Guanfacine: Difference between revisions
(Created page with "{{DrugProjectFormSinglePage |authorTag={{SS}} |genericName=Guanfacine |aOrAn=a |drugClass=Central alpha-2 Adrenergic Agonist |indication=hypertension |adverseReactions=O...") |
m (Protected "Guanfacine": Bot: Protecting all pages from category Drug ([Edit=Allow only administrators] (indefinite) [Move=Allow only administrators] (indefinite))) |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{DrugProjectFormSinglePage | {{DrugProjectFormSinglePage | ||
|authorTag={{SS}} | |authorTag={{SS}}; {{AJ}} | ||
|genericName=Guanfacine | |genericName=Guanfacine | ||
|aOrAn=a | |aOrAn=a | ||
|drugClass= | |drugClass=[[Alpha-2 adrenergic receptor|central alpha-2 adrenergic agonist]] | ||
|indicationType=treatment | |||
|indication=[[hypertension]] | |indication=[[hypertension]] | ||
|adverseReactions=[[ | |adverseReactions=[[orthostatic hypotension]], [[abdominal pain]], [[constipation]], [[xerostomia]], [[dizziness]], [[headache]], [[insomnia]], [[somnolence]], [[impotence]], [[fatigue]] | ||
|blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | |blackBoxWarningTitle=<b><span style="color:#FF0000;">TITLE</span></b> | ||
|blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | |blackBoxWarningBody=<i><span style="color:#FF0000;">Condition Name:</span></i> (Content) | ||
| Line 12: | Line 13: | ||
* Dosing information | * Dosing information | ||
:* Recommended initial dosage: '''1 mg/day''' given at bedtime to minimize somnolence. | :* Recommended initial dosage: '''1 mg/day''' given at bedtime to minimize [[somnolence]]. | ||
::* If after 3 to 4 weeks of therapy, 1 mg does not give a satisfactory result, a dose of '''2 mg''' may be given | ::* If after 3 to 4 weeks of therapy, 1 mg does not give a satisfactory result, a dose of '''2 mg''' may be given | ||
::* Higher daily doses have been used, but adverse reactions increase significantly with doses above '''3 mg/day.''' | ::* Higher daily doses have been used, but adverse reactions increase significantly with doses above '''3 mg/day.''' | ||
* The frequency of [[rebound hypertension]] is low, but it can occur. When rebound occurs, it does so after 2-4 days, which is delayed compared with [[clonidine]] hydrochloride. This is consistent with the longer half-life of guanfacine. In most cases, after abrupt withdrawal of guanfacine, blood pressure returns to pretreatment levels slowly (within 2-4 days) without ill effects. | * The frequency of [[rebound hypertension]] is low, but it can occur. When rebound occurs, it does so after 2-4 days, which is delayed compared with [[clonidine]] [[hydrochloride]]. This is consistent with the longer half-life of guanfacine. In most cases, after abrupt [[withdrawal]] of guanfacine, [[blood pressure]] returns to pretreatment levels slowly (within 2-4 days) without ill effects. | ||
|offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Guanfacine sandbox in adult patients. | |offLabelAdultGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Guanfacine sandbox in adult patients. | ||
|offLabelAdultNoGuideSupport=<h4>Prophylaxis of [[Migraine]]</h4> | |offLabelAdultNoGuideSupport=<h4>Prophylaxis of [[Migraine]]</h4> | ||
| Line 23: | Line 24: | ||
:* Not applicable | :* Not applicable | ||
|fdaLIADPed=FDA Package Insert for Guanfacine contains no information regarding FDA-labeled indications and dosage information for children. | |fdaLIADPed=FDA Package Insert for Guanfacine contains no information regarding FDA-labeled indications and dosage information for children. | ||
|offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Guanfacine sandbox in pediatric patients. | |offLabelPedGuideSupport=There is limited information regarding <i>Off-Label Guideline-Supported Use</i> of Guanfacine sandbox in pediatric patients. | ||
| Line 31: | Line 30: | ||
* Dosing information | * Dosing information | ||
:* Initial dosage: '''0.5 mg''' at bedtime for 3 days, followed by '''0.5 mg''' in the morning and at bedtime for 4 days, and then '''0.5 mg''' in the morning, afternoon, and evening (dose could be adjusted upward by the primary physician, maximum '''4 mg/day''').11431228 | :* Initial dosage: '''0.5 mg''' at bedtime for 3 days, followed by '''0.5 mg''' in the morning and at bedtime for 4 days, and then '''0.5 mg''' in the morning, afternoon, and evening (dose could be adjusted upward by the primary physician, maximum '''4 mg/day''').<ref name="pmid11431228">{{cite journal| author=Scahill L, Chappell PB, Kim YS, Schultz RT, Katsovich L, Shepherd E et al.| title=A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. | journal=Am J Psychiatry | year= 2001 | volume= 158 | issue= 7 | pages= 1067-74 | pmid=11431228 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11431228 }} </ref> | ||
:* '''2-4 mg/day''' 18166547 | :* '''2-4 mg/day''' <ref name="pmid18166547">{{cite journal| author=Biederman J, Melmed RD, Patel A, McBurnett K, Konow J, Lyne A et al.| title=A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. | journal=Pediatrics | year= 2008 | volume= 121 | issue= 1 | pages= e73-84 | pmid=18166547 | doi=10.1542/peds.2006-3695 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=18166547 }} </ref> | ||
:* '''1-4 mg/day''' 19106767,19519256 | :* '''1-4 mg/day''' <ref name="pmid19106767">{{cite journal| author=Sallee FR, McGough J, Wigal T, Donahue J, Lyne A, Biederman J et al.| title=Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial. | journal=J Am Acad Child Adolesc Psychiatry | year= 2009 | volume= 48 | issue= 2 | pages= 155-65 | pmid=19106767 | doi=10.1097/CHI.0b013e318191769e | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19106767 }} </ref>,<ref name="pmid19519256">{{cite journal| author=Sallee FR, Lyne A, Wigal T, McGough JJ| title=Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder. | journal=J Child Adolesc Psychopharmacol | year= 2009 | volume= 19 | issue= 3 | pages= 215-26 | pmid=19519256 | doi=10.1089/cap.2008.0080 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=19519256 }} </ref> | ||
<h4>[[Gilles de la Tourette's syndrome]]</h4> | <h4>[[Gilles de la Tourette's syndrome]]</h4> | ||
| Line 40: | Line 39: | ||
:* '''4/day''' 8567607 | :* '''4/day''' 8567607 | ||
:* Initial dosage: '''0.5 mg''' at bedtime for 3 days, followed by '''0.5 mg''' in the morning and at bedtime for 4 days, and then '''0.5 mg''' in the morning, afternoon, and evening (dose could be adjusted upward by the primary physician, maximum '''4 mg/day''').11431228 | :* Initial dosage: '''0.5 mg''' at bedtime for 3 days, followed by '''0.5 mg''' in the morning and at bedtime for 4 days, and then '''0.5 mg''' in the morning, afternoon, and evening (dose could be adjusted upward by the primary physician, maximum '''4 mg/day''').<ref name="pmid11431228">{{cite journal| author=Scahill L, Chappell PB, Kim YS, Schultz RT, Katsovich L, Shepherd E et al.| title=A placebo-controlled study of guanfacine in the treatment of children with tic disorders and [[attention deficit hyperactivity disorder]]. | journal=Am J Psychiatry | year= 2001 | volume= 158 | issue= 7 | pages= 1067-74 | pmid=11431228 | doi= | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=11431228 }} </ref> | ||
:* '''1.5 mg/day''' 7559307 | :* '''1.5 mg/day''' <ref name="pmid7559307">{{cite journal| author=Chappell PB, Riddle MA, Scahill L, Lynch KA, Schultz R, Arnsten A et al.| title=Guanfacine treatment of comorbid attention-deficit hyperactivity disorder and Tourette's syndrome: preliminary clinical experience. | journal=J Am Acad Child Adolesc Psychiatry | year= 1995 | volume= 34 | issue= 9 | pages= 1140-6 | pmid=7559307 | doi=10.1097/00004583-199509000-00010 | pmc= | url=http://www.ncbi.nlm.nih.gov/entrez/eutils/elink.fcgi?dbfrom=pubmed&tool=sumsearch.org/cite&retmode=ref&cmd=prlinks&id=7559307 }} </ref> | ||
|contraindications=Patients with a history of [[hypersensitivity]] to Guanfacine®, its inactive ingredients [see Description (11)] or other products containing guanfacine should not take Guanfacine® | |||
|contraindications=Patients with a history of [[hypersensitivity]] to | |warnings====General==== | ||
|warnings====General=== | |||
Like other antihypertensive agents, | Like other [[antihypertensive agents]], Guanfacine (guanfacine hydrochloride) should be used with caution in patients with severe coronary insufficiency, recent [[myocardial infarction]], [[Cerebrovascular Disease|cerebrovascular disease]], or [[Chronic renal failure|chronic renal]] or [[hepatic failure]]. | ||
===Sedation=== | ===Sedation=== | ||
Guanfacine, like other orally active [[Adrenergic agonists|central α2-adrenergic agonists]], causes [[sedation]] or [[drowsiness]], especially when beginning therapy. These symptoms are dose-related. When Guanfacine is used with other centrally active depressants (such as [[phenothiazines]], [[barbiturates]], or [[benzodiazepines]]), the potential for additive [[sedative]] effects should be considered. | |||
===Rebound=== | ===Rebound=== | ||
