Sudden cardiac death definitions and diagnosis: Difference between revisions
Jump to navigation
Jump to search
No edit summary |
No edit summary |
||
| (33 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
__NOTOC__ | __NOTOC__ | ||
{{ | {{Sudden cardiac death}} | ||
{{CMG}} {{AE}} {{Sara.Zand}} {{EdzelCo}} | |||
==Overview== | |||
*The diagnosis of [[sudden cardiac arrest]] ([[SCA]]) is made when the following diagnostic criteria are met: the absence of a [[palpable pulse]] of the [[heart]] due to abrupt cessation of [[pump function]], absent [[carotid pulse]],[[gasping respiration]] or no [[respiration]], loss of [[consciousness]] due to [[cerebral hypoperfusion]]. | |||
==Definitions and Diagnosis== | |||
*The [[diagnosis]] of [[SCA]] is made when the following [[diagnostic criteria]] are satisfied: | |||
:*Absence of a [[palpable pulse]] of the [[heart]] due to cessation of pumping function whether with prompt intervention will be reversible <ref name="Harrison"> [http://books.mcgraw-hill.com/medical/harrisons/ Harrison's Principles of Internal Medicine] 16th Edition, The McGraw-Hill Companies, ISBN 0-07-140235-7</ref> | |||
:*Absent [[carotid pulse]]<ref>Flesche CW, Breuer S, Mandel LP, Breivik H, Tarnow J. (1994) The ability of health professionals to check the carotid pulse. ''Circulation'' Vol. 90: I–288.</ref><ref name="pmid9715777">{{cite journal |author=Ochoa FJ, Ramalle-Gómara E, Carpintero JM, García A, Saralegui I |title=Competence of health professionals to check the carotid pulse |journal=Resuscitation |volume=37 |issue=3 |pages=173–5 |year=1998 |month=June |pmid=9715777 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0300957298000550}}</ref><ref name="pmid9259056">{{cite journal |author=Bahr J, Klingler H, Panzer W, Rode H, Kettler D |title=Skills of lay people in checking the carotid pulse |journal=Resuscitation |volume=35 |issue=1 |pages=23–6 |year=1997 |month=August |pmid=9259056 |doi= |url=http://linkinghub.elsevier.com/retrieve/pii/S0300957296010921}}</ref><ref name="pmid16314375">{{cite journal |author= |title=2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care |journal=Circulation |volume=112 |issue=24 Suppl |pages=IV1–203 |year=2005 |month=December |pmid=16314375 |doi=10.1161/CIRCULATIONAHA.105.166550 |url=}}</ref> | |||
:*[[Gasping respiration]] or no [[respiration]] | |||
:*Loss of [[consciousness]] due to [[cerebral hypoperfusion]] | |||
{| style="border: 2px solid #4479BA; align="left" | |||
! style="width: 200px; background: #4479BA;" | {{fontcolor|#FFF|Components}} | |||
! style="width: 300px; background: #4479BA;" | {{fontcolor|#FFF|Assessment and findings}} | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Symptoms | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
