Sorafenib
{{DrugProjectFormSinglePage |authorTag=Alberto Plate [1] |genericName=Sorafenib |aOrAn=a |drugClass=kinase inhibitor |indicationType=treatment |indication=unresectable hepatocellular carcinoma, advanced renal cell carcinoma, locally recurrent or metastatic, progressive, differentiated thyroid carcinoma refractory to radioactive iodine treatment |adverseReactions=hypertension, acral erythema, alopecia, peeling of skin, rash, hypoalbuminemia, hypocalcemia, hypophosphatemia, raised TSH level, weight decreased, abdominal pain, decrease in appetite, diarrhea, Increased serum lipase level, anorexia, nausea, serum amylase raised, lymphocytopenia, thrombocytopenia, ALT/SGPT level raised, infections, fatigue and pain |blackBoxWarningTitle=TITLE |blackBoxWarningBody=Condition Name: (Content) |fdaLIADAdult======Recommended Dose for Hepatocellular Carcinoma, Renal Cell Carcinoma, and Differentiated Thyroid Carcinoma=====
- Dosage: 200 mg q12h, taken 1 hour before or 2 hours after a meal. Treatment should continue until the patient is no longer clinically benefiting from therapy or until unacceptable toxicity occurs. Temporary interruption of Sorafenib is recommended in patients undergoing major surgical procedures.
- Temporary interruption or permanent discontinuation of Sorafenib may be required for the following:
- Cardiac ischemia or infarction
- Hemorrhage requiring medical intervention
- Severe or persistent hypertension despite adequate anti-hypertensive therapy
- Gastrointestinal perforation
- QTc prolongation
- Severe drug-induced liver injury
- Temporary interruption or permanent discontinuation of Sorafenib may be required for the following:
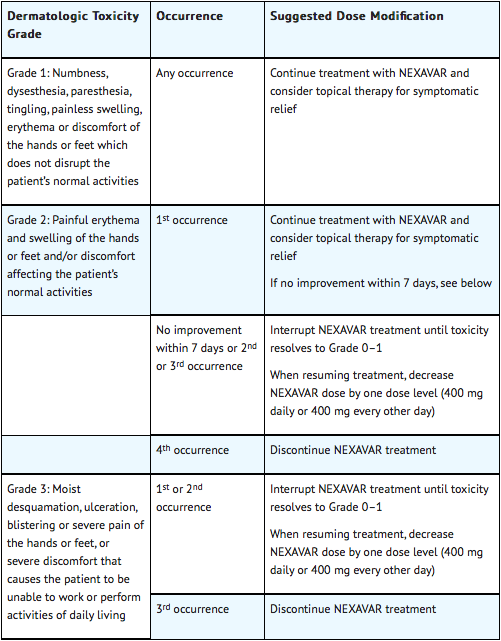
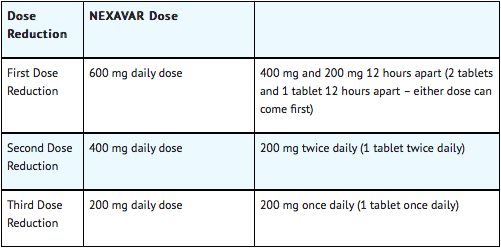
Dose modifications for Hepatocellular Carcinoma and Renal Cell Carcinoma
When dose reduction is necessary, the Sorafenib dose may be reduced to 400 mg once daily. If additional dose reduction is required, Sorafenib may be reduced to a single 400 mg dose every other day. If dermatological toxicity presented, the following scheme should be followed:
Dose Modifications for Differentiated Thyroid Carcinoma
Dose Modification in Skin Toxicity
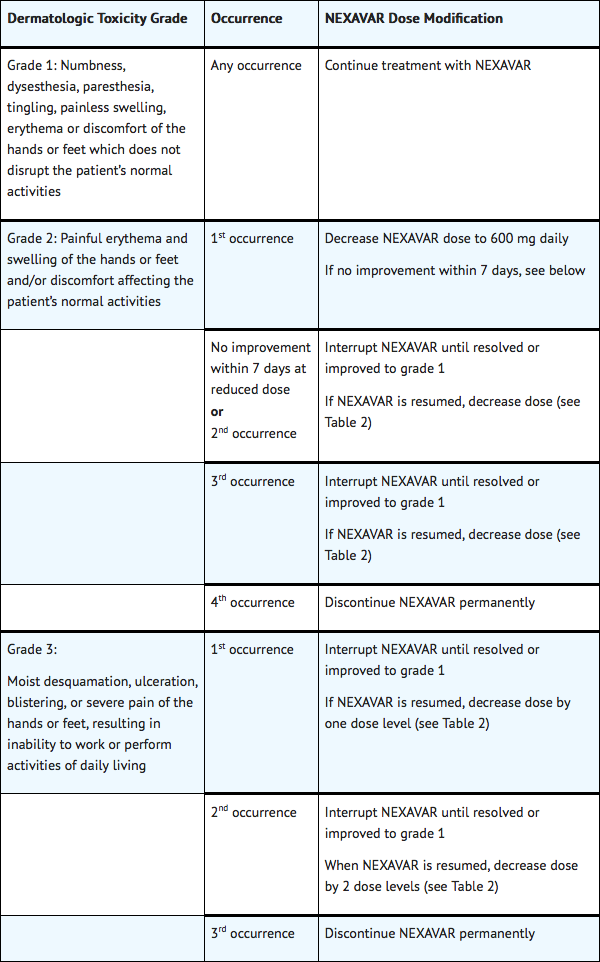
Following improvement of Grade 2 or 3 dermatologic toxicity to Grade 0–1 after at least 28 days of treatment on a reduced dose of Sorafenib, the dose of Sorafenib may be increased one dose level from the reduced dose. Approximately 50% of patients requiring a dose reduction for dermatologic toxicity are expected to meet these criteria for resumption of the higher dose and roughly 50% of patients resuming the previous dose are expected to tolerate the higher dose (that is, maintain the higher dose level without recurrent Grade 2 or higher dermatologic toxicity) |offLabelAdultGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Sorafenib in adult patients. |offLabelAdultNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Sorafenib in adult patients. |offLabelPedGuideSupport=There is limited information regarding Off-Label Guideline-Supported Use of Sorafenib in pediatric patients. |offLabelPedNoGuideSupport=There is limited information regarding Off-Label Non–Guideline-Supported Use of Sorafenib in pediatric patients. |contraindications=*Sorafenib is contraindicated in patients with known severe hypersensitivity to sorafenib or any other component of Sorafenib.
- Sorafenib in combination with carboplatin and paclitaxel is contraindicated in patients with squamous cell lung cancer.
|warnings======Risk of Cardiac Ischemia and/or Infarction=====
- In the HCC study, the incidence of cardiac ischemia/infarction was 2.7% in Sorafenib-treated patients compared with 1.3% in the placebo-treated group, in RCC Study 1, the incidence of cardiac ischemia/infarction was higher in the Sorafenib-treated group (2.9%) compared with the placebo-treated group (0.4%), and in the DTC study, the incidence of cardiac ischemia/infarction was 1.9% in the Sorafenib-treated group compared with 0% in the placebo-treated group. Patients with unstable coronary artery disease or recent myocardial infarction were excluded from this study. Temporary or permanent discontinuation of Sorafenib should be considered in patients who develop cardiac ischemia and/or infarction.
