Autonomic nervous system
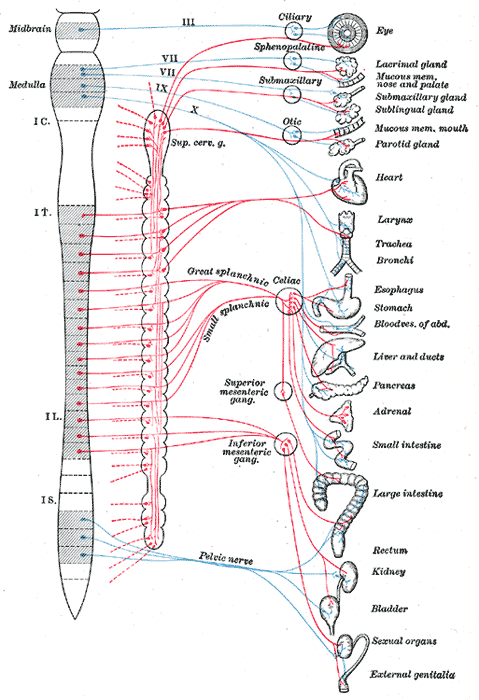
Blue = parasympathetic
Red = sympathetic
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview
The autonomic nervous system (ANS) (or visceral nervous system) is the part of the peripheral nervous system that acts as a control system, maintaining homeostasis in the body. These maintenance activities are primarily performed without conscious control or sensation. The ANS has far reaching effects, including: heart rate, digestion, respiration rate, salivation, perspiration, diameter of the pupils, micturition (the discharge of urine), and sexual arousal. Whereas most of its actions are involuntary, some ANS functions work in tandem with the conscious mind, such as breathing. Its main components are its sensory system, motor system (comprised of the parasympathetic nervous system and sympathetic nervous system), and the enteric nervous system.
The ANS is a classical term, widely used throughout the scientific and medical community. Its most useful definition could be: the sensory and motor neurons that innervate the viscera. These neurons form reflex arcs that pass through the lower brainstem or medulla oblongata. This explains that when the central nervous system (CNS) is damaged experimentally or by accident above that level, a vegetative life is still possible, whereby cardiovascular, digestive and respiratory functions are adequately regulated.
Anatomy
The reflex arcs of the ANS comprise a sensory (or afferent) arm, and a motor (or efferent, or effector) arm. The latter alone is represented on the figure.
Sensory neurons
The sensory arm is made of “primary visceral sensory neurons” found in the peripheral nervous system (PNS), in “cranial sensory ganglia”: the geniculate, petrosal and nodose ganglia, appended respectively to cranial nerves VII, IX and X. These sensory neurons monitor the levels of carbon dioxide, oxygen and sugar in the blood, arterial pressure and the chemical composition of the stomach and gut content. (They also convey the sense of taste, a conscious perception). Blood oxygen and carbon dioxide are in fact directly sensed by the carotid body, a small collection of chemosensors at the bifurcation of the carotid artery, innervated by the petrosal (IXth) ganglion.
Primary sensory neurons project (synapse) onto “second order” or relay visceral sensory neurons located in the medulla oblongata, forming the nucleus of the solitary tract (nTS), that integrates all visceral information. The nTS also receives input from a nearby chemosensory center, the area postrema, that detects toxins in the blood and the cerebrospinal fluid and is essential for chemically induced vomiting and conditional taste aversion (the memory that ensures that an animal which has been poisoned by a food never touches it again). All these visceral sensory informations constantly and unconsciously modulate the activity of the motor neurons of the ANS
Motor neurons
Motor neurons of the ANS are also located in ganglia of the PNS, called “autonomic ganglia”. They belong to three categories with different effects on their target organs (see below “Function”): sympathetic, parasympathetic and enteric.
Sympathetic ganglia are located in two sympathetic chains close to the spinal cord: the prevertebral and pre-aortic chains. Parasympathetic ganglia, in contrast, are located in close proximity to the target organ: the submandibular ganglion close to salivatory glands, paracardiac ganglia close to the heart etc… Enteric ganglia, which as their name implies innervate the digestive tube, are located inside its walls and collectively contain as many neurons as the entire spinal cord, including local sensory neurons, motor neurons and interneurons. It is the only truly autonomous part of the ANS and the digestive tube can function surprisingly well even in isolation. For that reason the enteric nervous system has been called “the second brain”.
The activity of autonomic ganglionic neurons is modulated by “preganglionic neurons” (also called improperly but classically "visceral motoneurons") located in the central nervous system. Preganglionc sympathetic neurons are in the spinal cord, at thoraco-lumbar levels. Preganglionic parasympathetic neurons are in the medulla oblongata (forming visceral motor nuclei: the dorsal motor nucleus of the vagus nerve (dmnX), the nucleus ambiguus, and salivatory nuclei) and in the sacral spinal cord. Enteric neurons are also modulated by input from the CNS, from preganglionic neurons located, like parasympathetic ones, in the medulla oblongata (in the dmnX).