Abrupt cessation of therapy with orally active central α2-adrenergic agonists may be associated with increases (from depressed on-therapy levels) in plasma and urinary | Abrupt cessation of therapy with orally active [[Adrenergic agonists|central α2-adrenergic agonists]] may be associated with increases (from depressed on-therapy levels) in [[plasma]] and urinary catecholamines]], symptoms of "[[nervousness]] and [[anxiety]]" and, less commonly, increases in [[blood pressure]] to levels significantly greater than those prior to therapy. | ||
===Information for Patients=== | ===Information for Patients=== | ||
Patients who receive | Patients who receive Guanfacine should be advised to exercise caution when operating dangerous machinery or driving motor vehicles until it is determined that they do not become [[drowsy]] or [[dizzy]] from the medication. Patients should be warned that their tolerance for alcohol and other [[CNS depressant|CNS depressants]] may be diminished. Patients should be advised not to discontinue therapy abruptly. | ||
===Laboratory Tests=== | ===Laboratory Tests=== | ||
In clinical trials, no clinically relevant laboratory test abnormalities were identified as causally related to drug during short-term treatment with | In [[clinical trials]], no clinically relevant laboratory test abnormalities were identified as causally related to drug during short-term treatment with Guanfacine (guanfancine hydrochloride). | ||
|clinicalTrials=Adverse reactions noted with | |clinicalTrials=Adverse reactions noted with Guanfacine (guanfacine hydrochloride) are similar to those of other drugs of the central α2-adrenoreceptor agonist class: [[dry mouth]], [[sedation]] ([[somnolence]]), [[weakness]] ([[asthenia]]), [[dizziness]], [[constipation]], and [[impotence]]. While the reactions are common, most are mild and tend to disappear on continued dosing. | ||
[[Skin rash]] with exfoliation has been reported in a few cases; although clear cause and effect relationships to Guanfacine could not be established, should a [[rash]] occur, Guanfacine should be discontinued and the patient monitored appropriately. | |||
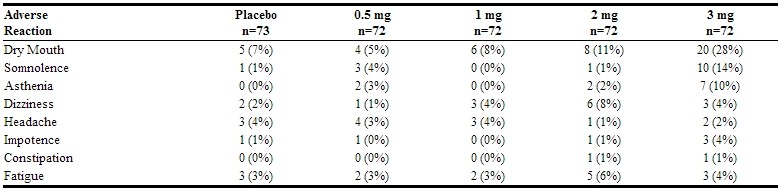
In the dose-response monotherapy study described under CLINICAL PHARMACOLOGY, the frequency of the most commonly observed adverse reactions showed a dose relationship from 0.5 to 3 mg as follows: | In the dose-response monotherapy study described under CLINICAL PHARMACOLOGY, the frequency of the most commonly observed adverse reactions showed a dose relationship from 0.5 to 3 mg as follows: | ||
[[File:TENEX01.jpg|thumb| | [[File:TENEX01.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
name="Table_4" style="color: rgb(0, 0, 0); font-family: 'Arial Unicode MS'; font-size: 16px; font-style: normal; font-variant: normal; font-weight: normal; letter-spacing: normal; line-height: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-stroke-width: 0px; background-color: rgb(255, 255, 255);" | name="Table_4" style="color: rgb(0, 0, 0); font-family: 'Arial Unicode MS'; font-size: 16px; font-style: normal; font-variant: normal; font-weight: normal; letter-spacing: normal; line-height: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-stroke-width: 0px; background-color: rgb(255, 255, 255);" | ||
| Line 73: | Line 71: | ||
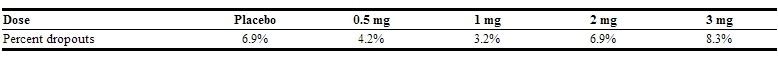
The percent of patients who dropped out because of adverse reactions are shown below for each dosage group. | The percent of patients who dropped out because of adverse reactions are shown below for each dosage group. | ||
[[File:TENEX02.jpg|thumb| | [[File:TENEX02.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
The most common reasons for dropouts among patients who received guanfacine were dry mouth, [[somnolence]], [[dizziness]], [[fatigue]], [[weakness]], and [[constipation]]. | The most common reasons for dropouts among patients who received guanfacine were dry mouth, [[somnolence]], [[dizziness]], [[fatigue]], [[weakness]], and [[constipation]]. | ||
In the 12-week, placebo-controlled, dose-response study of guanfacine administered with 25 mg [[chlorthalidone]] at bedtime, the frequency of the most commonly observed adverse reactions showed a clear dose relationship from 0.5 to 3 mg as follows: | In the 12-week, [[placebo]]-controlled, dose-response study of guanfacine administered with 25 mg [[chlorthalidone]] at bedtime, the frequency of the most commonly observed adverse reactions showed a clear dose relationship from 0.5 to 3 mg as follows: | ||
[[File:TENEX05.jpg|thumb| | [[File:TENEX05.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
There were 41 premature terminations because of adverse reactions in this study. The percent of patients who dropped out and the dose at which the dropout occurred were as follows: | There were 41 premature terminations because of adverse reactions in this study. The percent of patients who dropped out and the dose at which the dropout occurred were as follows: | ||
[[File:TENEX06.jpg|thumb| | [[File:TENEX06.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Reasons for dropouts among patients who received guanfacine were: [[somnolence]], [[headache]], [[weakness]], dry mouth, [[dizziness]], [[impotence]], [[insomnia]], [[constipation]], [[syncope]], [[urinary incontinence]], [[conjunctivitis]], [[paresthesia]], and [[dermatitis]]. | Reasons for dropouts among patients who received guanfacine were: [[somnolence]], [[headache]], [[weakness]], [[dry mouth]], [[dizziness]], [[impotence]], [[insomnia]], [[constipation]], [[syncope]], [[urinary incontinence]], [[conjunctivitis]], [[paresthesia]], and [[dermatitis]]. | ||
In a second 12-week placebo-controlled combination therapy study in which the dose could be adjusted upward to 3 mg per day in 1-mg increments at 3-week intervals, i.e., a setting more similar to ordinary clinical use, the most commonly recorded reactions were: dry mouth, 47%; [[constipation]], 16%; [[fatigue]], 12%; [[somnolence]], 10%; [[asthenia]], 6%; [[dizziness]], 6%; [[headache]], 4%; and [[insomnia]], 4%. | In a second 12-week [[placebo]]-controlled combination therapy study in which the dose could be adjusted upward to 3 mg per day in 1-mg increments at 3-week intervals, i.e., a setting more similar to ordinary clinical use, the most commonly recorded reactions were: dry mouth, 47%; [[constipation]], 16%; [[fatigue]], 12%; [[somnolence]], 10%; [[asthenia]], 6%; [[dizziness]], 6%; [[headache]], 4%; and [[insomnia]], 4%. | ||
Reasons for dropouts among patients who received guanfacine were: [[somnolence]], dry mouth, [[dizziness]], [[impotence]], [[constipation]], [[confusion]], [[depression]], and [[palpitations]]. | Reasons for dropouts among patients who received guanfacine were: [[somnolence]], dry mouth, [[dizziness]], [[impotence]], [[constipation]], [[confusion]], [[depression]], and [[palpitations]]. | ||
| Line 93: | Line 91: | ||
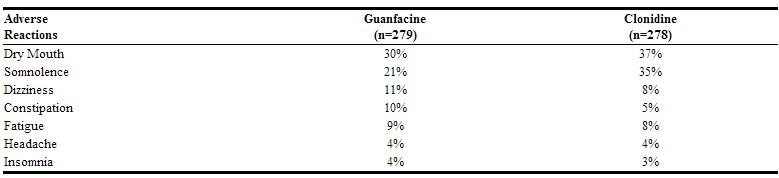
In the [[clonidine]]/guanfacine comparison described in CLINICAL PHARMACOLOGY, the most common adverse reactions noted were as follows: | In the [[clonidine]]/guanfacine comparison described in CLINICAL PHARMACOLOGY, the most common adverse reactions noted were as follows: | ||
[[File:TENEX03.jpg|thumb| | [[File:TENEX03.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Adverse reactions occurring in 3% or less of patients in the three controlled trials of | Adverse reactions occurring in 3% or less of patients in the three controlled trials of Guanfacine (guanfacine hydrochloride) with a [[diuretic]]were: | ||
'''Cardiovascular'''- [[bradycardia]], [[palpitations]], substernal pain | '''Cardiovascular'''- [[bradycardia]], [[palpitations]], substernal pain | ||
| Line 101: | Line 99: | ||
'''Gastrointestinal'''- abdominal pain, [[diarrhea]], [[dyspepsia]], [[dysphagia]], [[nausea]] | '''Gastrointestinal'''- abdominal pain, [[diarrhea]], [[dyspepsia]], [[dysphagia]], [[nausea]] | ||
'''CNS'''- [[amnesia]], [[confusion]], [[depression]], [[insomnia]], libido decrease | '''CNS'''- [[amnesia]], [[confusion]], [[depression]], [[insomnia]], [[libido]] decrease | ||
'''ENT disorders'''- [[rhinitis]], taste perversion, [[tinnitus]] | '''ENT disorders'''- [[rhinitis]], taste perversion, [[tinnitus]] | ||
| Line 107: | Line 105: | ||
'''Eye disorders'''- [[conjunctivitis]], [[iritis]], vision disturbance | '''Eye disorders'''- [[conjunctivitis]], [[iritis]], vision disturbance | ||
'''Musculoskeletal'''- leg cramps, [[hypokinesia]] | '''Musculoskeletal'''- [[leg cramps]], [[hypokinesia]] | ||
'''Respiratory'''- [[dyspnea]] | '''Respiratory'''- [[dyspnea]] | ||
| Line 117: | Line 115: | ||
'''Other'''- [[malaise]], [[paresthesia]], [[paresis]] | '''Other'''- [[malaise]], [[paresthesia]], [[paresis]] | ||