* Symptoms related to [[arrhythmia]]<ref name="ZimetbaumJosephson1998">{{cite journal|last1=Zimetbaum|first1=Peter|last2=Josephson|first2=Mark E.|title=Evaluation of Patients with Palpitations|journal=New England Journal of Medicine|volume=338|issue=19|year=1998|pages=1369–1373|issn=0028-4793|doi=10.1056/NEJM199805073381907}}</ref><ref name="NodaShimizu2005">{{cite journal|last1=Noda|first1=Takashi|last2=Shimizu|first2=Wataru|last3=Taguchi|first3=Atsushi|last4=Aiba|first4=Takeshi|last5=Satomi|first5=Kazuhiro|last6=Suyama|first6=Kazuhiro|last7=Kurita|first7=Takashi|last8=Aihara|first8=Naohiko|last9=Kamakura|first9=Shiro|title=Malignant Entity of Idiopathic Ventricular Fibrillation and Polymorphic Ventricular Tachycardia Initiated by Premature Extrasystoles Originating From the Right Ventricular Outflow Tract|journal=Journal of the American College of Cardiology|volume=46|issue=7|year=2005|pages=1288–1294|issn=07351097|doi=10.1016/j.jacc.2005.05.077}}</ref> | |||
: [[Palpitations]], [[lightheadedness]], [[syncope]], [[dyspnea]], [[chest pain]], [[cardiac arrest]] | |||
* Symptoms related to underlying [[heart disease]]: [[Dyspnea]] at rest or on exertion, [[orthopnea]], [[paroxysmal nocturnal dyspnea]], [[chest pain]], [[edema]] | |||
* Precipitating factors: [[Exercise]], [[emotional stress]] | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Past medical history | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
* [[Heart disease]]: [[Coronary]], [[valvular]] ([[mitral valve prolapse]]), [[congenital heart disease]] | |||
* [[Thyroid disease]] | |||
* [[Acute kidney injury]] | |||
* [[Chronic kidney disease]] | |||
* [[Electrolyte abnormalities]] | |||
* [[Stroke]],[[embolic events]] | |||
* [[Lung disease]] | |||
* [[Epilepsy]] ([[arrhythmic syncope]] can be misdiagnosed as [[epilepsy]]) | |||
* [[ Alcohol]], [[illicit drug]] use | |||
* Use of over-the-counter medications caused [[QT prolongation]] and [[torsades de pointes]] | |||
* [[ Unexplained motor vehicle accident]] | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Medications | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
* [[Antiarrhythmic]] medications | |||
* Medication with QT prolongation and torsades de pointes effect | |||
* [[Cocaine]],[[amphetamines]] | |||
* [[Anabolic steroids]] | |||
* Medication-medication interaction that could cause [[QT prolongation]] and [[torsades de pointes]] | |||
|- | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | Family history | |||
| style="padding: 0 5px; background: #F5F5F5; text-align: left;" | | |||
* [[SCD]], [[SCA]], [[unexplained drowning]] in a first-degree relative | |||
* [[SIDS]], repetitive spontaneous [[pregnancy losses]] concerning [[cardiac channelopathies]] | |||
* [[IHD]] | |||
* [[Cardiomyopathy]]: [[Hypertrophic]],[[ dilated]], [[ARVC]] | |||
* [[Congenital heart disease]] | |||
* [[ Cardiac channelopathies]]: [[Long QT]], [[Brugada]], [[Short QT]], [[CPVT]] | |||
* [[Arrhythmias]]: [[conduction disorders]], [[ pacemakers]]/[[ICDs]] | |||
* [[Neuromuscular disease]] associated with [[cardiomyopathies]] | |||
* [[Muscular dystrophy]] | |||
* [[Epilepsy]] | |||
|- | |||
|} | |||
Following initial diagnosis of cardiac arrest, healthcare professionals further | *Following an initial [[diagnosis]] of [[cardiac arrest]], [[healthcare professionals]] further categorize the [[diagnosis]] based on the [[ECG]] [[rhythm]]. | ||