Risk of Hemorrhage
- An increased risk of bleeding may occur following Sorafenib administration. In the HCC study, an excess of bleeding regardless of causality was not apparent and the rate of bleeding from esophageal varices was 2.4% in Sorafenib-treated patients and 4% in placebo-treated patients. Bleeding with a fatal outcome from any site was reported in 2.4% of Sorafenib-treated patients and 4% in placebo-treated patients. In RCC Study 1, bleeding regardless of causality was reported in 15.3% of patients in the Sorafenib-treated group and 8.2% of patients in the placebo-treated group. The incidence of CTCAE Grade 3 and 4 bleeding was 2% and 0%, respectively, in Sorafenib-treated patients, and 1.3% and 0.2%, respectively, in placebo-treated patients. There was one fatal hemorrhage in each treatment group in RCC Study 1. In the DTC study, bleeding was reported in 17.4% of Sorafenib-treated patients and 9.6% of placebo-treated patients; however the incidence of CTCAE Grade 3 bleeding was 1% in Sorafenib-treated patients and 1.4% in placebo-treated patients. There was no Grade 4 bleeding reported and there was one fatal hemorrhage in a placebo-treated patient. If any bleeding necessitates medical intervention, permanent discontinuation of Sorafenib should be considered. Due to the potential risk of bleeding, tracheal, bronchial, and esophageal infiltration should be treated with local therapy prior to administering Sorafenib in patients with DTC.
Risk of Hypertension
- Monitor blood pressure weekly during the first 6 weeks of Sorafenib. Thereafter, monitor blood pressure and treat hypertension, if required, in accordance with standard medical practice. In the HCC study, hypertension was reported in approximately 9.4% of Sorafenib-treated patients and 4.3% of patients in the placebo-treated group. In RCC Study 1, hypertension was reported in approximately 16.9% of Sorafenib-treated patients and 1.8% of patients in the placebo-treated group. In the DTC study, hypertension was reported in 40.6% of Sorafenib-treated patients and 12.4% of placebo-treated patients. Hypertension was usually mild to moderate, occurred early in the course of treatment, and was managed with standard antihypertensive therapy. In cases of severe or persistent hypertension despite institution of antihypertensive therapy, consider temporary or permanent discontinuation of Sorafenib. Permanent discontinuation due to hypertension occurred in 1 of 297 Sorafenib-treated patients in the HCC study, 1 of 451 Sorafenib-treated patients in RCC Study 1, and 1 of 207 Sorafenib-treated patients in the DTC study.
Risk of Dermatologic Toxicities
- Hand-foot skin reaction and rash represent the most common adverse reactions attributed to Sorafenib. Rash and hand-foot skin reaction are usually CTCAE Grade 1 and 2 and generally appear during the first six weeks of treatment with Sorafenib. Management of dermatologic toxicities may include topical therapies for symptomatic relief, temporary treatment interruption and/or dose modification of Sorafenib, or in severe or persistent cases, permanent discontinuation of Sorafenib. Permanent discontinuation of therapy due to hand-foot skin reaction occurred in 4 (1.3%) of 297 Sorafenib-treated patients with HCC, 3 (0.7%) of 451 Sorafenib-treated patients with RCC, and 11 (5.3%) of 207 Sorafenib-treated patients with DTC.
- There have been reports of severe dermatologic toxicities, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). These cases may be life-threatening. Discontinue Sorafenib if SJS or TEN are suspected.
Risk of Gastrointestinal Perforation
- Gastrointestinal perforation is an uncommon adverse reaction and has been reported in less than 1% of patients taking Sorafenib. In some cases this was not associated with apparent intra-abdominal tumor. In the event of a gastrointestinal perforation, discontinue Sorafenib.
Warfarin
- Infrequent bleeding or elevations in the International Normalized Ratio (INR) have been reported in some patients taking warfarin while on Sorafenib. Monitor patients taking concomitant warfarin regularly for changes in prothrombin time (PT), INR or clinical bleeding episodes.
Wound Healing Complications
- No formal studies of the effect of Sorafenib on wound healing have been conducted. Temporary interruption of Sorafenib is recommended in patients undergoing major surgical procedures. There is limited clinical experience regarding the timing of reinitiation of Sorafenib following major surgical intervention. Therefore, the decision to resume Sorafenib following a major surgical intervention should be based on clinical judgment of adequate wound healing.
Increased Mortality Observed with Sorafenib Administered in Combination with Carboplatin/Paclitaxel and Gemcitabine/Cisplatin in Squamous Cell Lung Cancer
- In a subset analysis of two randomized controlled trials in chemo-naive patients with Stage IIIB-IV non-small cell lung cancer, patients with squamous cell carcinoma experienced higher mortality with the addition of Sorafenib compared to those treated with carboplatin/paclitaxel alone (HR 1.81, 95% CI 1.19–2.74) and gemcitabine/cisplatin alone (HR 1.22, 95% CI 0.82-1.80). The use of Sorafenib in combination with carboplatin/paclitaxel is contraindicated in patients with squamous cell lung cancer. Sorafenib in combination with gemcitabine/cisplatin is not recommended in patients with squamous cell lung cancer. The safety and effectiveness of Sorafenib has not been established in patients with non-small cell lung cancer.
Risk of QT Interval Prolongation
- Sorafenib can prolong the QT/QTc interval. QT/QTc interval prolongation increases the risk for ventricular arrhythmias. Avoid Sorafenib in patients with congenital long QT syndrome. Monitor electrolytes and electrocardiograms in patients with congestive heart failure, bradyarrhythmias, drugs known to prolong the QT interval, including Class Ia and III antiarrhythmics. Correct electrolyte abnormalities (magnesium, potassium, calcium). Interrupt Sorafenib if QTc interval is greater than 500 milliseconds or for an increase from baseline of 60 milliseconds or greater.
Drug-Induced Hepatitis
- Sorafenib-induced hepatitis is characterized by a hepatocellular pattern of liver damage with significant increases of transaminases which may result in hepatic failure and death. Increases in bilirubin and INR may also occur. The incidence of severe drug-induced liver injury, defined as elevated transaminase levels above 20 times the upper limit of normal or transaminase elevations with significant clinical sequelae (for example, elevated INR, ascites, fatal, or transplantation), was two of 3,357 patients (0.06%) in a global monotherapy database. Monitor liver function tests regularly. In case of significantly increased transaminases without alternative explanation, such as viral hepatitis or progressing underlying malignancy, discontinue Sorafenib.
