Clopidogrel detailed information
 | |
 | |
| Clinical data | |
|---|---|
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | >50% |
| Protein binding | 94–98% |
| Metabolism | Hepatic |
| Elimination half-life | 7–8 hours (inactive metabolite) |
| Excretion | 50% renal 46% biliary |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| E number | {{#property:P628}} |
| ECHA InfoCard | {{#property:P2566}}Lua error in Module:EditAtWikidata at line 36: attempt to index field 'wikibase' (a nil value). |
| Chemical and physical data | |
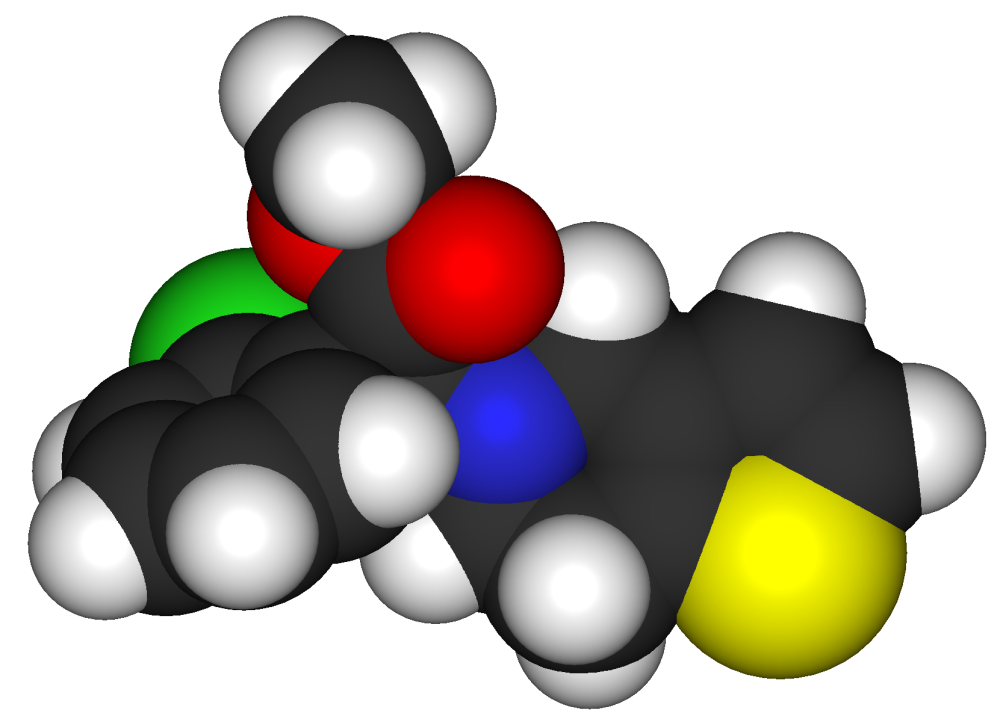
| Formula | C16H16ClNO2S |
| Molar mass | 321.82 g/mol |

For patient information, click here
Clopidogrel is a potent oral antiplatelet agent often used in the treatment of coronary artery disease, peripheral vascular disease, and cerebrovascular disease. It is marketed by Bristol-Myers Squibb and Sanofi-Aventis under the trade name Plavix. In 2006, generic clopidogrel was briefly marketed by Apotex, a Canadian generic pharmaceutical company before a court order halted further production until resolution of a patent infringement case brought by Bristol-Myers Squibb.[1] The court ruled that Bristol-Myers Squibb's patent was valid and has patent protection until November 2011.[2] In 2007, the production was halted to many retail pharmacies and will be changing back to Plavix. In 2005 it was reported that Plavix was the world's second highest selling pharmaceutical with sales of US$5.9 billion.[3]
Pharmacology
The mechanism of action of clopidogrel is irreversible blockade of the adenosine diphosphate (ADP) receptor on platelet cell membranes. This receptor is named P2Y12 and is important in platelet aggregation, the cross-linking of platelets by fibrin. The blockade of this receptor inhibits platelet aggregation by blocking activation of the glycoprotein IIb/IIIa pathway.
