Sudden cardiac death classification
|
Sudden cardiac death Microchapters |
|
Diagnosis |
|---|
|
Sudden cardiac death classification On the Web |
|
American Roentgen Ray Society Images of Sudden cardiac death classification |
|
Risk calculators and risk factors for Sudden cardiac death classification |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Sara Zand, M.D.[2] Edzel Lorraine Co, DMD, MD[3]
Overview
Sudden cardiac death (SCD) is defined as sudden and unexpected death within one hour of being symptomatic such as palpitation, chest pain, shortness of breath or within 24 hours in an asymptomatic patient due to arrhythmia or hemodynamic instability.Sudden cardiac arrest (SCA) is suddenly cessation of cardiac activity,unresponsive patient with gasping respiration or no respiratory movement and non-palpable pulses due to cardiac etiology such as arrhythmia, and pump failure. Aborted cardiac arrest is explained as unexpected circulatory collapse within one hour of being symptomatic, which is reversible after successful cardiopulmonary resuscitation. Sudden infant death syndrome (SIDS) is sudden death when the heart is structurally normal without any specific findings in autopsy or toxicology [1].
Classification
There are some definitions related to cardiac arrest including:[2]
| Classification | Definition |
|---|---|
| Sudden cardiac death (SCD) | Sudden and unexpected death within one hour of being symptomatic or whitin 24 hours in asymptomatic patient due to arrhythmia or hemodynamic instability |