Embryofetal Risk
- Based on its mechanism of action and findings in animals, Sorafenib may cause fetal harm when administered to a pregnant woman. Sorafenib caused embryo-fetal toxicities in animals at maternal exposures that were significantly lower than the human exposures at the recommended dose of 400 mg twice daily. Advise women of childbearing potential to avoid becoming pregnant while on Sorafenib because of the potential hazard to the fetus.
Impairment of Thyroid Stimulating Hormone Suppression in Differentiated Thyroid Carcinoma
- Sorafenib impairs exogenous thyroid suppression. In the DTC study, 99% of patients had a baseline thyroid stimulating hormone (TSH) level less than 0.5 mU/L. Elevation of TSH level above 0.5 mU/L was observed in 41% of Sorafenib-treated patients as compared with 16% of placebo-treated patients. For patients with impaired TSH suppression while receiving Sorafenib, the median maximal TSH was 1.6 mU/L and 25% had TSH levels greater than 4.4 mU/L. Monitor TSH levels monthly and adjust thyroid replacement medication as needed in patients with DTC.
|clinicalTrials=====Adverse Reactions in HCC Study==== Adverse Reactions Reported in at Least 10% of Patients and at a Higher Rate in Sorafenib Arm than the Placebo Arm – HCC Study:
Constitutional symptoms
Dermatological/skin Effects
- Rash/Desquamation
- Pruritus
- Hand-Foot skin reaction
- Dry skin
- Alopecia
Gastrointestinal Effects
Hepatobiliary/Pancreas Effects
- Liver dysfunction
- Abdominal pain
Hypertension was reported in 9% of patients treated with Sorafenib and 4% of those treated with placebo. CTCAE Grade 3 hypertension was reported in 4% of Sorafenib-treated patients and 1% of placebo-treated patients. No patients were reported with CTCAE Grade 4 reactions in either treatment group. Hemorrhage/bleeding was reported in 18% of those receiving Sorafenib and 20% of placebo-treated patients. The rates of CTCAE Grade 3 and 4 bleeding were also higher in the placebo-treated group (CTCAE Grade 3 – 3% Sorafenib and 5% placebo and CTCAE Grade 4 – 2% Sorafenib and 4% placebo). Bleeding from esophageal varices was reported in 2.4% in Sorafenib-treated patients and 4% of placebo-treated patients. Renal failure was reported in <1% of patients treated with Sorafenib and 3% of placebo-treated patients. The rate of adverse reactions (including those associated with progressive disease) resulting in permanent discontinuation was similar in both the Sorafenib and placebo-treated groups (32% of Sorafenib-treated patients and 35% of placebo-treated patients).
Laboratory Abnormalities
The following laboratory abnormalities were observed in patients with HCC:
- Hypophosphatemia was a common laboratory finding, observed in 35% of Sorafenib-treated patients compared to 11% of placebo-treated patients; CTCAE Grade 3 hypophosphatemia (1–2 mg/dL) occurred in 11% of Sorafenib-treated patients and 2% of patients in the placebo-treated group; there was 1 case of CTCAE Grade 4 hypophosphatemia (<1 mg/dL) reported in the placebo-treated group. The etiology of hypophosphatemia associated with Sorafenib is not known.
- Elevated lipase was observed in 40% of patients treated with Sorafenib compared to 37% of patients in the placebo-treated group. CTCAE Grade 3 or 4 lipase elevations occurred in 9% of patients in each group. Elevated amylase was observed in 34% of patients treated with Sorafenib compared to 29% of patients in the placebo-treated group. CTCAE Grade 3 or 4 amylase elevations were reported in 2% of patients in each group. Many of the lipase and amylase elevations were transient, and in the majority of cases Sorafenib treatment was not interrupted. Clinical pancreatitis was reported in 1 of 297 Sorafenib-treated patients (CTCAE Grade 2).
- Elevations in liver function tests were comparable between the 2 arms of the study. Hypoalbuminemia was observed in 59% of Sorafenib-treated patients and 47% of placebo-treated patients; no CTCAE Grade 3 or 4 hypoalbuminemia was observed in either group.
- INR elevations were observed in 42% of Sorafenib-treated patients and 34% of placebo-treated patients; CTCAE Grade 3 INR elevations were reported in 4% of Sorafenib-treated patients and 2% of placebo-treated patients; there was no CTCAE Grade 4 INR elevation in either group.
- Lymphopenia was observed in 47% of Sorafenib-treated patients and 42% of placebo-treated patients.
- Thrombocytopenia was observed in 46% of Sorafenib-treated patients and 41% of placebo-treated patients; CTCAE Grade 3 or 4 thrombocytopenia was reported in 4% of Sorafenib-treated patients and less than 1% of placebo-treated patients.
- Hypocalcemia was reported in 27% of Sorafenib-treated patients and 15% of placebo-treated patients. CTCAE Grade 3 hypocalcemia (6–7 mg /dL) occurred in 2% of Sorafenib-treated patients and 1% of placebo-treated patients. CTCAE Grade 4 hypocalcemia (<6 mg/dL) occurred in 0.4% of Sorafenib-treated patients and in no placebo-treated patients.
- Hypokalemia was reported in 9.5% of Sorafenib- treated patients compared to 5.9% of placebo-treated patients. Most reports of hypokalemia were low grade (CTCAE Grade 1). CTCAE Grade 3 hypokalemia occurred in 0.4% of Sorafenib-treated patients and 0.7% of placebo-treated patients. There were no reports of Grade 4 hypokalemia.
Adverse Reactions in RCC Study 1
Adverse Reactions Reported in at Least 10% of Patients and at a Higher Rate in Sorafenib Arm than the Placebo Arm – RCC Study 1:
Cardiovascular Effects
Constitutional Symptoms
Dermatologic Effects
- Rash/Desquamation
- Hand-foot skin reaction
- Alopecia
- Pruritus
- Dry skin
Gastrointestinal Effects
Hemorragic Effects
- Hemorrhage - All sites
Neurological Effects
Pain
Respiratory Effects
Laboratory Findings
The following laboratory abnormalities were observed in patients with RCC in Study 1:
- Hypophosphatemia was a common laboratory finding, observed in 45% of Sorafenib-treated patients compared to 11% of placebo-treated patients. CTCAE Grade 3 hypophosphatemia (1–2 mg/dL) occurred in 13% of Sorafenib-treated patients and 3% of patients in the placebo-treated group. There were no cases of CTCAE Grade 4 hypophosphatemia (<1 mg/dL) reported in either Sorafenib or placebo-treated patients. The etiology of hypophosphatemia associated with Sorafenib is not known.
- Elevated lipase was observed in 41% of patients treated with Sorafenib compared to 30% of patients in the placebo-treated group. CTCAE Grade 3 or 4 lipase elevations occurred in 12% of patients in the Sorafenib-treated group compared to 7% of patients in the placebo-treated group. Elevated amylase was observed in 30% of patients treated with Sorafenib compared to 23% of patients in the placebo-treated group. CTCAE Grade 3 or 4 amylase elevations were reported in 1% of patients in the Sorafenib-treated group compared to 3% of patients in the placebo-treated group. Many of the Sorafenib and amylase elevations were transient, and in the majority of cases Sorafenib treatment was not interrupted. Clinical pancreatitis was reported in 3 of 451 Sorafenib-treated patients (one CTCAE Grade 2 and two Grade 4) and 1 of 451 patients (CTCAE Grade 2) in the placebo-treated group.