Platelet inhibition can be demonstrated two hours after a single dose of oral clopidogrel, but the onset of action is slow, so that a loading-dose of 300-600 mg is usually administered.
Clinical use
Indications
Clopidogrel is indicated for:[4]
- Prevention of vascular ischaemic events in patients with symptomatic atherosclerosis
- Acute coronary syndrome without ST-segment elevation (NSTEMI), along with aspirin
It is also used, along with aspirin, for the prevention of thromboembolism after placement of intracoronary stent. [4]
Most consensus-based therapeutic guidelines recommend the use of clopidogrel, over aspirin, in patients requiring antiplatelet therapy but with a history of gastric ulceration, as inhibition of the synthesis of prostaglandins by aspirin (acetylsalicylic acid) can exacerbate this condition. A recent study has shown that in patients with healed aspirin-induced ulcers, however, patients receiving aspirin plus the proton pump inhibitor esomeprazole had a lower incidence of recurrent ulcer bleeding than patients receiving clopidogrel. [5]
Dosage forms
Clopidogrel is marketed as clopidogrel bisulfate (clopidogrel hydrogen sulfate), most commonly under the trade names Plavix or Iscover, as 75 mg oral tablets.
Use in percutaneous coronary intervention (PCI)
In a 2008 systematic review of literature from the last twenty years, investigators found that ST-segment elevation myocardial infarction (STEMI) patients pretreated with clopidogrel prior to percutaneous coronary intervention (PCI) had better pre-PCI patency and outcomes than those who did not undergo pretreatment. Data was collected from 26 randomized, controlled studies comprising of 38 treatment groups and 8,429 patients. Of the patients who received a clopidogrel loading dose prior to PCI (n=4,114), 34.3% had a pre-PCI TIMI flow grade of 2 or 3, whereas this flow was achieved in 25.8% of those who were not pretreated (n=4,315). Although the follow-up duration varied among the studies, rates of mortality and of the composite of death and reinfarction were lower in pretreated patients (2.4% vs 4.6% and 3.3% vs. 6.3% respectively). While recommendations currently include pretreatment with clopidogrel for acute coronary syndromes and thrombolytic studies, the results of this systematic review suggest the benefits of this treatment strategy for STEMI patients. The study is not a pooled analysis or meta-analysis and is further limited by including data from studies with different designs and interventional strategies.[6]
Pharmacokinetics and Metabolism
After repeated 75-mg oral doses of clopidogrel (base), plasma concentrations of the parent compound, which has no platelet inhibiting effect, are very low and are generally below the quantification limit (0.000258 mg/L) beyond 2 hours after dosing. Clopidogrel is extensively metabolized by the liver. The main circulating metabolite is the carboxylic acid derivative, and it too has no effect on platelet aggregation. It represent about 85% of the circulating drug-related compound in plasma.
Following an oral dose of 14C-labeled clopidogrel in humans, approximately 50% was excreted in the urine and approximately 46% in the feces in the 5 days after dosing. The elimination half-life of the main circulating metabolite was 8 hours after single and repeated administration. Covalent binding to platelets accounted for 2% of radiolabel with a half-life of 11 days. Effect of Food: Administration of PLAVIX (clopidogrel bisulfate) with meals did not significantly modify the bioavailability of clopidogrel as assessed by the pharmacokinetics of the main circulating metabolite.
Absorption and Distribution: Clopidogrel is rapidly absorbed after oral administration of repeated doses of 75 mg clopidogrel (base), with peak plasma levels (appx. 3 mg/L) of the main circulating metabolite occurring approximately 1 hour after dosing. The pharmacokinetics of the main circulating metabolite are linear (plasma concentrations increased in proportion to does) in the dose range of 50 to 150 mg of clopidogrel. Absorption is at least 50% based on urinary excretion of clopidogrel-related metabolites. Clopidogrel and the main circulating metabolite bind reversibly in vitro to human plasma proteins (98% and 94%, respectively). The binding is nonsaturable in vitro up to a concentration of 110 μg/mL.
