Cannabinoid receptor: Difference between revisions
Adeeljamil (talk | contribs) No edit summary |
m (Bot: Automated text replacement (-{{SIB}} + & -{{EH}} + & -{{EJ}} + & -{{Editor Help}} + & -{{Editor Join}} +)) |
||
| Line 41: | Line 41: | ||
{{SI}} | {{SI}} | ||
The '''cannabinoid receptors''' are a class of [[Receptor (biochemistry)|receptor]]s under the [[G-protein coupled receptor]] superfamily. Their [[ligand (biochemistry)|ligand]]s are known as [[cannabinoids]]. | The '''cannabinoid receptors''' are a class of [[Receptor (biochemistry)|receptor]]s under the [[G-protein coupled receptor]] superfamily. Their [[ligand (biochemistry)|ligand]]s are known as [[cannabinoids]]. | ||
| Line 107: | Line 107: | ||
[[Category:G protein coupled receptors]] | [[Category:G protein coupled receptors]] | ||
[[de:Cannabinoid-Rezeptor]] | [[de:Cannabinoid-Rezeptor]] | ||
[[it:Recettori cannabinoidi]] | [[it:Recettori cannabinoidi]] | ||
Revision as of 23:24, 8 August 2012
| cannabinoid receptor 1 (brain) | |
|---|---|
| Identifiers | |
| Symbol | CNR1 |
| Alt. symbols | CNR |
| Entrez | 1268 |
| HUGO | 2159 |
| OMIM | 114610 |
| RefSeq | NM_033181 |
| UniProt | P21554 |
| Other data | |
| Locus | Chr. 6 q14-q15 |
| cannabinoid receptor 2 (macrophage) | |
|---|---|
| Identifiers | |
| Symbol | CNR2 |
| Entrez | 1269 |
| HUGO | 2160 |
| OMIM | 605051 |
| RefSeq | NM_001841 |
| UniProt | P34972 |
| Other data | |
| Locus | Chr. 1 p |
The cannabinoid receptors are a class of receptors under the G-protein coupled receptor superfamily. Their ligands are known as cannabinoids.
Classification
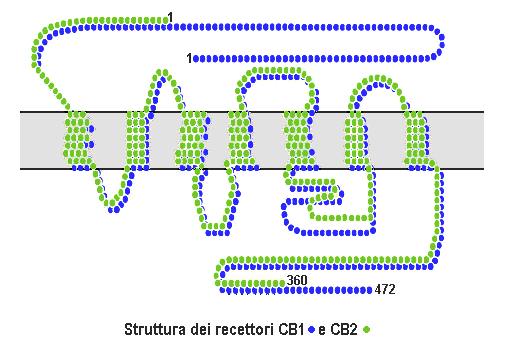
There are currently two known subtypes, CB1[1][2] which is expressed mainly in the brain, but also in the lungs, liver and kidneys and CB2 which is mainly expressed in the immune system and in hematopoietic cells. Mounting evidence suggests that there are novel cannabinoid receptors[3] that is, non-CB1 and non-CB2, which are expressed in endothelial cells and in the CNS. In 2007, the binding of several cannabinoids to a GPCR in the brain was described.[4]
The protein sequences of CB1 and CB2 receptors are about 45% similar. In addition, minor variations in each receptor have been identified. Cannabinoids bind reversibly and stereo-selectively to the cannabinoid receptors. The affinity of an individual cannabinoid to each receptor determines the effect of that cannabinoid. Cannabinoids that bind more selectively to certain receptors are more desirable for medical usage.