- Lymphopenia was observed in 23% of Sorafenib-treated patients and 13% of placebo-treated patients. CTCAE Grade 3 or 4 lymphopenia was reported in 13% of Sorafenib-treated patients and 7% of placebo-treated patients. Neutropenia was observed in 18% of Sorafenib-treated patients and 10% of placebo-treated patients. CTCAE Grade 3 or 4 neutropenia was reported in 5% of Sorafenib-treated patients and 2% of placebo-treated patients.
- Anemia was observed in 44% of Sorafenib-treated patients and 49% of placebo-treated patients. CTCAE Grade 3 or 4 anemia was reported in 2% of Sorafenib-treated patients and 4% of placebo-treated patients.
- Thrombocytopenia was observed in 12% of Sorafenib-treated patients and 5% of placebo-treated patients. CTCAE Grade 3 or 4 thrombocytopenia was reported in 1% of Sorafenib-treated patients and in no placebo-treated patients.
- Hypocalcemia was reported in 12% of Sorafenib-treated patients and 8% of placebo-treated patients. CTCAE Grade 3 hypocalcemia (6–7 mg/dL) occurred in 1% of Sorafenib-treated patients and 0.2% of placebo-treated patients, and CTCAE Grade 4 hypocalcemia (<6 mg/dL) occurred in 1% of Sorafenib-treated patients and 0.5% of placebo-treated patients.
- Hypokalemia was reported in 5.4% of Sorafenib-treated patients compared to 0.7% of placebo-treated patients. Most reports of hypokalemia were low grade (CTCAE Grade 1). CTCAE Grade 3 hypokalemia occurred in 1.1% of Sorafenib-treated patients and 0.2% of placebo-treated patients. There were no reports of Grade 4 hypokalemia.
Adverse Reactions in DTC Study
Per-Patient Incidence of Selected Adverse Reactions Occurring at a Higher Incidence in Sorafenib-Treated Patients [Between Arm Difference of ≥ 5% (All Grades)1 or ≥ 2% (Grades 3 and 4)]:
Gastrointestinal Effects
General Disorders and Administration Site Conditions
Investigations
Metabolism and Nutrition Disorders
Musculoskeletal and connective tissue disorders
Neoplasms benign, malignant and unspecified
Central Nervous System Effects
Respiratory, thoracic and mediastinal disorders
Skin and Subcutaneous Tissue Disorders
Vascular Disorders
Laboratory Findings
- Elevated TSH levels are discussed elsewhere in the labeling. The relative increase for the following laboratory abnormalities observed in Sorafenib-treated DTC patients as compared to placebo-treated patients is similar to that observed in the RCC and HCC studies: lipase, amylase, hypokalemia, hypophosphatemia, neutropenia, lymphopenia, anemia, and thrombocytopenia.
- Serum ALT and AST elevations were observed in 59% and 54% of the Sorafenib-treated patients as compared to 24% and 15% of placebo-treated patients, respectively. High grade (≥ 3) ALT and AST elevations were observed in 4% and 2%, respectively, in the Sorafenib-treated patients as compared to none of the placebo-treated patients.
- Hypocalcemia was more frequent and more severe in patients with DTC, especially those with a history of hypoparathyroidism, compared to patients with RCC or HCC. Hypocalcemia was observed in 36% of DTC patients receiving Sorafenib (with 10% ≥ Grade 3) as compared with 11% of placebo-treated patients (3% ≥ Grade 3). In the DTC study, serum calcium levels were monitored monthly.
Additional Data from Multiple Clinical Trials
The following additional drug-related adverse reactions and laboratory abnormalities were reported from clinical trials of Sorafenib (very common 10% or greater, common 1 to less than 10%, uncommon 0.1% to less than 1%, rare less than 0.1 %):
- Cardiovascular
- Common: congestive heart failure, myocardial ischemia and/or infarction
- Uncommon: hypertensive crisis
- Rare: QT prolongation
- Dermatologic
- Very common: erythema
- Common: exfoliative dermatitis, acne, flushing, folliculitis, hyperkeratosis
- Uncommon: eczema, erythema and multiform.
- Digestive
- Very common: increased lipase, increased amylase
- Common: mucositis, stomatitis (including dry mouth and glossodynia), dyspepsia, dysphagia, gastrointestinal reflux
- Uncommon: pancreatitis, gastritis, gastrointestinal perforations, cholecystitis, cholangitis
- Note that elevations in lipase are very common (41%, see below); a diagnosis of pancreatitis should not be made solely on the basis of abnormal laboratory values
- General Disorders
- Very common: infection, hemorrhage (including gastrointestinal and respiratory tract and uncommon cases of cerebral hemorrhage), asthenia, pain (including mouth, bone, and tumor pain), pyrexia, decreased appetite
- Common: influenza-like illness.
- Hematologic
- Very common: leukopenia, lymphopenia
- Common: anemia, neutropenia, thrombocytopenia
- Uncommon: INR abnormal
- Hepatobiliary disorders:
Rare: drug-induced hepatitis (including hepatic failure and death)
- Hypersensitivity
- Uncommon: hypersensitivity reactions (including skin reactions and urticaria), anaphylactic reaction
- Metabolic and Nutritional
- Very common: hypophosphatemia
- Common: transient increases in transaminases, hypocalcemia, hypokalemia, hyponatremia, hypothyroidism
- Uncommon: dehydration, transient increases in alkaline phosphatase, increased bilirubin (including jaundice), hyperthyroidism
- Musculoskeletal
- Very common: arthralgia
- Common: myalgia, muscle spasms
- Nervous System and Psychiatric
- Common: depression, dysgeusia
- Uncommon: tinnitus, reversible posterior leukoencephalopathy
- Renal and Genitourinary
- Common: renal failure, proteinuria
- Rare: nephrotic syndrome
- Reproductive
- Common: erectile dysfunction
- Uncommon: gynecomastia
- Respiratory
- Common: rhinorrhea
- Uncommon: interstitial lung disease-like events (includes reports of pneumonitis, radiation pneumonitis, acute respiratory distress, interstitial pneumonia, pulmonitis and lung inflammation)
In addition, the following medically significant adverse reactions were uncommon during clinical trials of Sorafenib: transient ischemic attack, arrhythmia, and thromboembolism. For these adverse reactions, the causal relationship of Sorafenib has not been established. |postmarketing=The following adverse drug reactions have been identified during post-approval use of Sorafenib. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Dermatologic: Stevens-Johnson syndrome and toxic epidermal necrolysis (TEN)
- Hypersensitivity: Angioedema
- Musculoskeletal: Rhabdomyolysis, osteonecrosis of the jaw
- Respiratory: Interstitial lung disease-like events (which may have a life-threatening or fatal outcome)
|drugInteractions======Effect of Strong CYP3A4 Inducers on Sorafenib=====
- Rifampin, a strong CYP3A4 inducer, administered at a dose of 600 mg once daily for 5 days with a single oral dose of Sorafenib 400 mg in healthy volunteers resulted in a 37% decrease in the mean AUC of sorafenib. Avoid concomitant use of strong CYP3A4 inducers (such as, carbamazepine, dexamethasone, phenobarbital, phenytoin, rifampin, rifabutin, St. John’s wort), when possible, because these drugs can decrease the systemic exposure to sorafenib.