Adverse reaction reports tend to decrease over time. In an open-label trial of one year's duration, 580 hypertensive subjects were given guanfacine, titrated to achieve goal blood pressure, alone (51%), with [[diuretic]](38%), with [[beta blocker]] (3%), with [[diuretic]]plus [[beta blocker]] (6%), or with [[diuretic]]plus vasodilator (2%). The mean daily dose of guanfacine reached was 4.7 mg. | Adverse reaction reports tend to decrease over time. In an open-label trial of one year's duration, 580 hypertensive subjects were given guanfacine, titrated to achieve goal [[blood pressure]], alone (51%), with [[diuretic]](38%), with [[beta blocker]] (3%), with [[diuretic]]plus [[beta blocker]] (6%), or with [[diuretic]]plus [[vasodilator]] (2%). The mean daily dose of guanfacine reached was 4.7 mg. | ||
[[File:TENEX04.jpg|thumb| | [[File:TENEX04.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
There were 52 (8.9%) dropouts due to adverse effects in this 1-year trial. The causes were: dry mouth (n = 20), weakness (n = 12), [[constipation]] (n = 7), [[somnolence]] (n = 3), [[nausea]] (n = 3), | There were 52 (8.9%) dropouts due to adverse effects in this 1-year trial. The causes were: [[dry mouth]] (n = 20), weakness (n = 12), [[constipation]] (n = 7), [[somnolence]] (n = 3), [[nausea]] (n = 3), [[orthostatic hypotension]] (n = 2), [[insomnia]] (n = 1), [[rash]] (n = 1), nightmares (n = 1), [[headache]] (n = 1), and [[depression]] (n = 1). | ||
|postmarketing=An open-label postmarketing study involving 21,718 patients was conducted to assess the safety of | |postmarketing=An open-label postmarketing study involving 21,718 patients was conducted to assess the safety of Guanfacine (guanfacine hydrochloride) 1 mg/day given at bedtime for 28 days. Guanfacine was administered with or without other [[antihypertensive agents]]. Adverse events reported in the postmarketing study at an incidence greater than 1% included [[dry mouth]], [[dizziness]], [[somnolence]], [[fatigue]], [[headache]] and [[nausea]]. The most commonly reported adverse events in this study were the same as those observed in controlled [[clinical trials]]. | ||
Less frequent, possibly | Less frequent, possibly Guanfacine-related events observed in the postmarketing study and/or reported spontaneously include: | ||
'''BODY AS A WHOLE''' [[asthenia]], chest pain, [[edema]], [[malaise]], [[tremor]] | '''BODY AS A WHOLE''' [[asthenia]], chest pain, [[edema]], [[malaise]], [[tremor]] | ||
| Line 134: | Line 132: | ||
'''EYE DISORDERS''' [[blurred vision]] | '''EYE DISORDERS''' [[blurred vision]] | ||
'''GASTROINTESTINAL SYSTEM''' abdominal pain, [[constipation]], [[diarrhea]], [[dyspepsia]] | '''GASTROINTESTINAL SYSTEM''' [[abdominal pain]], [[constipation]], [[diarrhea]], [[dyspepsia]] | ||
'''LIVER AND BILLIARY SYSTEM''' abnormal liver function tests | '''LIVER AND BILLIARY SYSTEM''' [[Abnormal liver function test|abnormal liver function tests]] | ||
'''MUSCULO-SKELETAL SYSTEM''' [[arthralgia]], leg cramps, leg pain, [[myalgia]] | '''MUSCULO-SKELETAL SYSTEM''' [[arthralgia]], [[leg cramps]], [[leg pain]], [[myalgia]] | ||
'''PSYCHIATRIC''' [[agitation]], [[anxiety]], [[confusion]], [[depression]], [[insomnia]], [[nervousness]] | '''PSYCHIATRIC''' [[agitation]], [[anxiety]], [[confusion]], [[depression]], [[insomnia]], [[nervousness]] | ||
'''RREPRODUCTIVE SYSTEM''', Male- impotence | '''RREPRODUCTIVE SYSTEM''', Male- [[impotence]] | ||
'''RESPIRATORY SYSTEM''' [[dyspnea]] | '''RESPIRATORY SYSTEM''' [[dyspnea]] | ||
'''SKIN AND APPENDAGES''' [[alopecia]], [[dermatitis]], exfoliative dermatitis, [[pruritus]], [[rash]] | '''SKIN AND APPENDAGES''' [[alopecia]], [[dermatitis]], [[exfoliative dermatitis]], [[pruritus]], [[rash]] | ||
'''SPECIAL SENSES''' alterations in taste | '''SPECIAL SENSES''' alterations in taste | ||
'''URINARY SYSTEM''' [[nocturia]], urinary frequency | '''URINARY SYSTEM''' [[nocturia]], [[urinary frequency]] | ||
Rare, serious disorders with no definitive cause and effect relationship to | Rare, serious disorders with no definitive cause and effect relationship to Guanfacine have been reported spontaneously and/or in the postmarketing study. These events include [[acute renal failure]], [[cardiac fibrillation]], [[cerebrovascular accident]], [[congestive heart failure]], [[heart block]], and [[myocardial infarction]]. | ||
|drugInteractions=The potential for increased sedation when | |drugInteractions=The potential for increased [[sedation]] when Guanfacine is given with other [[CNS Depressant|CNS-depressant drugs]] should be appreciated. | ||
The administration of guanfacine concomitantly with a known microsomal enzyme inducer (phenobarbital or phenytoin) to two patients with renal impairment reportedly resulted in significant reductions in elimination half-life and plasma concentration. In such cases, therefore, more frequent dosing may be required to achieve or maintain the desired hypotensive response. Further, if guanfacine is to be discontinued in such patients, careful tapering of the dosage may be necessary in order to avoid rebound phenomena (see Rebound above). | The administration of guanfacine concomitantly with a known [[microsomal]] enzyme inducer ([[phenobarbital]] or [[phenytoin]]) to two patients with [[renal impairment]] reportedly resulted in significant reductions in elimination half-life and plasma concentration. In such cases, therefore, more frequent dosing may be required to achieve or maintain the desired [[hypotensive]] response. Further, if guanfacine is to be discontinued in such patients, careful tapering of the dosage may be necessary in order to avoid rebound phenomena (see Rebound above). | ||
===Anticoagulants=== | ===Anticoagulants=== | ||
Ten patients who were stabilized on oral anticoagulants were given guanfacine, 1 - 2 mg/day, for 4 weeks. No changes were observed in the degree of anticoagulation. | Ten patients who were stabilized on oral [[anticoagulants]] were given guanfacine, 1 - 2 mg/day, for 4 weeks. No changes were observed in the degree of [[anticoagulation]]. | ||
In several well-controlled studies, guanfacine was administered together with diuretics with no drug interactions reported. In the long-term safety studies, | In several well-controlled studies, guanfacine was administered together with diuretics with no drug interactions reported. In the long-term safety studies, Guanfacine was given concomitantly with many drugs without evidence of any interactions. The principal drugs given (number of patients in parentheses) were: cardiac [[glycosides]] (115), [[sedatives]] and [[hypnotics]] (103), [[coronary]] [[vasodilators]] (52), [[oral hypoglycemics]] (45), [[cough]] and cold preparations (45), [[NSAIDs]] (38), [[antihyperlipidemics]] (29), [[Antigout|antigout drugs]] (24), [[oral contraceptives]] (18), [[bronchodilators]] (13), [[insulin]] (10), and [[beta blockers]](10). | ||
|FDAPregCat=B | |FDAPregCat=B | ||
|useInPregnancyFDA=Administration of guanfacine to rats at 70 times the maximum recommended human dose and to rabbits at 20 times the maximum recommended human dose resulted in no evidence of harm to the fetus. Higher doses (100 and 200 times the maximum recommended human dose in rabbits and rats respectively) were associated with reduced fetal survival and maternal toxicity. Rat experiments have shown that guanfacine crosses the placenta. | |useInPregnancyFDA=Administration of guanfacine to rats at 70 times the maximum recommended human dose and to rabbits at 20 times the maximum recommended human dose resulted in no evidence of harm to the [[fetus]]. Higher doses (100 and 200 times the maximum recommended human dose in rabbits and rats respectively) were associated with reduced fetal survival and maternal [[toxicity]]. Rat experiments have shown that guanfacine crosses the [[placenta]]. | ||
There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. | There are, however, no adequate and well-controlled studies in [[pregnant]] women. Because animal [[reproduction]] studies are not always predictive of human response, this drug should be used during [[pregnancy]] only if clearly needed. | ||
|useInLaborDelivery= | |useInLaborDelivery=Guanfacine (guanfacine hydrochloride) is not recommended in the treatment of acute [[hypertension]] associated with [[toxemia]] of [[pregnancy]]. There is no information available on the effects of guanfacine on the course of [[labor]] and [[delivery]]. | ||
|useInNursing=It is not known whether | |useInNursing=It is not known whether Guanfacine (guanfacine hydrochloride) is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Guanfacine is administered to a nursing woman. Experiments with rats have shown that guanfacine is excreted in the milk. | ||
|useInPed=Safety and effectiveness in children under 12 years of age have not been demonstrated. Therefore, the use of | |useInPed=Safety and effectiveness in children under 12 years of age have not been demonstrated. Therefore, the use of Guanfacine in this age group is not recommended. There have been spontaneous postmarketing reports of [[mania]] and aggressive [[behavioral]] changes in [[pediatric]] patients with attention-deficit [[hyperactivity]] disorder ([[ADHD]]) receiving Guanfacine. The reported cases were from a single center. All patients had medical or family risk factors for [[bipolar disorder]]. All patients recovered upon discontinuation of guanfacine HCl. Hallucinations have been reported in pediatric patients receiving Guanfacine for treatment of [[attention-deficit hyperactivity disorder]]. | ||