The feedback from the sensory to the motor arm of visceral reflex pathways is provided by direct or indirect connections between the nucleus of the solitary tract and visceral motoneurons.
Function
Sympathetic and parasympathetic divisions typically function in opposition to each other. But this opposition is better termed complementary in nature rather than antagonistic. For an analogy, one may think of the sympathetic division as the accelerator and the parasympathetic division as the brake. The sympathetic division typically functions in actions requiring quick responses. The parasympathetic division functions with actions that do not require immediate reaction. Consider sympathetic as "fight or flight" and parasympathetic as "rest and digest".
However, many instances of sympathetic and parasympathetic activity cannot be ascribed to "fight" or "rest" situations. For example, standing up from a reclining or sitting position would entail an unsustainable drop in blood pressure if not for a compensatory increase in the arterial sympathetic tonus. Another example is the constant, second to second modulation of heart rate by sympathetic and parasympathetic influences, as a function of the respiratory cycles. More generally, these two systems should be seen as permanently modulating vital functions, in usually antagonistic fashion, to achieve homeostasis. Some typical actions of the sympathetic and parasympathetic systems are listed below:
Promotes a "fight or flight" response, corresponds with arousal and energy generation, inhibits digestion:
- Diverts blood flow away from the gastro-intestinal (GI) tract and skin via vasoconstriction.
- Blood flow to skeletal muscles, the lung is not only maintained, but enhanced (by as much as 1200%, in the case of skeletal muscles).
- Dilates bronchioles of the lung, which allows for greater alveolar oxygen exchange.
- Increases heart rate and the contractility of cardiac cells (myocytes), thereby providing a mechanism for the enhanced blood flow to skeletal muscles.
- Dilates pupils and relaxes the lens, allowing more light to enter the eye.
Promotes a *rest and digest" response; promotes calming of the nerves and return to regular function, enhances digestion.
- Dilates blood vessels leading to the GI tract, increasing blood flow. This is important following the consumption of food, due to the greater metabolic demands placed on the body by the gut.
- The parasympathetic nervous system can also constrict the bronchiolar diameter when the need for oxygen has diminished.
- During accommodation, the parasympathetic nervous system causes constriction of the pupil and lens.
- The parasympathetic nervous system stimulates salivary gland secretion, and accelerates peristalsis, so, in keeping with the rest and digest functions, appropriate PNS activity mediates digestion of food and indirectly, the absorption of nutrients.
- Is also involved in erection of genitals, via the pelvic splanchnic nerves 2–4.
Neurotransmitters and pharmacology
At the effector organs, sympathetic ganglionic neurons release noradrenaline (norepinephrine), along with other cotransmittors such as ATP, to act on adrenergic receptors, with the exception of the sweat glands and the adrenal medulla:
- acetycholine is the preganglionic neurotransmitter for both divisions of the ANS, as well as the postganglionic neurotransmitter of parasympathetic neurons. Nerves that release acetylcholine are said to be cholinergic. In the parasympathetic system, ganglionic neurons use acetylcholine as a neurotransmitter, to stimulate muscarinic receptors.
- At the adrenal cortex, there is no postsynaptic neuron. Instead the presynaptic neuron releases acetylcholine to act on nicotinic receptors.
- Stimulation of the adrenal medulla releases adrenaline (epinephrine) into the bloodstream which will act on adrenoceptors, producing a widespread increase in sympathetic activity.
The following table reviews the actions of these neurotransmitters as a function of their receptors.
