Aripiprazole (intramuscular)
{{DrugProjectFormSinglePage |authorTag=Martin Nino [1] |genericName=Aripiprazole lauroxil |aOrAn=an |drugClass=atypical antipsychotic |indicationType=treatment |indication=patients with schizophrenia |adverseReactions=akathisia (≥5%) |hasBlackBoxWarning=Yes |blackBoxWarningTitle=WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS |blackBoxWarningBody= Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. ARISTADA is not approved for the treatment of patients with dementia-related psychosis. |fdaLIADAdult=
Indications
ARISTADA is indicated for treatment of schizophrenia.
Dosage
- Treatment of Schizophrenia
- ARISTADA is only to be administered as an intramuscular injection by a healthcare professional. For patients who have never taken aripiprazole, establish tolerability with oral aripiprazole prior to initiating treatment with ARISTADA. Due to the half-life of oral aripiprazole, it may take up to 2 weeks to fully assess tolerability. Refer to the prescribing information of oral aripiprazole for the recommended dosage and administration of the oral formulation.
- Depending on individual patient's needs, treatment with ARISTADA can be initiated at a dose of 441 mg, 662 mg or 882 mg administered monthly, which corresponds to 300 mg, 450 mg and 600 mg of aripiprazole, respectively. Treatment may also be initiated with the 882 mg dose every 6 weeks.
- Administer ARISTADA either in the deltoid muscle (441 mg dose only) or gluteal muscle (441 mg, 662 mg or 882 mg).
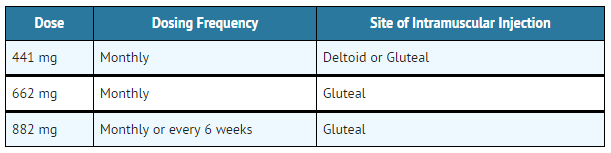
- Table 1: ARISTADA Dosing Frequency and Site of Injection
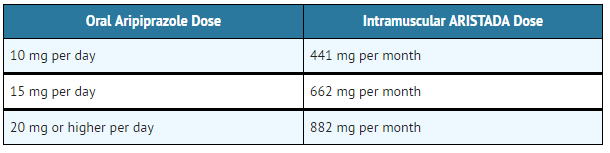
- Use the following ARISTADA doses for patients who are stabilized on oral aripiprazole, as shown in TABLE 2.
- Table 2: ARISTADA Doses Based on Oral Aripiprazole Total Daily Dose
- In conjunction with the first ARISTADA injection, administer treatment with oral aripiprazole for 21 consecutive days.
- Dose may be adjusted as needed. When making dose and dosing interval adjustments, the pharmacokinetics and prolonged-release characteristics of ARISTADA should be considered.
- Missed Doses
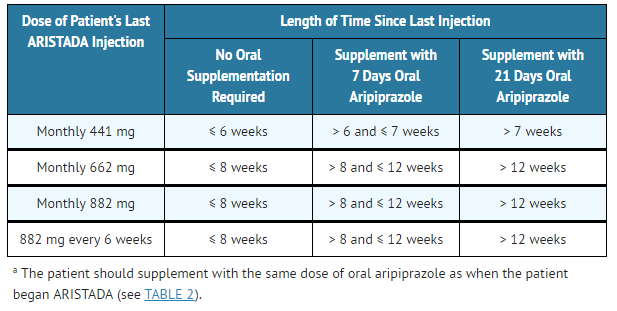
- When a dose is missed, administer the next injection of ARISTADA as soon as possible. If the time elapsed since the last ARISTADA injection exceeds the length of time noted in TABLE 3, use oral aripiprazole supplementation with the next ARISTADA injection as recommended below.
- Table 3: Recommendation for Concomitant Oral Aripiprazole Supplementation Following Missed Doses(a)
ARISTADA: Aripiprazole lauroxil's Brand name
- Early Dosing
- The recommended ARISTADA dosing interval is either monthly for the 441 mg, 662 mg and 882 mg doses or every 6 weeks for 882 mg dose and should be maintained. In the event of early dosing, an ARISTADA injection should not be given earlier than 14 days after the previous injection.