Effect of Strong CYP3A4 Inhibitors on Sorafenib
- Ketoconazole, a strong inhibitor of CYP3A4 and P-glycoprotein, administered at a dose of 400 mg once daily for 7 days did not alter the mean AUC of a single oral dose of Sorafenib 50 mg in healthy volunteers.
Effect of Sorafenib on Other Drugs
- Sorafenib 400 mg twice daily for 28 days did not increase the systemic exposure of concomitantly administered midazolam (CYP3A4 substrate), dextromethorphan (CYP2D6 substrate), and omeprazole (CYP2C19 substrate)
Neomycin
- Neomycin administered as an oral dose of 1 g three times daily for 5 days decreased the mean AUC of sorafenib by 54% in healthy volunteers administered a single oral dose of Sorafenib 400 mg. The effects of other antibiotics on the pharmacokinetics of sorafenib have not been studied.
Drugs that Increase Gastric pH
- The aqueous solubility of sorafenib is pH dependent, with higher pH resulting in lower solubility. However, omeprazole, a proton pump inhibitor, administered at a dose of 40 mg once daily for 5 days, did not result in a clinically meaningful change in sorafenib single dose exposure. No dose adjustment for Sorafenib is necessary.
|FDAPregCat=D |useInPregnancyFDA=*Based on its mechanism of action and findings in animals, Sorafenib may cause fetal harm when administered to a pregnant woman. Sorafenib caused embryo-fetal toxicities in animals at maternal exposures that were significantly lower than the human exposures at the recommended dose of 400 mg twice daily. There are no adequate and well-controlled studies in pregnant women using Sorafenib Inform patients of childbearing potential that Sorafenib can cause birth defects or fetal loss. Instruct both men and women of childbearing potential to use effective birth control during treatment with Sorafenib and for at least 2 weeks after stopping treatment. Counsel female patients to contact their healthcare provider if they become pregnant while taking Sorafenib.
- When administered to rats and rabbits during the period of organogenesis, sorafenib was teratogenic and induced embryo-fetal toxicity (including increased post-implantation loss, resorptions, skeletal retardations, and retarded fetal weight). The effects occurred at doses considerably below the recommended human dose of 400 mg twice daily (approximately 500 mg/m2/day on a body surface area basis). Adverse intrauterine development effects were seen at doses ≥0.2 mg/kg/day (1.2 mg/m2/day) in rats and 0.3 mg/kg/day (3.6 mg/m2/day) in rabbits. These doses result in exposures (AUC) approximately 0.008 times the AUC seen in patients at the recommended human dose. A NOAEL (no observed adverse effect level) was not defined for either species, since lower doses were not tested.
|useInNursing=*It is not known whether sorafenib is excreted in human milk. Because many drugs are excreted in human milk and because of the potential for serious adverse reactions in nursing infants from Sorafenib, a decision should be made whether to discontinue nursing or to discontinue the drug, taking into account the importance of the drug to the mother.
- Following administration of radiolabeled sorafenib to lactating Wistar rats, approximately 27% of the radioactivity was secreted into the milk. The milk to plasma AUC ratio was approximately 5:1.
|useInPed=The safety and effectiveness of Sorafenib in pediatric patients have not been studied.
- Repeat dosing of sorafenib to young and growing dogs resulted in irregular thickening of the femoral growth plate at daily sorafenib doses ≥ 600 mg/m2 (approximately 0.3 times the AUC at the recommended human dose), hypocellularity of the bone marrow adjoining the growth plate at 200 mg/m2/day (approximately 0.1 times the AUC at the recommended human dose), and alterations of the dentin composition at 600 mg/m2/day. Similar effects were not observed in adult dogs when dosed for 4 weeks or less.
|useInGeri=*In total, 59% of HCC patients treated with Sorafenib were age 65 years or older, and 19% were 75 and older. In total, 32% of RCC patients treated with Sorafenib were age 65 years or older, and 4% were 75 and older. No differences in safety or efficacy were observed between older and younger patients, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. |useInRenalImpair=*No correlation between sorafenib exposure and renal function was observed following administration of a single oral dose of Sorafenib 400 mg to subjects with normal renal function and subjects with mild (CLcr 50–80 mL/min), moderate (CLcr 30–<50 mL/min), or severe (CLcr <30 mL/min) renal impairment who are not on dialysis. No dose adjustment is necessary for patients with mild, moderate or severe renal impairment who are not on dialysis. The pharmacokinetics of sorafenib have not been studied in patients who are on dialysis |useInHepaticImpair=*In a trial of HCC patients with mild (Child-Pugh A) or moderate (Child-Pugh B) hepatic impairment, the systemic exposure (AUC) of sorafenib was within the range observed in patients without hepatic impairment. In another trial in subjects without HCC, the mean AUC was similar for subjects with mild (n=15) and moderate (n=14) hepatic impairment compared to subjects (n=15) with normal hepatic function. No dose adjustment is necessary for patients with mild or moderate hepatic impairment. The pharmacokinetics of sorafenib have not been studied in patients with severe (Child-Pugh C) hepatic impairment |administration=*Oral (tablets) |overdose=*There is no specific treatment for Sorafenib overdose. The highest dose of Sorafenib studied clinically is 800 mg twice daily. The adverse reactions observed at this dose were primarily diarrhea and dermatologic. No information is available on symptoms of acute overdose in animals because of the saturation of absorption in oral acute toxicity studies conducted in animals. In cases of suspected overdose, Sorafenib should be withheld and supportive care instituted. |drugBox=
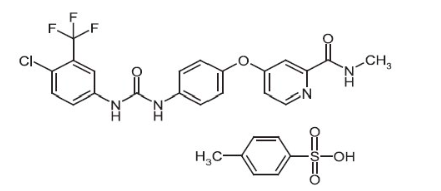
|mechAction=*Sorafenib is a kinase inhibitor that decreases tumor cell proliferation in vitro. Sorafenib was shown to inhibit multiple intracellular (c-CRAF, BRAF and mutant BRAF) and cell surface kinases (KIT, FLT- 3, RET, RET/PTC, VEGFR-1, VEGFR- 2, VEGFR- 3, and PDGFR-ß). Several of these kinases are thought to be involved in tumor cell signaling, angiogenesis and apoptosis. Sorafenib inhibited tumor growth of HCC, RCC, and DTC human tumor xenografts in immunocompromised mice. Reductions in tumor angiogenesis were seen in models of HCC and RCC upon sorafenib treatment, and increases in tumor apoptosis were observed in models of HCC, RCC, and DTC. |structure=*Sorafenib tosylate has the chemical name 4-(4-{3-[4-Chloro-3-(trifluoromethyl)phenyl]ureido}phenoxy)N2-methylpyridine-2-carboxamide 4-methylbenzenesulfonate and its structural formula is:
|PD=*The effect of Sorafenib 400 mg twice daily on the QTc interval was evaluated in a multi-center, open-label, non-randomized trial in 53 patients with advanced cancer. No large changes in the mean QTc intervals (that is, >20 ms) from baseline were detected in the trial. After one 28-day treatment cycle, the largest mean QTc interval change of 8.5 ms (upper bound of two-sided 90% confidence interval, 13.3 ms) was observed at 6 hours post-dose on day 1 of cycle 2 |PK=*The mean elimination half-life of sorafenib was approximately 25 to 48 hours. Multiple doses of Sorafenib for 7 days resulted in a 2.5- to 7-fold accumulation compared to a single dose. Steady-state plasma sorafenib concentrations were achieved within 7 days, with a peak-to-trough ratio of mean concentrations of less than 2. The steady-state concentrations of sorafenib following administration of 400 mg Sorafenib twice daily were evaluated in DTC, RCC and HCC patients. Patients with DTC have mean steady-state concentrations that are 1.8-fold higher than patients with HCC and 2.3-fold higher than those with RCC. The reason for increased sorafenib concentrations in DTC patients is unknown.