Expression
CB1
CB1 receptors are thought to be the most widely expressed G-protein coupled receptors in the brain. This is due to endocannabinoid-mediated depolarization-induced suppression of inhibition, a very common form of short-term plasticity in which the depolarization of a single neuron induces a reduction in GABA-mediated neurotransmission. Endocannabinoids released from the depolarized neuron bind to CB1 receptors in the pre-synaptic neuron and cause a reduction in GABA release. Varying levels of CB1 expression can be detected in the olfactory bulb, cortical regions (neocortex, pyriform cortex, hippocampus, and amygdala), several parts of basal ganglia, thalamic and hypothalamic nuclei and other subcortical regions (e.g. the septal region), cerebellar cortex, and brainstem nuclei (e.g. the periaqueductal gray).[5]
CB1 is expressed on several cell types of the pituitary gland, in the thyroid gland, and most likely in the adrenal gland.[5] CB1 is also expressed in several cells relating to metabolism, such as fat cells, muscle cells, liver cells (and also in the endothelial cells, Kupffer cells and stellate cells of the liver), and in the digestive tract.[5] It is also expressed in the lungs and the kidney. In the liver, activation of the CB1 receptor is known to increase de novo lipogenesis,[6] Activation of presynaptic CB1 receptors is also known to inhibit sympathetic innervation of blood vessels and contributes to the suppression of the neurogenic vasopressor response in septic shock.[7]
CB1 is present on Leydig cells and human sperms. In females, it is present in the ovaries, oviducts myometrium, decidua and placenta. It is probably important also for the embryo.[5]
Neuroimaging
The inverse agonist MK-9470 makes it possible to produce in vivo images of the distribution of CB1 receptors in the human brain with positron emission tomography.[8]
CB2
CB2 receptors are mainly expressed on T cells of the immune system, on macrophages and B cells, and in hematopoietic cells. They also have a function in keratinocytes, and are expressed on mouse pre-implantation embryos. It is also expressed on peripheral nerve terminals.In the brain, they are mainly expressed by microglial cells, where their role remains unclear.
Signaling
Cannabinoid receptors are activated by cannabinoids, generated naturally inside the body (endocannabinoids) or introduced into the body as cannabis or a related synthetic compound.
After the receptor is engaged, multiple intracellular signal transduction pathways are activated. At first, it was thought that cannabinoid receptors mainly inhibited the enzyme adenylate cyclase (and thereby the production of the second messenger molecule cyclic AMP), and positively influenced inwardly rectifying potassium channels (=Kir or IRK).[9] However, a much more complex picture has appeared in different cell types, implicating other potassium ion channels, calcium channels, protein kinase A and C, Raf-1, ERK, JNK, p38, c-fos, c-jun and many more[5]
Separation between the therapeutically undesirable psychotropic effects, and the clinically desirable ones however, has not been reported with agonists that bind to cannabinoid receptors. THC, as well as the two major endogenous compounds identified so far that bind to the cannabinoid receptors —anandamide and 2-arachidonylglycerol (2-AG)— produce most of their effects by binding to both the CB1 and CB2 cannabinoid receptors. While the effects mediated by CB1, mostly in the CNS, have been thoroughly investigated, those mediated by CB2 are not equally well defined.
Physiology
Gastrointestinal activity
Inhibition of gastrointestinal activity has been observed after administration of Δ9-THC, or of anandamide. This effect has been assumed to be CB1-mediated since the specific CB1 antagonist SR 141716A (Rimonabant) blocks the effect. Another report, however, suggests that inhibition of intestinal motility may also have a CB2-mediated component.[10]
Cardiovascular activity
Cannabinoids are well known for their cardiovascular activity. Activation of peripheral CB1 receptors contributes to hemorrhagic and endotoxin-induced hypotension. Anandamide and 2-AG, produced by macrophages and platelets respectively, may mediate this effect.
The hypotension in hemorrhaged rats was prevented by the CB1 antagonist SR 141716A. Recently the same group found that anandamide-induced mesenteric vasodilation is mediated by an endothelially located SR 141716A-sensitive "anandamide receptor," distinct from the CB1 cannabinoid receptor, and that activation of such a receptor by an endocannabinoid, possibly anandamide, contributes to endotoxin-induced mesenteric vasodilation in vivo. The highly potent synthetic cannabinoid HU-210, as well as 2-AG, had no mesenteric vasodilator activity. Furthermore it was shown that mesenteric vasodilation by anandamide apparently has 2 components, one mediated by a SR 141716-sensitive non-CB1 receptor (located on the endothelium) and the other by an SR 141716A-resistant direct action on vascular smooth muscle.
The production of 2-AG is enhanced in normal, but not in endothelium-denuded rat aorta on stimulation with Carbachol, an acetylcholine receptor agonist. 2-AG potently reduces blood pressure in rats and may represent an endothelium-derived hypotensive factor.