|useInGeri=Clinical studies of | |useInGeri=Clinical studies of Guanfacine did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. | ||
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy | In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased [[hepatic]], [[renal]] or [[cardiac]] function, and of concomitant disease or other drug therapy. | ||
|administration=Oral | |administration=Oral | ||
|monitoring=FDA Package Insert for Guanfacine contains no information regarding drug monitoring. | |monitoring=FDA Package Insert for Guanfacine contains no information regarding drug monitoring. | ||
|IVCompat=There is limited information about the IV Compatibility. | |IVCompat=There is limited information about the IV Compatibility. | ||
|overdose====Signs and Symptoms=== | |overdose====Signs and Symptoms==== | ||
[[Drowsiness]], [[lethargy]], [[bradycardia]] and [[hypotension]] have been observed following overdose with guanfacine. | [[Drowsiness]], [[lethargy]], [[bradycardia]] and [[hypotension]] have been observed following overdose with guanfacine. | ||
A 25-year-old female intentionally ingested 60 mg. She presented with severe [[drowsiness]] and [[bradycardia]] of 45 beats/minute. Gastric lavage was performed and an infusion of [[isoproterenol]] (0.8 mg in 12 hours) was administered. She recovered quickly and without sequelae. | A 25-year-old female intentionally ingested 60 mg. She presented with severe [[drowsiness]] and [[bradycardia]] of 45 beats/minute. [[Gastric lavage]] was performed and an infusion of [[isoproterenol]] (0.8 mg in 12 hours) was administered. She recovered quickly and without sequelae. | ||
A 28-year-old female who ingested 30 - 40 mg developed only lethargy, was treated with activated [[charcoal]] and a [[cathartic]], was monitored for 24 hours, and was discharged in good health. | A 28-year-old female who ingested 30 - 40 mg developed only [[lethargy]], was treated with activated [[charcoal]] and a [[cathartic]], was monitored for 24 hours, and was discharged in good health. | ||
A 2-year-old male weighing 12 kg who ingested up to 4 mg of guanfacine developed lethargy. Gastric lavage (followed by activated charcoal and sorbitol slurry via NG tube) removed some tablet fragments within 2 hours after ingestion, and vital signs were normal. | A 2-year-old male weighing 12 kg who ingested up to 4 mg of guanfacine developed [[lethargy]]. [[Gastric lavage]] (followed by [[activated charcoal]] and [[sorbitol]] slurry via [[NG tube]]) removed some tablet fragments within 2 hours after [[ingestion]], and vital signs were normal. | ||
During 24-hour observation in ICU, systolic pressure was 58 and heart rate 70 at 16 hours post-ingestion. No intervention was required, and child was discharged fully recovered the next day. | During 24-hour observation in ICU, systolic pressure was 58 and heart rate 70 at 16 hours post-ingestion. No intervention was required, and child was discharged fully recovered the next day. | ||
| Line 194: | Line 192: | ||
| verifiedrevid = 461124228 | | verifiedrevid = 461124228 | ||
| IUPAC_name = ''N''-(diaminomethylidene)-2-(2,6-dichlorophenyl)acetamide | | IUPAC_name = ''N''-(diaminomethylidene)-2-(2,6-dichlorophenyl)acetamide | ||
| image = Guanfacine2DACS. | | image = Guanfacine2DACS.png | ||
| width = 200 | | width = 200 | ||
| image2 = Guanfacine3Dan.gif | | image2 = Guanfacine3Dan.gif | ||
| Line 200: | Line 198: | ||
<!--Clinical data--> | <!--Clinical data--> | ||
| tradename = Afken, Estulic, | | tradename = Afken, Estulic, Guanfacine, Guanfacine | ||
| Drugs.com = {{drugs.com|monograph|guanfacine}} | | Drugs.com = {{drugs.com|monograph|guanfacine}} | ||
| licence_US = Guanfacine | | licence_US = Guanfacine | ||
| Line 210: | Line 208: | ||
<!--Pharmacokinetic data--> | <!--Pharmacokinetic data--> | ||
| bioavailability = 80-100% (IR), 58% (XR)<ref name = DM>{{cite web|title=Guanfacine (guanfacine) Tablet [Genpharm Inc.]|work=DailyMed|publisher=Genpharm Inc.|date=March 2007|accessdate=9 November 2013|url=http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=9fc0bdc2-5ba2-48dd-aa87-7b0050a2d6ce}}</ref><ref name = MSR>{{cite web|title=guanfacine (Rx) - | | bioavailability = 80-100% (IR), 58% (XR)<ref name = DM>{{cite web|title=Guanfacine (guanfacine) Tablet [Genpharm Inc.]|work=DailyMed|publisher=Genpharm Inc.|date=March 2007|accessdate=9 November 2013|url=http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=9fc0bdc2-5ba2-48dd-aa87-7b0050a2d6ce}}</ref><ref name = MSR>{{cite web|title=guanfacine (Rx) - Guanfacine, Guanfacine|work=Medscape Reference|publisher=WebMD|accessdate=9 November 2013|url=http://reference.medscape.com/drug/Guanfacine-Guanfacine-guanfacine-342384}}</ref> | ||
| protein_bound = 70%<ref name = DM/><ref name = MSR/> | | protein_bound = 70%<ref name = DM/><ref name = MSR/> | ||
| metabolism = [[CYP3A4]]<ref name = DM/><ref name = MSR/> | | metabolism = [[CYP3A4]]<ref name = DM/><ref name = MSR/> | ||
| Line 247: | Line 245: | ||
| StdInChIKey = INJOMKTZOLKMBF-UHFFFAOYSA-N | | StdInChIKey = INJOMKTZOLKMBF-UHFFFAOYSA-N | ||
}} | }} | ||
|mechAction=Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of central α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate. | |mechAction=Guanfacine hydrochloride is an orally active [[antihypertensive agent]] whose principal mechanism of action appears to be stimulation of [[central Adrenergic receptor|α2-adrenergic receptors]]. By stimulating these receptors, guanfacine reduces [[sympathetic nerve]] impulses from the [[vasomotor]] center to the [[heart]] and [[blood vessels]]. This results in a decrease in [[peripheral vascular resistance]] and a reduction in [[heart rate]]. | ||
|structure= | |structure=Guanfacine (guanfacine hydrochloride) is a centrally acting [[antihypertensive]] with [[Adrenergic agonist|α2-adrenoceptor agonist]] properties in tablet form for oral administration. | ||
The chemical name of | The chemical name of Guanfacine (guanfacine hydrochloride) is N-amidino- 2-(2,6-dichlorophenyl) acetamide hydrochloride and its molecular weight is 282.56. Its structural formula is: | ||
[[File:TENEX07.jpg|thumb| | [[File:TENEX07.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | ||
Guanfacine hydrochloride is a white to off-white powder; sparingly soluble in water and alcohol and slightly soluble in acetone. The tablets contain the following inactive ingredients: | Guanfacine hydrochloride is a white to off-white powder; sparingly soluble in water and alcohol and slightly soluble in acetone. The tablets contain the following inactive ingredients: | ||
1 mg—FD&C Red 40 aluminum lake, lactose, microcrystalline cellulose, povidone, stearic acid | 1 mg—FD&C Red 40 aluminum lake, [[lactose]], [[microcrystalline cellulose]], [[povidone]], [[stearic acid]]. | ||
[[ | 2 mg—D&C Yellow 10 aluminum lake, [[lactose]], [[microcrystalline cellulose]], [[povidone]], [[stearic acid]]. | ||
|PD=The dose-response relationship for [[blood pressure]] and adverse effects of guanfacine given once a day as [[monotherapy]] has been evaluated in patients with mild to moderate [[hypertension]]. In this study patients were randomized to [[placebo]] or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of Guanfacine. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions. | |||
[[File:TENEX08.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
[[ | Controlled [[clinical trials]] in patients with mild to moderate [[hypertension]] who were receiving a [[thiazide]]-type [[diuretic ]]have defined the dose-response relationship for [[blood pressure]] response and adverse reactions of guanfacine given at bedtime and have shown that the [[blood pressure]] response to guanfacine can persist for 24 hours after a single dose. In the 12-week [[placebo]]-controlled dose-response study, patients were randomized to [[placebo]] or to doses of 0.5, 1, 2, and 3 mg of guanfacine, in addition to 25 mg [[chlorthalidone]], each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for [[placebo]] and the 0.5 mg dose. Doses of 1, 2, and 3 mg resulted in decreased [[blood pressure]] in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose. | ||
[[File:TENEX09.jpg|thumb|none|400px|This image is provided by the National Library of Medicine.]] | |||
While most of the effectiveness of guanfacine in combination (and as [[monotherapy]] in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with [[placebo]]. Adverse reactions were clearly present at 2 and 3 mg. | |||
In a | In a second 12-week placebo-controlled study of 1, 2 or 3 mg of Guanfacine (guanfacine hydrochloride) administered with 25 mg of [[chlorthalidone ]]once daily, a significant decrease in [[blood pressure]] was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 and 24 hour [[blood pressure]] readings, the fall in [[blood pressure]] at 24 hours was numerically smaller, suggesting possible escape of [[blood pressure]] in some patients and the need for individualization of therapy. | ||
