Beta blockers: Difference between revisions
Matt Pijoan (talk | contribs) m (Protected "Beta-blockers": Protecting pages from unwanted edits ([edit=sysop] (indefinite) [move=sysop] (indefinite))) |
m (Bot: Adding CME Category::Cardiology) |
||
| (8 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
'''For patient information click '''[[Beta-blockers (patient information)|here]]''' | |||
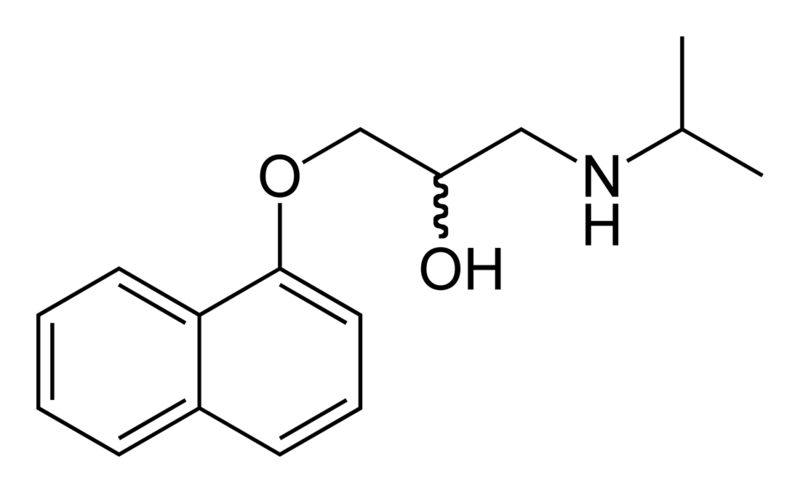
[[Image:Propranolol-2D-skeletal.png|thumb|[[Skeletal formula]] of [[propranolol]], the first clinically successful beta blocker]] | [[Image:Propranolol-2D-skeletal.png|thumb|[[Skeletal formula]] of [[propranolol]], the first clinically successful beta blocker]] | ||
{{SI}} | {{SI}} | ||
{{CMG}} | {{CMG}} | ||
'''''Synonyms and Kewords:''''' Beta-adrenergic blocking agents, beta-adrenergic antagonists, or beta antagonists. | |||
'''''Synonyms:''''' Beta | |||
==Overview== | |||
'''Beta blockers''' (sometimes written as '''β-blockers''') are a class of [[medication|drugs]] used for various indications, but particularly for the management of [[cardiac arrhythmia]]s and cardioprotection after [[myocardial infarction]]. Whilst once first-line treatment for [[hypertension]], their role was downgraded in June 2006 in the United Kingdom to fourth-line as they do not perform as well as other drugs, particularly in the elderly, and there is increasing evidence that the most frequently used beta-blockers especially in combination with [[thiazide]]-type diuretics carry an unacceptable risk of provoking [[Diabetes mellitus type 2|type 2 diabetes]].<ref name="ref1">{{cite web | author= Sheetal Ladva | title=NICE and BHS launch updated hypertension guideline | url=http://www.nelm.nhs.uk/Record%20Viewing/viewRecord.aspx?id=567178 | date=28/06/2006 | publisher=[[National Institute for Health and Clinical Excellence]] }}</ref> | '''Beta blockers''' (sometimes written as '''β-blockers''') are a class of [[medication|drugs]] used for various indications, but particularly for the management of [[cardiac arrhythmia]]s and cardioprotection after [[myocardial infarction]]. Whilst once first-line treatment for [[hypertension]], their role was downgraded in June 2006 in the United Kingdom to fourth-line as they do not perform as well as other drugs, particularly in the elderly, and there is increasing evidence that the most frequently used beta-blockers especially in combination with [[thiazide]]-type diuretics carry an unacceptable risk of provoking [[Diabetes mellitus type 2|type 2 diabetes]].<ref name="ref1">{{cite web | author= Sheetal Ladva | title=NICE and BHS launch updated hypertension guideline | url=http://www.nelm.nhs.uk/Record%20Viewing/viewRecord.aspx?id=567178 | date=28/06/2006 | publisher=[[National Institute for Health and Clinical Excellence]] }}</ref> | ||
[[Propranolol]] was the first clinically useful beta adrenergic [[receptor antagonist]]. Invented by Sir [[James W. Black]], it revolutionized the medical management of [[angina pectoris]] and is considered to be one of the most important contributions to clinical medicine and [[pharmacology]] of the 20th century.<ref name="propranolol">{{cite web | year=1997| url=http://texasheart.org/Education/THIJournal/SIRJAMES.cfm | author=Melanie Patricia Stapleton | title=Sir James Black and Propranolol | publisher=Texas Heart Institute Journal }}</ref> | [[Propranolol]] was the first clinically useful beta adrenergic [[receptor antagonist]]. Invented by Sir [[James W. Black]], it revolutionized the medical management of [[angina pectoris]] and is considered to be one of the most important contributions to clinical medicine and [[pharmacology]] of the 20th century.<ref name="propranolol">{{cite web | year=1997| url=http://texasheart.org/Education/THIJournal/SIRJAMES.cfm | author=Melanie Patricia Stapleton | title=Sir James Black and Propranolol | publisher=Texas Heart Institute Journal }}</ref> | ||