| Sudden cardiac arrest (SCA) | Suddenly cessation of cardiac activity,unresponsive patient with gasping respiration or no respiratory movement and unpalpable pulses due to cardiac etiology such as arrhythmia, pump failure |
| Aborted cardiac arrest | Unexpected circulatory collapse within one hour of being symptomatic, which is turned back after successful cardiopulmonary resuscitation |
| Sudden infant death syndrome (SIDS) sudden arrhythmic death syndrome (SADS) | Sudden death if structurally normal heart without any specific findings in autopsy or toxicology |
| sudden unexplained death in infancy (SUDI), sudden unexplained death syndrome (SUDS) | Sudden death without any specific findings in autopsy in adult (SUDS) or infants less than 1 year (SUDI) |
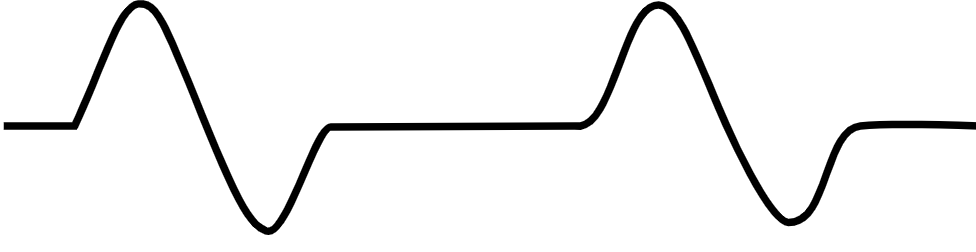
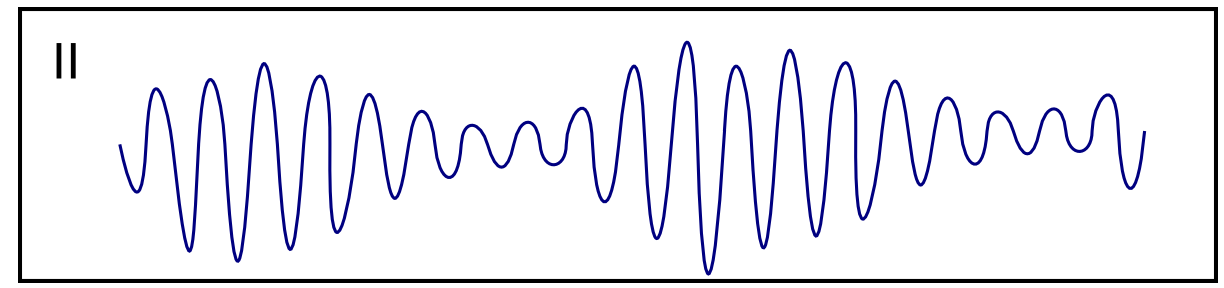
- The table below provides information on the characteristics of sudden cardiac arrest in terms of ECG appearance:
| Classification | Causes | ECG Characteristics | ECG view |
|---|---|---|---|
| Ventricular tachycardia [3][4][5][6][7] |
|
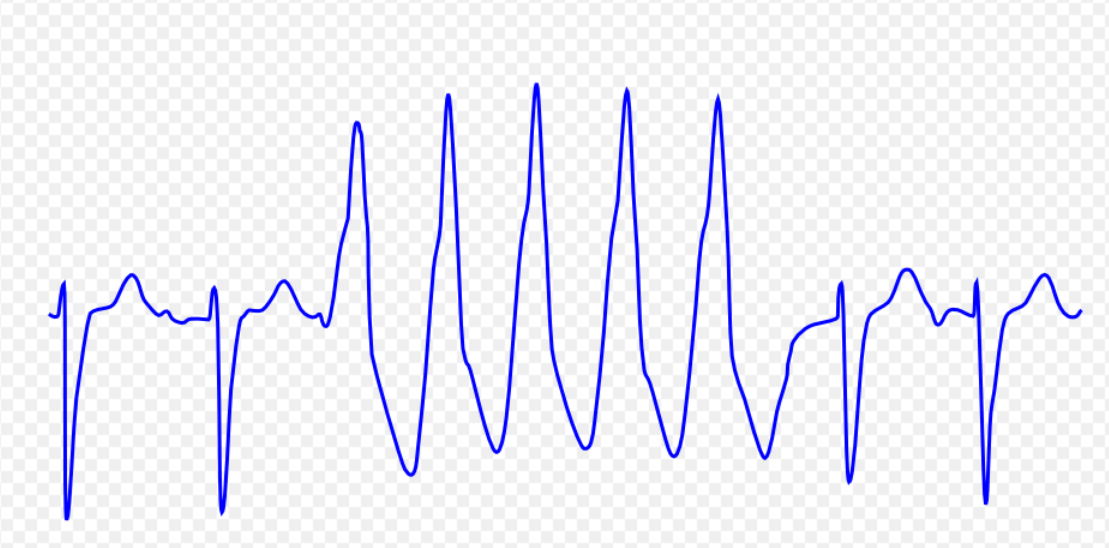 | |
| Ventricular fibrillation [9][10][11][12] |
|
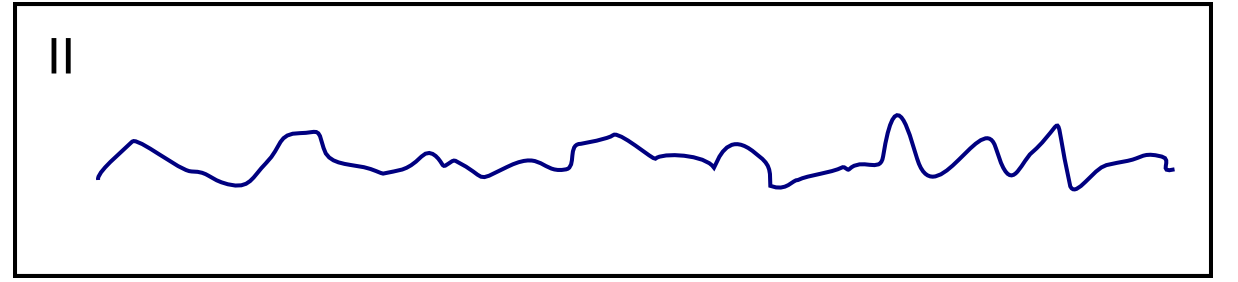 | |
| Ventricular flutter [14][15][16] |
|
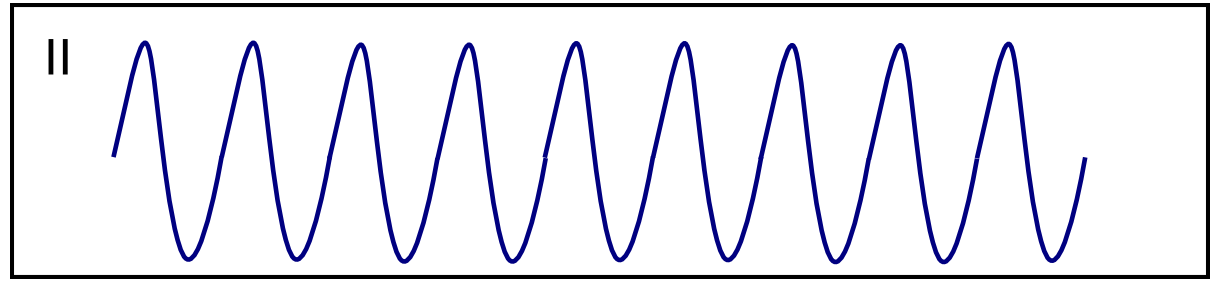 | |
| Asystole [18][19] |
|
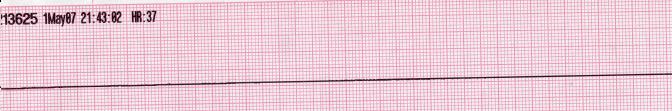 | |
| Pulseless electrical activity [21][22] |
|
|
 |
| Torsade de Pointes [24][25][26] |
|
 |
References
- ↑ Calvo Cuervo D (2023). "Comment on the ESC Guidelines 2022 for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death". Eur Cardiol. 18: e01. doi:10.15420/ecr.2022.48. PMC 9947934 Check