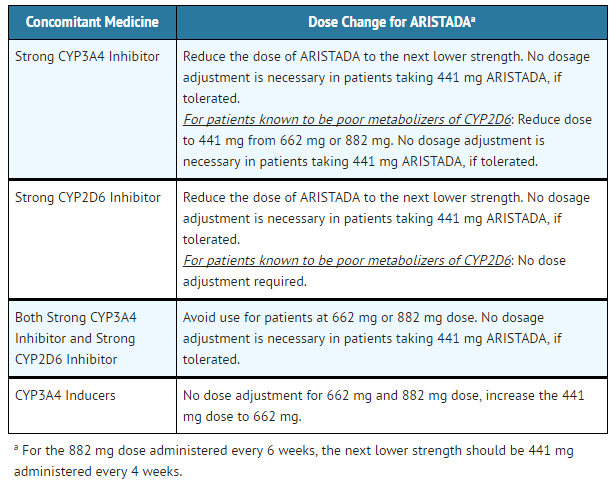
- Dose Adjustments for CYP450 Considerations
- Refer to the prescribing information for oral aripiprazole for recommendations regarding dosage adjustments due to drug interactions, for the first 21 days when the patient is taking oral aripiprazole concomitantly with the first dose of ARISTADA.
- Table 4: ARISTADA Dose Adjustments with Concomitant CYP450 Modulator Use
ARISTADA: Aripiprazole lauroxil's Brand name
|offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Aripiprazole lauroxil in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Aripiprazole lauroxil in adult patients. |fdaLIADPed=Safety and effectiveness of ARISTADA in patients <18 years of age have not been evaluated. |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Aripiprazole lauroxil in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Aripiprazole lauroxil in pediatric patients. |contraindications=ARISTADA is contraindicated in patients with a known hypersensitivity reaction to aripiprazole. Hypersensitivity reactions have ranged from pruritus/urticaria to anaphylaxis. |warnings=
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of 17 placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group.
Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. ARISTADA is not approved for the treatment of patients with dementia-related psychosis.
Cerebrovascular Adverse Reactions, Including Stroke
In placebo-controlled trials with risperidone, aripiprazole, and olanzapine in elderly patients with dementia, there was a higher incidence of cerebrovascular adverse reactions (cerebrovascular accidents and transient ischemic attacks) including fatalities compared to placebo-treated patients. ARISTADA is not approved for the treatment of patients with dementia-related psychosis.
Neuroleptic Malignant Syndrome
A potentially fatal symptom complex sometimes referred to as Neuroleptic Malignant Syndrome (NMS) may occur in association with antipsychotic drugs, including ARISTADA. Clinical manifestations of NMS are hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure.
The diagnostic evaluation of patients with this syndrome is complicated. In arriving at a diagnosis, it is important to identify cases in which the clinical presentation includes both serious medical illness (e.g., pneumonia, systemic infection, etc.) and untreated or inadequately treated extrapyramidal signs and symptoms (EPS). Other important considerations in the differential diagnosis include central anticholinergic toxicity, heat stroke, drug fever, and primary central nervous system pathology.
The management of NMS should include: (1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; (2) intensive symptomatic treatment and medical monitoring; and (3) treatment of any concomitant serious medical problems for which specific treatments are available. There is no general agreement about specific pharmacological treatment regimens for uncomplicated NMS.
If a patient appears to require antipsychotic drug treatment after recovery from NMS, reintroduction of drug therapy should be closely monitored, since recurrences of NMS have been reported.
Tardive Dyskinesia
A syndrome of potentially irreversible, involuntary, dyskinetic movements may develop in patients treated with antipsychotic drugs. Although the prevalence of the syndrome appears to be highest among the elderly, especially elderly women, it is impossible to predict which patients will develop the syndrome. Whether antipsychotic drug products differ in their potential to cause tardive dyskinesia is unknown.
The risk of developing tardive dyskinesia and the likelihood that it will become irreversible appear to increase as the duration of treatment and the total cumulative dose of antipsychotic drugs administered to the patient increase, but the syndrome can develop after relatively brief treatment periods at low doses, although this is uncommon.
There is no known treatment for established tardive dyskinesia, although the syndrome may remit, partially or completely, if antipsychotic treatment is withdrawn. Antipsychotic treatment itself may suppress (or partially suppress) the signs and symptoms of the syndrome and may thus mask the underlying process. The effect of symptomatic suppression on the long-term course of the syndrome is unknown.
Given these considerations, ARISTADA should be prescribed in a manner that is most likely to minimize the occurrence of tardive dyskinesia. Chronic antipsychotic treatment should generally be reserved for patients who suffer from a chronic illness that is known to respond to antipsychotic drugs. In patients who do require chronic treatment, the smallest dose and the shortest duration of treatment producing a satisfactory clinical response should be sought. The need for continued treatment should be reassessed periodically.
If signs and symptoms of tardive dyskinesia appear in a patient treated with ARISTADA drug discontinuation should be considered. However, some patients may require treatment with ARISTADA despite the presence of the syndrome.