== Pharmacology == | ==Pharmacology== | ||
Beta blockers block the action of [[endogenous]] [[catecholamine]]s ([[epinephrine]] (adrenaline) and [[norepinephrine]] (noradrenaline) in particular), on β-[[adrenergic receptor]]s, part of the [[sympathetic nervous system]] which mediates the "[[fight or flight]]" response. | Beta blockers block the action of [[endogenous]] [[catecholamine]]s ([[epinephrine]] (adrenaline) and [[norepinephrine]] (noradrenaline) in particular), on β-[[adrenergic receptor]]s, part of the [[sympathetic nervous system]] which mediates the "[[fight or flight]]" response. | ||
| Line 48: | Line 47: | ||
Beta blockers can impair the relaxation of bronchial muscle (mediated by beta-2) and so should be avoided by asthmatics. | Beta blockers can impair the relaxation of bronchial muscle (mediated by beta-2) and so should be avoided by asthmatics. | ||
== Clinical use == | ==Clinical use== | ||
Large differences exist in the pharmacology of agents within the class, thus not all beta blockers are used for all indications listed below. | Large differences exist in the pharmacology of agents within the class, thus not all beta blockers are used for all indications listed below. | ||
| Line 59: | Line 58: | ||
* [[Myocardial infarction]] | * [[Myocardial infarction]] | ||
* [[Glaucoma]] | * [[Glaucoma]] | ||
* [[Migraine | * [[Migraine secondary prevention|Migraine (secondary prevention)]] | ||
* Symptomatic control ([[tachycardia]], [[tremor]]) in [[anxiety]] and [[hyperthyroidism]] | * Symptomatic control ([[tachycardia]], [[tremor]]) in [[anxiety]] and [[hyperthyroidism]] | ||
* [[Essential tremor]] | * [[Essential tremor]] | ||
| Line 86: | Line 85: | ||
Since they lower heart rate and reduce tremor, beta blockers have been used by some Olympic marksmen to enhance performance, though beta blockers are banned by the International Olympic Committee (IOC).<ref name="ref4">{{cite web | author= World Anti-Doping Agency | title=The World Anti-Doping Code: The 2006 Prohibited List International Standard | url=http://multimedia.olympic.org/pdf/en_report_1037.pdf | date=19/09/2005 | publisher=[[World Anti-Doping Agency]]}}</ref> Although they have no recognisable benefit to most sports, it is acknowledged that they are beneficial to sports such as archery and shooting. | Since they lower heart rate and reduce tremor, beta blockers have been used by some Olympic marksmen to enhance performance, though beta blockers are banned by the International Olympic Committee (IOC).<ref name="ref4">{{cite web | author= World Anti-Doping Agency | title=The World Anti-Doping Code: The 2006 Prohibited List International Standard | url=http://multimedia.olympic.org/pdf/en_report_1037.pdf | date=19/09/2005 | publisher=[[World Anti-Doping Agency]]}}</ref> Although they have no recognisable benefit to most sports, it is acknowledged that they are beneficial to sports such as archery and shooting. | ||
== Adverse effects == | ==Adverse effects== | ||
[[Adverse drug reaction]]s (ADRs) associated with the use of beta blockers include: [[nausea]], [[diarrhea]], [[bronchospasm]], [[dyspnea]], cold extremities, exacerbation of [[Raynaud's syndrome]], [[bradycardia]], [[hypotension]], [[heart failure]], [[heart block]], [[fatigue (medical)|fatigue]], [[dizziness]], abnormal vision, decreased concentration, [[hallucinations]], [[insomnia]], nightmares, [[clinical depression]], [[sexual dysfunction]], [[erectile dysfunction]] and/or alteration of [[glucose]] and [[lipid]] [[metabolism]]. Mixed α<sub>1</sub>/β-antagonist therapy is also commonly associated with [[orthostatic hypotension]]. [[Carvedilol]] therapy is commonly associated with [[edema]].<ref name="Rossi"/> | [[Adverse drug reaction]]s (ADRs) associated with the use of beta blockers include: [[nausea]], [[diarrhea]], [[bronchospasm]], [[dyspnea]], cold extremities, exacerbation of [[Raynaud's syndrome]], [[bradycardia]], [[hypotension]], [[heart failure]], [[heart block]], [[fatigue (medical)|fatigue]], [[dizziness]], abnormal vision, decreased concentration, [[hallucinations]], [[insomnia]], nightmares, [[clinical depression]], [[sexual dysfunction]], [[erectile dysfunction]] and/or alteration of [[glucose]] and [[lipid]] [[metabolism]]. Mixed α<sub>1</sub>/β-antagonist therapy is also commonly associated with [[orthostatic hypotension]]. [[Carvedilol]] therapy is commonly associated with [[edema]].<ref name="Rossi"/> | ||