Metabolism and Elimination: In vitro and in vivo, clopidogrel undergoes rapid hydrolysis into its carboxylic acid derivative. In plasma and urine, the glucuronide of the carboxylic acid derivative is also observed.
Effect of Calcium-Channel Blockers: An October 2008 Austrian study demonstrates that calcium-channel blockers (CCBs) reduce the antiplatelet effect of clopidogrel. The study examined the interaction by comparing the platelet reactivity index (PRI) (as determined by vasodilator-stimulated phosphoprotein (VASP) phosphorylation assay) for 200 patients with coronary artery disease who were undergoing percutaneous coronary intervention. Patients taking concomitant CCBs and clopidogrel had displayed a PRI of 61%, while patients receiving clopidogrel alone demonstrated a PRI of 48% (absolute difference 13%; 95% CI: 6% to 20%; p = 0.001). The relative difference between the two sets of patients was approximately 21%. An in vitro experiment involving the incubation of blood from 10 additional patients, who received clopidogrel alone, with CCBs showed no difference in the PRI. This finding led the research team to hypothesize that the CCBs block the in vivo bioactivation of clopidogrel by the cytochrome P450 isoform 3A4. The majority of patients in the CCB subset received amlodipine, so additional studies are required to help establish a class effect.[7]
Adverse effects
Serious adverse drug reactions associated with clopidogrel therapy include:
- Severe neutropenia (Incidence: 5/10,000)
- Thrombotic thrombocytopenic purpura (TTP) (Incidence: 4/1,000,000 patients treated)
- Hemorrhage - The incidence of hemorrhage may be increased by the co-administration of aspirin.
- Gastrointestinal Hemorrhage (Incidence: 2.0%)
- Cerebral Hemorrhage (Incidence: 0.1 to 0.4%)
- Erectile Dyfunction (Incidence as yet unknown)
References
- ↑ "Preliminary Injunction Against Apotex Upheld on Appeal - Press Release".
- ↑ "U.S. judge upholds Bristol, Sanofi patent on Plavix". Text " Reuters " ignored (help)
- ↑ "IMS HEALTH".
- ↑ 4.0 4.1 Rossi S, editor. Australian Medicines Handbook 2006. Adelaide: Australian Medicines Handbook; 2006. ISBN 0-9757919-2-3
- ↑ Chan FK, Ching JY, Hung LC; et al. (2005). "Clopidogrel versus aspirin and esomeprazole to prevent recurrent ulcer bleeding". N. Engl. J. Med. 352 (3): 238–44. doi:10.1056/NEJMoa042087. PMID 15659723.
- ↑ Vlaar PJ, Svilaas T, Damman K, de Smet BJ, Tijssen JG, Hillege HL, Zijlstra F (2008). "Impact of pretreatment with clopidogrel on initial patency and outcome in patients treated with primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review". Circulation. 118 (18): 1828–36. doi:10.1161/CIRCULATIONAHA.107.749531. PMID 18852370.
- ↑ Jolanta M. Siller-Matula, Irene Lang, Guenter Christ, and Bernd Jilma (2008). "Calcium-Channel Blockers Reduce the Antiplatelet Effect of Clopidogrel". JACC. 52 (19): 1557–1563. doi:10.1016/j.jacc.2008.07.055.
External links
- Template:DailyMed
- Plavix : Information for the General Public
- Plavix, Aspirin and Stents : Patients' Forum : Angioplasty.Org
- Pages with script errors
- Pages with citations using unnamed parameters
- CS1 maint: Explicit use of et al.
- CS1 maint: Multiple names: authors list
- E number from Wikidata
- ECHA InfoCard ID from Wikidata
- Chemical articles with unknown parameter in Infobox drug
- Articles without EBI source
- Chemical pages without ChemSpiderID
- Articles without KEGG source
- Articles without InChI source
- Articles without UNII source
- Articles containing unverified chemical infoboxes
- Antiplatelet drugs
- ADP receptor inhibitors
- Sanofi-Aventis
- Thiophenes
- Drugs