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| cardiac output | β1, (β2): increases | M2: decreases |
SA node: heart rate (chronotropic) β1, (β2) [1]: increases M2: decreases Atrial cardiac muscle: contractility (inotropic) β1, (β2)[1]: increases M2: decreases Ventricular cardiac muscle β1, (β2):
increases contractility (inotropic)
increases cardiac muscle automaticity [2]--- at AV node β1:
increases conduction
increases cardiac muscle automaticity [2]M2:
decreases conduction
Atrioventricular block [2]
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| vascular smooth muscle | α: contracts; β2: relaxes | M3: relaxes [2] |
renal artery α1[3]: constricts --- larger coronary arteries α1 and α2[4]: constricts [2] --- smaller coronary arteries β2:dilates [5] --- arteries to viscera α: constricts --- arteries to skin α: constricts --- arteries to brain α1[6]: constricts [2] --- arteries to erectile tissue α1[7]: constricts M3: dilates arteries to salivary glands α: constricts M3: dilates hepatic artery β2: dilates --- arteries to skeletal muscle β2: dilates ---
Other
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| platelets | α2: aggregates | --- |
| mast cells - histamine | β2: inhibits | --- |
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| smooth muscles of bronchioles | β2: relaxes (major contribution) α1: contracts (minor contribution) |
M3: contracts |
The bronchioles have no sympathetic innervation, but are instead affected by circulating adrenaline [2]
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| pupil of eye | α1: relaxes | M3: contracts |
| ciliary muscle | β2: relaxes | M3: contracts |
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| salivary glands: secretions | β: stimulates viscous, amylase secretions α1: stimulates potassium cation |
M3: stimulates watery secretions |
| lacrimal glands (tears) | β2: Protein secretion [9] | M3: increases |
| kidney (renin) | β2: secretes | --- |
| parietal cells | --- | M1: Gastric acid secretion |
| liver | α1, β2: glycogenolysis, gluconeogenesis | --- |
| adipose cells | β3: stimulates lipolysis | --- |
| GI tract (smooth muscle) motility | α1, α2[10], β2: decreases | M3, (M1) [1]: increases |
| sphincters of GI tract | α2 [2], β2: contracts | M3: relaxes |
| glands of GI tract | no effect [2] | M3: secretes |
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| pancreas (islets) | α2: decreases secretion from beta cells, increases secretion from alpha cells | increases stimulation from alpha cells and beta cells |
| adrenal medulla | N: secretes Acetylcholine | --- |
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| Detrusor urinae muscle of bladder wall | β2: relaxes | contracts |
| ureter | α1: contracts | relaxes |
| sphincter | α1: contracts; β2 relaxes | relaxes |
| Target | Sympathetic (adrenergic) | Parasympathetic (muscarinic) |
| uterus | α1: contracts (pregnant[2]) β2: relaxes (non-pregnant[2]) |
--- |
| genitalia | α: contracts (ejaculation) | M3: erection |
| Target | Sympathetic (muscarinic and adrenergic) | Parasympathetic (muscarinic) |
| sweat gland secretions | M: stimulates (major contribution); α1: stimulates (minor contribution) | --- |
| arrector pili | α1: stimulates | --- |
See also
References
- ↑ 1.0 1.1 1.2 "ref name=Rang" mentions only the one without brackets
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 Pharmacology, (Rang, Dale, Ritter & Moore, ISBN 0443071454, 5:th ed., Churchill Livingstone 2003). Page 127
- ↑ Renal alpha-1 and alpha-2 adrenergic receptors: biochemical and pharmacological correlations JM Schmitz, RM Graham, A Sagalowsky and WA Pettinger
- ↑ Coronary vasoconstriction mediated by alpha 1- and alpha 2-adrenoceptors in conscious dogs O. L. Woodman and S. F. Vatner
- ↑ Rang, H. P. (2003). Pharmacology. Edinburgh: Churchill Livingstone. ISBN 0-443-07145-4. Page 270
- ↑ Circulation & Lung Physiology I M.A.S.T.E.R. Learning Program, UC Davis School of Medicine
- ↑ 1A-Adrenoceptors mediate contractions to phenylephrine in rabbit penile arteries J S Morton1, C J Daly1, V M Jackson2 and J C McGrath1: "1A-ARs could be utilized to aid the erectile response in male erectile dysfunction sufferers by reducing vasoconstriction of the penile arteries"
- ↑ [http://www.ingentaconnect.com/content/bsc/jvpt/1997/00000020/00000004/art00009;jsessionid=8lm5thggpj1x.alice?format=print IngentaConnect Alpha-adrenoceptors in equine digital veins ...
- ↑ Protein secretion induced by isoproterenol or pentoxifylline in lacrimal gland P. Mauduit, G. Herman and B. Rossignol
- ↑ Involvement of alpha-1 and alpha-2 adrenoceptors in the postlaparotomy intestinal motor disturbances in the rat. A Sagrada, M J Fargeas, and L Bueno
External links
Template:Nervous system
Template:Autonomic
ar:جهاز عصبي تلقائي
bs:Vegetativni nervni sistem
da:Autonome nervesystem
de:Vegetatives Nervensystem
dv:އުޓޮނޮމިކް ނާރވަސް ސިސްޓަމް
fa:سامانه عصبی خودگردان
is:Dultaugakerfið
it:Sistema nervoso autonomo
he:מערכת העצבים האוטונומית
mk:Вегетативен нервен систем
nl:Autonoom zenuwstelsel
no:Det autonome nervesystem
simple:Autonomic nervous system
sl:Avtonomno živčevje
sr:Аутономни нервни систем
fi:Autonominen hermosto
uk:Автономна нервова система