*There are 4 [[rhythm]]s that result in a [[cardiac arrest]]. [[Ventricular fibrillation]] ([[VF]]) and [[Pulseless]] [[Ventricular tachycardia]] ([[VTach]]) are both responsive to a [[defibrillator]] and so are colloquially referred to as [[Shockable]] [[rhythm]]s, whereas [[Asystole]] and [[Pulseless electrical activity|Pulseless Electrical Activity]] ([[PEA]]) are non-shockable. | |||
*The nature of the presenting [[heart]] [[rhythm]] suggests different causes and [[treatment]] and is used to guide the rescuer as to what treatment may be appropriate<ref name="RCUK2005">Resuscitation Council UK (2005). ''Resuscitation Guidelines 2005'' London: Resuscitation Council UK.</ref> (see [[Advanced Life Support]] and [[Advanced Cardiac Life Support]], as well as the causes of arrest (below)) | |||
*The table below provides information on the differential diagnosis of [[sudden cardiac death]] in terms of [[ECG]] appearance: | |||
{| border="3" | |||
|+ | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Disease Name}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| Causes}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG Characteristics}} | |||
! style="background: #4479BA; width: 150px;" | {{fontcolor|#FFF| ECG view}} | |||
|- | |||
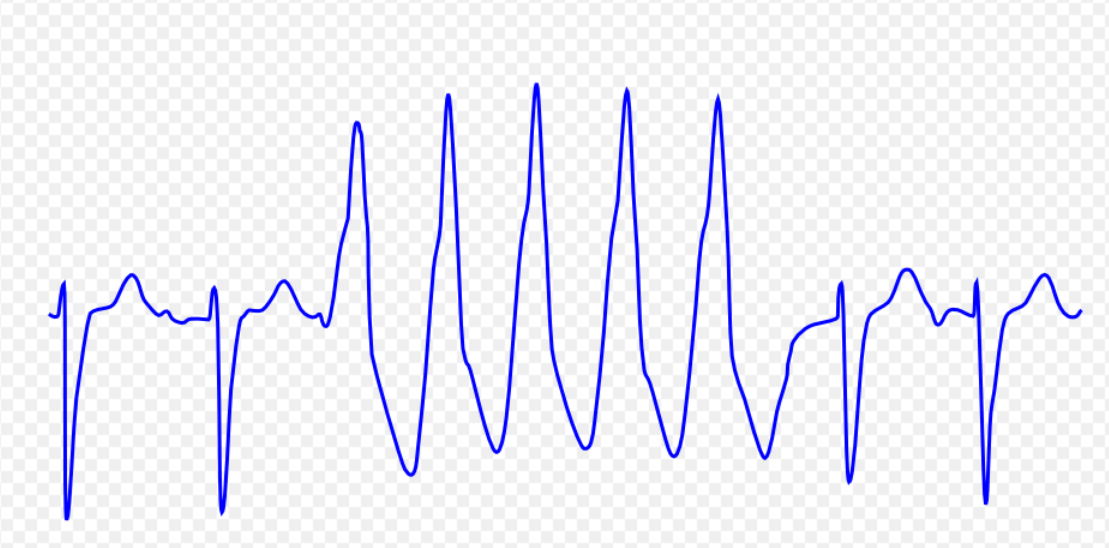
! style="padding: 5px 5px; background: #DCDCDC; " align="left"| '''[[Ventricular tachycardia]]''' <ref name="AjijolaTung2014">{{cite journal|last1=Ajijola|first1=Olujimi A.|last2=Tung|first2=Roderick|last3=Shivkumar|first3=Kalyanam|title=Ventricular tachycardia in ischemic heart disease substrates|journal=Indian Heart Journal|volume=66|year=2014|pages=S24–S34|issn=00194832|doi=10.1016/j.ihj.2013.12.039}}</ref><ref name="Meja LopezMalhotra2019">{{cite journal|last1=Meja Lopez|first1=Eliany|last2=Malhotra|first2=Rohit|title=Ventricular Tachycardia in Structural Heart Disease|journal=Journal of Innovations in Cardiac Rhythm Management|volume=10|issue=8|year=2019|pages=3762–3773|issn=21563977|doi=10.19102/icrm.2019.100801}}</ref><ref name="CoughtrieBehr2017">{{cite journal|last1=Coughtrie|first1=Abigail L|last2=Behr|first2=Elijah R|last3=Layton|first3=Deborah|last4=Marshall|first4=Vanessa|last5=Camm|first5=A John|last6=Shakir|first6=Saad A W|title=Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort|journal=BMJ Open|volume=7|issue=10|year=2017|pages=e016627|issn=2044-6055|doi=10.1136/bmjopen-2017-016627}}</ref><ref name="El-Sherif2001">{{cite journal|last1=El-Sherif|first1=Nabil|title=Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics|journal=Journal of Cardiovascular Electrophysiology|volume=12|issue=8|year=2001|pages=973–976|issn=1045-3873|doi=10.1046/j.1540-8167.2001.00973.x}}</ref><ref name="de RivaWatanabe2015">{{cite journal|last1=de Riva|first1=Marta|last2=Watanabe|first2=Masaya|last3=Zeppenfeld|first3=Katja|title=Twelve-Lead ECG of Ventricular Tachycardia in Structural Heart Disease|journal=Circulation: Arrhythmia and Electrophysiology|volume=8|issue=4|year=2015|pages=951–962|issn=1941-3149|doi=10.1161/CIRCEP.115.002847}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Ischemic heart disease]] | |||