In a double-blind, randomized trial, either guanfacine or [[clonidine ]]was given at recommended doses with 25 mg [[chlorthalidone ]]for 24 weeks and then abruptly discontinued. Results showed equal degrees of [[blood pressure]] reduction with the two drugs and there was no tendency for [[blood pressures]] to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of [[clonidine ]]produced a rapid return of [[diastolic]] and especially [[systolic blood pressure]] to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline. | |||
[[Hemodynamic]] studies in man showed that the decrease in [[blood pressure]] observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in [[peripheral resistance]] and a slight reduction in [[heart rate]] (5 [[beats]]/min). [[Cardiac output]] under conditions of rest or exercise was not altered by guanfacine. | |||
Guanfacine (guanfacine hydrochloride) lowered elevated plasma [[renin]] activity and plasma [[catecholamine]] levels in [[hypertensive]] patients, but this does not correlate with individual [[blood-pressure]] responses. | |||
Guanfacine had no effect on | [[Growth hormone]] secretion was stimulated with single oral doses of 2 and 4 mg of guanfacine. Long-term use of Guanfacine had no effect on [[growth hormone]] levels. | ||
|PK=Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80%. Peak plasma concentrations occur from 1 to 4 hours with an average of 2.6 hours after single oral doses or at steady state. | Guanfacine had no effect on plasma [[aldosterone]]. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes. | ||
|PK=Relative to an intravenous dose of 3 mg, the absolute oral [[bioavailability]] of guanfacine is about 80%. Peak plasma concentrations occur from 1 to 4 hours with an average of 2.6 hours after single oral doses or at steady state. | |||
The area under the concentration-time curve (AUC) increases linearly with the dose. | The area under the concentration-time curve (AUC) increases linearly with the dose. | ||
In individuals with normal renal function, the average elimination half-life is approximately 17 hr (range 10 - 30 hr). Younger patients tend to have shorter elimination half-lives (13 - 14 hr) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects. | In individuals with normal renal function, the average elimination half-life is approximately 17 hr (range 10 - 30 hr). Younger patients tend to have shorter elimination half-lives (13 - 14 hr) while older patients tend to have half-lives at the upper end of the range. Steady state [[blood]] levels were attained within 4 days in most subjects. | ||
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50% (40 - 75%) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring. | In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50% (40 - 75%) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by [[oxidative]] metabolism of the aromatic ring. | ||
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs. | The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs. | ||
| Line 295: | Line 292: | ||
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues. | The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues. | ||
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed. | The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with [[renal impairment]], the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly [[dialusis|dialyzed]]. | ||
|nonClinToxic=Carcinogenesis, Mutagenesis, Impairment of Fertility | |nonClinToxic=Carcinogenesis, Mutagenesis, Impairment of Fertility | ||
No carcinogenic effect was observed in studies of 78 weeks in mice at doses more than 150 times the maximum recommended human dose and 102 weeks in rats at doses more than 100 times the maximum recommended human dose. In a variety of test models, guanfacine was not mutagenic. | No carcinogenic effect was observed in studies of 78 weeks in mice at doses more than 150 times the maximum recommended human dose and 102 weeks in rats at doses more than 100 times the maximum recommended human dose. In a variety of test models, guanfacine was not [[mutagenic]]. | ||
No adverse effects were observed in fertility studies in male and female rats. | No adverse effects were observed in [[fertility]] studies in male and female rats. | ||
|clinicalStudies=FDA Package Insert for Guanfacine contains no information regarding clinical studies. | |clinicalStudies=FDA Package Insert for Guanfacine contains no information regarding clinical studies. | ||
|howSupplied=Guanfacine Tablets USP, 1 mg are available as white, round, flat-faced beveled-edge tablets, debossed “Є48” on one side and plain on the other side. These are supplied in bottles of 100 and 500. | |howSupplied=Guanfacine Tablets USP, 1 mg are available as white, round, flat-faced beveled-edge tablets, debossed “Є48” on one side and plain on the other side. These are supplied in bottles of 100 and 500. | ||
Guanfacine Tablets USP, 2 mg are available as yellow, round, flat-faced beveled-edge tablets, debossed “Є49” on one side and plain on the other side. These are supplied in bottles of 100 and 500. | Guanfacine Tablets USP, 2 mg are available as yellow, round, flat-faced beveled-edge tablets, debossed “Є49” on one side and plain on the other side. These are supplied in bottles of 100 and 500. | ||
|storage=Store at 20°-25°C (68°-77°F). | |||
|storage=Store at 20°-25°C (68°-77°F). | |||
Dispense in a tight, light-resistant container. | Dispense in a tight, light-resistant container. | ||
|fdaPatientInfo=Patients who receive guanfacine should be advised to exercise caution when operating dangerous machinery or driving motor vehicles until it is determined that they do not become drowsy or dizzy from the medication. Patients should be warned that their tolerance for alcohol and other CNS depressants may be diminished. Patients should be advised not to discontinue therapy abruptly. | |fdaPatientInfo=Patients who receive guanfacine should be advised to exercise caution when operating dangerous machinery or driving motor vehicles until it is determined that they do not become drowsy or dizzy from the medication. Patients should be warned that their tolerance for alcohol and other [[CNS depressant|CNS depressants]] may be diminished. Patients should be advised not to discontinue therapy abruptly. | ||
|alcohol= | |alcohol=Patients should be warned that their tolerance for alcohol and other [[CNS depressant|CNS depressants]] may be diminished | ||
|brandNames=* | |brandNames=* INTUNIV | ||
* | * TENEX | ||
|lookAlike=GUANFACINE - GUAIFENESIN<ref name="www.ismp.org">{{Cite web | last = | first = | title =https://www.ismp.org | url = https://www.ismp.org | publisher = | date = | accessdate = }}</ref> | |lookAlike=GUANFACINE - GUAIFENESIN<ref name="www.ismp.org">{{Cite web | last = | first = | title =https://www.ismp.org | url = https://www.ismp.org | publisher = | date = | accessdate = }}</ref> | ||
}} | }} | ||
| Line 338: | Line 334: | ||
}} | }} | ||
{{LabelImage | {{LabelImage | ||
|fileName= | |fileName=Guanfacine_label_01.jpg | ||
}} | }} | ||
{{LabelImage | {{LabelImage | ||
|fileName= | |fileName=Guanfacine_label_02.jpg | ||
}} | }} | ||
{{LabelImage | {{LabelImage | ||
|fileName= | |fileName=Guanfacine_label_01.png | ||
}} | }} | ||
[[Category:Antihypertensive agents]] | |||
[[Category:Cardiovascular Drugs]] | |||
[[Category:Drug]] | |||
Latest revision as of 16:27, 20 August 2015
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Sheng Shi, M.D. [2]; Adeel Jamil, M.D. [3]
Disclaimer
WikiDoc MAKES NO GUARANTEE OF VALIDITY. WikiDoc is not a professional health care provider, nor is it a suitable replacement for a licensed healthcare provider. WikiDoc is intended to be an educational tool, not a tool for any form of healthcare delivery. The educational content on WikiDoc drug pages is based upon the FDA package insert, National Library of Medicine content and practice guidelines / consensus statements. WikiDoc does not promote the administration of any medication or device that is not consistent with its labeling. Please read our full disclaimer here.
Overview
Guanfacine is a central alpha-2 adrenergic agonist that is FDA approved for the treatment of hypertension. Common adverse reactions include orthostatic hypotension, abdominal pain, constipation, xerostomia, dizziness, headache, insomnia, somnolence, impotence, fatigue.
Adult Indications and Dosage
FDA-Labeled Indications and Dosage (Adult)
Hypertension
- Dosing information
- Recommended initial dosage: 1 mg/day given at bedtime to minimize somnolence.
- If after 3 to 4 weeks of therapy, 1 mg does not give a satisfactory result, a dose of 2 mg may be given
- Higher daily doses have been used, but adverse reactions increase significantly with doses above 3 mg/day.