| Line 99: | Line 98: | ||
An October 2008 meta-analysis by Dr. Sripal Bangalore, et al. suggests that hypertensive patients who have a reduced heart rate as a result of beta-blocker therapy face an increased risk of cardiovascular events and death. The analysis pooled data from 9 randomized clinical trials that evaluated using beta-blockers as a primary treatment of hypertension, and included 34,096 patients who received beta-blockers, 30,139 patients who received other antihypertensive drugs, and 3,987 patients who received a placebo. Patients who had a reduced heart rate as result of beta-blocker therapy had a greater risk of all-cause mortality, cardiovascular mortality, myocardial infarction, stroke , and heart failure. The study's authors suggested that these increased risks could be due to the increase in central aortic pressure and/or pulse pressure resulting from beta-blocker use. A major limitation of the study is the fact that that the majority of patients received atenolol, so the findings may not translate to all beta-blockers.<ref> {{cite journal |author=Sripal Bangalore, MD, MHA, Sabrina Sawhney, MD and Franz H. Messerli, MD |title=Relation of Beta-Blocker–Induced Heart Rate Lowering and Cardioprotection in Hypertension |journal=JACC |issue=52 |pages=1482-1489 |year=2008}}</ref> | An October 2008 meta-analysis by Dr. Sripal Bangalore, et al. suggests that hypertensive patients who have a reduced heart rate as a result of beta-blocker therapy face an increased risk of cardiovascular events and death. The analysis pooled data from 9 randomized clinical trials that evaluated using beta-blockers as a primary treatment of hypertension, and included 34,096 patients who received beta-blockers, 30,139 patients who received other antihypertensive drugs, and 3,987 patients who received a placebo. Patients who had a reduced heart rate as result of beta-blocker therapy had a greater risk of all-cause mortality, cardiovascular mortality, myocardial infarction, stroke , and heart failure. The study's authors suggested that these increased risks could be due to the increase in central aortic pressure and/or pulse pressure resulting from beta-blocker use. A major limitation of the study is the fact that that the majority of patients received atenolol, so the findings may not translate to all beta-blockers.<ref> {{cite journal |author=Sripal Bangalore, MD, MHA, Sabrina Sawhney, MD and Franz H. Messerli, MD |title=Relation of Beta-Blocker–Induced Heart Rate Lowering and Cardioprotection in Hypertension |journal=JACC |issue=52 |pages=1482-1489 |year=2008}}</ref> | ||
== Examples of beta blockers == | ==Examples of beta blockers== | ||
[[Image:Dichloroisoprenaline.png|thumb|Dichloroisoprenaline, the first beta blocker.|200px|right]] | [[Image:Dichloroisoprenaline.png|thumb|Dichloroisoprenaline, the first beta blocker.|200px|right]] | ||
| Line 106: | Line 105: | ||
*[[Carteolol]] | *[[Carteolol]] | ||
*[[Levobunolol]] | *[[Levobunolol]] | ||
*Mepindolol | *[[Mepindolol]] | ||
*[[Metipranolol]] | *[[Metipranolol]] | ||
*[[Nadolol]] | *[[Nadolol]] | ||
| Line 160: | Line 159: | ||
==References== | ==References== | ||
{{reflist|2}} | {{reflist|2}} | ||
{{Beta blockers}} | {{Beta blockers}} | ||
| Line 174: | Line 165: | ||
{{Major Drug Groups}} | {{Major Drug Groups}} | ||
{{Receptor agonists and antagonists}} | {{Receptor agonists and antagonists}} | ||