*Illicit drug use such as [[cocaine]] and [[methamphetamine]] | |||
*[[Structural heart diseases]] | |||
*[[Electrolyte disturbances]] | |||
*[[Congestive heart failure]] | |||
*[[Myocarditis]] | |||
*[[Obstructive sleep apnea]] | |||
*[[Pulmonary artery catheter]] | |||
*[[Long QT syndrome]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Ventricular tachycardia]] ([[VTach]] originates from a [[ventricular]] focus. | |||
* Lasts more than 30 seconds. | |||
* [[Broad QRS complex]]es: rate of >90 BPM. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[File:Capture V tach.PNG|center|300px]]<ref> ECG found in of https://en.ecgpedia.org/index.php?title=Main_Page </ref> | |||
|- | |||
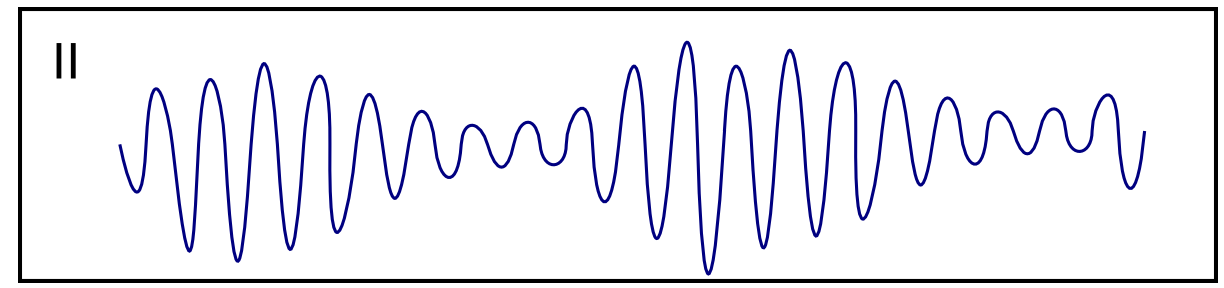
! style="padding: 5px 5px; background: #DCDCDC; " align="left"| '''[[Ventricular fibrillation]]''' <ref name="pmid19252119">{{cite journal |vauthors=Koplan BA, Stevenson WG |title=Ventricular tachycardia and sudden cardiac death |journal=Mayo Clin. Proc. |volume=84 |issue=3 |pages=289–97 |date=March 2009 |pmid=19252119 |pmc=2664600 |doi=10.1016/S0025-6196(11)61149-X |url=}}</ref><ref name="pmid28222965">{{cite journal |vauthors=Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S |title=Ventricular arrhythmias and sudden death in tetralogy of Fallot |journal=Arch Cardiovasc Dis |volume=110 |issue=5 |pages=354–362 |date=May 2017 |pmid=28222965 |doi=10.1016/j.acvd.2016.12.006 |url=}}</ref><ref name="pmid1638716">{{cite journal |vauthors=Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ |title=Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms |journal=Circulation |volume=86 |issue=2 |pages=467–74 |date=August 1992 |pmid=1638716 |doi=10.1161/01.cir.86.2.467 |url=}}</ref><ref name="BektasSoyuncu2012">{{cite journal|last1=Bektas|first1=Firat|last2=Soyuncu|first2=Secgin|title=Hypokalemia-induced Ventricular Fibrillation|journal=The Journal of Emergency Medicine|volume=42|issue=2|year=2012|pages=184–185|issn=07364679|doi=10.1016/j.jemermed.2010.05.079}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Coronary ischemia|Acute coronary ischemia]] | |||
*[[cardiomyopathy|Cardiomyopathies]] | |||
*[[Congenital heart disease]] | |||
*[[Myocardial infarction]] | |||
*[[Heart surgery]] | |||
*[[Electrolyte abnormalities]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
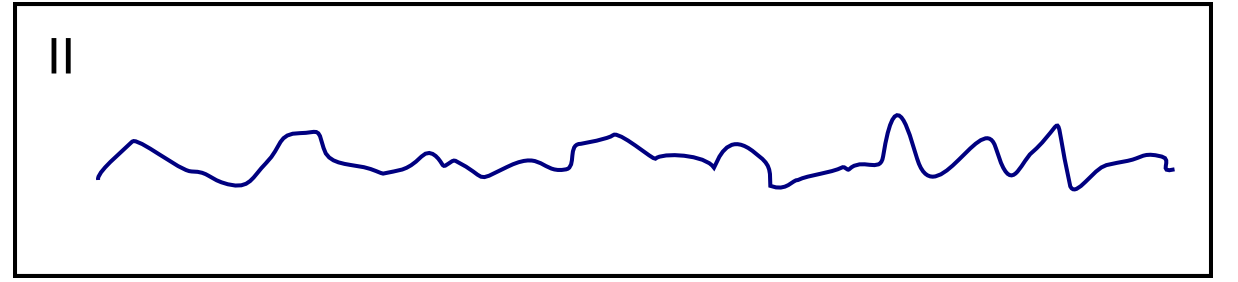
* Poorly identifiable [[QRS complexes]] and absent [[P waves]] | |||
* The [[heart rate]] is >300 BPM | |||
*[[Rhythm]] is irregular | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[File:Capture VF.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | |||
|- | |||
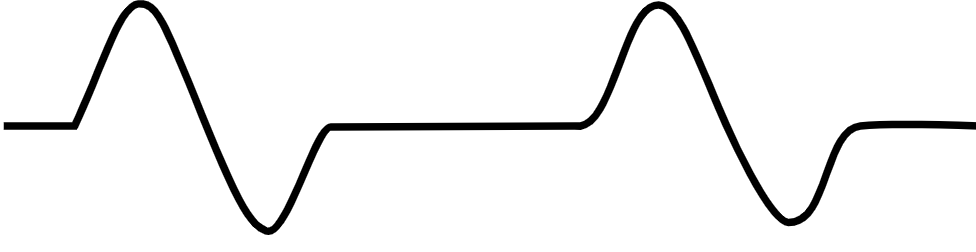