Metabolic Changes
Atypical antipsychotic drugs have been associated with metabolic changes that include hyperglycemia/diabetes mellitus, dyslipidemia, and weight gain. While all drugs in the class have been shown to produce some metabolic changes, each drug has its own specific risk profile.
- Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with oral aripiprazole. Assessment of the relationship between atypical antipsychotic use and glucose abnormalities is complicated by the possibility of an increased background risk of diabetes mellitus in patients with schizophrenia and the increasing incidence of diabetes mellitus in the general population. Given these confounders, the relationship between atypical antipsychotic use and hyperglycemia-related adverse events is not completely understood. However, epidemiological studies suggest an increased risk of hyperglycemia-related adverse reactions in patients treated with the atypical antipsychotics.
- Patients with an established diagnosis of diabetes mellitus who are started on atypical antipsychotics should be monitored regularly for worsening of glucose control. Patients with risk factors for diabetes mellitus (e.g., obesity, family history of diabetes) who are starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment and periodically during treatment. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients require continuation of anti-diabetic treatment despite discontinuation of the suspect drug.
- In the long-term, open-label schizophrenia study with ARISTADA, 14% of patients with normal hemoglobin A1c (<5.7%) at baseline developed elevated levels (≥5.7%) post-baseline.
- Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.
- In the long-term, open-label schizophrenia study with ARISTADA, shifts in baseline fasting total cholesterol from normal (<200 mg/dL) to high (≥240 mg/dL) were reported in 1% of patients; shifts in baseline fasting LDL cholesterol from normal (<100 mg/dL) to high (≥160 mg/dL) were reported in 1% of patients; and shifts in baseline fasting triglycerides from normal (<150 mg/dL) to high (≥200 mg/dL) were reported in 8% of patients. In the same study, shifts in baseline fasting total cholesterol from borderline (≥ 200 mg/dL and <240 mg/dL) to high (≥240 mg/dL) were reported in 15% of patients; shifts in baseline fasting LDL cholesterol from borderline (≥100 mg/dL and <160 mg/dL) to high (≥160 mg/dL) were reported in 8% of patients; and shifts in baseline fasting triglycerides from borderline (≥150 mg/dL and <200 mg/dL) to high (≥200 mg/dL) were reported in 35% of patients. In addition, the proportion of patients with shifts in fasting HDL cholesterol from normal (≥40 mg/dL) to low (<40 mg/dL) was reported in 15% of patients.
- Weight Gain
- Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
- The proportion of adult patients with weight gain ≥7% of body weight is presented in TABLE 6.
- Table 6: Proportion of Adult Patients with Shifts in Weight in the 12-Week, Placebo-Controlled, Fixed-Dose Schizophrenia Trial
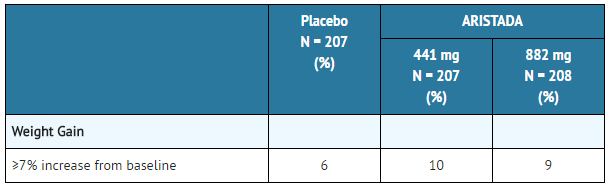
ARISTADA: Aripiprazole lauroxil's Brand name
Pathological Gambling and Other Compulsive Behaviors
Post-marketing case reports suggest that patients can experience intense urges, particularly for gambling, and the inability to control these urges while taking aripiprazole. Other compulsive urges, reported less frequently include: sexual urges, shopping, eating or binge eating, and other impulsive or compulsive behaviors. Because patients may not recognize these behaviors as abnormal, it is important for prescribers to ask patients or their caregivers specifically about the development of new or intense gambling urges, compulsive sexual urges, compulsive shopping, binge or compulsive eating, or other urges while being treated with aripiprazole. It should be noted that impulse-control symptoms can be associated with the underlying disorder. In some cases, although not all, urges were reported to have stopped when the dose was reduced or the medication was discontinued. Compulsive behaviors may result in harm for the patient and others if not recognized. Consider dose reduction or stopping the medication if a patient develops such urges.
Orthostatic Hypotension
Aripiprazole may cause orthostatic hypotension, perhaps due to its α1-adrenergic receptor antagonism. Associated adverse reactions related to orthostatic hypotension can include dizziness, lightheadedness and tachycardia. Generally, these risks are greatest at the beginning of treatment and during dose escalation. Patients at increased risk of these adverse reactions or at increased risk of developing complications from hypotension include those with dehydration, hypovolemia, treatment with antihypertensive medication, history of cardiovascular disease (e.g., heart failure, myocardial infarction, ischemia, or conduction abnormalities), history of cerebrovascular disease, as well as patients who are antipsychotic-naïve. In such patients, consider using a lower starting dose, and monitor orthostatic vital signs.