Absorption and Distribution
- After administration of Sorafenib tablets, the mean relative bioavailability was 38–49% when compared to an oral solution. Following oral administration, sorafenib reached peak plasma levels in approximately 3 hours. With a moderate-fat meal (30% fat; 700 calories), bioavailability was similar to that in the fasted state. With a high-fat meal (50% fat; 900 calories), bioavailability was reduced by 29% compared to that in the fasted state. It is recommended that Sorafenib be administered without food. Mean Cmax and AUC increased less than proportionally beyond oral doses of 400 mg administered twice daily. In vitro binding of sorafenib to human plasma proteins was 99.5%.
Metabolism and Elimination
- Sorafenib undergoes oxidative metabolism by hepatic CYP3A4, as well as glucuronidation by UGT1A9. Inducers of CYP3A4 activity can decrease the systemic exposure of sorafenib. Sorafenib accounted for approximately 70–85% of the circulating analytes in plasma at steady-state. Eight metabolites of sorafenib have been identified, of which 5 have been detected in plasma. The main circulating metabolite of sorafenib, the pyridine N-oxide that comprises approximately 9–16% of circulating analytes at steady-state, showed in vitro potency similar to that of sorafenib. Following oral administration of a 100 mg dose of a solution formulation of sorafenib, 96% of the dose was recovered within 14 days, with 77% of the dose excreted in feces and 19% of the dose excreted in urine as glucuronidated metabolites. Unchanged sorafenib, accounting for 51% of the dose, was found in feces but not in urine.
Effects of Age, Gender and Race
- A study of the pharmacokinetics of sorafenib indicated that the mean AUC of sorafenib in Asians (N=78) was 30% lower than in Caucasians (N=40). Gender and age do not have a clinically meaningful effect on the pharmacokinetics of sorafenib.
Renal Impairment
- Mild (CLcr 50-80 mL/min), moderate (CLcr 30 - <50 mL/min), and severe (CLcr <30 mL/min) renal impairment do not affect the pharmacokinetics of sorafenib. No dose adjustment is necessary.
Hepatic Impairment
- Mild (Child-Pugh A) and moderate (Child-Pugh B) hepatic impairment do not affect the pharmacokinetics of sorafenib. No dose adjustment is necessary.
Drug-Drug Interactions
Studies in human liver microsomes demonstrated that sorafenib competitively inhibited CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, and CYP3A4. However, Sorafenib 400 mg twice daily for 28 days with substrates of CYP3A4, CYP2D6 and CYP2C19 did not increase the systemic exposure of these substrates. Studies with cultured human hepatocytes demonstrated that sorafenib did not increase CYP1A2 and CYP3A4 activities, suggesting that sorafenib is unlikely to induce CYP1A2 or CYP3A4 in humans. Sorafenib inhibits glucuronidation by UGT1A1 and UGT1A9 in vitro. Sorafenib could increase the systemic exposure of concomitantly administered drugs that are UGT1A1 or UGT1A9 substrates. Sorafenib inhibited P-glycoprotein in vitro. Sorafenib could increase the concentrations of concomitantly administered drugs that are P-glycoprotein substrates. |nonClinToxic======Carcinogenesis, Mutagenesis, Impairment of Fertility=====
- Carcinogenicity studies have not been performed with sorafenib. Sorafenib was clastogenic when tested in an in vitro mammalian cell assay (Chinese hamster ovary) in the presence of metabolic activation. Sorafenib was not mutagenic in the in vitro Ames bacterial cell assay or clastogenic in an in vivo mouse micronucleus assay. One intermediate in the manufacturing process, which is also present in the final drug substance (<0.15%), was positive for mutagenesis in an in vitro bacterial cell assay (Ames test) when tested independently.
- No specific studies with sorafenib have been conducted in animals to evaluate the effect on fertility. However, results from the repeat-dose toxicity studies suggest there is a potential for sorafenib to impair reproductive function and fertility. Multiple adverse effects were observed in male and female reproductive organs, with the rat being more susceptible than mice or dogs. Typical changes in rats consisted of testicular atrophy or degeneration, degeneration of epididymis, prostate, and seminal vesicles, central necrosis of the corpora lutea and arrested follicular development. Sorafenib-related effects on the reproductive organs of rats were manifested at daily oral doses ≥ 5 mg/kg (30 mg/m2). This dose results in an exposure (AUC) that is approximately 0.5 times the AUC in patients at the recommended human dose. Dogs showed tubular degeneration in the testes at 30 mg/kg/day (600 mg/m2/day). This dose results in an exposure that is approximately 0.3 times the AUC at the recommended human dose. Oligospermia was observed in dogs at 60 mg/kg/day (1200 mg/m2/day) of sorafenib. Adequate contraception should be used during therapy and for at least 2 weeks after completing therapy.