! style="padding: 5px 5px; background: #DCDCDC; " align="left"| '''[[Ventricular flutter]]''' <ref name="ThiesBoos2000">{{cite journal|last1=Thies|first1=Karl-Christian|last2=Boos|first2=Karin|last3=Müller-Deile|first3=Kai|last4=Ohrdorf|first4=Wolfgang|last5=Beushausen|first5=Thomas|last6=Townsend|first6=Peter|title=Ventricular flutter in a neonate—severe electrolyte imbalance caused by urinary tract infection in the presence of urinary tract malformation|journal=The Journal of Emergency Medicine|volume=18|issue=1|year=2000|pages=47–50|issn=07364679|doi=10.1016/S0736-4679(99)00161-4}}</ref><ref name="KosterWellens1976">{{cite journal|last1=Koster|first1=Rudolph W.|last2=Wellens|first2=Hein J.J.|title=Quinidine-induced ventricular flutter and fibrillation without digitalis therapy|journal=The American Journal of Cardiology|volume=38|issue=4|year=1976|pages=519–523|issn=00029149|doi=10.1016/0002-9149(76)90471-9}}</ref><ref name="pmid250503">{{cite journal |vauthors=Dhurandhar RW, Nademanee K, Goldman AM |title=Ventricular tachycardia-flutter associated with disopyramide therapy: a report of three cases |journal=Heart Lung |volume=7 |issue=5 |pages=783–7 |date=1978 |pmid=250503 |doi= |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Electrolyte disturbances]] | |||
*[[Medications]] such as: | |||
**[[Disopyramide]] | |||
**[[Quinidine]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
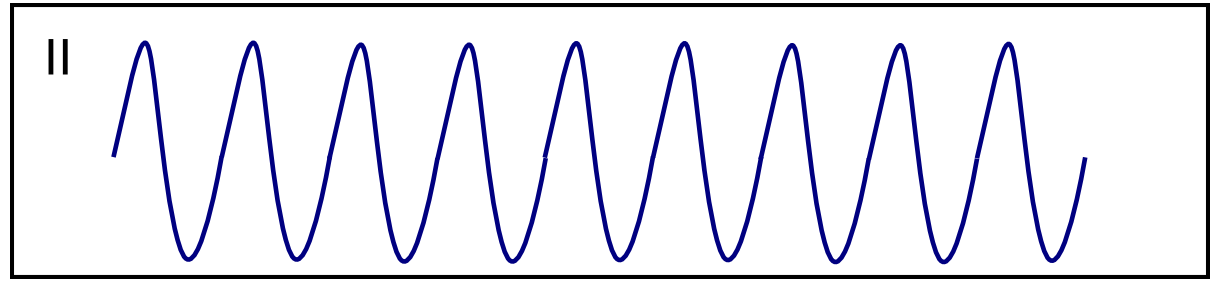
*The [[ECG]] shows: | |||
**A typical [[sinusoidal]] pattern | |||
**Frequency of 300 bpm | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[File:Capture Ven Flu.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Asystole]]''' <ref name="ACLS_2003_H_T">''ACLS: Principles and Practice''. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.</ref><ref name="ACLS_2003_EP_HT">''ACLS for Experienced Providers''. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Hypovolemia]] | |||
*[[Hypoxia (medical)|Hypoxia]] | |||
*[[Acidosis]] | |||
*[[Hypothermia|Hypothermia]] | |||
*[[Hyperkalemia|Hyperkalemia]] or [[Hypokalemia|Hypokalemia]] | |||
*[[Hypoglycemia|Hypoglycemia]] | |||
*[[Cardiac tamponade|Cardiac Tamponade]] | |||
*[[Tension pneumothorax|Tension pneumothorax]] | |||
*[[Thrombosis|Thrombosis]] | |||
*[[Myocardial infarction]] | |||
*[[Thrombosis|Thrombosis]] | |||
*[[Pulmonary embolism]] | |||
*[[Cardiogenic shock]] | |||
*Degeneration of the [[sinoatrial]] or [[atrioventricular]] nodes | |||
*[[Ischemic stroke]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
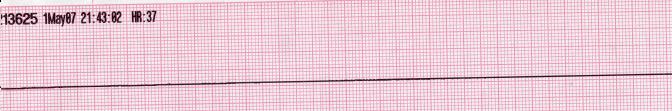
* There is no electrical activity in the asystole | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[Image:Lead II rhythm generated asystole.JPG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" | '''[[Pulseless electrical activity]]''' <ref name="ECC_2005_7.2">"2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." ''Circulation'' 2005; '''112''': IV-58 - IV-66.</ref><ref>Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*[[Hypovolemia]] | |||
*[[Hypoxia]] | |||
*Hydrogen ions ([[Acidosis]]) | |||
*[[Hypothermia]] | |||
*[[Electrolyte disturbances]] | |||
*[[Hypoglycemia]] | |||
*[[Tablets]] or [[Toxins]] (Drug overdose) such as [[beta blockers]], [[tricyclic antidepressants]], or [[calcium channel blockers]] | |||
*[[Tamponade]] | |||
*[[Tension pneumothorax]] | |||
*[[Thrombosis]] ([[Myocardial infarction]]) | |||