Orthostatic hypotension was reported for one patient in the ARISTADA 882 mg group (0.5%) and no patients in the ARISTADA 441 mg and placebo groups in the 12-week schizophrenia efficacy study. In the long-term open-label schizophrenia study, orthostatic hypotension was reported for 1 (0.2%) patient treated with ARISTADA. Orthostatic hypotension was defined as a decrease in systolic blood pressure ≥20 mmHg accompanied by an increase in heart rate ≥25 bpm when comparing standing to supine values.
Leukopenia, Neutropenia, and Agranulocytosis
In clinical trials and/or postmarketing experience, events of leukopenia and neutropenia have been reported temporally related to antipsychotic agents. Agranulocytosis has also been reported.
Possible risk factors for leukopenia/neutropenia include pre-existing low white blood cell count (WBC)/absolute neutrophil count (ANC) and history of drug-induced leukopenia/neutropenia. In patients with a history of a clinically significant low WBC/ANC or drug-induced leukopenia/neutropenia, perform a complete blood count (CBC) frequently during the first few months of therapy. In such patients, consider discontinuation of ARISTADA at the first sign of a clinical significant decline in WBC in the absence of other causative factors.
Monitor patients with clinically significant neutropenia for fever or other symptoms or signs of infection and treat promptly if such symptoms or signs occur. Discontinue ARISTADA in patients with severe neutropenia (absolute neutrophil count <1000/mm3) and follow their WBC until recovery.
Seizures
As with other antipsychotic drugs, use ARISTADA cautiously in patients with a history of seizures or with conditions that lower the seizure threshold. Conditions that lower the seizure threshold may be more prevalent in a population of 65 years or older.
Potential for Cognitive and Motor Impairment
ARISTADA, like other antipsychotics, has the potential to impair judgment, thinking or motor skills. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are reasonably certain that therapy with ARISTADA does not affect them adversely.
Body Temperature Regulation
Disruption of the body's ability to reduce core body temperature has been attributed to antipsychotic agents. Appropriate care is advised when prescribing ARISTADA for patients who will be experiencing conditions which may contribute to an elevation in core body temperature, (e.g., exercising strenuously, exposure to extreme heat, receiving concomitant medication with anticholinergic activity, or being subject to dehydration).
Dysphagia
Esophageal dysmotility and aspiration have been associated with antipsychotic drug use. ARISTADA and other antipsychotic drugs should be used cautiously in patients at risk for aspiration pneumonia.
|clinicalTrials= The following are discussed in more details in other sections of the labeling:
- Increased Mortality in Elderly Patients with Dementia-related Psychosis
- Cerebrovascular Adverse Reactions, Including Stroke
- Neuroleptic Malignant Syndrome
- Tardive Dyskinesia
- Metabolic Changes
- Pathological Gambling and Other Compulsive Behaviors
- Orthostatic Hypotension
- Leukopenia, Neutropenia, and Agranulocytosis
- Seizures
- Potential for Cognitive and Motor Impairment
- Body Temperature Regulation
- Dysphagia
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
ARISTADA
- Patient Exposure: ARISTADA has been evaluated for safety in 880 adult patients in clinical trials in schizophrenia.
- Commonly Observed Adverse Reactions: The most common adverse reaction (incidence ≥5% and at least twice the rate of placebo in patients treated with ARISTADA) was akathisia.
- Adverse Reactions Occurring at an Incidence of 2% or More in ARISTADA-Treated Patients: Adverse reactions associated with the use of ARISTADA (incidence of 2% or greater, rounded to the nearest percent and ARISTADA incidence greater than placebo) that occurred are shown in TABLE 7.