- The frequency of rebound hypertension is low, but it can occur. When rebound occurs, it does so after 2-4 days, which is delayed compared with clonidine hydrochloride. This is consistent with the longer half-life of guanfacine. In most cases, after abrupt withdrawal of guanfacine, blood pressure returns to pretreatment levels slowly (within 2-4 days) without ill effects.
Off-Label Use and Dosage (Adult)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Guanfacine sandbox in adult patients.
Non–Guideline-Supported Use
Prophylaxis of Migraine
- Dosing information
- Not applicable
Pediatric Indications and Dosage
FDA-Labeled Indications and Dosage (Pediatric)
FDA Package Insert for Guanfacine contains no information regarding FDA-labeled indications and dosage information for children.
Off-Label Use and Dosage (Pediatric)
Guideline-Supported Use
There is limited information regarding Off-Label Guideline-Supported Use of Guanfacine sandbox in pediatric patients.
Non–Guideline-Supported Use
<H4Attention deficit hyperactivity disorder- Dosing information
Gilles de la Tourette's syndrome
- Dosing information
Contraindications
Patients with a history of hypersensitivity to Guanfacine®, its inactive ingredients [see Description (11)] or other products containing guanfacine should not take Guanfacine®
Warnings
General=
Like other antihypertensive agents, Guanfacine (guanfacine hydrochloride) should be used with caution in patients with severe coronary insufficiency, recent myocardial infarction, cerebrovascular disease, or chronic renal or hepatic failure.
Sedation
Guanfacine, like other orally active central α2-adrenergic agonists, causes sedation or drowsiness, especially when beginning therapy. These symptoms are dose-related. When Guanfacine is used with other centrally active depressants (such as phenothiazines, barbiturates, or benzodiazepines), the potential for additive sedative effects should be considered.
Rebound
Abrupt cessation of therapy with orally active central α2-adrenergic agonists may be associated with increases (from depressed on-therapy levels) in plasma and urinary catecholamines]], symptoms of "nervousness and anxiety" and, less commonly, increases in blood pressure to levels significantly greater than those prior to therapy.
Information for Patients
Patients who receive Guanfacine should be advised to exercise caution when operating dangerous machinery or driving motor vehicles until it is determined that they do not become drowsy or dizzy from the medication. Patients should be warned that their tolerance for alcohol and other CNS depressants may be diminished. Patients should be advised not to discontinue therapy abruptly.
Laboratory Tests
In clinical trials, no clinically relevant laboratory test abnormalities were identified as causally related to drug during short-term treatment with Guanfacine (guanfancine hydrochloride).
Adverse Reactions
Clinical Trials Experience
Adverse reactions noted with Guanfacine (guanfacine hydrochloride) are similar to those of other drugs of the central α2-adrenoreceptor agonist class: dry mouth, sedation (somnolence), weakness (asthenia), dizziness, constipation, and impotence. While the reactions are common, most are mild and tend to disappear on continued dosing.
Skin rash with exfoliation has been reported in a few cases; although clear cause and effect relationships to Guanfacine could not be established, should a rash occur, Guanfacine should be discontinued and the patient monitored appropriately.
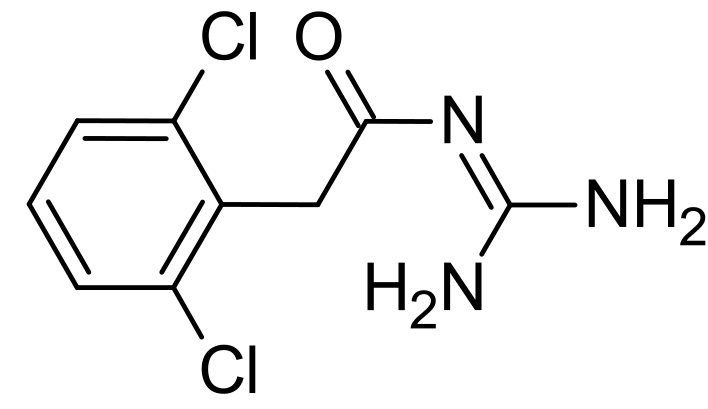
In the dose-response monotherapy study described under CLINICAL PHARMACOLOGY, the frequency of the most commonly observed adverse reactions showed a dose relationship from 0.5 to 3 mg as follows:
name="Table_4" style="color: rgb(0, 0, 0); font-family: 'Arial Unicode MS'; font-size: 16px; font-style: normal; font-variant: normal; font-weight: normal; letter-spacing: normal; line-height: normal; orphans: auto; text-align: start; text-indent: 0px; text-transform: none; white-space: normal; widows: auto; word-spacing: 0px; -webkit-text-stroke-width: 0px; background-color: rgb(255, 255, 255);"
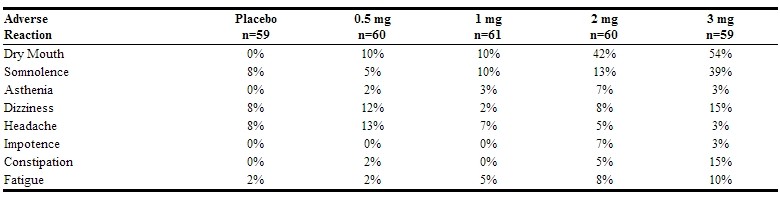
The percent of patients who dropped out because of adverse reactions are shown below for each dosage group.
The most common reasons for dropouts among patients who received guanfacine were dry mouth, somnolence, dizziness, fatigue, weakness, and constipation.
In the 12-week, placebo-controlled, dose-response study of guanfacine administered with 25 mg chlorthalidone at bedtime, the frequency of the most commonly observed adverse reactions showed a clear dose relationship from 0.5 to 3 mg as follows:
There were 41 premature terminations because of adverse reactions in this study. The percent of patients who dropped out and the dose at which the dropout occurred were as follows:
Reasons for dropouts among patients who received guanfacine were: somnolence, headache, weakness, dry mouth, dizziness, impotence, insomnia, constipation, syncope, urinary incontinence, conjunctivitis, paresthesia, and dermatitis.
In a second 12-week placebo-controlled combination therapy study in which the dose could be adjusted upward to 3 mg per day in 1-mg increments at 3-week intervals, i.e., a setting more similar to ordinary clinical use, the most commonly recorded reactions were: dry mouth, 47%; constipation, 16%; fatigue, 12%; somnolence, 10%; asthenia, 6%; dizziness, 6%; headache, 4%; and insomnia, 4%.
Reasons for dropouts among patients who received guanfacine were: somnolence, dry mouth, dizziness, impotence, constipation, confusion, depression, and palpitations.
In the clonidine/guanfacine comparison described in CLINICAL PHARMACOLOGY, the most common adverse reactions noted were as follows:
Adverse reactions occurring in 3% or less of patients in the three controlled trials of Guanfacine (guanfacine hydrochloride) with a diureticwere:
Cardiovascular- bradycardia, palpitations, substernal pain
Gastrointestinal- abdominal pain, diarrhea, dyspepsia, dysphagia, nausea
CNS- amnesia, confusion, depression, insomnia, libido decrease
ENT disorders- rhinitis, taste perversion, tinnitus
Eye disorders- conjunctivitis, iritis, vision disturbance
Musculoskeletal- leg cramps, hypokinesia
Respiratory- dyspnea
Dermatologic- dermatitis, pruritus, purpura, sweating
Urogenital- testicular disorder, urinary incontinence
Other- malaise, paresthesia, paresis
Adverse reaction reports tend to decrease over time. In an open-label trial of one year's duration, 580 hypertensive subjects were given guanfacine, titrated to achieve goal blood pressure, alone (51%), with diuretic(38%), with beta blocker (3%), with diureticplus beta blocker (6%), or with diureticplus vasodilator (2%). The mean daily dose of guanfacine reached was 4.7 mg.
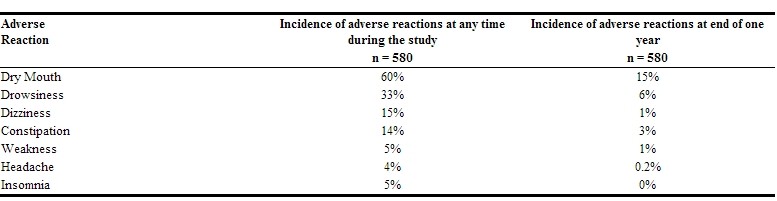
There were 52 (8.9%) dropouts due to adverse effects in this 1-year trial. The causes were: dry mouth (n = 20), weakness (n = 12), constipation (n = 7), somnolence (n = 3), nausea (n = 3), orthostatic hypotension (n = 2), insomnia (n = 1), rash (n = 1), nightmares (n = 1), headache (n = 1), and depression (n = 1).
Postmarketing Experience
An open-label postmarketing study involving 21,718 patients was conducted to assess the safety of Guanfacine (guanfacine hydrochloride) 1 mg/day given at bedtime for 28 days. Guanfacine was administered with or without other antihypertensive agents. Adverse events reported in the postmarketing study at an incidence greater than 1% included dry mouth, dizziness, somnolence, fatigue, headache and nausea. The most commonly reported adverse events in this study were the same as those observed in controlled clinical trials.