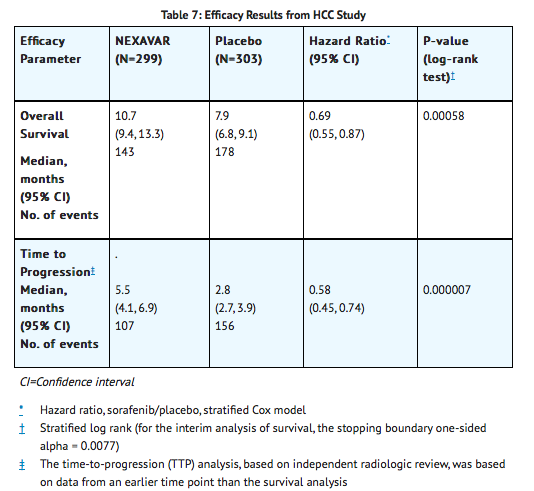
|clinicalStudies======Hepatocellular Carcinoma=====
- The HCC Study was a Phase 3, international, multicenter, randomized, double blind, placebo-controlled trial in patients with unresectable hepatocellular carcinoma. Overall survival was the primary endpoint. A total of 602 patients were randomized; 299 to Sorafenib 400 mg twice daily and 303 to matching placebo. Demographics and baseline disease characteristics were similar between the Sorafenib and placebo-treated groups with regard to age, gender, race, performance status, etiology (including hepatitis B, hepatitis C and alcoholic liver disease), TNM stage (stage I: <1% vs. <1%; stage II: 10.4% vs. 8.3%; stage III: 37.8% vs. 43.6%; stage IV: 50.8% vs. 46.9%), absence of both macroscopic vascular invasion and extrahepatic tumor spread (30.1% vs. 30.0%), and Barcelona Clinic Liver Cancer stage (stage B: 18.1% vs. 16.8%; stage C: 81.6% vs. 83.2%; stage D: <1% vs. 0%). Liver impairment by Child-Pugh score was comparable between the Sorafenib and placebo-treated groups (Class A: 95% vs. 98%; B: 5% vs. 2%). Only one patient with Child-Pugh class C was entered. Prior treatments included surgical resection procedures (19.1% vs. 20.5%), locoregional therapies (including radiofrequency ablation, percutaneous ethanol injection and transarterial chemoembolization; 38.8% vs. 40.6%), radiotherapy (4.3% vs. 5.0%) and systemic therapy (3.0% vs. 5.0%).
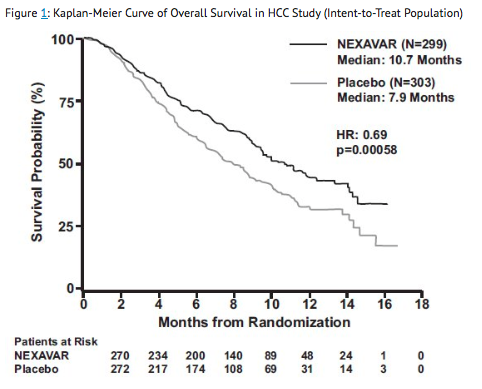
- The trial was stopped for efficacy following a pre-specified second interim analysis for survival showing a statistically significant advantage for Sorafenib over placebo for overall survival (HR: 0.69, p= 0.00058) (see Table 4 and Figure 1). This advantage was consistent across all subsets analyzed. Final analysis of time to tumor progression (TTP) based on data from an earlier time point (by independent radiologic review) also was significantly longer in the Sorafenib arm (HR: 0.58, p=0.000007).
Renal Cell Carcinoma
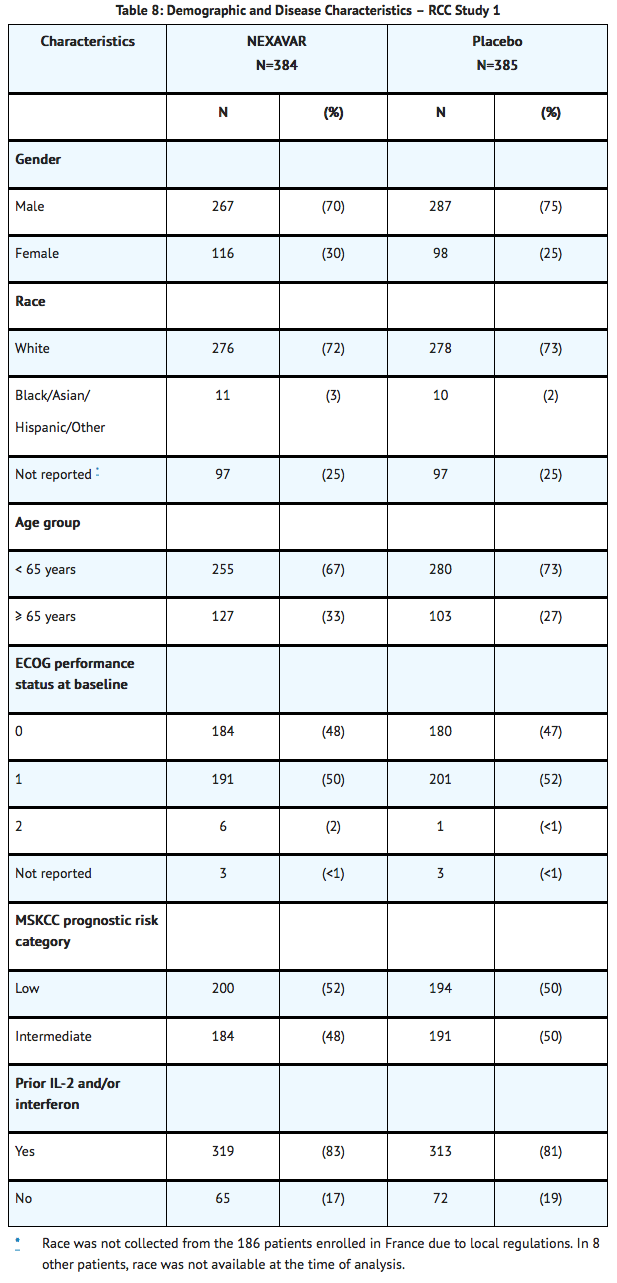
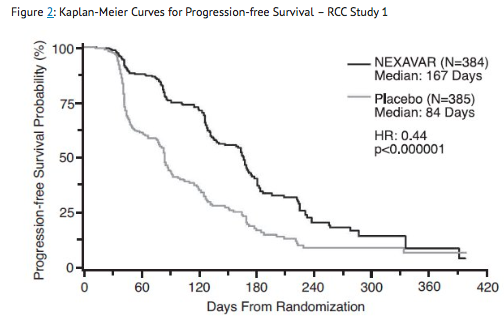
- The safety and efficacy of Sorafenib in the treatment of advanced renal cell carcinoma (RCC) were studied in the following two randomized controlled clinical trials. RCC Study 1 was a Phase 3, international, multicenter, randomized, double blind, placebo-controlled trial in patients with advanced renal cell carcinoma who had received one prior systemic therapy. Primary study endpoints included overall survival and progression-free survival (PFS). Tumor response rate was a secondary endpoint. The PFS analysis included 769 patients stratified by MSKCC (Memorial Sloan Kettering Cancer Center) prognostic risk category (low or intermediate) and country and randomized to Sorafenib 400 mg twice daily (N=384) or to placebo (N=385). Table 8 summarizes the demographic and disease characteristics of the study population analyzed. Baseline demographics and disease characteristics were well balanced for both treatment groups. The median time from initial diagnosis of RCC to randomization was 1.6 and 1.9 years for the Sorafenib and placebo-treated groups, respectively.