*[[Thrombosis]] ([[Pulmonary embolism]]) | |||
*[[Trauma]] ([[Hypovolemia]] from [[blood loss]]) | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
*Several ppattern are possible including: | |||
**[[Normal sinus rhythm]] | |||
**[[Sinus tachycardia]], with discernible [[P waves]] and [[QRS complexes]] | |||
**[[Bradycardia]], with or without [[P waves]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[File:Capture PEA.PNG|center|300px]]<ref> ECG found in wikimedia Commons </ref> | |||
|- | |||
! style="padding: 5px 5px; background: #DCDCDC;" align="left" |'''[[Torsade de Pointes]]''' <ref name="pmid28674475">{{cite journal |vauthors=Li M, Ramos LG |title=Drug-Induced QT Prolongation And Torsades de Pointes |journal=P T |volume=42 |issue=7 |pages=473–477 |date=July 2017 |pmid=28674475 |pmc=5481298 |doi= |url=}}</ref><ref name="SharainMay2015">{{cite journal|last1=Sharain|first1=Korosh|last2=May|first2=Adam M.|last3=Gersh|first3=Bernard J.|title=Chronic Alcoholism and the Danger of Profound Hypomagnesemia|journal=The American Journal of Medicine|volume=128|issue=12|year=2015|pages=e17–e18|issn=00029343|doi=10.1016/j.amjmed.2015.06.051}}</ref><ref name="pmid11330748">{{cite journal |vauthors=Khan IA |title=Twelve-lead electrocardiogram of torsades de pointes |journal=Tex Heart Inst J |volume=28 |issue=1 |pages=69 |date=2001 |pmid=11330748 |pmc=101137 |doi= |url=}}</ref> | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
* *[[Electrolyte disturbances]] | |||
*[[Medications]] such as: | |||
**[[Amiodarone]] | |||
**[[Azithromycin]] | |||
**[[Clozapine]] | |||
**[[Famotidine]] | |||
**[[Flecainide]] | |||
**[[Foscarnet]] | |||
**[[Levofloxacin]] | |||
**[[Lithium]] | |||
**[[Mirtazapine]] | |||
**[[Quetiapine]] | |||
**[[Risperidone]] | |||
**[[Tacrolimus]] | |||
**[[Tamoxifen]] | |||
**[[Ziprasidone]] | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
# Paroxysms of [[VTach]] with irregular RR intervals. | |||
# A [[ventricular]] [[rate]] between 200 and 250 beats per minute. | |||
# Two or more cycles of [[QRS complex]]es with alternating polarity. | |||
# Changing the amplitude of the [[QRS complexes]] in each cycle in a sinusoidal fashion. | |||
# Prolongation of the [[QT interval]]. | |||
# Is often initiated by a [[PVC]] with a long coupling interval, R on T phenomenon. | |||
# There are usually 5 to 20 complexes in each cycle. | |||
| style="padding: 5px 5px; background: #F5F5F5;" align="left" | | |||
[[File:Capture Tors De P.PNG|center|300px]]<ref> ECG found in https://en.ecgpedia.org/index.php?title=Main_Page </ref> | |||
|} | |||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
[[Category:Cardiology]] | |||
[[Category:Public health]] | |||
[[Category:Electrophysiology]] | |||
[[Category:Emergency medicine]] | |||
Latest revision as of 19:28, 19 July 2023
|
Sudden cardiac death Microchapters |
|
Diagnosis |
|---|
|
Sudden cardiac death definitions and diagnosis On the Web |
|
American Roentgen Ray Society Images of Sudden cardiac death definitions and diagnosis |
|