|pmc=value (help). PMID 36844932 Check|pmid=value (help). - ↑ Priori, Silvia G.; Blomström-Lundqvist, Carina; Mazzanti, Andrea; Blom, Nico; Borggrefe, Martin; Camm, John; Elliott, Perry Mark; Fitzsimons, Donna; Hatala, Robert; Hindricks, Gerhard; Kirchhof, Paulus; Kjeldsen, Keld; Kuck, Karl-Heinz; Hernandez-Madrid, Antonio; Nikolaou, Nikolaos; Norekvål, Tone M.; Spaulding, Christian; Van Veldhuisen, Dirk J. (2015). "2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death". European Heart Journal. 36 (41): 2793–2867. doi:10.1093/eurheartj/ehv316. ISSN 0195-668X.
- ↑ Ajijola, Olujimi A.; Tung, Roderick; Shivkumar, Kalyanam (2014). "Ventricular tachycardia in ischemic heart disease substrates". Indian Heart Journal. 66: S24–S34. doi:10.1016/j.ihj.2013.12.039. ISSN 0019-4832.
- ↑ Meja Lopez, Eliany; Malhotra, Rohit (2019). "Ventricular Tachycardia in Structural Heart Disease". Journal of Innovations in Cardiac Rhythm Management. 10 (8): 3762–3773. doi:10.19102/icrm.2019.100801. ISSN 2156-3977.
- ↑ Coughtrie, Abigail L; Behr, Elijah R; Layton, Deborah; Marshall, Vanessa; Camm, A John; Shakir, Saad A W (2017). "Drugs and life-threatening ventricular arrhythmia risk: results from the DARE study cohort". BMJ Open. 7 (10): e016627. doi:10.1136/bmjopen-2017-016627. ISSN 2044-6055.
- ↑ El-Sherif, Nabil (2001). "Mechanism of Ventricular Arrhythmias in the Long QT Syndrome: On Hermeneutics". Journal of Cardiovascular Electrophysiology. 12 (8): 973–976. doi:10.1046/j.1540-8167.2001.00973.x. ISSN 1045-3873.