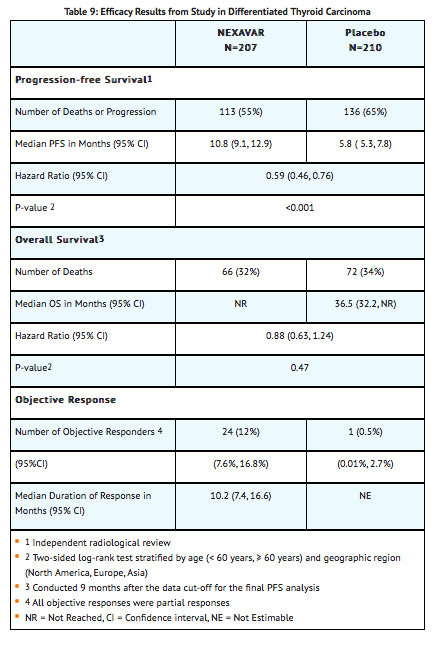
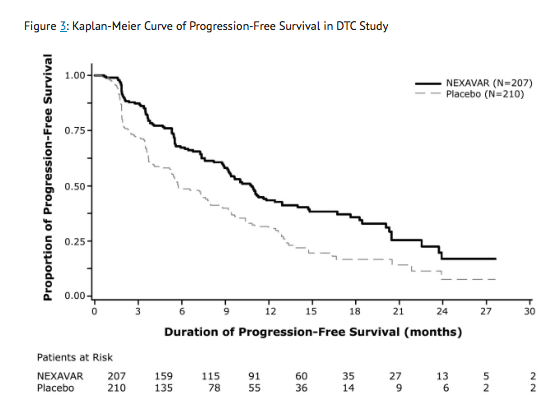
Differentiated Thyroid Carcinoma
- The safety and effectiveness of Sorafenib was established in a multicenter, randomized (1:1), double-blind, placebo-controlled trial conducted in 417 patients with locally recurrent or metastatic, progressive differentiated thyroid carcinoma (DTC) refractory to radioactive iodine] (RAI) treatment]. Randomization was stratified by age (< 60 years versus ≥ 60 years) and geographical region (North America, Europe, and Asia).
- All patients were required to have actively progressing disease defined as progression within 14 months of enrollment. RAI-refractory disease was defined based on four criteria that were not mutually exclusive. All RAI treatments and diagnostic scans were to be performed under conditions of a low iodine diet and adequate TSH stimulation. Following are the RAI-refractory criteria and the proportion of patients in the study that met each one: a target lesion with no iodine uptake on RAI scan (68%); tumors with iodine uptake and progression after RAI treatment within 16 months of enrollment (12%); tumors with iodine uptake and multiple RAI treatments with the last treatment greater than 16 months prior to enrollment, and disease progression after each of two RAI treatments administered within 16 months of each other (7%); cumulative RAI dose ≥ 600 mCi administered (34%). The major efficacy outcome measure was progression-free survival (PFS) as determined by a blinded, independent radiological review using a modified Response Evaluation Criteria in Solid Tumors v. 1.0 (RECIST). RECIST was modified by inclusion of clinical progression of bone lesions based on the need for external beam radiation (4.4% of progression events). Additional efficacy outcomes measures included overall survival (OS), tumor response rate, and duration of response.
- Patients were randomized to receive Sorafenib 400 mg twice daily (n=207) or placebo (n=210). Of the 417 patients randomized, 48% were male, the median age was 63 years, 61% were 60 years or older, 60% were white, 62% had an ECOG performance status of 0, and 99% had undergone thyroidectomy. The histological diagnoses were papillary carcinoma in 57%, follicular carcinoma (including Hürthle cell) in 25%, and poorly differentiated carcinoma in 10%, and other in 8% of the study population. Metastases were present in 96% of the patients: lungs in 86%, lymph nodes in 51%, and bone in 27%. The median cumulative RAI activity administered prior to study entry was 400 mCi. A statistically significant prolongation in PFS was demonstrated among Sorafenib-treated patients compared to those receiving placebo. Following investigator-determined disease progression, 157 (75%) patients randomized to placebo crossed over to open-label Sorafenib, and 61 (30%) patients randomized to Sorafenib received open-label Sorafenib There was no statistically significant difference in overall survival between the two treatment arms (see Table 9 and Figure 3).
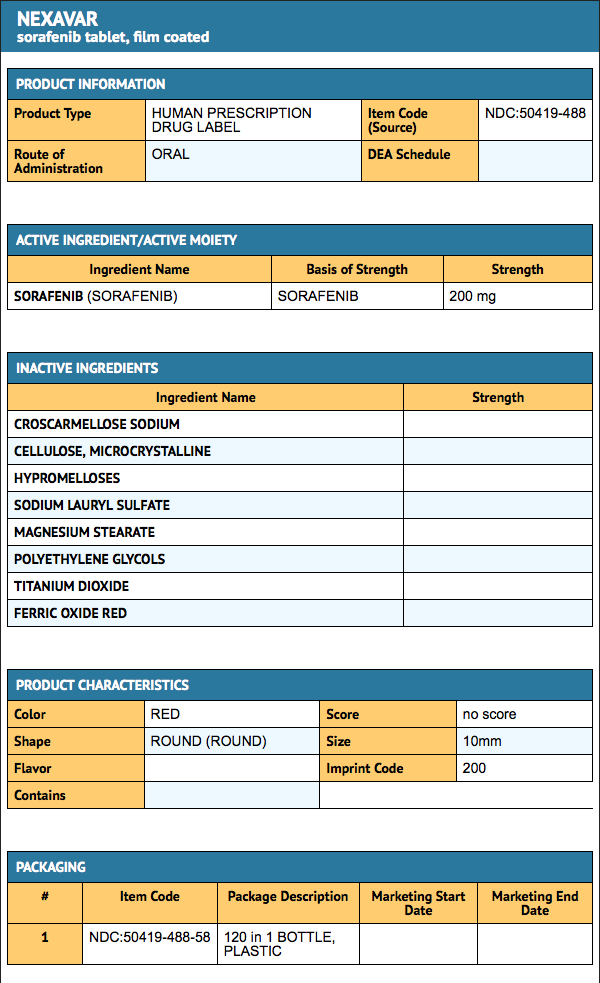
|howSupplied=Sorafenib tablets are supplied as round, biconvex, red film-coated tablets, debossed with the “Bayer cross” on one side and “200” on the other side, each containing sorafenib tosylate equivalent to 200 mg of sorafenib.
Bottles of 120 tablets NDC 50419-488-58 |storage=Store at 25°C (77°F); excursions permitted to 15–30°C (59–86°F). Store in a dry place.
|drugImages=

|packLabel=
|alcohol=Alcohol-Sorafenib interaction has not been established. Talk to your doctor about the effects of taking alcohol with this medication. |brandNames=*NexAVAR }} {{#subobject:
|Label Page=Sorafenib |Label Name=SorafenibPackage.png
}}