Pain
Anandamide attenuates the early phase or the late phase of pain behavior produced by formalin-induced chemical damage. This effect is produced by interaction with CB1 (or CB1-like) receptors, located on peripheral endings of sensory neurons involved in pain transmission. Palmitylethanolamide, which like anandamide is present in the skin, also exhibits peripheral antinociceptive activity during the late phase of pain behavior. Palmitylethanolamide, however does not bind to either CB1 or CB2. Its analgetic activity is blocked by the specific CB2 antagonist SR 144528, though not by the specific CB1 antagonist SR 141716A. Hence a CB2-like receptor was postulated.
Cannabinoid treatments
Cannabis sativa preparations have been known as therapeutic agents against various diseases for millennia.[11] The native active constituent, Δ9-tetrahydrocannabinol (Δ9-THC) was found to be the principal mediator of the effects of cannabis.[12] Synthetic Δ9-THC is prescribed today under the generic name Dronabinol, to treat vomiting and for enhancement of appetite, mainly in AIDS patients. U.S. Pat. No. 5,434,295 discloses a family of novel 4-phenyl pinene derivatives, and teaches how to use those compounds in pharmaceutical compositions useful for treating various pathological conditions associated with damage to the central nervous system. U.S. Pat. No. 4,282,248 discloses additional pinene derivatives. These patents do not mention that any of the disclosed compounds are selective for peripheral cannabinoid receptors.
Several synthetic cannabinoids have been shown to bind to the CB2 receptor with a higher affinity than to the CB1 receptor. Most of these compounds exhibit only modest selectivity. One of the described compounds, a classical THC-type cannabinoid, L-759,656, in which the phenolic group is blocked as a methyl ether, has a CB1/CB2 binding ratio > 1000. The pharmacology of those known agonists has yet to be described.
Certain tumors, especially gliomas, express CB2 receptors. Guzman and coworkers have shown that Δ9-tetrahydrocannabinol and WIN-55,212-2, two non-selective cannabinoid agonists, induce the regression or eradication of malignant brain tumors in rats and mice.[13] CB2 selective agonists are effective in the treatment of pain, various inflammatory diseases in different animal models,[14]
[15] osteoporosis[15] and atherosclerosis.[16] CB1 selective antagonists are used for weight reduction and smoking cessation (see Rimonabant). Activation of CB1 provides neuroprotection after brain injury.[17]
References
- ↑ Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI (1990). "Structure of a cannabinoid receptor and functional expression of the cloned cDNA". Nature. 346 (6284): 561–4. doi:10.1038/346561a0. PMID 2165569.
- ↑ Gérard CM, Mollereau C, Vassart G, Parmentier M (1991). "Molecular cloning of a human cannabinoid receptor which is also expressed in testis". Biochem. J. 279 ( Pt 1): 129–34. PMID 1718258.
- ↑ Begg M, Pacher P, Bátkai S, Osei-Hyiaman D, Offertáler L, Mo FM, Liu J, Kunos G (2005). "Evidence for novel cannabinoid receptors". Pharmacol. Ther. 106 (2): 133–45. doi:10.1016/j.pharmthera.2004.11.005. PMID 15866316.
- ↑ Ryberg E, Larsson N, Sjögren S, Hjorth S, Hermansson NO, Leonova J, Elebring T, Nilsson K, Drmota T, Greasley PJ (2007). "The orphan receptor GPR55 is a novel cannabinoid receptor". Br. J. Pharmacol. 152 (7): 1092–101. doi:10.1038/sj.bjp.0707460. PMID 17876302.
- ↑ 5.0 5.1 5.2 5.3 5.4 Pagotto U, Marsicano G, Cota D, Lutz B, Pasquali R (2006). "The emerging role of the endocannabinoid system in endocrine regulation and energy balance". Endocr. Rev. 27 (1): 73–100. doi:10.1210/er.2005-0009. PMID 16306385.
- ↑ Osei-Hyiaman D, DePetrillo M, Pacher P, Liu J, Radaeva S, Bátkai S, Harvey-White J, Mackie K, Offertáler L, Wang L, Kunos G (2005). "Endocannabinoid activation at hepatic CB1 receptors stimulates fatty acid synthesis and contributes to diet-induced obesity". J. Clin. Invest. 115 (5): 1298–305. doi:10.1172/JCI200523057. PMID 15864349.