- Table 7: Adverse Reaction in 2% or More of ARISTADA-Treated Patients and That Occurred at Greater Incidence than in the Placebo-Treated Patients in the 12-Week, Placebo-Controlled, Fixed-Dose Schizophrenia Trial
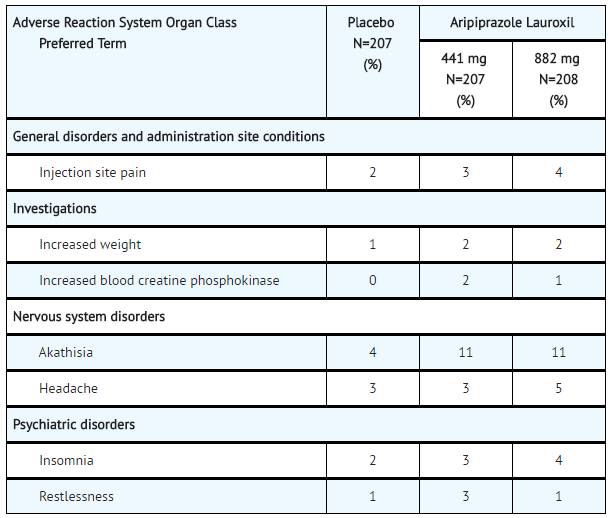
- Injection Site Reactions: Injection site reactions were reported by 4% of patients treated with 441 mg ARISTADA and 5% of patients treated with 882 mg ARISTADA compared to 2% of patients treated with placebo. Most of these were injection site pain (3%, 4% and 2% in the 441 mg ARISTADA, 882 mg ARISTADA and placebo groups, respectively) and most were associated with the first injection, and decreased with each subsequent injection to less than or equal to 1% for both doses of ARISTADA and placebo. Other injection site reactions (induration, swelling and redness) occurred at less than 1%.
- Extrapyramidal Symptoms: In the 12-week schizophrenia efficacy study, for ARISTADA-treated patients, the incidence of other EPS-related events, excluding akathisia and restlessness, was 5% and 7% for patients on 441 mg and 882 mg, respectively, versus 4% for placebo-treated patient (TABLE 8).
- Table 8: Incidence of EPS Compared to Placebo
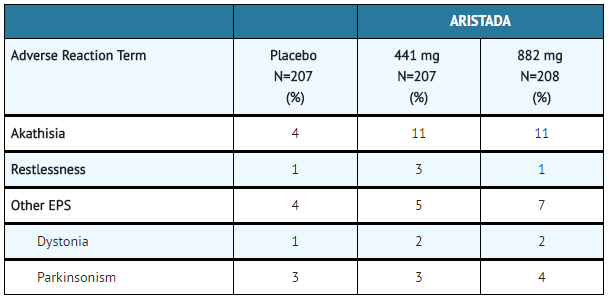
ARISTADA: Aripiprazole lauroxil's Brand name
- Dystonia: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first few days of treatment. Dystonic symptoms include: spasm of the neck muscles, sometimes progressing to tightness of the throat, swallowing difficulty, difficulty breathing, and/or protrusion of the tongue. While these symptoms can occur at low doses, they occur more frequently and with greater severity with high potency and at higher doses of first generation antipsychotic drugs. An elevated risk of acute dystonia is observed in males and younger age groups.
- Other Adverse Reactions Observed in Clinical Studies: The following listing does not include reactions: 1) already listed in previous tables or elsewhere in labeling, 2) for which a drug cause was remote, 3) which were so general as to be uninformative, 4) which were not considered to have significant clinical implications, or 5) which occurred at a rate equal to or less than placebo.
- Cardiac – angina pectoris, tachycardia, palpitations
- Gastrointestinal disorders – constipation, dry mouth
- General disorders – asthenia
- Musculoskeletal – muscular weakness
- Nervous system disorders – dizziness
Adverse Reactions Reported in Clinical Trials with Oral Aripiprazole
The following is a list of additional adverse reactions that have been reported in clinical trials with oral aripiprazole and not reported above for ARISTADA.