Risk calculators and risk factors for Sudden cardiac death definitions and diagnosis |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Zand, M.D.[2] Edzel Lorraine Co, DMD, MD[3]
Overview
- The diagnosis of sudden cardiac arrest (SCA) is made when the following diagnostic criteria are met: the absence of a palpable pulse of the heart due to abrupt cessation of pump function, absent carotid pulse,gasping respiration or no respiration, loss of consciousness due to cerebral hypoperfusion.
Definitions and Diagnosis
- The diagnosis of SCA is made when the following diagnostic criteria are satisfied:
- Absence of a palpable pulse of the heart due to cessation of pumping function whether with prompt intervention will be reversible [1]
- Absent carotid pulse[2][3][4][5]
- Gasping respiration or no respiration
- Loss of consciousness due to cerebral hypoperfusion
- Following an initial diagnosis of cardiac arrest, healthcare professionals further categorize the diagnosis based on the ECG rhythm.
- There are 4 rhythms that result in a cardiac arrest. Ventricular fibrillation (VF) and Pulseless Ventricular tachycardia (VTach) are both responsive to a defibrillator and so are colloquially referred to as Shockable rhythms, whereas Asystole and Pulseless Electrical Activity (PEA) are non-shockable.
- The nature of the presenting heart rhythm suggests different causes and treatment and is used to guide the rescuer as to what treatment may be appropriate[8] (see Advanced Life Support and Advanced Cardiac Life Support, as well as the causes of arrest (below))
- The table below provides information on the differential diagnosis of sudden cardiac death in terms of ECG appearance:
| Disease Name | Causes | ECG Characteristics | ECG view |
|---|---|---|---|
| Ventricular tachycardia [9][10][11][12][13] |
|
 | |
| Ventricular fibrillation [15][16][17][18] |
|
 | |
| Ventricular flutter [20][21][22] |
|
 | |
| Asystole [24][25] |
|
 | |
| Pulseless electrical activity [27][28] |
|
|
 |
| Torsade de Pointes [30][31][32] |
|
 |
References
- ↑ Harrison's Principles of Internal Medicine 16th Edition, The McGraw-Hill Companies, ISBN 0-07-140235-7
- ↑ Flesche CW, Breuer S, Mandel LP, Breivik H, Tarnow J. (1994) The ability of health professionals to check the carotid pulse. Circulation Vol. 90: I–288.
- ↑ Ochoa FJ, Ramalle-Gómara E, Carpintero JM, García A, Saralegui I (1998). "Competence of health professionals to check the carotid pulse". Resuscitation. 37 (3): 173–5. PMID 9715777. Unknown parameter
|month=ignored (help) - ↑ Bahr J, Klingler H, Panzer W, Rode H, Kettler D (1997). "Skills of lay people in checking the carotid pulse". Resuscitation. 35 (1): 23–6. PMID 9259056. Unknown parameter
|month=ignored (help) - ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 112 (24 Suppl): IV1–203. 2005. doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375. Unknown parameter
|month=ignored (help) - ↑ Zimetbaum, Peter; Josephson, Mark E. (1998). "Evaluation of Patients with Palpitations". New England Journal of Medicine. 338 (19): 1369–1373. doi:10.1056/NEJM199805073381907. ISSN 0028-4793.