{{WikiDoc Help Menu}} | {{WikiDoc Help Menu}} | ||
{{WikiDoc Sources}} | {{WikiDoc Sources}} | ||
[[CME Category::Cardiology]] | |||
[[Category:Beta blockers]] | |||
[[Category:Antihypertensive agents]] | |||
[[Category:Drug]] | |||
[[Category:Cardiology]] | |||
Latest revision as of 05:00, 15 March 2016
For patient information click here
|
WikiDoc Resources for Beta blockers |
|
Articles |
|---|
|
Most recent articles on Beta blockers Most cited articles on Beta blockers |
|
Media |
|
Powerpoint slides on Beta blockers |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Beta blockers at Clinical Trials.gov Trial results on Beta blockers Clinical Trials on Beta blockers at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Beta blockers NICE Guidance on Beta blockers
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Beta blockers Discussion groups on Beta blockers Patient Handouts on Beta blockers Directions to Hospitals Treating Beta blockers Risk calculators and risk factors for Beta blockers
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Beta blockers |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Synonyms and Kewords: Beta-adrenergic blocking agents, beta-adrenergic antagonists, or beta antagonists.
Overview
Beta blockers (sometimes written as β-blockers) are a class of drugs used for various indications, but particularly for the management of cardiac arrhythmias and cardioprotection after myocardial infarction. Whilst once first-line treatment for hypertension, their role was downgraded in June 2006 in the United Kingdom to fourth-line as they do not perform as well as other drugs, particularly in the elderly, and there is increasing evidence that the most frequently used beta-blockers especially in combination with thiazide-type diuretics carry an unacceptable risk of provoking type 2 diabetes.[1]
Propranolol was the first clinically useful beta adrenergic receptor antagonist. Invented by Sir James W. Black, it revolutionized the medical management of angina pectoris and is considered to be one of the most important contributions to clinical medicine and pharmacology of the 20th century.[2]
Pharmacology
Beta blockers block the action of endogenous catecholamines (epinephrine (adrenaline) and norepinephrine (noradrenaline) in particular), on β-adrenergic receptors, part of the sympathetic nervous system which mediates the "fight or flight" response.
There are three known types of beta receptor, designated β1, β2 and β3. β1-Adrenergic receptors are located mainly in the heart and in the kidneys. β2-Adrenergic receptors are located mainly in the lungs, gastrointestinal tract, liver, uterus, vascular smooth muscle, and skeletal muscle. β3-receptors are located in fat cells.
β-Receptor antagonism
Stimulation of β1 receptors by epinephrine induces a positive chronotropic and inotropic effect on the heart and increases cardiac conduction velocity and automaticity. Stimulation of β1 receptors on the kidney causes renin release. Stimulation of β2 receptors induces smooth muscle relaxation (resulting in vasodilation and bronchodilation amongst other actions), induces tremor in skeletal muscle, and increases glycogenolysis in the liver and skeletal muscle. Stimulation of β3 receptors induces lipolysis.
Beta blockers inhibit these normal epinephrine-mediated sympathetic actions, but have minimal effect on resting subjects. That is, they reduce the effect of excitement/physical exertion on heart rate and force of contraction, dilation of blood vessels and opening of bronchi, and also reduce tremor and breakdown of glycogen.
It is therefore expected that non-selective beta blockers have an antihypertensive effect. The antihypertensive mechanism appears to involve: reduction in cardiac output (due to negative chronotropic and inotropic effects), reduction in renin release from the kidneys, and a central nervous system effect to reduce sympathetic activity.