- Blood and Lymphatic System Disorders: thrombocytopenia
- Eye Disorders: photophobia, diplopia
- Gastrointestinal Disorders: gastroesophageal reflux disease
- General Disorders and Administration Site Conditions: peripheral edema, chest pain, face edema
- Immune System Disorders: hypersensitivity
- Injury, Poisoning, and Procedural Complications: fall, heat stroke
- Investigations: weight decreased, hepatic enzyme increased, blood glucose increased, blood lactate dehydrogenase increased, gamma glutamyl transferase increased, blood prolactin increased, blood urea increased, blood creatinine increased, blood bilirubin increased, electrocardiogram QT prolonged, glycosylated hemoglobin increased
- Metabolism and Nutrition Disorders: anorexia, hypokalemia, hyponatremia, hypoglycemia
- Musculoskeletal and Connective Tissue Disorders: muscle tightness, rhabdomyolysis, mobility decreased
- Nervous System Disorders: memory impairment, cogwheel rigidity, hypokinesia, myoclonus, bradykinesia, akinesia, myoclonus, coordination abnormal, speech disorder, choreoathetosis
- Psychiatric Disorders: aggression, loss of libido, delirium, libido increased, anorgasmia, tic, homicidal ideation, catatonia, sleep walking
- Renal and Urinary Disorders: urinary retention, nocturia
- Reproductive System and Breast Disorders: erectile dysfunction, gynaecomastia, menstruation irregular, amenorrhea, breast pain, priapism
- Respiratory, Thoracic, and Mediastinal Disorders: nasal congestion, dyspnea
- Skin and Subcutaneous Tissue Disorders: rash, hyperhidrosis, pruritus, photosensitivity reaction, alopecia, urticaria
- Vascular Disorders: hypotension, hypertension
|postmarketing=The following adverse reactions have been identified during post-approval use of oral aripiprazole. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or to establish a causal relationship to drug exposure: occurrences of allergic reaction (anaphylactic reaction, angioedema, laryngospasm, pruritus/urticaria, or oropharyngeal spasm), pathological gambling, hiccups and blood glucose fluctuation. |drugInteractions=
Drugs Having Clinically Important Interactions with ARISTADA
- Table 9: Clinically Important Drug Interactions with ARISTADA
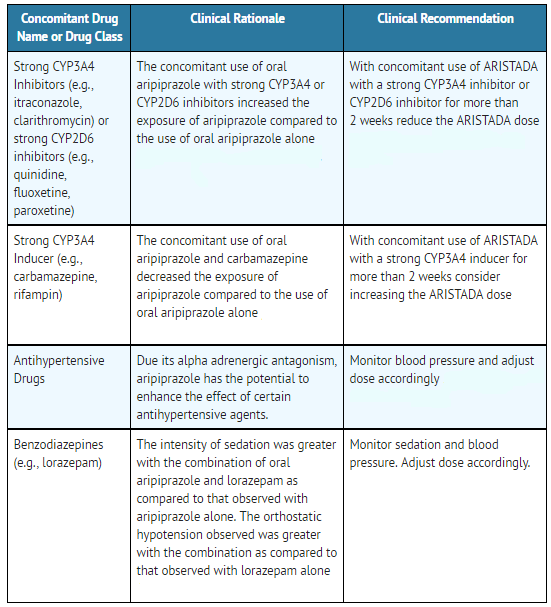
ARISTADA: Aripiprazole lauroxil's Brand name
Drugs Having No Clinically Important Interactions with ARISTADA
Based on pharmacokinetic studies with oral aripiprazole, no dosage adjustment of ARISTADA is required when administered concomitantly with famotidine, valproate, lithium.
In addition, no dosage adjustment is necessary for substrates of CYP2D6 (e.g., dextromethorphan, fluoxetine, paroxetine, or venlafaxine), CYP2C9 (e.g., warfarin), CYP2C19 (e.g., omeprazole, warfarin, escitalopram), or CYP3A4 (e.g., dextromethorphan) when co-administered with ARISTADA. Additionally, no dosage adjustment is necessary for valproate, lithium, lamotrigine, or sertraline when co-administered with ARISTADA.
|FDAPregCat= |useInPregnancyFDA=
- Pregnancy Exposure Registry
- There is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to ARISTADA during pregnancy. For more information, contact the National Pregnancy Registry for Atypical Antipsychotics at 1-866-961-2388 or visit http://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/ .
- Risk Summary
- Neonates exposed to antipsychotic drugs during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms following delivery. Limited published data on aripiprazole use in pregnant women are not sufficient to inform any drug-associated risks for birth defects or miscarriage. No teratogenicity was observed in animal reproductive studies with intramuscular administration of aripiprazole lauroxil to rats and rabbits during organogenesis at doses up to 6 and 18 times, respectively, the maximum recommended human dose (MRHD) of 882 mg based on body surface area (mg/m2). However, aripiprazole caused developmental toxicity and possible teratogenic effects in rats and rabbits. The background risk of major birth defects and miscarriage for the indicated population are unknown. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively. Advise pregnant women of the potential risk to a fetus.
- Clinical Considerations
- Fetal/Neonatal Adverse Reactions
- Extrapyramidal and/or withdrawal symptoms, including agitation, hypertonia, hypotonia, tremor, somnolence, respiratory distress and feeding disorder have been reported in neonates who were exposed to antipsychotic drugs during the third trimester of pregnancy. These symptoms have varied in severity. Monitor neonates for extrapyramidal and/or withdrawal symptoms and manage symptoms appropriately. Some neonates recover within hours or days without specific treatment; others required prolonged hospitalization.