Less frequent, possibly Guanfacine-related events observed in the postmarketing study and/or reported spontaneously include:
BODY AS A WHOLE asthenia, chest pain, edema, malaise, tremor
CARDIOVASCULAR bradycardia, palpitations, syncope, tachycardia
CENTRAL NERVOUS SYSTEM paresthesias, vertigo
EYE DISORDERS blurred vision
GASTROINTESTINAL SYSTEM abdominal pain, constipation, diarrhea, dyspepsia
LIVER AND BILLIARY SYSTEM abnormal liver function tests
MUSCULO-SKELETAL SYSTEM arthralgia, leg cramps, leg pain, myalgia
PSYCHIATRIC agitation, anxiety, confusion, depression, insomnia, nervousness
RREPRODUCTIVE SYSTEM, Male- impotence
RESPIRATORY SYSTEM dyspnea
SKIN AND APPENDAGES alopecia, dermatitis, exfoliative dermatitis, pruritus, rash
SPECIAL SENSES alterations in taste
URINARY SYSTEM nocturia, urinary frequency
Rare, serious disorders with no definitive cause and effect relationship to Guanfacine have been reported spontaneously and/or in the postmarketing study. These events include acute renal failure, cardiac fibrillation, cerebrovascular accident, congestive heart failure, heart block, and myocardial infarction.
Drug Interactions
The potential for increased sedation when Guanfacine is given with other CNS-depressant drugs should be appreciated.
The administration of guanfacine concomitantly with a known microsomal enzyme inducer (phenobarbital or phenytoin) to two patients with renal impairment reportedly resulted in significant reductions in elimination half-life and plasma concentration. In such cases, therefore, more frequent dosing may be required to achieve or maintain the desired hypotensive response. Further, if guanfacine is to be discontinued in such patients, careful tapering of the dosage may be necessary in order to avoid rebound phenomena (see Rebound above).
Anticoagulants
Ten patients who were stabilized on oral anticoagulants were given guanfacine, 1 - 2 mg/day, for 4 weeks. No changes were observed in the degree of anticoagulation.
In several well-controlled studies, guanfacine was administered together with diuretics with no drug interactions reported. In the long-term safety studies, Guanfacine was given concomitantly with many drugs without evidence of any interactions. The principal drugs given (number of patients in parentheses) were: cardiac glycosides (115), sedatives and hypnotics (103), coronary vasodilators (52), oral hypoglycemics (45), cough and cold preparations (45), NSAIDs (38), antihyperlipidemics (29), antigout drugs (24), oral contraceptives (18), bronchodilators (13), insulin (10), and beta blockers(10).
Use in Specific Populations
Pregnancy
Pregnancy Category (FDA): B Administration of guanfacine to rats at 70 times the maximum recommended human dose and to rabbits at 20 times the maximum recommended human dose resulted in no evidence of harm to the fetus. Higher doses (100 and 200 times the maximum recommended human dose in rabbits and rats respectively) were associated with reduced fetal survival and maternal toxicity. Rat experiments have shown that guanfacine crosses the placenta.
There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Pregnancy Category (AUS):
There is no Australian Drug Evaluation Committee (ADEC) guidance on usage of Guanfacine in women who are pregnant.
Labor and Delivery
Guanfacine (guanfacine hydrochloride) is not recommended in the treatment of acute hypertension associated with toxemia of pregnancy. There is no information available on the effects of guanfacine on the course of labor and delivery.
Nursing Mothers
It is not known whether Guanfacine (guanfacine hydrochloride) is excreted in human milk. Because many drugs are excreted in human milk, caution should be exercised when Guanfacine is administered to a nursing woman. Experiments with rats have shown that guanfacine is excreted in the milk.
Pediatric Use
Safety and effectiveness in children under 12 years of age have not been demonstrated. Therefore, the use of Guanfacine in this age group is not recommended. There have been spontaneous postmarketing reports of mania and aggressive behavioral changes in pediatric patients with attention-deficit hyperactivity disorder (ADHD) receiving Guanfacine. The reported cases were from a single center. All patients had medical or family risk factors for bipolar disorder. All patients recovered upon discontinuation of guanfacine HCl. Hallucinations have been reported in pediatric patients receiving Guanfacine for treatment of attention-deficit hyperactivity disorder.
Geriatic Use
Clinical studies of Guanfacine did not include sufficient numbers of subjects aged 65 and over to determine whether they responded differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal or cardiac function, and of concomitant disease or other drug therapy.
Gender
There is no FDA guidance on the use of Guanfacine with respect to specific gender populations.
Race
There is no FDA guidance on the use of Guanfacine with respect to specific racial populations.
Renal Impairment
There is no FDA guidance on the use of Guanfacine in patients with renal impairment.
Hepatic Impairment
There is no FDA guidance on the use of Guanfacine in patients with hepatic impairment.
Females of Reproductive Potential and Males
There is no FDA guidance on the use of Guanfacine in women of reproductive potentials and males.
Immunocompromised Patients
There is no FDA guidance one the use of Guanfacine in patients who are immunocompromised.
Administration and Monitoring
Administration
Oral
Monitoring
FDA Package Insert for Guanfacine contains no information regarding drug monitoring.
IV Compatibility
There is limited information about the IV Compatibility.
Overdosage
Signs and Symptoms=
Drowsiness, lethargy, bradycardia and hypotension have been observed following overdose with guanfacine.
A 25-year-old female intentionally ingested 60 mg. She presented with severe drowsiness and bradycardia of 45 beats/minute. Gastric lavage was performed and an infusion of isoproterenol (0.8 mg in 12 hours) was administered. She recovered quickly and without sequelae.
A 28-year-old female who ingested 30 - 40 mg developed only lethargy, was treated with activated charcoal and a cathartic, was monitored for 24 hours, and was discharged in good health.
A 2-year-old male weighing 12 kg who ingested up to 4 mg of guanfacine developed lethargy. Gastric lavage (followed by activated charcoal and sorbitol slurry via NG tube) removed some tablet fragments within 2 hours after ingestion, and vital signs were normal.
During 24-hour observation in ICU, systolic pressure was 58 and heart rate 70 at 16 hours post-ingestion. No intervention was required, and child was discharged fully recovered the next day.
Treatment of Overdosage
Gastric lavage and supportive therapy as appropriate. Guanfacine is not dialyzable in clinically significant amounts (2.4%).
Pharmacology
Mechanism of Action
Guanfacine hydrochloride is an orally active antihypertensive agent whose principal mechanism of action appears to be stimulation of α2-adrenergic receptors. By stimulating these receptors, guanfacine reduces sympathetic nerve impulses from the vasomotor center to the heart and blood vessels. This results in a decrease in peripheral vascular resistance and a reduction in heart rate.
Structure
Guanfacine (guanfacine hydrochloride) is a centrally acting antihypertensive with α2-adrenoceptor agonist properties in tablet form for oral administration.
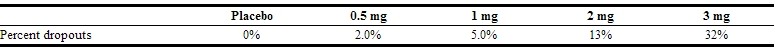
The chemical name of Guanfacine (guanfacine hydrochloride) is N-amidino- 2-(2,6-dichlorophenyl) acetamide hydrochloride and its molecular weight is 282.56. Its structural formula is:
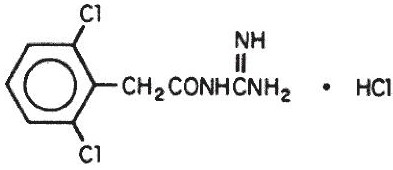
Guanfacine hydrochloride is a white to off-white powder; sparingly soluble in water and alcohol and slightly soluble in acetone. The tablets contain the following inactive ingredients:
1 mg—FD&C Red 40 aluminum lake, lactose, microcrystalline cellulose, povidone, stearic acid.
2 mg—D&C Yellow 10 aluminum lake, lactose, microcrystalline cellulose, povidone, stearic acid.
Pharmacodynamics
The dose-response relationship for blood pressure and adverse effects of guanfacine given once a day as monotherapy has been evaluated in patients with mild to moderate hypertension. In this study patients were randomized to placebo or to 0.5 mg, 1 mg, 2 mg, 3 mg, or 5 mg of Guanfacine. Results are shown in the following table. A useful effect was not observed overall until doses of 2 mg were reached, although responses in white patients were seen at 1 mg; 24 hour effectiveness of 1 mg to 3 mg doses was documented using 24 hour ambulatory monitoring. While the 5 mg dose added an increment of effectiveness, it caused an unacceptable increase in adverse reactions.

Controlled clinical trials in patients with mild to moderate hypertension who were receiving a thiazide-type diuretic have defined the dose-response relationship for blood pressure response and adverse reactions of guanfacine given at bedtime and have shown that the blood pressure response to guanfacine can persist for 24 hours after a single dose. In the 12-week placebo-controlled dose-response study, patients were randomized to placebo or to doses of 0.5, 1, 2, and 3 mg of guanfacine, in addition to 25 mg chlorthalidone, each given at bedtime. The observed mean changes from baseline, tabulated below, indicate the similarity of response for placebo and the 0.5 mg dose. Doses of 1, 2, and 3 mg resulted in decreased blood pressure in the sitting position with no real differences among the three doses. In the standing position, there was some increase in response with dose.