Antianginal effects result from negative chronotropic and inotropic effects, which decrease cardiac workload and oxygen demand.
The antiarrhythmic effects of beta blockers arise from sympathetic nervous system blockade – resulting in depression of sinus node function and atrioventricular node conduction, and prolonged atrial refractory periods. Sotalol, in particular, has additional antiarrhythmic properties and prolongs action potential duration through potassium channel blockade.
Blockade of the sympathetic nervous system on renin release leads to reduced aldosterone via the renin angiotensin aldosterone system with a resultant decrease in blood pressure due to decreased sodium and water retention.
Intrinsic sympathomimetic activity
Some beta blockers (e.g. oxprenolol and pindolol) exhibit intrinsic sympathomimetic activity (ISA). These agents are capable of exerting low level agonist activity at the β-adrenergic receptor while simultaneously acting as a receptor site antagonist. These agents, therefore, may be useful in individuals exhibiting excessive bradycardia with sustained beta blocker therapy.
Agents with ISA are not used in post-myocardial infarction as they have not been demonstrated to be beneficial. They may also be less effective than other beta blockers in the management of angina and tachyarrhythmia.[3]
α1-Receptor antagonism
Some beta blockers (e.g. labetalol and carvedilol) exhibit mixed antagonism of both β- and α1-adrenergic receptors, which provides additional arteriolar vasodilating action.
Other effects
Beta blockers decrease nocturnal melatonin release, perhaps partly accounting for sleep disturbance caused by some agents.[4] Beta blockers protect against social anxiety: "Improvement of physical symptoms has been demonstrated with beta-blockers such as propranolol; however, these effects are limited to the social anxiety experienced in performance situations." [5] Beta blockers can impair the relaxation of bronchial muscle (mediated by beta-2) and so should be avoided by asthmatics.
Clinical use
Large differences exist in the pharmacology of agents within the class, thus not all beta blockers are used for all indications listed below.
Indications for beta blockers include:
- Hypertension
- Angina
- Mitral valve prolapse
- Cardiac arrhythmia
- Congestive heart failure
- Myocardial infarction
- Glaucoma
- Migraine (secondary prevention)
- Symptomatic control (tachycardia, tremor) in anxiety and hyperthyroidism
- Essential tremor
- Phaeochromocytoma, in conjunction with α-blocker
Beta blockers have also been used in the following conditions:
- Hypertrophic obstructive cardiomyopathy
- Acute dissecting aortic aneurysm
- Marfan syndrome (chronic treatment with propranolol slows progression of aortic dilation and its complications)
- Prevention of variceal bleeding in portal hypertension
- Possible mitigation of hyperhidrosis
Congestive heart failure
Although beta blockers were once contraindicated in congestive heart failure, as they have the potential to worsen the condition, studies in the late 1990s showed their positive effects on morbidity and mortality in congestive heart failure.[6] [7] [8] Bisoprolol, carvedilol and sustained-release metoprolol are specifically indicated as adjuncts to standard ACE inhibitor and diuretic therapy in congestive heart failure.
The beta blockers are a benefit due to the reduction of the heart rate which will lower the myocardial energy expenditure. This is turns prolongs the diastolic filling and lengthens coronary perfusion.[9] Beta blockers have also been a benefit to improving the ejection fraction of the heart despite an initial reduction in it.
Trials have shown that Beta blockers reduce the absolute risk of death by 4.5% over a 13 month period. As well as reducing the risk of mortality, the number of hospital visits and hospitalizations were also reduced in the trials.[9]
Anxiety and performance enhancement
Some people, particularly musicians, use beta blockers to avoid stage fright and tremor during public performance and auditions. The physiological symptoms of the fight/flight response associated with performance anxiety and panic (pounding heart, cold/clammy hands, increased respiration, sweating, etc.) are significantly reduced, thus enabling anxious individuals to concentrate on the task at hand. Officially, beta blockers are not approved for anxiolytic use by the U.S. Food and Drug Administration. [10]
Since they lower heart rate and reduce tremor, beta blockers have been used by some Olympic marksmen to enhance performance, though beta blockers are banned by the International Olympic Committee (IOC).[11] Although they have no recognisable benefit to most sports, it is acknowledged that they are beneficial to sports such as archery and shooting.