- ↑ Godlewski G, Malinowska B, Schlicker E (2004). "Presynaptic cannabinoid CB1 receptors are involved in the inhibition of the neurogenic vasopressor response during septic shock in pithed rats". Br. J. Pharmacol. 142 (4): 701–8. doi:10.1038/sj.bjp.0705839. PMID 15159284.
- ↑ Burns HD, Van Laere K, Sanabria-Bohórquez S, Hamill TG, Bormans G, Eng WS, Gibson R, Ryan C, Connolly B, Patel S, Krause S, Vanko A, Van Hecken A, Dupont P, De Lepeleire I, Rothenberg P, Stoch SA, Cote J, Hagmann WK, Jewell JP, Lin LS, Liu P, Goulet MT, Gottesdiener K, Wagner JA, de Hoon J, Mortelmans L, Fong TM, Hargreaves RJ (2007). "[18F]MK-9470, a positron emission tomography (PET) tracer for in vivo human PET brain imaging of the cannabinoid-1 receptor". Proc. Natl. Acad. Sci. U.S.A. 104 (23): 9800–5. doi:10.1073/pnas.0703472104. PMID 17535893.
- ↑ Demuth DG, Molleman A (2006). "Cannabinoid signalling". Life Sci. 78 (6): 549–63. doi:10.1016/j.lfs.2005.05.055. PMID 16109430.
- ↑ Mathison R, Ho W, Pittman QJ, Davison JS, Sharkey KA (2004). "Effects of cannabinoid receptor-2 activation on accelerated gastrointestinal transit in lipopolysaccharide-treated rats". Br. J. Pharmacol. 142 (8): 1247–54. doi:10.1038/sj.bjp.0705889. PMID 15249429.
- ↑ Pacher P, Bátkai S, Kunos G (2006). "The endocannabinoid system as an emerging target of pharmacotherapy". Pharmacol. Rev. 58 (3): 389–462. doi:10.1124/pr.58.3.2. PMID 16968947.
- ↑ Gaoni Y, Mechoulam R (1964). "Isolation, structure and partial synthesis of an active constituent of hashish". J. Am. Chem. Soc. 86 (8): 1646–1647. doi:10.1021/ja01062a046.
- ↑ Galve-Roperh I, Sánchez C, Cortés ML, del Pulgar TG, Izquierdo M, Guzmán M (2000). "Anti-tumoral action of cannabinoids: involvement of sustained ceramide accumulation and extracellular signal-regulated kinase activation". Nat. Med. 6 (3): 313–9. doi:10.1038/73171. PMID 10700234.
- ↑ Whiteside GT, Lee GP, Valenzano KJ (2007). "The role of the cannabinoid CB2 receptor in pain transmission and therapeutic potential of small molecule CB2 receptor agonists". Curr. Med. Chem. 14 (8): 917–36. PMID 17430144.
- ↑ 15.0 15.1 Ofek O, Karsak M, Leclerc N, Fogel M, Frenkel B, Wright K, Tam J, Attar-Namdar M, Kram V, Shohami E, Mechoulam R, Zimmer A, Bab I (2006). "Peripheral cannabinoid receptor, CB2, regulates bone mass". Proc. Natl. Acad. Sci. U.S.A. 103 (3): 696–701. doi:10.1073/pnas.0504187103. PMID 16407142.
- ↑ Steffens S, Veillard NR, Arnaud C, Pelli G, Burger F, Staub C, Karsak M, Zimmer A, Frossard JL, Mach F (2005). "Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice". Nature. 434 (7034): 782–6. doi:10.1038/nature03389. PMID 15815632.
- ↑ Panikashvili D, Simeonidou C, Ben-Shabat S, Hanus L, Breuer A, Mechoulam R, Shohami E (2001). "An endogenous cannabinoid (2-AG) is neuroprotective after brain injury". Nature. 413 (6855): 527–31. doi:10.1038/35097089. PMID 11586361.
External links
- The Endocannabinoid System Network (ECSN) - CB1 receptor
- Cannabinoid+Receptors at the US National Library of Medicine Medical Subject Headings (MeSH)
de:Cannabinoid-Rezeptor it:Recettori cannabinoidi fi:Kannabinoidireseptori