcohol Alcohol. 34 (1): 15–24. PMID 10075397.
- ↑ Zvosec et al. American Academy of Forensic Science in Seattle, 2006
- ↑ PMID 19269893 (PMID 19269893)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ Feldman NT (2009). "Xyrem safety: the debate continues". Sleep Med. 10 (4): 405–6. doi:10.1016/j.sleep.2009.02.002. PMID 19332385. Unknown parameter
|month=ignored (help) - ↑ Zvosec DL, Smith SW, Porrata T, Strobl AQ, Dyer JE. Case series of 226 gamma-hydroxybutyrate-associated deaths: lethal toxicity and trauma. Am J Emerg Med In Press.
- ↑ PMID 19959395 (PMID 19959395)
Citation will be completed automatically in a few minutes. Jump the queue or expand by hand - ↑ "Microsoft Word - HC1031.doc" (PDF). BBC News. Retrieved 2010-08-01.
- ↑ Allen, L. (1 April 2006). "Gammahydroxybutyrate overdose and physostigmine". Emergency Medicine Journal. 23 (4): 300. doi:10.1136/emj.2006.035139. PMC 2579509. PMID 16549578. Unknown parameter
|coauthors=ignored (help) - ↑ Michael, H. (1 January 2005). "Endotracheal intubation in γ-hydroxybutyric acid intoxication and overdose". Emergency Medicine Journal. 22 (1): 43. doi:10.1136/emj.2004.021154. PMC 1726538. PMID 15611542. Unknown parameter
|coauthors=ignored (help) - ↑ 61.0 61.1 Zvosec, DL, Smith, SW, Porrata, T, et al. Preventable deaths from Gamma hydroxybutyrate ingestion (Abstract). Ann Emerg Med 2006; 48:S75
- ↑ Carai, M.A.M. (2005). "Resuscitative Effect of a γ-Aminobutyric Acid B Receptor Antagonist on γ-Hydroxybutyric Acid Mortality in Mice". Annals of Emergency Medicine. 45 (6): 614–619. doi:10.1016/j.annemergmed.2004.12.013. PMID 15940094. Unknown parameter
|coauthors=ignored (help) - ↑ Couper FJ, Thatcher JE, Logan BK. Suspected GHB overdoses in the emergency department. J. Anal. Toxicol. 28: 481-484, 2004.
- ↑ Marinetti LJ, Isenschmid DS, Hepler BR, Kanluen S. Analysis of GHB and 4-methyl-GHB in postmortem matrices after long-term storage. J. Anal. Toxicol. 29: 41-47, 2005.
- ↑ R. Baselt, Disposition of Toxic Drugs and Chemicals in Man, 8th edition, Biomedical Publications, Foster City, CA, 2008, pp. 680-684.
- ↑ 66.0 66.1 Sircar R, Basak A (2004). "Adolescent gamma-hydroxybutyric acid exposure decreases cortical N-methyl-D-aspartate receptor and impairs spatial learning". Pharmacology, Biochemistry, and Behavior. 79 (4): 701–8. doi:10.1016/j.pbb.2004.09.022. PMID 15582677. Unknown parameter
|month=ignored (help) - ↑ García FB, Pedraza C, Arias JL, Navarro JF (2006). "[Effects of subchronic administration of gammahydroxybutyrate (GHB) on spatial working memory in rats]". Psicothema (in Spanish; Castilian). 18 (3): 519–24. PMID 17296081. Unknown parameter
|month=ignored (help) - ↑ Sircar R, Basak A, Sircar D (2008). "Gamma-hydroxybutyric acid-induced cognitive deficits in the female adolescent rat". Annals of the New York Academy of Sciences. 1139: 386–9. doi:10.1196/annals.1432.044. PMID 18991885. Unknown parameter
|month=ignored (help) - ↑ 69.0 69.1 69.2 Pedraza C, García FB, Navarro JF (2009). "Neurotoxic effects induced by gammahydroxybutyric acid (GHB) in male rats". The International Journal of Neuropsychopharmacology / Official Scientific Journal of the Collegium Internationale Neuropsychopharmacologicum (CINP). 12 (9): 1165–77. doi:10.1017/S1461145709000157. PMID 19288974. Unknown parameter
|month=ignored (help) - ↑ Sgaravatti AM, Sgarbi MB, Testa CG; et al. (2007). "Gamma-hydroxybutyric acid induces oxidative stress in cerebral cortex of young rats". Neurochemistry International. 50 (3): 564–70. doi:10.1016/j.neuint.2006.11.007. PMID 17197055. Unknown parameter
|month=ignored (help) - ↑ Sgaravatti AM, Magnusson AS, Oliveira AS; et al. (2009). "Effects of 1,4-butanediol administration on oxidative stress in rat brain: study of the neurotoxicity of gamma-hydroxybutyric acid in vivo". Metabolic Brain Disease. 24 (2): 271–82. doi:10.1007/s11011-009-9136-7. ISBN 1101100991367 Check
|isbn=value: invalid prefix (help). PMID 19296210. Unknown parameter|month=ignored (help) - ↑ 72.0 72.1 Galloway GP, Frederick SL, Staggers FE, Gonzales M, Stalcup SA, Smith DE. Gamma-hydroxybutyrate: an emerging drug of abuse that causes physical dependence. Addiction. 1997;92(1):89-96.