Adverse effects
Adverse drug reactions (ADRs) associated with the use of beta blockers include: nausea, diarrhea, bronchospasm, dyspnea, cold extremities, exacerbation of Raynaud's syndrome, bradycardia, hypotension, heart failure, heart block, fatigue, dizziness, abnormal vision, decreased concentration, hallucinations, insomnia, nightmares, clinical depression, sexual dysfunction, erectile dysfunction and/or alteration of glucose and lipid metabolism. Mixed α1/β-antagonist therapy is also commonly associated with orthostatic hypotension. Carvedilol therapy is commonly associated with edema.[3]
Central nervous system (CNS) adverse effects (hallucinations, insomnia, nightmares, depression) are more common in agents with greater lipid solubility, which are able to cross the blood-brain barrier into the CNS. Similarly, CNS adverse effects are less common in agents with greater aqueous solubility (listed below).
Adverse effects associated with β2-adrenergic receptor antagonist activity (bronchospasm, peripheral vasoconstriction, alteration of glucose and lipid metabolism) are less common with β1-selective (often termed "cardioselective") agents, however receptor selectivity diminishes at higher doses. Beta blockade, especially of the beta-1 receptor at the macula densa inhibits renin release, thus decreasing the release of aldosterone. This causes hyponatremia and hyperkalemia.
A 2007 study revealed that diuretics and beta-blockers used for hypertension increase a patient's risk of developing diabetes whilst ACE inhibitors and Angiotensin II receptor antagonists (Angiotensin Receptor Blockers) actually decrease the risk of diabetes.[12] Clinical guidelines in Great Britain, but not in the United States, call for avoiding diuretics and beta-blockers as first-line treatment of hypertension due to the risk of diabetes.[13]
Beta blockers must not be used in the treatment of cocaine, amphetamine, or other alpha adrenergic stimulant overdose. The blockade of only beta receptors increases hypertension, reduces coronary blood flow, left ventricular function, and cardiac output and tissue perfusion by means of leaving the alpha adrenergic system stimulation unopposed. [14] The appropriate antihypertensive drugs to administer during hypertensive crisis resulting from stimulant abuse are vasodilators like nitroglycerin, diuretics like furosemide and alpha blockers like phentolamine. [15]
An October 2008 meta-analysis by Dr. Sripal Bangalore, et al. suggests that hypertensive patients who have a reduced heart rate as a result of beta-blocker therapy face an increased risk of cardiovascular events and death. The analysis pooled data from 9 randomized clinical trials that evaluated using beta-blockers as a primary treatment of hypertension, and included 34,096 patients who received beta-blockers, 30,139 patients who received other antihypertensive drugs, and 3,987 patients who received a placebo. Patients who had a reduced heart rate as result of beta-blocker therapy had a greater risk of all-cause mortality, cardiovascular mortality, myocardial infarction, stroke , and heart failure. The study's authors suggested that these increased risks could be due to the increase in central aortic pressure and/or pulse pressure resulting from beta-blocker use. A major limitation of the study is the fact that that the majority of patients received atenolol, so the findings may not translate to all beta-blockers.[16]
Examples of beta blockers
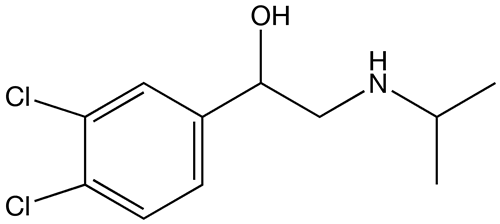
Non-selective agents
- Alprenolol
- Carteolol
- Levobunolol
- Mepindolol
- Metipranolol
- Nadolol
- Oxprenolol
- Penbutolol
- Pindolol
- Propranolol
- Sotalol
- Timolol
β1-Selective agents
Mixed α1/β-adrenergic antagonists
β2-Selective agents
- Butaxamine (weak α-adrenergic agonist activity)
Comparative information
Pharmacological differences
- Agents with intrinsic sympathomimetic action (ISA)
- Acebutolol, carteolol, celiprolol, mepindolol, oxprenolol, pindolol
- Agents with greater aqueous solubility
- Atenolol, celiprolol, nadolol, sotalol
- Agents with membrane stabilising activity
- Acebutolol, betaxolol, pindolol, propranolol
- Agents with antioxidant effect
- Carvedilol
- Nebivolol
Indication differences
- Agents specifically indicated for cardiac arrhythmia
- Agents specifically indicated for congestive heart failure
- Agents specifically indicated for glaucoma
- Agents specifically indicated for myocardial infarction
- Agents specifically indicated for migraine prophylaxis
Propranolol is the only agent indicated for control of tremor, portal hypertension and esophageal variceal bleeding, and used in conjunction with α-blocker therapy in phaeochromocytoma.[3]
References
- ↑ Sheetal Ladva (28/06/2006). "NICE and BHS launch updated hypertension guideline". National Institute for Health and Clinical Excellence. Check date values in:
|date=(help) - ↑ Melanie Patricia Stapleton (1997). "Sir James Black and Propranolol". Texas Heart Institute Journal.