While most of the effectiveness of guanfacine in combination (and as monotherapy in white patients) was present at 1 mg, adverse reactions at this dose were not clearly distinguishable from those associated with placebo. Adverse reactions were clearly present at 2 and 3 mg.
In a second 12-week placebo-controlled study of 1, 2 or 3 mg of Guanfacine (guanfacine hydrochloride) administered with 25 mg of chlorthalidone once daily, a significant decrease in blood pressure was maintained for a full 24 hours after dosing. While there was no significant difference between the 12 and 24 hour blood pressure readings, the fall in blood pressure at 24 hours was numerically smaller, suggesting possible escape of blood pressure in some patients and the need for individualization of therapy.
In a double-blind, randomized trial, either guanfacine or clonidine was given at recommended doses with 25 mg chlorthalidone for 24 weeks and then abruptly discontinued. Results showed equal degrees of blood pressure reduction with the two drugs and there was no tendency for blood pressures to increase despite maintenance of the same daily dose of the two drugs. Signs and symptoms of rebound phenomena were infrequent upon discontinuation of either drug. Abrupt withdrawal of clonidine produced a rapid return of diastolic and especially systolic blood pressure to approximately pretreatment levels, with occasional values significantly greater than baseline, whereas guanfacine withdrawal produced a more gradual increase to pretreatment levels, but also with occasional values significantly greater than baseline.
Hemodynamic studies in man showed that the decrease in blood pressure observed after single-dose or long-term oral treatment with guanfacine was accompanied by a significant decrease in peripheral resistance and a slight reduction in heart rate (5 beats/min). Cardiac output under conditions of rest or exercise was not altered by guanfacine.
Guanfacine (guanfacine hydrochloride) lowered elevated plasma renin activity and plasma catecholamine levels in hypertensive patients, but this does not correlate with individual blood-pressure responses.
Growth hormone secretion was stimulated with single oral doses of 2 and 4 mg of guanfacine. Long-term use of Guanfacine had no effect on growth hormone levels.
Guanfacine had no effect on plasma aldosterone. A slight but insignificant decrease in plasma volume occurred after one month of guanfacine therapy. There were no changes in mean body weight or electrolytes.
Pharmacokinetics
Relative to an intravenous dose of 3 mg, the absolute oral bioavailability of guanfacine is about 80%. Peak plasma concentrations occur from 1 to 4 hours with an average of 2.6 hours after single oral doses or at steady state.
The area under the concentration-time curve (AUC) increases linearly with the dose.
In individuals with normal renal function, the average elimination half-life is approximately 17 hr (range 10 - 30 hr). Younger patients tend to have shorter elimination half-lives (13 - 14 hr) while older patients tend to have half-lives at the upper end of the range. Steady state blood levels were attained within 4 days in most subjects.
In individuals with normal renal function, guanfacine and its metabolites are excreted primarily in the urine. Approximately 50% (40 - 75%) of the dose is eliminated in the urine as unchanged drug; the remainder is eliminated mostly as conjugates of metabolites produced by oxidative metabolism of the aromatic ring.
The guanfacine-to-creatinine clearance ratio is greater than 1.0, which would suggest that tubular secretion of drug occurs.
The drug is approximately 70% bound to plasma proteins, independent of drug concentration.
The whole body volume of distribution is high (a mean of 6.3 L/kg), which suggests a high distribution of drug to the tissues.
The clearance of guanfacine in patients with varying degrees of renal insufficiency is reduced, but plasma levels of drug are only slightly increased compared to patients with normal renal function. When prescribing for patients with renal impairment, the low end of the dosing range should be used. Patients on dialysis also can be given usual doses of guanfacine hydrochloride as the drug is poorly dialyzed.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility No carcinogenic effect was observed in studies of 78 weeks in mice at doses more than 150 times the maximum recommended human dose and 102 weeks in rats at doses more than 100 times the maximum recommended human dose. In a variety of test models, guanfacine was not mutagenic. No adverse effects were observed in fertility studies in male and female rats.
Clinical Studies
FDA Package Insert for Guanfacine contains no information regarding clinical studies.
How Supplied
Guanfacine Tablets USP, 1 mg are available as white, round, flat-faced beveled-edge tablets, debossed “Є48” on one side and plain on the other side. These are supplied in bottles of 100 and 500. Guanfacine Tablets USP, 2 mg are available as yellow, round, flat-faced beveled-edge tablets, debossed “Є49” on one side and plain on the other side. These are supplied in bottles of 100 and 500.
Storage
Store at 20°-25°C (68°-77°F). Dispense in a tight, light-resistant container.
Images
Drug Images
{{#ask: Page Name::Guanfacine |?Pill Name |?Drug Name |?Pill Ingred |?Pill Imprint |?Pill Dosage |?Pill Color |?Pill Shape |?Pill Size (mm) |?Pill Scoring |?NDC |?Drug Author |format=template |template=DrugPageImages |mainlabel=- |sort=Pill Name }}
Package and Label Display Panel
{{#ask: Label Page::Guanfacine |?Label Name |format=template |template=DrugLabelImages |mainlabel=- |sort=Label Page }}
Patient Counseling Information
Patients who receive guanfacine should be advised to exercise caution when operating dangerous machinery or driving motor vehicles until it is determined that they do not become drowsy or dizzy from the medication. Patients should be warned that their tolerance for alcohol and other CNS depressants may be diminished. Patients should be advised not to discontinue therapy abruptly.
Precautions with Alcohol
Patients should be warned that their tolerance for alcohol and other CNS depressants may be diminished
Brand Names
- INTUNIV
- TENEX
Look-Alike Drug Names
GUANFACINE - GUAIFENESIN[8]
Drug Shortage Status
Price
References
The contents of this FDA label are provided by the National Library of Medicine.
- ↑ 1.0 1.1 Scahill L, Chappell PB, Kim YS, Schultz RT, Katsovich L, Shepherd E; et al. (2001). "A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder". Am J Psychiatry. 158 (7): 1067–74. PMID 11431228.
- ↑ Biederman J, Melmed RD, Patel A, McBurnett K, Konow J, Lyne A; et al. (2008). "A randomized, double-blind, placebo-controlled study of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder". Pediatrics. 121 (1): e73–84. doi:10.1542/peds.2006-3695. PMID 18166547.
- ↑ Sallee FR, McGough J, Wigal T, Donahue J, Lyne A, Biederman J; et al. (2009). "Guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder: a placebo-controlled trial". J Am Acad Child Adolesc Psychiatry. 48 (2): 155–65. doi:10.1097/CHI.0b013e318191769e. PMID 19106767.
- ↑ Sallee FR, Lyne A, Wigal T, McGough JJ (2009). "Long-term safety and efficacy of guanfacine extended release in children and adolescents with attention-deficit/hyperactivity disorder". J Child Adolesc Psychopharmacol. 19 (3): 215–26. doi:10.1089/cap.2008.0080. PMID 19519256.
- ↑ Chappell PB, Riddle MA, Scahill L, Lynch KA, Schultz R, Arnsten A; et al. (1995). "Guanfacine treatment of comorbid attention-deficit hyperactivity disorder and Tourette's syndrome: preliminary clinical experience". J Am Acad Child Adolesc Psychiatry. 34 (9): 1140–6. doi:10.1097/00004583-199509000-00010. PMID 7559307.
- ↑ 6.0 6.1 6.2 6.3 6.4 "Guanfacine (guanfacine) Tablet [Genpharm Inc.]". DailyMed. Genpharm Inc. March 2007. Retrieved 9 November 2013.
- ↑ 7.0 7.1 7.2 7.3 7.4 "guanfacine (Rx) - Guanfacine, Guanfacine". Medscape Reference. WebMD. Retrieved 9 November 2013.
- ↑ "https://www.ismp.org". External link in
|title=(help)
{{#subobject:
|Page Name=Guanfacine |Pill Name=No_image.jpg |Drug Name=guanfacine tablet |Pill Ingred=ANHYDROUS LACTOSE, CELLULOSE, MICROCRYSTALLINE, STARCH, CORN,, MAGNESIUM STEARATE, TALC|+sep=; |Pill Imprint=E48 |Pill Dosage=1 mg |Pill Color=White|+sep=; |Pill Shape=Round |Pill Size (mm)=7.00 |Pill Scoring= |Pill Image= |Drug Author=Epic Pharma, LLC |NDC=42806-048
}}
{{#subobject:
|Page Name=Guanfacine |Pill Name=No_image.jpg |Drug Name=guanfacine tablet |Pill Ingred=ANHYDROUS LACTOSE, CELLULOSE, MICROCRYSTALLINE, STARCH, CORN,, MAGNESIUM STEARATE, TALC|+sep=; |Pill Imprint=E49 |Pill Dosage=2 mg |Pill Color=Yellow|+sep=; |Pill Shape=Round |Pill Size (mm)=7.00 |Pill Scoring= |Pill Image= |Drug Author=Epic Pharma, LLC |NDC=42806-049
}}
{{#subobject:
|Label Page=Guanfacine |Label Name=Guanfacine_label_01.jpg
}}
{{#subobject:
|Label Page=Guanfacine |Label Name=Guanfacine_label_02.jpg
}}
{{#subobject:
|Label Page=Guanfacine |Label Name=Guanfacine_label_01.png
}}