- ↑ de Riva, Marta; Watanabe, Masaya; Zeppenfeld, Katja (2015). "Twelve-Lead ECG of Ventricular Tachycardia in Structural Heart Disease". Circulation: Arrhythmia and Electrophysiology. 8 (4): 951–962. doi:10.1161/CIRCEP.115.002847. ISSN 1941-3149.
- ↑ ECG found in of https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Koplan BA, Stevenson WG (March 2009). "Ventricular tachycardia and sudden cardiac death". Mayo Clin. Proc. 84 (3): 289–97. doi:10.1016/S0025-6196(11)61149-X. PMC 2664600. PMID 19252119.
- ↑ Maury P, Sacher F, Rollin A, Mondoly P, Duparc A, Zeppenfeld K, Hascoet S (May 2017). "Ventricular arrhythmias and sudden death in tetralogy of Fallot". Arch Cardiovasc Dis. 110 (5): 354–362. doi:10.1016/j.acvd.2016.12.006. PMID 28222965.
- ↑ Saumarez RC, Camm AJ, Panagos A, Gill JS, Stewart JT, de Belder MA, Simpson IA, McKenna WJ (August 1992). "Ventricular fibrillation in hypertrophic cardiomyopathy is associated with increased fractionation of paced right ventricular electrograms". Circulation. 86 (2): 467–74. doi:10.1161/01.cir.86.2.467. PMID 1638716.
- ↑ Bektas, Firat; Soyuncu, Secgin (2012). "Hypokalemia-induced Ventricular Fibrillation". The Journal of Emergency Medicine. 42 (2): 184–185. doi:10.1016/j.jemermed.2010.05.079. ISSN 0736-4679.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ Thies, Karl-Christian; Boos, Karin; Müller-Deile, Kai; Ohrdorf, Wolfgang; Beushausen, Thomas; Townsend, Peter (2000). "Ventricular flutter in a neonate—severe electrolyte imbalance caused by urinary tract infection in the presence of urinary tract malformation". The Journal of Emergency Medicine. 18 (1): 47–50. doi:10.1016/S0736-4679(99)00161-4. ISSN 0736-4679.
- ↑ Koster, Rudolph W.; Wellens, Hein J.J. (1976). "Quinidine-induced ventricular flutter and fibrillation without digitalis therapy". The American Journal of Cardiology. 38 (4): 519–523. doi:10.1016/0002-9149(76)90471-9. ISSN 0002-9149.
- ↑ Dhurandhar RW, Nademanee K, Goldman AM (1978). "Ventricular tachycardia-flutter associated with disopyramide therapy: a report of three cases". Heart Lung. 7 (5): 783–7. PMID 250503.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ ACLS: Principles and Practice. p. 71-87. Dallas: American Heart Association, 2003. ISBN 0-87493-341-2.
- ↑ ACLS for Experienced Providers. p. 3-5. Dallas: American Heart Association, 2003. ISBN 0-87493-424-9.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page
- ↑ "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest." Circulation 2005; 112: IV-58 - IV-66.
- ↑ Foster B, Twelve Lead Electrocardiography, 2nd edition, 2007
- ↑ ECG found in wikimedia Commons
- ↑ Li M, Ramos LG (July 2017). "Drug-Induced QT Prolongation And Torsades de Pointes". P T. 42 (7): 473–477. PMC 5481298. PMID 28674475.
- ↑ Sharain, Korosh; May, Adam M.; Gersh, Bernard J. (2015). "Chronic Alcoholism and the Danger of Profound Hypomagnesemia". The American Journal of Medicine. 128 (12): e17–e18. doi:10.1016/j.amjmed.2015.06.051. ISSN 0002-9343.
- ↑ Khan IA (2001). "Twelve-lead electrocardiogram of torsades de pointes". Tex Heart Inst J. 28 (1): 69. PMC 101137. PMID 11330748.
- ↑ ECG found in https://en.ecgpedia.org/index.php?title=Main_Page