- ↑ 3.0 3.1 3.2 Editor Rossi S, ed. (2006). Australian Medicines Handbook. Adelaide: Australian Medicines Handbook.
- ↑ Stoschitzky K, Sakotnik A, Lercher P; et al. (1999). "Influence of beta-blockers on melatonin release". Eur. J. Clin. Pharmacol. 55 (2): 111–5. PMID 10335905.
- ↑ Davidson, M.D., Jonathan (1999). "Social Anxiety Disorder: A Treatable Condition". Drug Benefit Trends 11(5). Cliggott Publishing, Division of SCP Communications. pp. 5BH–7BH. Unknown parameter
|coauthors=ignored (help) - ↑ Hjalmarson A, Goldstein S, Fagerberg B; et al. (2000). "Effects of controlled-release metoprolol on total mortality, hospitalizations, and well-being in patients with heart failure: the Metoprolol CR/XL Randomized Intervention Trial in congestive heart failure (MERIT-HF). MERIT-HF Study Group". JAMA. 283 (10): 1295–302. PMID 10714728.
- ↑ Leizorovicz A, Lechat P, Cucherat M, Bugnard F (2002). "Bisoprolol for the treatment of chronic heart failure: a meta-analysis on individual data of two placebo-controlled studies--CIBIS and CIBIS II. Cardiac Insufficiency Bisoprolol Study". Am. Heart J. 143 (2): 301–7. PMID 11835035.
- ↑ Packer M, Fowler MB, Roecker EB; et al. (2002). "Effect of carvedilol on the morbidity of patients with severe chronic heart failure: results of the carvedilol prospective randomized cumulative survival (COPERNICUS) study". Circulation. 106 (17): 2194–9. PMID 12390947.
- ↑ 9.0 9.1 Pritchett AM, Redfield MM (2002). "Beta-blockers: new standard therapy for heart failure" (PDF). Mayo Clin. Proc. 77 (8): 839–45, quiz 845–6. PMID 12173717.
- ↑ Schneier FR (2006). "Clinical practice. Social anxiety disorder". N. Engl. J. Med. 355 (10): 1029–36. doi:10.1056/NEJMcp060145. PMID 16957148.
- ↑ World Anti-Doping Agency (19/09/2005). "The World Anti-Doping Code: The 2006 Prohibited List International Standard" (PDF). World Anti-Doping Agency. Check date values in:
|date=(help) - ↑ Elliott WJ, Meyer PM (2007). "Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis". Lancet. 369 (9557): 201–7. doi:10.1016/S0140-6736(07)60108-1. PMID 17240286.
- ↑ Mayor S (2006). "NICE removes beta blockers as first line treatment for hypertension". BMJ. 333 (7557): 8. doi:10.1136/bmj.333.7557.8-a. PMID 16809680.
- ↑ http://www.emedicine.com/med/topic400.htm
- ↑ http://www.emedicine.com/EMERG/topic23.htm
- ↑ Sripal Bangalore, MD, MHA, Sabrina Sawhney, MD and Franz H. Messerli, MD (2008). "Relation of Beta-Blocker–Induced Heart Rate Lowering and Cardioprotection in Hypertension". JACC (52): 1482–1489.
- ↑ Bisoprolol MedlinePlus
Template:Antiglaucoma preparations and miotics Template:Major Drug Groups Template:Receptor agonists and antagonists