- ↑ Department of Health and Human Services, SAMHSA Office of Applied Studies 2005 National Survey on Drug Use and Health (ages 12 years and up); American Heart Association; Johns Hopkins University study, Principles of Addiction Medicine; Psychology Today; National Gambling Impact Commission Study; National Council on Problem Gambling; Illinois Institute for Addiction Recovery; Society for Advancement of Sexual Health; All Psych Journal
- ↑
- ↑ Colombo, Giancarlo; Agabio, Roberta. "Oral self-administration of gamma-hydroxybutyric acid in the rat". European Journal of Pharmacology. 1995. 285(1). 103-107. RT 120 E 4.
- ↑ <Is GHB toxic? Addictive? Dangerous?=http://www.lycaeum.org/~ghbfaq/dangerous.html>
- ↑ Letourneau JL, (12 February 2008). "Baclofen and Gamma-Hydroxybutyrate Withdrawal". Neurocrit Care. Humana Press Inc. 8 (3): 430. doi:10.1007/s12028-008-9062-2. PMC 2630388. PMID 18266111. Unknown parameter
|coauthors=ignored (help) - ↑ Carter, LP.; Koek, W.; France, CP. (2009). "Behavioral analyses of GHB: receptor mechanisms" (PDF). Pharmacol Ther. 121 (1): 100–14. doi:10.1016/j.pharmthera.2008.10.003. PMID 19010351. Unknown parameter
|month=ignored (help) - ↑ van Noorden, MS.; van Dongen, LC.; Zitman, FG.; Vergouwen, TA. (2009). "Gamma-hydroxybutyrate withdrawal syndrome: dangerous but not well-known". Gen Hosp Psychiatry. 31 (4): 394–6. doi:10.1016/j.genhosppsych.2008.11.001. PMID 19555805.
- ↑ ProjectGHB.org[dead link]
- ↑ Whitehousedrugpolicy.org.
- ↑ "FOR 30 June 1978 nr 08: Forskrift om narkotika m.v. (Narkotikalisten)".
- ↑ "Xyrem untersteht dem Bundesgesetz über die Betäubungsmittel und die psychotropen Stoffe".
External links
- The Cognitive Enhancement Research Institute - Research findings on GHB and other substances
- EMCDDA Report on the risk assessment of GHB in the framework of the joint action on new synthetic drugs
- Erowid GHB Vault (also contains information about addiction and dangers)
- InfoFacts - Rohypnol and GHB (National Institute on Drug Abuse)
- Pubmed/Medline search on sodium oxybate and alcohol-related disorders
Template:Drug use Template:Depressants Template:Sedatives
Template:Link GA ca:Èxtasi líquid cs:GHB da:GHB de:4-Hydroxybutansäure eu:GHB fa:گاما-هیدروکسیبوتیریک اسید ko:감마 하이드록시뷰티린산 is:Smjörsýra it:Gamma-idrossibutirrato he:GHB lv:Oksisviestskābe lt:GHB hu:GHB ms:GHB nl:4-hydroxybutaanzuur no:GHB nn:GHB simple:Gamma-Hydroxybutyric acid sl:Gama-hidroksibutirat sr:GHB fi:Gammahydroksivoihappo sv:GHB
- Pages with script errors
- Pages with reference errors
- Pages with citations using unsupported parameters
- Pages with citations lacking titles
- Pages with citations having bare URLs
- CS1 maint: Unrecognized language
- CS1 maint: Multiple names: authors list
- CS1 maint: Explicit use of et al.
- Pages with incomplete PMID references
- CS1 errors: ISBN
- All articles with dead external links
- Articles with dead external links from August 2010
- Articles with invalid date parameter in template
- Pages with broken file links
- Drugs with non-standard legal status
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Articles without KEGG source
- Articles without InChI source
- All articles with unsourced statements
- Articles with unsourced statements from June 2010
- Articles with unsourced statements from March 2010
- Articles with unsourced statements from August 2008
- Use dmy dates from August 2010
- Sedatives
- General anesthetics
- Hydroxy acids
- Neurotransmitters
- Drug culture
- Euphoriants