- Data
- Animal Data for Aripiprazole Lauroxil
- Aripiprazole lauroxil did not cause adverse developmental or maternal effects in rats or rabbits when administered intramuscularly during the period of organogenesis at doses of 18, 49, or 144 mg/animal in pregnant rats which are approximately 0.7 to 6 times the maximum recommended human dose (MRHD) of 882 mg on mg/m2 basis, and at doses of 241, 723, and 2893 mg/animal in pregnant rabbits which are approximately 1 to 18 times the MRHD on mg/m2 basis. However, aripiprazole caused developmental toxicity and possible teratogenic effects in rats and rabbits.
- Animal Data for Aripiprazole
- Pregnant rats were treated with oral doses of 3, 10, and 30 mg/kg/day which are approximately 1 to 10 times the oral maximum recommended human dose [MRHD] of 30 mg/day on mg/m2 basis of aripiprazole during the period of organogenesis. Treatment at the highest dose caused a slight prolongation of gestation and delay in fetal development, as evidenced by decreased fetal weight, and undescended testes. Delayed skeletal ossification was observed at 3 and 10 times the oral MRHD on mg/m2 basis.
- At 3 and 10 times the oral MRHD on mg/m2 basis, delivered offspring had decreased body weights. Increased incidences of hepatodiaphragmatic nodules and diaphragmatic hernia were observed in offspring from the highest dose group (the other dose groups were not examined for these findings). A low incidence of diaphragmatic hernia was also seen in the fetuses exposed to the highest dose. Postnatally, delayed vaginal opening was seen at 3 and 10 times the oral MRHD on mg/m2 basis and impaired reproductive performance (decreased fertility rate, corpora lutea, implants, live fetuses, and increased post-implantation loss, likely mediated through effects on female offspring) along with some maternal toxicity were seen at the highest dose; however, there was no evidence to suggest that these developmental effects were secondary to maternal toxicity.
- In pregnant rabbits treated with oral doses of 10, 30, and 100 mg/kg/day which are 2 to 11 times human exposure at the oral MRHD based on AUC and 6 to 65 times the oral MRHD on mg/m2 basis of aripiprazole during the period of organogenesis decreased maternal food consumption and increased abortions were seen at the highest dose as well as increased fetal mortality. Decreased fetal weight and increased incidence of fused sternebrae were observed at 3 and 11 times the oral MRHD based on AUC.
- In rats treated with oral doses of 3, 10, and 30 mg/kg/day which are 1 to 10 times the oral MRHD on mg/m2 basis of aripiprazole perinatally and postnatally (from day 17 of gestation through day 21 postpartum), slight maternal toxicity and slightly prolonged gestation were seen at the highest dose. An increase in stillbirths and decreases in pup weight (persisting into adulthood) and survival were also seen at this dose.
|useInNursing=Aripiprazole is present in human breast milk; however, there are insufficient data to assess the amount in human milk, the effects on the breastfed infant, or the effects on milk production. The development and health benefits of breastfeeding should be considered along with the mother's clinical need for ARISTADA and any potential adverse effects on the breastfed infant from ARISTADA or from the underlying maternal condition. |useInPed=Safety and effectiveness of ARISTADA in patients <18 years of age have not been evaluated. |useInGeri=Safety and effectiveness of ARISTADA in patients >65 years of age have not been evaluated. |useInRenalImpair=No dosage adjustment for ARISTADA is required based on a patient's renal function (mild to severe renal impairment, glomerular filtration rate between 15 and 90 mL/minute). |useInHepaticImpair=No dosage adjustment for ARISTADA is required based on a patient's hepatic function (mild to severe hepatic impairment, Child-Pugh score between 5 and 15).
|othersTitle=CYP2D6 Poor Metabolizers
|useInOthers=Dosage adjustment is recommended in known CYP2D6 poor metabolizers due to high aripiprazole concentrations. Approximately 8% of Caucasians and 3-8% of Black/African Americans cannot metabolize CYP2D6 substrates and are classified as poor metabolizers (PM).
|othersTitle=Other Specific Populations
|useInOthers=No dosage adjustment for ARISTADA is required on the basis of a patient's sex, race, or smoking status.
|administration=
- Instructions for Use
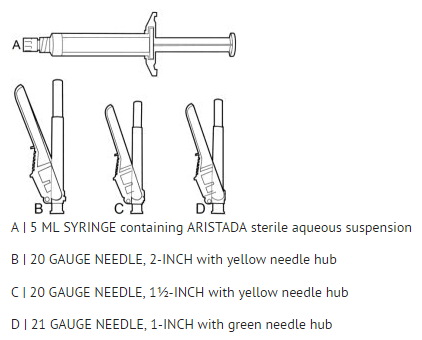
- The kit contains a syringe containing ARISTADA sterile aqueous suspension and 2 or 3 safety needles depending on dose (a 2-inch 20 gauge needle with yellow needle hub, a 1 ½-inch 20 gauge needle with yellow needle hub, and a 1-inch 21 gauge needle with green needle hub (441 mg kit only)) for intramuscular injection. All materials should be stored at room temperature.