- ↑ Noda, Takashi; Shimizu, Wataru; Taguchi, Atsushi; Aiba, Takeshi; Satomi, Kazuhiro; Suyama, Kazuhiro; Kurita, Takashi; Aihara, Naohiko; Kamakura, Shiro (2005). "Malignant Entity of Idiopathic Ventricular Fibrillation and Polymorphic Ventricular Tachycardia Initiated by Premature Extrasystoles Originating From the Right Ventricular Outflow Tract". Journal of the American College of Cardiology. 46 (7): 1288–1294. doi:10.1016/j.jacc.2005.05.077. ISSN 0735-1097.
- ↑ Resuscitation Council UK (2005). Resuscitation Guidelines 2005 London: Resuscitation Council UK.
- ↑ Ajijola, Olujimi A.; Tung, Roderick; Shivkumar, Kalyanam (2014). "Ventricular tachycardia in ischemic heart disease substrates". Indian Heart Journal. 66: S24–S34. doi:10.1016/j.ihj.2013.12.039. ISSN 0019-4832.
- ↑ Meja Lopez, Eliany; Malhotra, Rohit (2019). "Ventricular Tachycardia in Structural Heart Disease". Journal of Innovations in Cardiac Rhythm Management. 10 (8): 3762–3773. doi:10.19102/icrm.2019.100801. ISSN 2156-3977.
- ↑ Coughtrie, Abigail L; Behr, Elijah R; Layton, Deborah; Marshall, Vanessa; Camm, A John; Shakir, Saad A W (2017). "Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort". BMJ Open. 7 (10): e016627. doi:10.1136/bmjopen-2017-016627. ISSN 2044-6055.
- ↑ El-Sherif, Nabil (2001). "Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics". Journal of Cardiovascular Electrophysiology. 12 (8): 973–976. doi:10.1046/j.1540-8167.2001.00973.x. ISSN 1045-3873.
- ↑ de Riva, Marta; Watanabe, Masaya; Zeppenfeld, Katja (2015). "Twelve-Lead ECG of Ventricular Tachycardia in Structural Heart Disease". Circulation: Arrhythmia and Electrophysiology. 8 (4): 951–962. doi:10.1161/CIRCEP.115.002847. ISSN 1941-3149.
- ↑ ECG found in of https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S (May 2017). "Ventricular arrhythmias and sudden death in tetralogy of Fallot". Arch Cardiovasc Dis. 110 (5): 354–362. doi:10.1016/j.acvd.2016.12.006. PMID 28222965.
- ↑ Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ (August 1992). "Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms". Circulation. 86 (2): 467–74. doi:10.1161/01.cir.86.2.467. PMID 1638716.
- ↑ Bektas, Firat; Soyuncu, Secgin (2012). "Hypokalemia-induced Ventricular Fibrillation". The Journal of Emergency Medicine. 42 (2): 184–185. doi:10.1016/j.jemermed.2010.05.079. ISSN 0736-4679.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Thies, Karl-Christian; Boos, Karin; Müller-Deile, Kai; Ohrdorf, Wolfgang; Beushausen, Thomas; Townsend, Peter (2000). "Ventricular flutter in a neonate—severe electrolyte imbalance caused by urinary tract infection in the presence of urinary tract malformation". The Journal of Emergency Medicine. 18 (1): 47–50. doi:10.1016/S0736-4679(99)00161-4. ISSN 0736-4679.
- ↑ Koster, Rudolph W.; Wellens, Hein J.J. (1976). "Quinidine-induced ventricular flutter and fibrillation without digitalis therapy". The American Journal of Cardiology. 38 (4): 519–523. doi:10.1016/0002-9149(76)90471-9. ISSN 0002-9149.
- ↑ Dhurandhar RW, Nademanee K, Goldman AM (1978). "Ventricular tachycardia-flutter associated with disopyramide therapy: a report of three cases". Heart Lung. 7 (5): 783–7. PMID 250503.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
- ↑ Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
- ↑ ECG found in wikimedia Commons
- ↑ Li M, Ramos LG (July 2017). "Drug-Induced QT Prolongation And Torsades de Pointes". P T. 42 (7): 473–477. PMC 5481298. PMID 28674475.
- ↑ Sharain, Korosh; May, Adam M.; Gersh, Bernard J. (2015). "Chronic Alcoholism and the Danger of Profound Hypomagnesemia". The American Journal of Medicine. 128 (12): e17–e18. doi:10.1016/j.amjmed.2015.06.051. ISSN 0002-9343.
- ↑ Khan IA (2001). "Twelve-lead electrocardiogram of torsades de pointes". Tex Heart Inst J. 28 (1): 69. PMC 101137. PMID 11330748.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page