ARISTADA: Aripiprazole lauroxil's Brand name
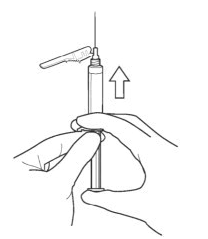
- 1. TAP and SHAKE the syringe.

- 1a. Tap the syringe at least 10 times to dislodge any material which may have settled.
- 1b. Shake the syringe vigorously for a minimum of 30 seconds to ensure a uniform suspension. If the syringe is not used within 15 minutes, shake again for 30 seconds.
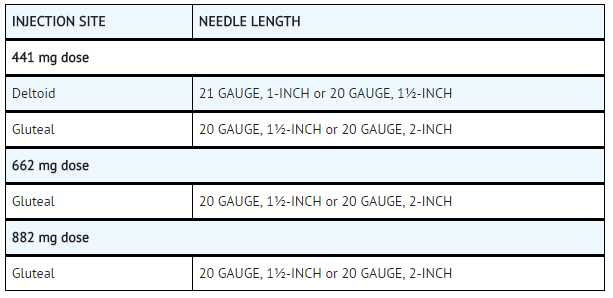
- 2. SELECT the injection needle.
- 2a. Select injection site.
- 2b. Select needle length based on injection site. For patients with a larger amount of subcutaneous tissue overlaying the injection site muscle, use the longer of the needles provided.
- Table 5: Injection Site and Associated Needle Length
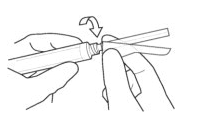
- 3. ATTACH the injection needle.
- Attach the appropriate needle securely with a clockwise twisting motion. Do NOT overtighten. Overtightening could lead to needle hub cracking.
- 4. PRIME the syringe to remove air.
- 4a. Bring the syringe into upright position and tap the syringe to bring air to the top.
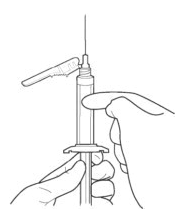
- 4b. Remove air by depressing the plunger rod. A few drops of suspension will be released.
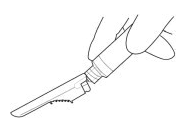
- 5. ADMINISTER the entire content intramuscularly. Do not inject by any other route. Inject in a rapid and continuous manner (less than 10 seconds).
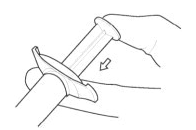
- 6. DISPOSE of the needle. Cover the needle by pressing the safety device. Dispose of used and unused items in a proper waste container.
|overdose=
- Human Experience
- The largest known case of acute ingestion with a known outcome involved 1260 mg of oral aripiprazole (42 times the maximum recommended daily dose) in a patient who fully recovered.
- Common adverse reactions (reported in at least 5% of all overdose cases) reported with oral aripiprazole overdosage (alone or in combination with other substances) include vomiting, somnolence, and tremor. Other clinically important signs and symptoms observed in one or more patients with aripiprazole overdoses (alone or with other substances) include acidosis, aggression, aspartate aminotransferase increased, atrial fibrillation, bradycardia, coma, confusional state, convulsion, blood creatine phosphokinase increased, depressed level of consciousness, hypertension, hypokalemia, hypotension, lethargy, loss of consciousness, QRS complex prolonged, QT prolonged, pneumonia aspiration, respiratory arrest, status epilepticus, and tachycardia.
- Management of Overdosage
- In case of overdosage, call the Poison control center immediately at 1-800-222-1222.
|drugBox=
Aripiprazole (intramuscular)
| |
| Systematic (IUPAC) name | |
| ? | |
| Identifiers | |
| CAS number | ? |
| ATC code | ? |
| PubChem | ? |
| Chemical data | |
| Formula | ? |
| Mol. mass | ? |
| Pharmacokinetic data | |
| Bioavailability | ? |
| Metabolism | ? |
| Half life | ? |
| Excretion | ? |
| Therapeutic considerations | |
| Pregnancy cat. |
? |
| Legal status | |
| Routes | ? |